Introduction
Dietary salt restriction is recommended for the
prevention of cardiovascular disease in patients with hypertension
and heart failure as well as in the general population (1,2).
However, salt reduction is challenging to achieve in the real
world, particularly in countries in which salt consumption is
extremely high, such as Japan. We have previously reported that the
estimation of salt intake using the spot urine method may be a
useful tool to motivate patients to reduce their salt intake for
8–26 weeks (3), and the efficacy of
this method was found to be maintained at long-term (up to 2 years)
follow-up (4). However, the
percentage of patients who could achieve a reduction in salt intake
to the recommended level was very low (<10–15%) (3,4). In
particular, patients who habitually consume large amounts of salt
at baseline find it difficult to reduce salt intake to the
recommended level regardless of gender, age and body weight
(4). This might be partly explained
by the lack of dietary counseling by expert dietitians in the
majority (93%) of the patients included in the previous study
(4).
The purpose of the present study was to assess the
effects of single-session dietary counseling on salt reduction in
addition to the spot urine-guided salt reduction approach in
outpatients who consumed large amounts of salt.
Materials and methods
Patients
This was a prospective observational study of
patients who visited the outpatient cardiology clinic of Ueki
Hospital (Kumamoto, Japan) between May 2011 and October 2013. These
patients were followed up until April 2014. Salt excretion was
measured at the time of enrollment, the next office visit (3–9
weeks) and at 24–52 weeks during follow-up. The average level of
salt excretion during the 24 weeks prior to the time of enrollment
was used as the baseline value. The average level of salt excretion
during weeks 24–52 was used as the week 24–52 value. Salt excretion
at the time of the next office visit at 3–9 weeks was not averaged
(single value). Attending physicians explained the individual data
to the patients and encouraged them to reduce their salt intake by
simple counseling at every office visit when their salt excretion
was measured. Dietary counseling by expert dietitians was provided
to the patients at the discretion of the attending physicians.
Patients who had a salt intake of >8.0 g/day as estimated using
the spot urine method at baseline and received dietary counseling
by expert dieticians were included in this study. Age- and
gender-matched patients who did not received dietary counseling by
dieticians and consumed >8 g/day of salt served as control
patients. They were retrospectively selected between January 2013
and June 2013, and the follow-up data were obtained between July
2013 and December 2013. For the evaluation of salt excretion levels
in the control group, the average values obtained between January
2013 and June 2013 were used as the baseline values and those
obtained between July 2013 and December 2013 were used as the
follow-up values.
Hypertension was defined as a systolic blood
pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg or treatment
with antihypertensive medications. Changes in blood pressure were
evaluated in patients in whom antihypertensive medications were
unchanged during follow-up. Congestive heart failure was defined as
having symptoms of class II or above according to the New York
Heart Association (NYHA) classification and/or congestive signs
requiring loop diuretics at the time of entry. Diabetes mellitus
was defined as fasting plasma glucose ≥126 mg/dl, casual glucose
level ≥200 mg/dl, glycated hemoglobin levels ≥6.5%, receiving oral
hypoglycemic medications or using insulin.
The study protocol was approved by the ethics
committee of Ueki Hospital, and informed written consent was
obtained from all patients.
Estimation of salt excretion
Daily salt excretion levels were estimated using the
following equation (5,6): Estimated 24-h urinary salt excretion
(g/day) = 1.285 × [Na(mEq/l)/Cr(mg/l) in spot urine × expected 24 h
Cr excretion]0.392, where the expected 24-h Cr excretion
(mg/day) = −2.04 × age (years) + 14.89 × weight (kg) + 16.14 ×
height (cm) – 2244.45.
Statistical analysis
Data are presented as the means ± standard
deviation. The event frequencies were compared using the
χ2 test. Differences in the variables were compared
using one-way analysis of variance when there were 3 groups,
followed by Tukey-Kramer honest significant difference tests.
Comparisons between the two groups of data were made using paired
or unpaired Student's t-tests. A P level of <0.05 was considered
to be statistically significant. The statistical software package
JMP (version 9; SAS Institute, Cary, NC, USA) was used for the
analyses.
Results
Characteristics of the patients
A total of 72 patients were included in this study.
