Introduction
Traumatic carotid-cavernous fistula (TCCF) is a rare
complication of head trauma that comprises an abnormal
communication between the internal carotid artery and the cavernous
sinus. It is characterized by the following cardinal symptoms:
Exophthalmos, ocular pulsation, intracranial bruit, cranial nerve
palsy, epistaxis, brain ischemia and intracranial hemorrhage
(1); however, the clinical
presentation of brainstem edema in TCCF is rare, and only six cases
to date have been reported (2–6).
Clinical symptoms are primarily determined by the direction of the
venous drainage. For instance, ophthalmic symptoms are more likely
with venous drainage through the ophthalmic vein, and intracranial
hemorrhage is more common with venous drainage via the cortical
veins. In addition, high-flow shunting often leads to intracranial
bruit (7). Due to its rarity,
however, there is little information available regarding the
clinical characteristics and the underlying mechanisms of brainstem
edema caused by TCCF. The present report describes a rare case of
TCCF with brainstem edema. In addition, we review the six known
cases of brainstem edema in TCCF and discuss the potential
mechanisms and prognosis of the condition.
Case report
A 51-year-old man presenting with right exophthalmos
and intracranial bruit for 1 week was admitted to the First
Affiliated Hospital of Jilin University (Changchun, China). The
patient had a bone fracture in the frontal and ethmoid sinuses due
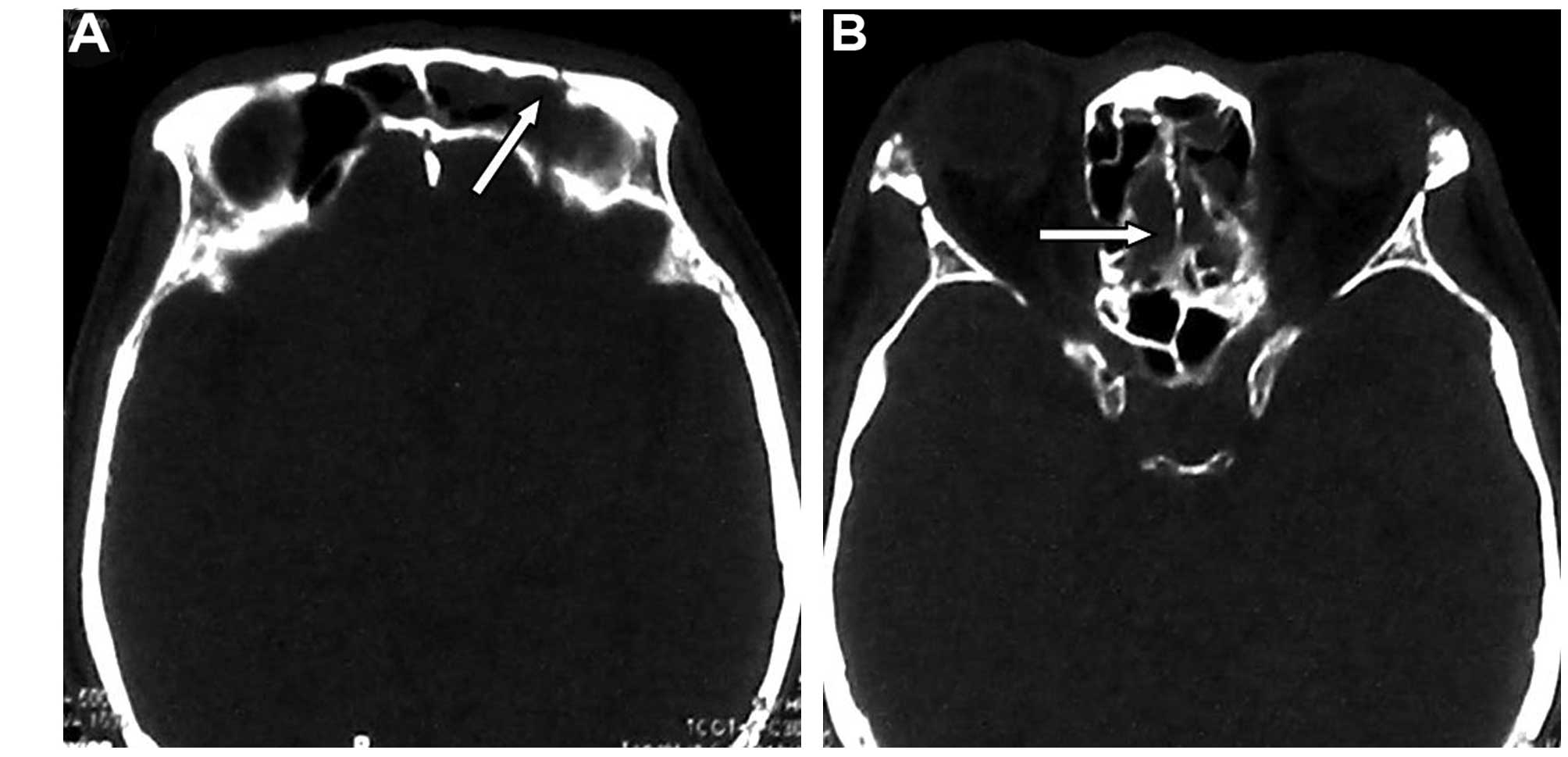
to a car accident 1 month prior to admission. Cranial computed
tomography (CT) bone window photography performed at the time of
the accident revealed a bone fracture and hemorrhage in the frontal
and ethmoid sinuses (Fig. 1). He
