Introduction
Obstructive bronchiolitis (OB) is a rare disease and
affects small airways of the lung and is associated with
restriction of the airways (1). OB
must be considered as a potential diagnosis in patients with
obstructive respiratory impairment, the most common symptom of
which is dyspnea (1). This
inflammatory process is associated with various conditions,
including ulcerative colitis (UC) and toxic epidermal necrolysis
(TEN). UC is a chronic relapsing inflammatory bowel disease of
uncertain etiology. UC may occur at any age, but is most commonly
diagnosed in late adolescence or early adulthood (2). The incidence of UC has increased
worldwide over recent decades, particularly in developing nations
(2). Typical symptoms of UC include,
bloody diarrhea, abdominal pain, urinary urgency and tenesmus
(2). TEN is acute drug-induced
condition associated with severe blistering, skin peeling and
multi-organ damage, and is classed in the same spectrum of diseases
as Stevens-Johnson syndrome (3,4). TEN
symptoms typically resemble severe scalding, with ≥30% top layer of
skin detaching from the lower dermis (3). OB must be considered as a differential
diagnosis in patients with obstructive respiratory impairment
(4). In the case reported in the
present study a patient with ulcerative colitis (UC), who developed
toxic epidermal necrolysis (TEN) (5)
following mesalazine therapy, presented with severe airflow
limitation.
Case report
A 53-year-old male was received at the Mito Medical
Center (Mito, Japan) with a two-month history of exertional
dyspnea, which was not accompanied by a dry cough, fever, chill or
chest pain. There was no history of antecedent respiratory tract
infection. The patient had a 15-pack-year smoking history, having
stopped 20 years previously, and no allergies. There was no
recognized history of exposure to fumes or mineral dusts. The
patient had been diagnosed as having UC 25 years previously and was
given mesalazine therapy, since therapy with prednisolone had not
led to any improvement in the UC. Following an increase in the dose