The baseline characteristics of the patients are presented in
Table I; these characteristics were
similar to those reported in previous studies (3,4), with
the exception that the salt excretion levels were considerably
higher. There were no differences in the characteristics between
patients who received dietary counseling and those who did not (the
control group).
 | Table I.Characteristics of the patients. |
Table I.
Characteristics of the patients.
| Characteristics | Case (dietary
counseling) | Control | P-value |
|---|
| Number | 72 | 72 |
|
| Gender,
female/male | 30/42 | 30/42 |
|
| Age, years | 73±11 (40–94) | 73±10 (46–92) | 0.90 |
| Body mass index,
kg/m2 | 25±3.3 (17–37) | 25±3.7 (15–34) | 0.82 |
| Salt excretion,
g/day | 11.3±1.5
(8.6–16.4) | 11.2±1.4
(8.7–14.8) | 0.59 |
| Hypertension, n
(%) | 57 (79) | 60 (83) | 0.41 |
| Diabetes mellitus, n
(%) | 16 (22) | 21 (29) | 0.34 |
| Congestive heart
failure, n (%) | 16 (22) | 10 (14) | 0.19 |
| Permanent atrial
fibrillation, n (%) | 15 (21) | 11 (15) | 0.39 |
| Medications, n
(%) |
|
|
|
|
ACEI/ARBs | 41 (57) | 46 (64) | 0.39 |
| Calcium
channel blockers | 27 (38) | 37 (51) | 0.094 |
|
β-blockers | 25 (35) | 17 (24) | 0.14 |
| Loop
diuretics | 13 (18) | 11 (15) | 0.65 |