received conservative treatment and was discharged following the
alleviation of the symptoms.
On examination, the right eye was proptotic with
conjunctival congestion, and the visual acuity in the right eye of
the patient was 0.5. Fundus examination revealed venous congestion
and edema. A loud bruit in synchronization with the heartbeat was
auscultated over the right orbit and the temporal bone. The eyeball
was fixed with a dilated pupil that exhibited decreased pupillary
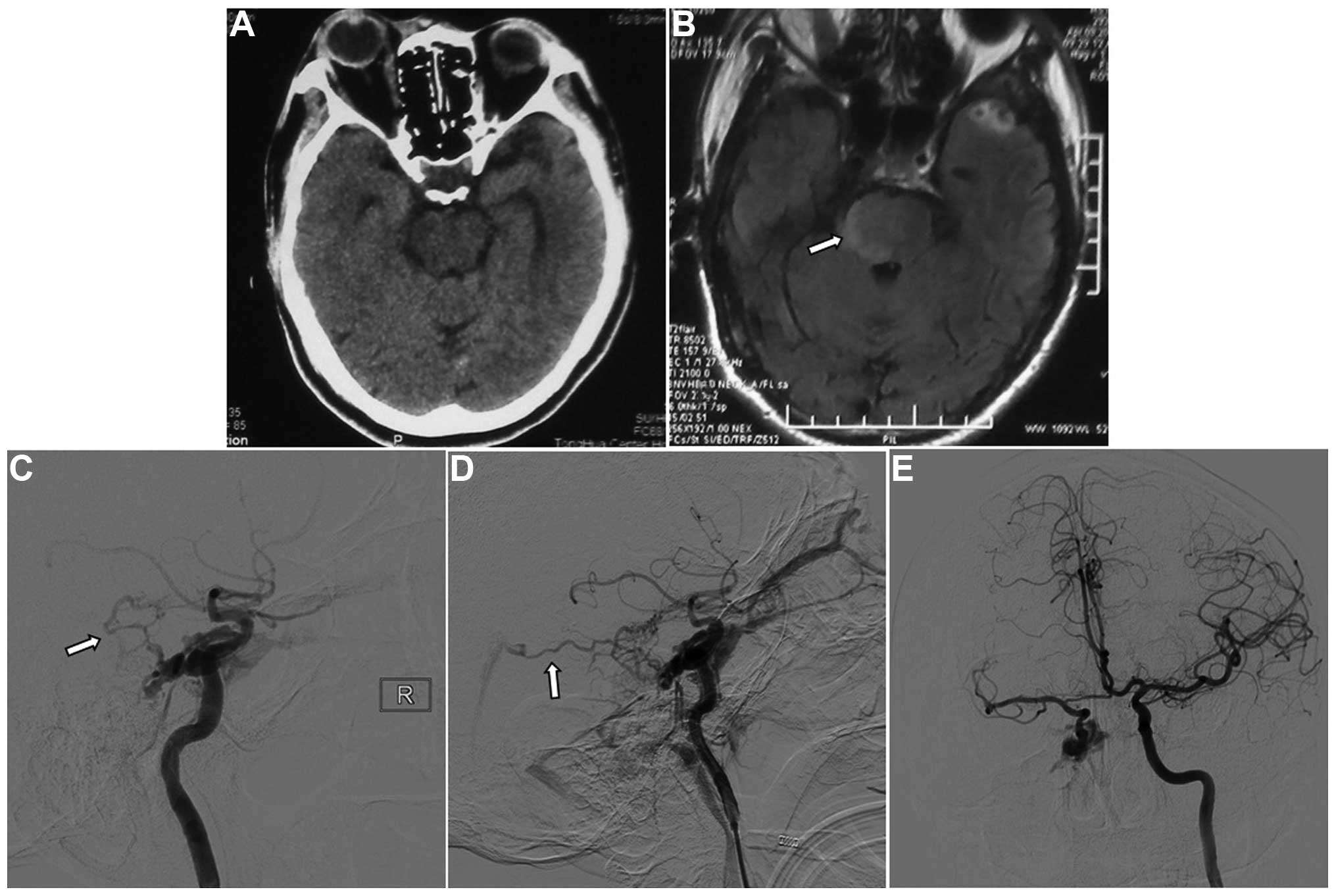
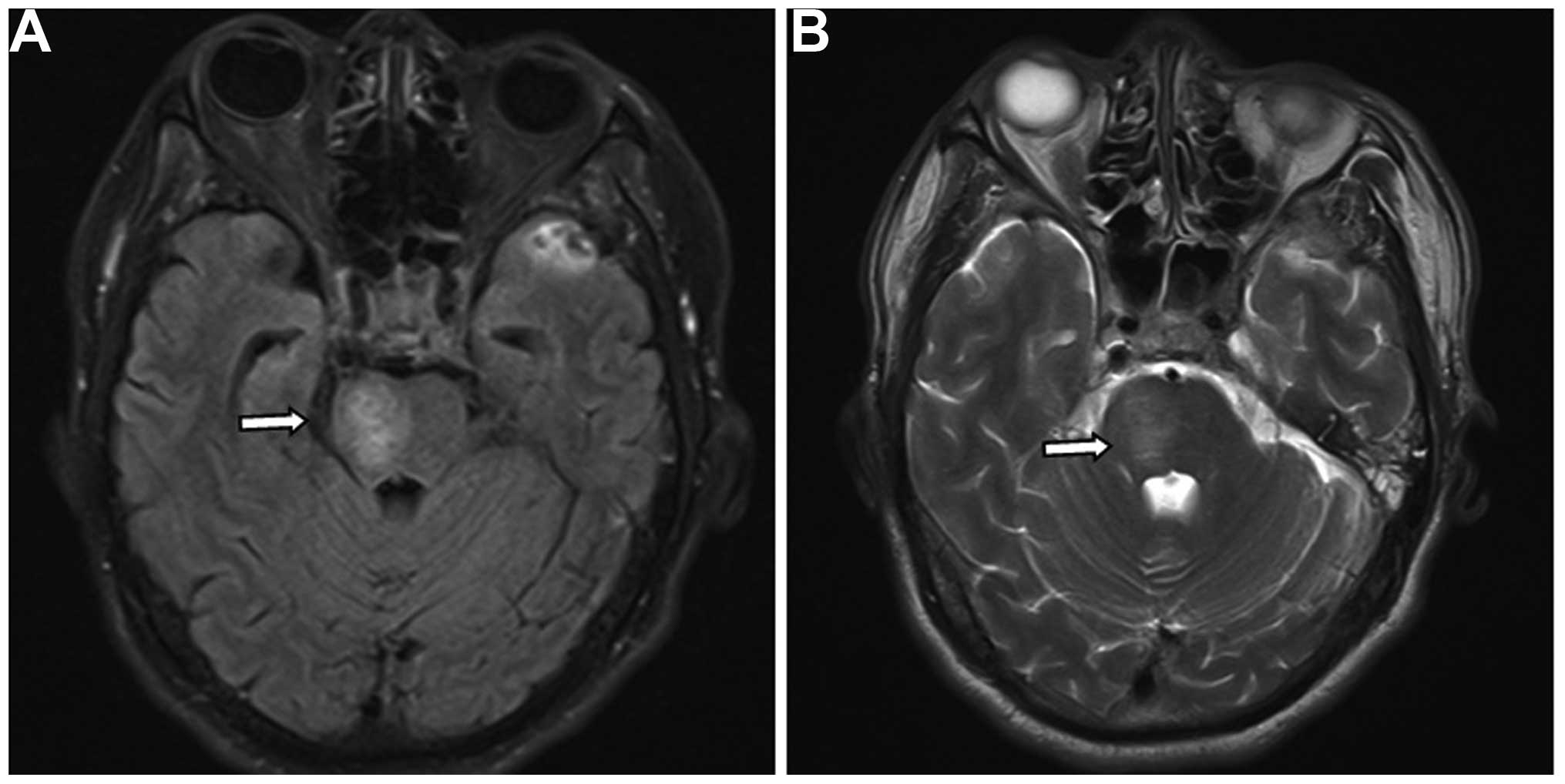
light reflex. The cranial CT scan was normal (Fig. 2A). Fluid-attenuated inversion
recovery magnetic resonance imaging (MRI) showed a hyperintense
signal on the right side of the pons, consistent with brainstem
edema (Fig. 2B). Digital subtraction
angiography (DSA) showed that the cavernous sinus drained into the