of mesalazine to 2,250 mg/day, the patient developed a high fever
(>38°C) and a large number of red papules and erythemas. The
eruptions rapidly spread to the whole body and changed to
erythroderma in one week. The eruptions additionally caused
blistering, epidermolysis and erosion of >10% of the body's
surfaces a few days later. No findings suggested staphylococcal
scalded skin syndrome. Based on the skin symptoms and clinical
course, the patient was diagnosed with TEN due to the mesalazine.
The patient received several courses of steroid pulse therapy with
methylprednisolone and plasma exchange therapy. The patient
recovered from the TEN as a result of these intensive therapies,
although scars and pigmentation in the trunk and extremities
remained. Informed consent was obtained from the patient.
On admission, the respiratory rate of the patient
was 18 beats/min and his breath sound was diminished, without any
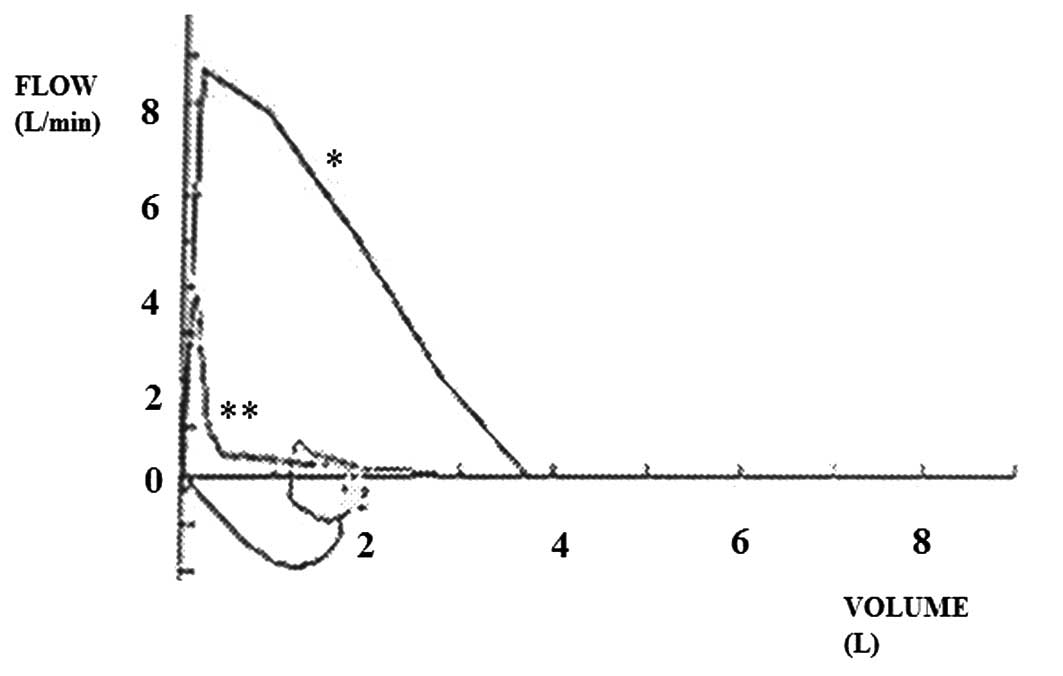
expiratory rhonchi. Clubbing was absent. The forced expiratory
volume in one second (FEV1.0) was 0.77 liters (36.4% of
predicted) and the forced vital capacity was 2.97 liters (80.1% of
predicted). A flow-volume curve showed airflow limitation (Fig. 1). The residual volume was 2.57 liters
(153% of predicted), the functional residual capacity was 3.97
liters (97% of predicted) and the single-breath diffusing capacity
of the lung for carbon monoxide (DLCO) and
DLCO divided by alveolar volume (DLCO/VA)
were 105 and 93% of the predicted values, respectively. A chest
radiograph showed scarce hyperinflation. No improvement in the
FEV1.0 was observed following inhalation of a
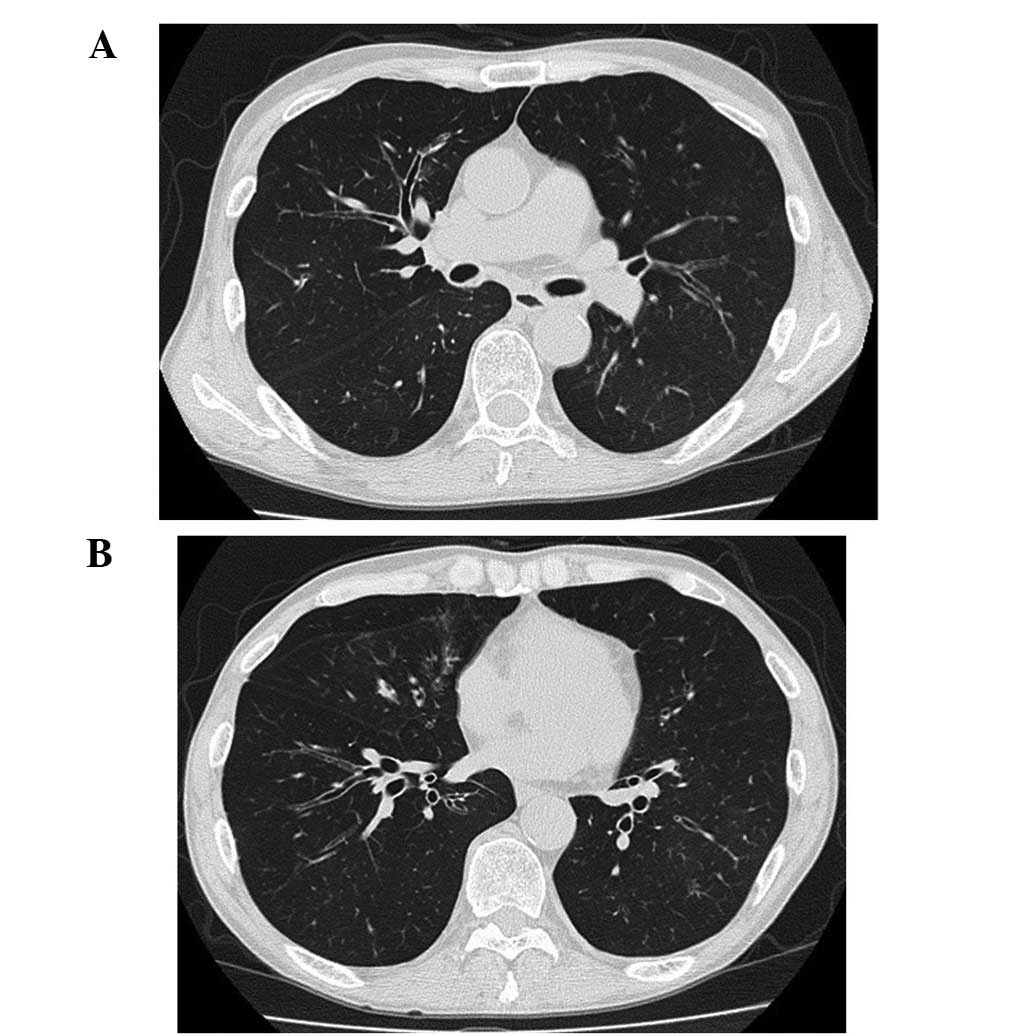
β-stimulant. A chest computed tomography (CT) scan showed only a
small number of low-attenuation areas and bullae and demonstrated
central bronchiectasis and a mosaic pattern, which intensified on
expiration (Fig. 2). These findings
were not consistent with pulmonary emphysema as a cause of severe
airflow limitation. The results, including a respiratory function
test and radiological examination, were highly suggestive of OB.