| Thiazide
diuretics | 10 (14) | 4 (5.6) | 0.092 |
Changes in daily salt excretion
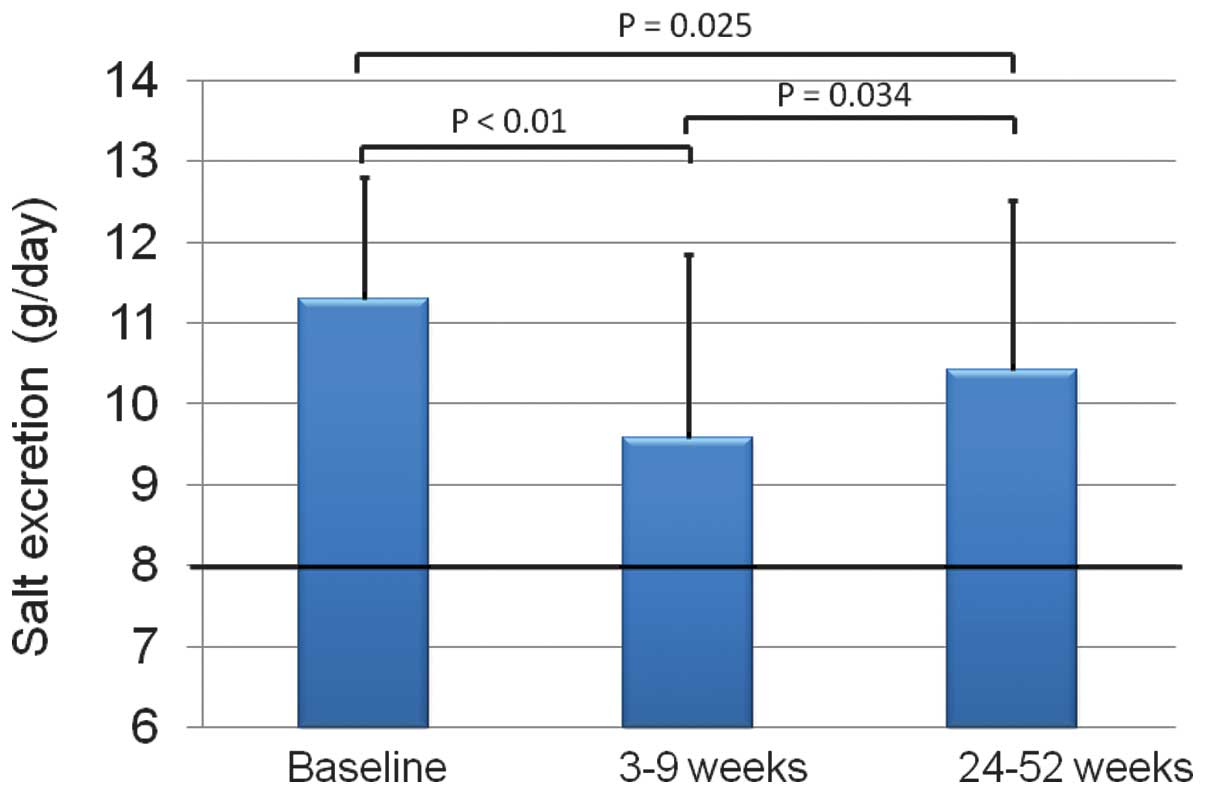
Fig. 1 shows the
dietary salt excretion levels at baseline, 3–9 weeks and 24–52
weeks. The baseline estimated level of salt excretion was 11.3±1.5
(range, 8.6–16.4) g/day, which was reduced to 9.6±2.3 (range,
4.6–14.4) g/day at 3–9 weeks, but increased again at 24–52 weeks to
10.4±2.1 (range, 6.4–17.2) g/day, which was less than the baseline
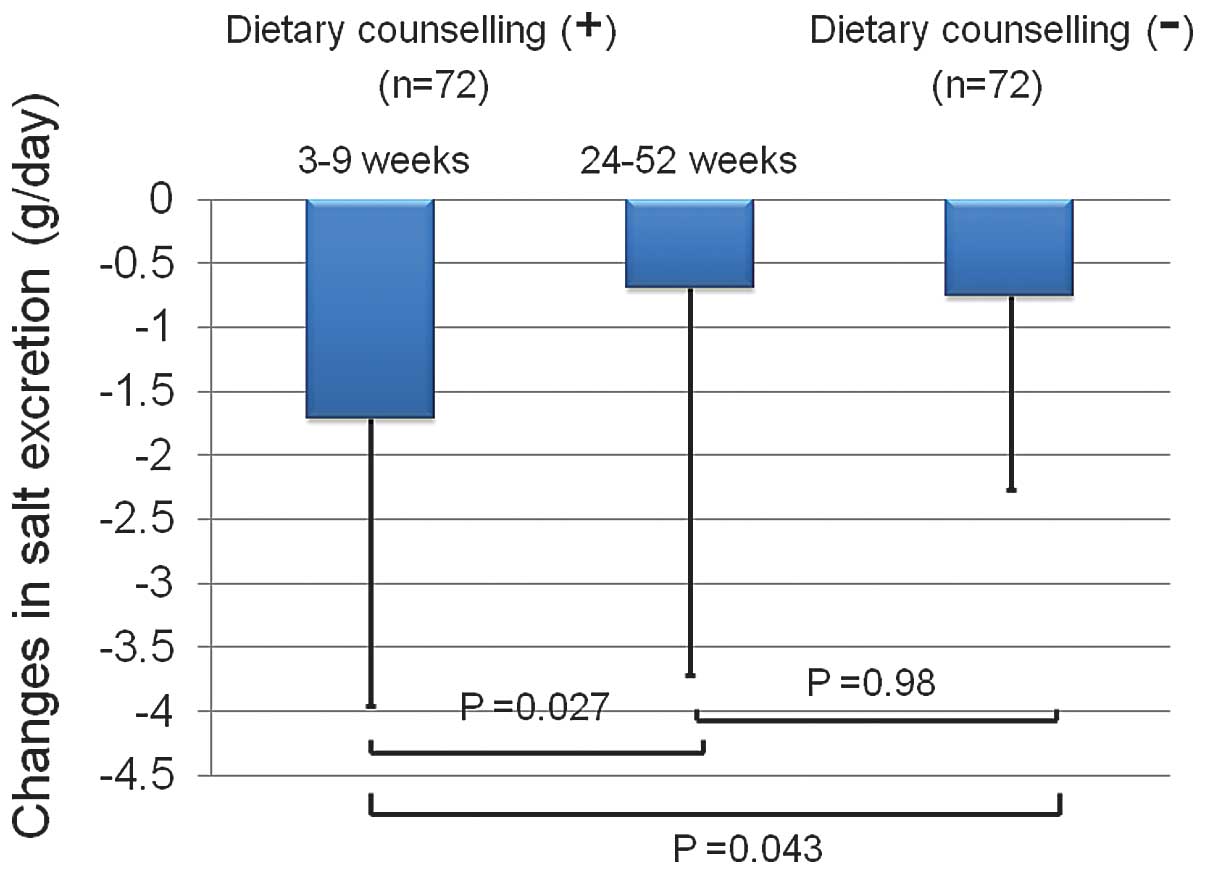
value. Fig. 2 shows the changes in
the level of salt excretion from the baseline value. At 3–9 weeks,
the change in salt excretion was −1.7±2.5 (range, −8.0 to 1.3)
g/day, but at 24–52 weeks the change was reduced to −0.69±3.0
(range, −6.8 to 6.4) g/day, which was not different from that of
age- and gender- matched control patients without dietary
counseling (−0.76±1.5 g/day; range, −5.4 to 3.0 g/day). The number
of patients in whom the reduction in salt excretion was >2 g/day
from baseline was 29 (40%) at 3–9 weeks. Of these 29 patients, salt
excretion was reduced by <2 g/day or increased from baseline at
24–52 weeks in 14 patients. However, of the 43 patients in whom the