ophthalmic vein, inferior petrosal sinus and clival venous plexus.
The enlarged vein in front of the brainstem drained to the straight
sinus via the basal vein of Rosenthal and the vein of Galen. There
was no filling of the superior petrosal sinus. Left carotid artery
angiography was performed with cross compression of the right
carotid artery, demonstrating normal collateral circulation in the
right carotid artery and no contrast delay in the middle cerebral
artery (Fig. 2C-E). The patient was
diagnosed with TCCF.
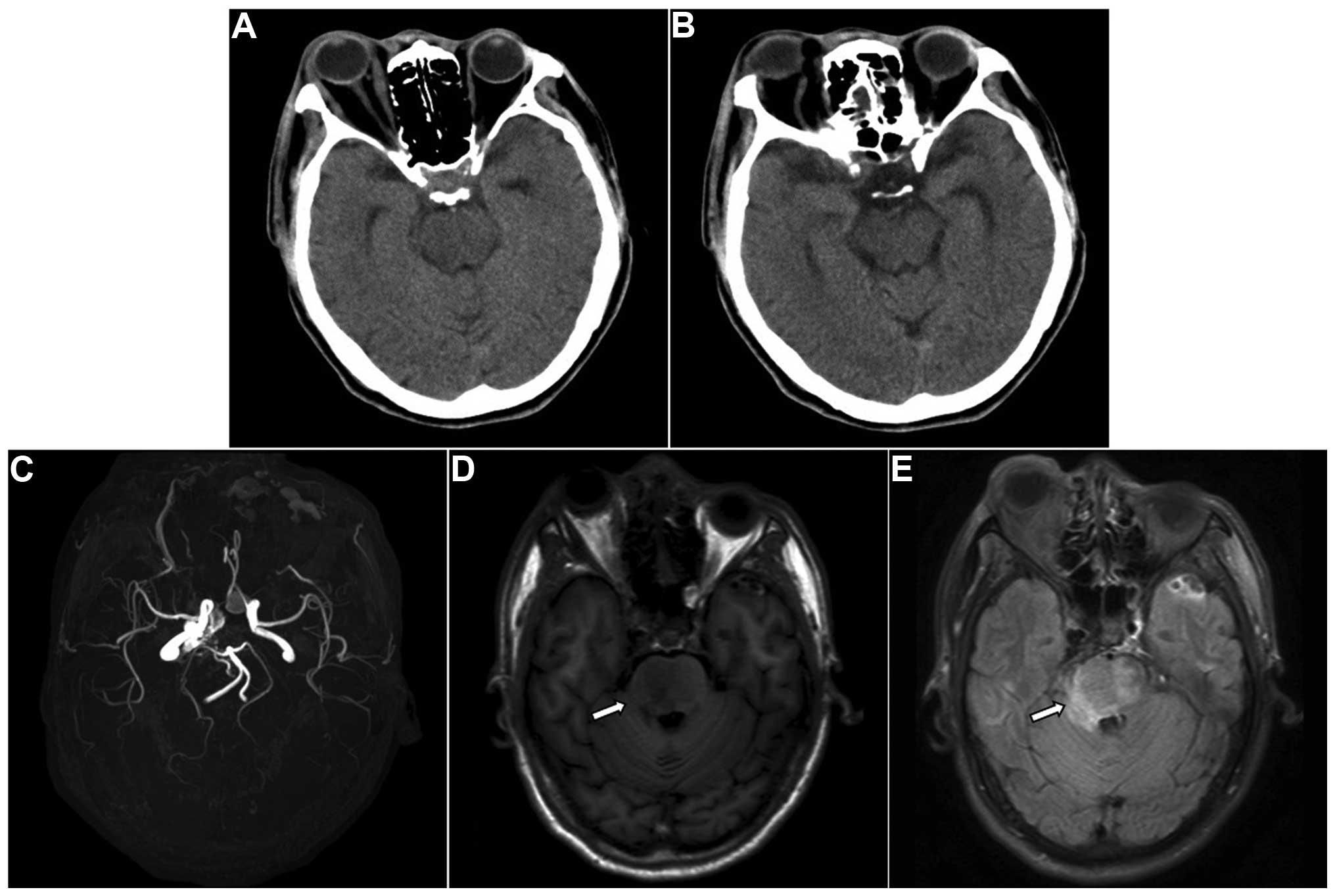
In order to improve the collateral circulation, the
patient was treated with neck compression. Five days after
admission, he developed left hemiparesis and right facial paralysis
with shallow nasolabial folds. The muscle strength of the patient
was 2/5 in the extremities with positive pathological signs, and CT