Inhalation of corticosteroid and anticholinergic agents, oral
theophylline and inhaled corticosteroid were not effective in this
patient. Respiratory rehabilitation and long-acting
β2-agonist/inhaled corticosteroid appeared to cause a slight
reduction in his exertional dyspnea; however, the potential role of
these therapies requires further examination. The patient did not
recover completely. Twenty-six months following disease onset the
patient remained alive and was discharged from the outpatient
clinic.
Discussion
OB is an inflammatory process that primarily affects
small conducting airways of the lungs, resulting in differing
levels of airflow limitation (2).
This inflammatory process is associated with numerous conditions,
including UC (5–7), bullous skin disease (8), Stevens-Johnson syndrome (9–14), graft
versus host disease following a lung or bone marrow transplant
(15–18) and certain drugs (1,6). The
current patient was a middle-aged ex-smoker who complained of
sub-acutely developed exertional dyspnea. Early-onset chronic
obstructive pulmonary disease was initially suspected from the
patient's symptoms and severe irreversible airway limitation;
however, the chest CT scan was not consistent with smoking-induced
centrilobular emphysema in this case, although the diagnosis of
panlobular emphysema could not be refuted. It is generally accepted
that decreases in DLCO and DLCO/VA are useful
indicators of pulmonary emphysema (19,20);
therefore, these parameters were evaluated, but no decreases were
found despite severe irreversible airflow limitation. A mosaic
pattern and bronchiectasis have been reported to be the typical
findings in OB, although there have been cases demonstrating only
diffuse hyperinflation, bronchial wall thickening and
bronchiectasis, or even normal findings on a CT scan (21,22). In
the present patient, a chest CT scan showed bronchiectasis and
thickening of the walls of the central bronchi in both lungs.
In the present case, the patient had UC and had
received plasma exchange for the treatment of TEN, which are known
causes of OB (1,4–6,23). TEN and Stevens-Johnson syndrome are
defined as drug-related dermatopathies on the same spectrum
(4), and a case of severe OB
associated with TEN has been previously reported (24). We speculated that the OB in the
present case may have developed as a result of an impairment of the
respiratory mucous membrane, as observed in Stevens-Johnson
syndrome, and that there was a high probability that this severe
airflow limitation had an association with the development of TEN
due to mesalazine therapy. Thus, if drugs were directly responsible
for the development of OB in this patient, mesalazine would be a
highly probable candidate.
Regarding adverse events due to mesalazine, certain
pulmonary toxicities have already been reported (5,6,25). Notably, two previous reports have
described OB in patients with UC receiving mesalazine (6,7), as
observed in the present case; however, the cause and precise
mechanism of OB resulting from mesalazine treatment is not
currently known.
Pathological examination of the affected bronchioles
is important to the diagnosis of OB (1,26). The
narrowing of bronchioles by necrotic and fibrotic changes are the
main pathogeneses of OB (1,26); however, the majority of the patients
with OB have exertional dyspnea with airflow limitation and it may,
therefore, be challenging to obtain sufficient specimens from these
individuals. The present patient declined a surgical approach, and
the lung specimen could not be obtained.
In conclusion, the present study describes a case of
OB in a patient with UC who developed TEN following mesalazine
therapy. This rare clinical combination should be considered as a
differential diagnosis, even for middle-aged, ex-smoking subjects
presenting with sub-acutely developed airflow obstruction, if the
findings in the chest CT scan demonstrate hyperinflation but few
low-attenuation areas. Relatively well-preserved DLCO
and DLCO/VA can provide a clue to establishing a correct
diagnosis.
References
|
1
|
Burgel PR, Bergeron A, de Blic J, et al:
Small airways diseases, excluding asthma and COPD: An overview. Eur
Respir Rev. 22:131–147. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Feuerstein JD and Cheifetz AS: Ulcerative
colitis: Epidemiology, diagnosis, and management. Mayo Clin Proc.
89:1553–1563. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mawson AR, Eriator I and Karre S:
Stevens-Johnson syndrome and Toxic Epidermal Necrolysis (SJS/TEN):
Could retinoids play a causative role? Med Sci Monit. 21:133–143.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Letko E, Papaliodis DN, Papaliodis GN,
Daoud YJ, Ahmed AR and Foster CS: Stevens-Johnson syndrome and
toxic epidermal necrolysis: A review of the literature. Ann Allergy
Asthma Immunol. 94:419–436. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nanayakkara PW, de Jong E and Postmus PE:
Bilateral pulmonary infiltrates in a patient with ulcerative
colitis receiving mesalazine. Eur J Intern Med. 15:470–472. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Haralambou G, Teirstein AS, Gil J and
Present DH: Bronchiolitis obliterans in a patient with ulcerative
colitis receiving mesalazine. Mt Sinai J Med. 68:384–388.