reduction in salt excretion was <2 g/day at 3–9 weeks, a
reduction of >2 g/day was newly achieved in 7 patients; thus a
reduction in salt excretion of >2 g/day was achieved in 22 (31%)
patients at 24–52 weeks during follow-up evaluation. The numbers of
patients who achieved salt excretion levels of <6.0 and <8.0
g/day were only 4 (5.6%) and 19 (26%) at 3–9 weeks, respectively,
and were further reduced to no patients (0%; P=0.043 vs. 3–9 weeks)
and 9 (13%; P=0.035 vs. 3–9 weeks) patients at 24–52 weeks
follow-up, respectively.
Effect of the number of measurements
prior to dietary counseling on salt excretion
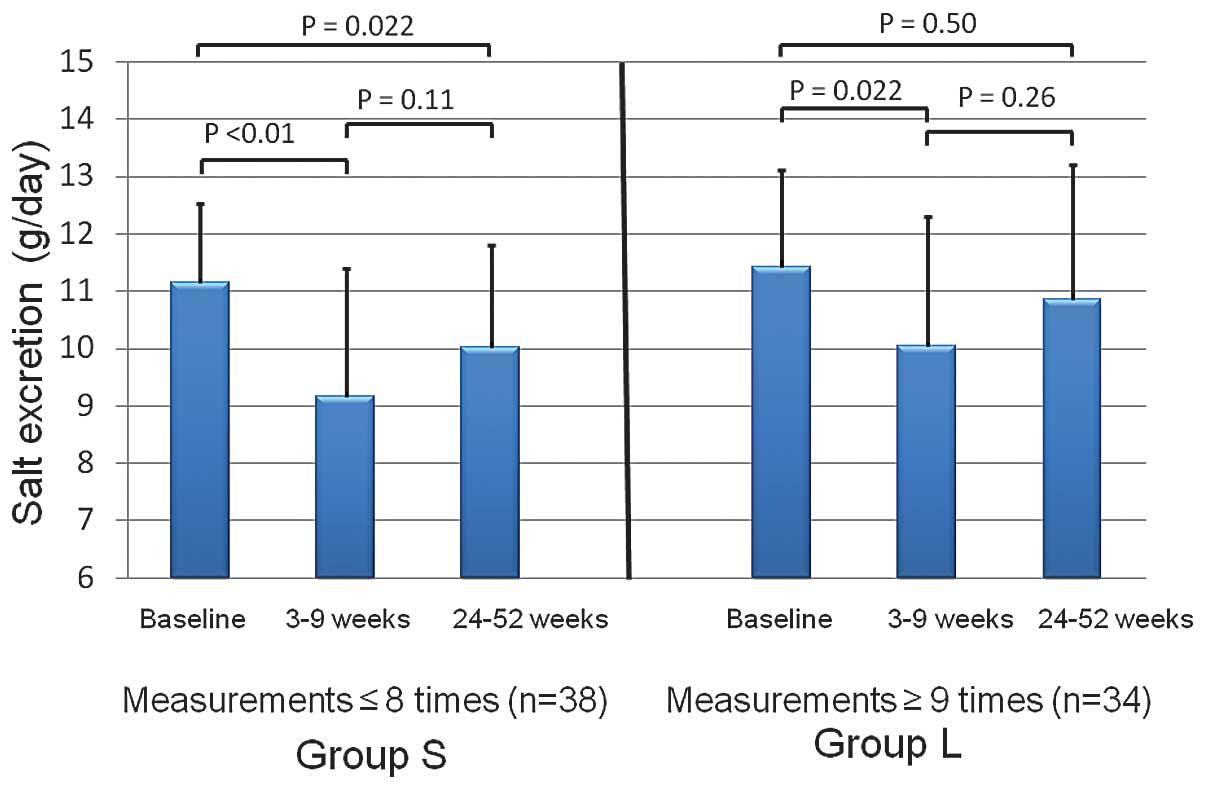
Fig. 3 shows the
effect of the number of measurements made prior to dietary
counseling on the levels of salt excretion. Salt excretion was
measured 8.7±6.1 (range, 1–24; median, 8) times prior to dietary
counseling. Thus, the patients were divided into two groups
according to the median number of measurements. Salt excretion was
measured 4.0±2.6 (range, 1–8; median, 3.5) times in group S (n=38),
and 14.1±4.1 (range, 9–24; median, 13) times in group L (n=34). The
baseline level of salt excretion was not different between these
two groups (11.2±1.4 vs. 11.4±1.7 g/day, respectively; P=0.44).