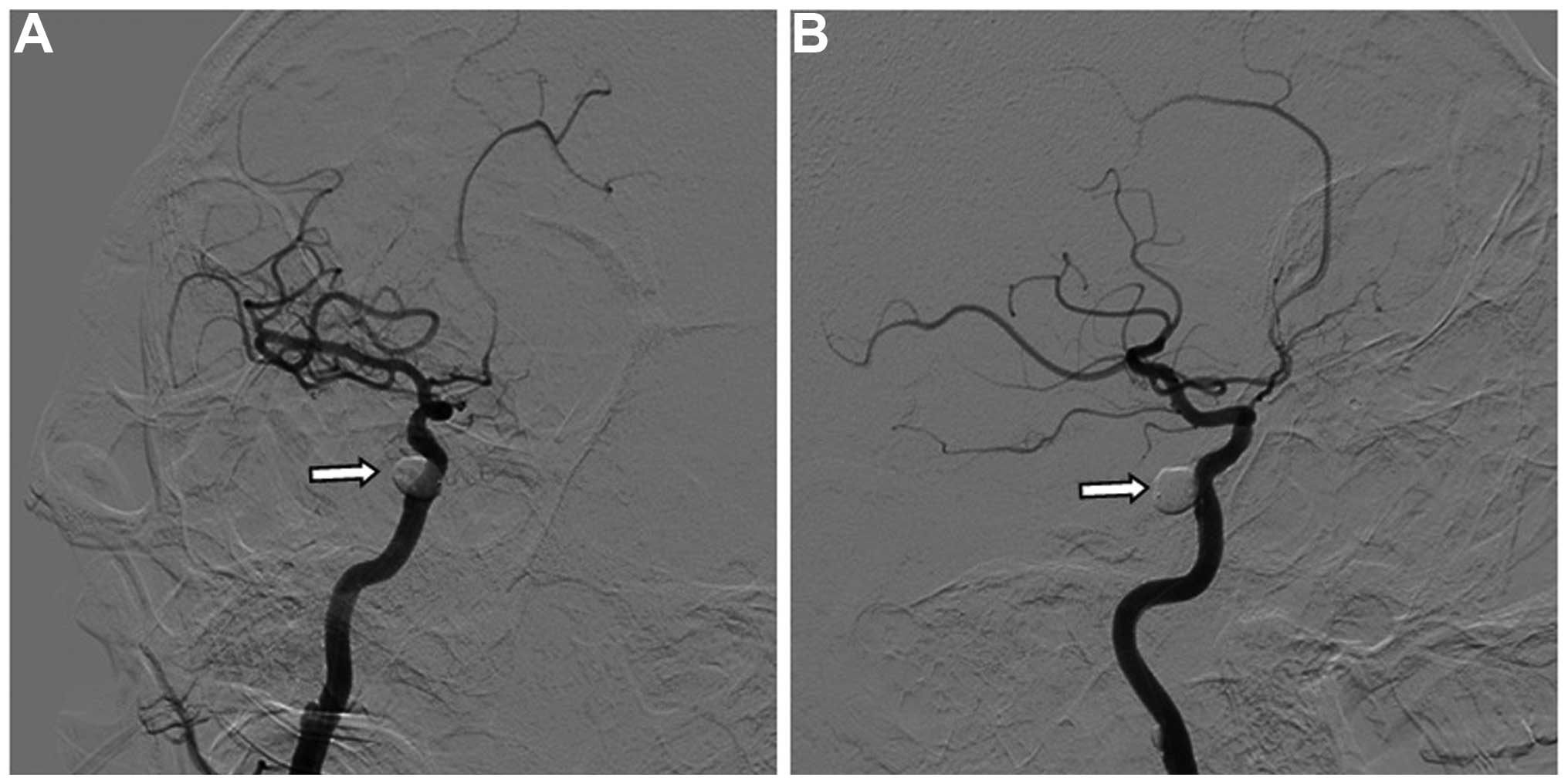
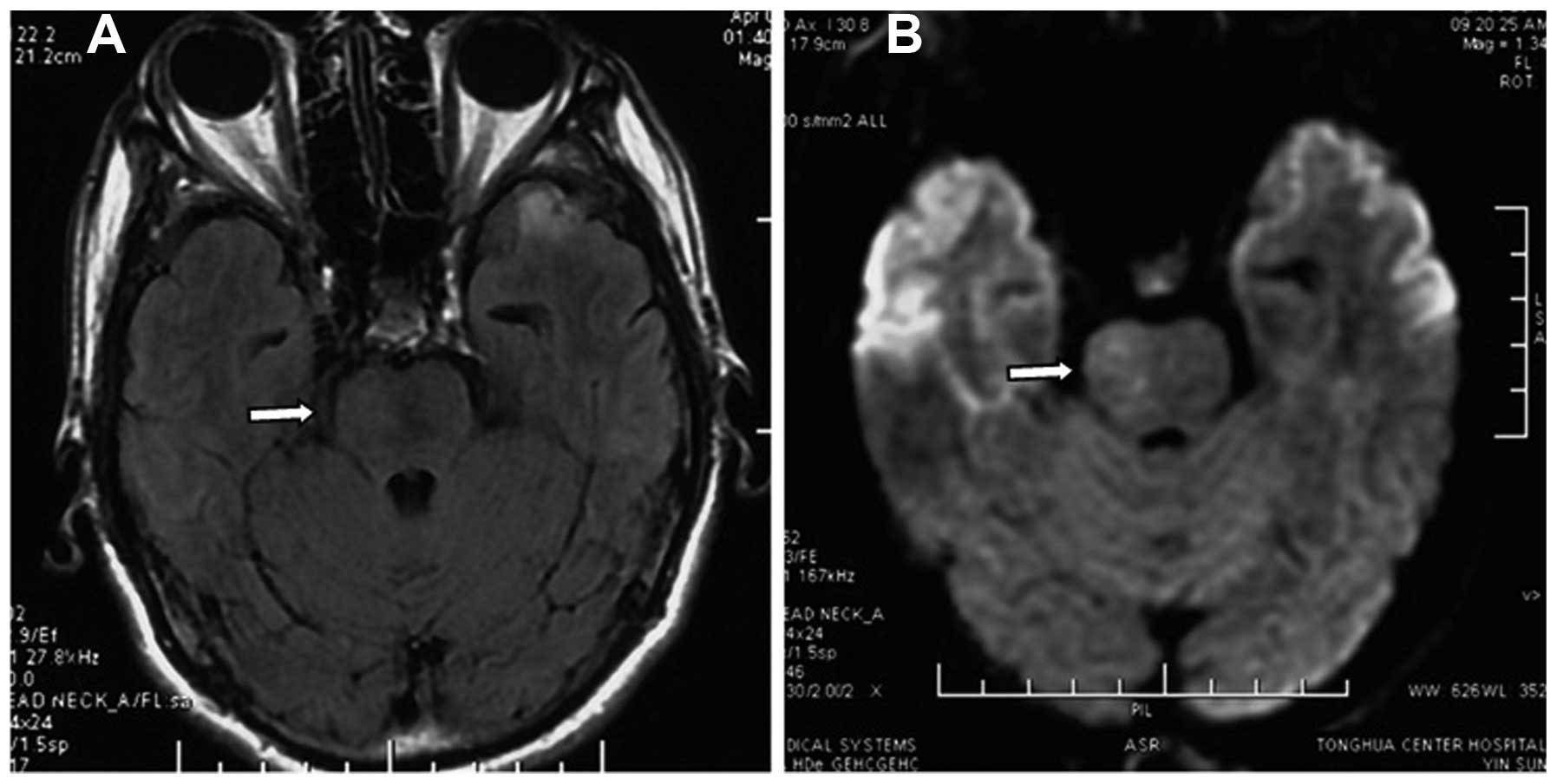
and MRI revealed aggravation of the brainstem edema (Fig. 3). The CCF was successfully embolized
endovascularly with a detachable balloon on emergency. Angiography
showed that the internal carotid artery was patent, and there was
no contrast filling in the cavernous sinus (Fig. 4).
Following embolization, the ophthalmic signs were
relieved, the intracranial bruit disappeared and the left
hemiparesis gradually recovered. MRI performed 1 week
postoperatively showed reduced brainstem edema (Fig. 5). At the 1-month follow-up, all
symptoms, including hemiparesis, had disappeared, and MRI showed an
absence of brainstem edema (Fig. 6).
The patient was found to be normal at the 6-month follow-up
performed via telephone.
Discussion
TCCF is not uncommon clinically, and the symptoms