2001.PubMed/NCBI
|
|
7
|
Sakamoto N, Ishimatsu Y, Koyama H, et al:
Bronchiolitis in a patient with ulcerative colitis treated with
erythromycin. Intern Med. 53:875–877. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Oshikawa K, Sugiyama Y and Kitamura S:
Diffuse panbronchioliltis associated with bullous pemphigoid. Nihon
Kyobu Shikkan Gakkai Zasshi. 33:1019–1023. 1995.[(In Japanese)].
PubMed/NCBI
|
|
9
|
Tsunoda N, Iwanaga T, Saito T, Kitamura S
and Saito K: Rapidly progressive bronchiolitis obliterans
associated with Stevens-Johnson syndrome. Chest. 98:243–245. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shah AP, Xu H, Sime PJ and Trawick DR:
Severe airflow obstruction and eosinophilic lung disease after
Stevens-Johnson syndrome. Eur Respir J. 28:1276–1279. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Basker M, Cherian T and Raghupathy P:
Chronic lung disease following Stevens-Johnson syndrome. Indian
Pediatr. 34:831–835. 1997.PubMed/NCBI
|
|
12
|
Yatsunami J, Nakanishi Y, Matsuki H, et
al: Chronic bronchobronchiolitis obliterans associated with
Stevens-Johnson syndrome. Intern Med. 34:772–775. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
de la Rocha Reyes S, Leonard JC and
Demetriou E: Potential permanent respiratory sequela of
Stevens-Johnson syndrome in an adolescent. J Adolesc Health Care.
6:220–223. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Virant FS, Redding GJ and Novack AH:
Multiple pulmonary complications in a patient with Stevens-Johnson
syndrome. Clin Pediatr (Phila). 23:412–414. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ryu JH, Myers JL and Swensen SJ:
Bronchiolar disorders. Am J Respir Crit Care Med. 168:1277–1292.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Epler GR: Bronchiolitis obliterans and
airways obstruction associated with graft-versus-host disease. Clin
Chest Med. 9:551–556. 1988.PubMed/NCBI
|
|
17
|
Wyatt SE, Nunn P, Hows JM, et al: Airways
obstruction associated with graft versus host disease after bone
marrow transplantation. Thorax. 39:887–894. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ralph DD, Springmeyer SC, Sullivan KM,
Hackman RC, Storb R and Thomas ED: Rapidly progressive air-flow
obstruction in marrow transplant recipients. Possible association
between obliterative bronchiolitis and chronic graft-versus-host
disease. Am Rev Respir Dis. 129:641–644. 1984.PubMed/NCBI
|
|
19
|
Morrison NJ, Abboud RT, Ramadan F, et al:
Comparison of single breath carbon monoxide diffusing capacity and
pressure-volume curves in detecting emphysema. Am Rev Respir Dis.
139:1179–1187. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Biernacki W, Gould GA, Whyte KF and
Flenley DC: Pulmonary hemodynamics, gas exchange and the severity
of emphysema as assessed by quantitative CT scan in chronic
bronchitis and emphysema. Am Rev Respir Dis. 139:1509–1515. 1989.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tsujino I, Nishimura M, Ohira K, Yoshimura
H, Fukuda Y and Kawakami Y: A case of idiopathic constrictive
bronchiolitis in a middle-aged male smoker. Respirology. 5:305–307.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Karadag F, Ozhan MH, Akçiçek E, Günel O,
Alper H and Veral A: Is it possible to detect ulcerative
colitis-related respiratory syndrome early? Respirology. 6:341–346.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ishida T, Yokoyama E, Muto M, et al: A
case of paraneoplastic pemphigus associated with bronchiolitis
obliterans-like respiratory symptoms in the absence of a known
neoplasm. Nishi Nihon Hifuka. 66:236–240. 2004.[(In Japanese)].
View Article : Google Scholar
|
|
24
|
Kamada N, Kinoshita K, Togawa Y, et al:
Chronic pulmonary complications associated with toxic epidermal
necrolysis: Report of a severe case with anti-Ro/SS-A and a review
of the published work. J Dermatol. 33:616–622. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kim JH, Lee JH, Koh ES, et al: Acute
eosinophilic pneumonia related to a mesalazine suppository. Asia
Pac Allergy. 3:136–139. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Allen TC: Pathology of small airways
disease. Arch Pathol Lab Med. 134:702–718. 2010.PubMed/NCBI
|