Changes in salt excretion following dietary counseling at 3–9 weeks
were also not different between these groups (−2.0±2.6 vs. −1.4±1.8
g/day respectively; P=0.26). However, while salt excretion remained
different from the baseline value at 24–52 weeks in patients in
group S (P=0.022), the difference disappeared in patients in group
L (P=0.50).
Effects on blood pressure
Of the 57 hypertensive patients included in this
study, hypertensive medications remained unchanged in 34 patients.
The systolic blood pressure was numerically reduced from 129.2±10.3
to 125.2±11.7 mmHg; however, the difference did not reach
statistical significance (P=0.066, by paired t-test). The diastolic
pressure was also not significantly changed from 75.1±8.0 to
72.7±10.2 mmHg (P=0.13, by paired t-test).
Discussion
This study demonstrated that the efficacy of
single-session dietary counseling by expert dieticians in reducing
the salt intake of cardiology outpatients who consumed large
amounts of salt was modest and only temporary, and achieving salt
reductions to the level recommended by the guideline (7,8) was very
difficult in Japanese outpatients.
Previously, Buccicone et al (9) reported that single short (15 min)
counseling sessions with advice on salt reduction by dieticians
reduced the sodium intake estimated from the patients' recall of
food eaten over the previous 24 h from 115.5 ± 48.1 to 51.7 ± 33.9
mEq/24 h (p<0.01). However, no effects were actually observed
when using sodium excretion calculated from a 24-h urine sample
(155.4 ± 99.8 to 137.4 ± 52.8 mEq/24 h; not significant).
Similarly, Korhonen et al (10) reported that the 2-year net changes in
daily sodium excretion were not different between a group that
received intensified diet counseling (every 3 months) and a control
group. The findings of the present study are consistent with these
reports. However, more vigorous intervention, including group
meetings and a free supply of low-salt bread, did reduce salt
excretion (11,12). Although single-session dietary
counseling by dieticians in addition to simple counseling by
attending physicians may seem to be unproductive efforts,
particularly in patients who consume large amounts of salt despite
repeated instructions by their attending physicians (Fig. 3), it was at least temporarily
effective in some patients. Thus, it should always be considered
possible to achieve reductions in salt intake in individual
resistant patients. More comprehensive approaches, such as repeated
dietary counseling in every office visit with multiple medical
staff, including physicians, nurses as well as expert dieticians;
group meetings or cooking sessions among similar patients who have
not been able to reduce salt intake; and a short-term provision of
low salt-containing food, for example, low salt soy sauce and low
salt miso (fermented soybean paste) in the case of Japan, may be a
feasible next step for further salt reduction in primary care
settings (13).
The present study has certain limitations. First,
the estimation of daily urinary salt excretion using a spot urine
sample may be less accurate than that using 24-h urine collection,
as previously noted (3,4). However, it is difficult to collect 24-h
urine in real-world practice. Second, this was not a randomized
study and the patients were enrolled solely at the discretion of
the attending physicians. Furthermore, control patients were
retrospectively included. However, the control patients were well
matched with the case patients for age, gender, body mass index and
daily salt excretion (Table I), and
the changes in salt excretion were consistent with those previously
reported (3,4). Thus, it is considered that selection
bias was not sufficiently large to affect the main conclusions of
the study. Third, dietary counseling by expert dieticians was
performed only once according to the study design, and repeated
counseling might have produced better outcomes. Fourth, the
antihypertensive medications were changed in more than half of the
patients who were included in this study during follow-up; thus, an
evaluation of the changes in blood pressure observed in the present
study is of limited value. Finally, this was a single-center study
with a small number of patients; additional multicenter studies
including a large number of patients are required.
In conclusion, the efficacy of salt restriction by
dietary counseling by expert dieticians in patients who consumed
large amounts of salt was modest and temporary. Multiple
nutritional- and behavioral-oriented approaches should be
considered for further salt reduction.
References
|
1
|
Appel LJ, Frohlich ED, Hall JE, Pearson
TA, Sacco RL, Seals DR, Sacks FM, Smith SC Jr, Vafiadis DK and Van
Horn LV: The importance of population-wide sodium reduction as a
means to prevent cardiovascular disease and stroke. A call to
action from the American Heart Association. Circulation.
123:1138–1143. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
He FJ and MacGregor GA: A comprehensive
review on salt and health and current experience of worldwide salt
reduction programmes. J Hum Hypertens. 23:363–384. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hirota S, Sadanaga T, Mitamura H and
Fukuda K: Spot urine-guided salt reduction is effective in Japanese
cardiology outpatients. Hypertens Res. 35:1069–1071. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hirota S, Sadanaga T, Mitamura H and
Fukuda K: Long-term compliance with salt restriction assessed using
the spot urine method in Japanese cardiology outpatients. Hypertens
Res. 36:1096–1099. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Matsuo S, Imai E, Horio M, Yasuda Y,
Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H and Hishida A:
Collaborators developing the Japanese equation for estimated GFR:
Revised equations for estimated GFR from serum creatinine in Japan.
Am J Kidney Dis. 53:982–992. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tanaka T, Okamura T, Miura K, Kadowaki T,
Ueshima H, Nakagawa H and Hashimoto T: A simple method to estimate
populational 24-h urinary sodium and potassium excretion using a
casual urine specimen. J Hum Hypertens. 16:97–103. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kawano Y, Tsuchihashi T, Matsuura H, Ando
K, Fujita T and Ueshima H: Working Group for Dietary Salt Reduction
of the Japanese Society of Hypertension: Report of the Working
Group for Dietary Salt Reduction of the Japanese Society of
Hypertension: (2) Assessment of salt intake in the management of
hypertension. Hypertens Res. 30:887–893. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ogihara T, Kikuchi K, Matsuoka H, Fujita
T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario
K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H,
Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S,
Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura
S, Ishimitsu T and Rakugi H: Japanese Society of Hypertension
Committee: The Japanese Society of Hypertension Guidelines for the
Management of Hypertension (JSH 2009). Hypertens Res. 32:3–107.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Buccicone J and McAllister RG Jr: Failure
of single-session dietary counseling to reduce salt intake in
hypertensive patients. South Med J. 70:1436–1438. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Korhonen M, Kastarinen M, Uusitupa M,
Puska P and Nissinen A: The effect of intensified diet counseling
on the diet of hypertensive subjects in primary health care: A
2-year open randomized controlled trial of lifestyle intervention
against hypertension in eastern Finland. Prev Med. 36:8–16. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Korhonen MH, Litmanen H, Rauramaa R,
Väisänen SB, Niskanen L and Uusitupa M: Adherence to the salt
restriction diet among people with mildly elevated blood pressure.
Eur J Clin Nutr. 53:880–885. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Elmer PJ, Grimm RH Jr, Flack J and Laing
B: Dietary sodium reduction for hypertension prevention and
treatment. Hypertension. 17:(Suppl 1). I182–I189. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ruzicka M, Hiremath S, Steiner S, Helis E,
Szczotka A, Baker P and Fodor G: What is the feasibility of
implementing effective sodium reduction strategies to treat
hypertension in primary care settings? A systematic review. J
Hypertens. 32:1388–1394. 2014. View Article : Google Scholar : PubMed/NCBI
|