are mainly dependent on the direction of the cavernous sinus
drainage. The cavernous sinus lies laterally to the pituitary gland
and sphenoid bone and extends from the superior orbital fissure to
the tip of the petrous bone. The cavernous sinus receives blood
from the superior and inferior ophthalmic veins, superficial
cortical vein and sphenoparietal sinus and drains into the superior
and inferior petrosal sinus and pterygoid venous plexus. The C4
segment of the internal carotid artery passes through the cavernous
sinuses, and they communicate with each other via the
intercavernous sinus (8). When a
sphenoid bone fracture punctures the internal carotid artery or a
pseudoaneurysm is ruptured, arterial blood can enter the cavernous
sinus, causing a TCCF. As high-flow and high-pressure arterial
blood enters the cavernous sinus, an intracranial bruit can occur
at the fistula. In addition, the hemodynamic changes in the
cavernous sinus can reverse flow into tributaries. Reflux into the
ophthalmic vein can lead to ophthalmic signs, and reflux into the
ulnar vein can cause enlargement of the vein on the surface of the
brain and cerebral hemorrhage (9).
Due to these anatomic and hemodynamic characteristics of TCCF,
patients with TCCF often exhibit atypical clinical symptoms as a
result of the intracranial hemorrhage, in addition to typical
clinical symptoms such as exophthalmos and intracranial bruit
(10–12); however, the clinical symptoms of TCCF
patients with brainstem edema are rarely reported, and the
mechanisms and prognosis of TCCF with brainstem edema remain
unclear. Here, we review the clinical characteristics of the
present case along with the other six cases available from the
literature (2–6).
TCCF-associated brainstem edema appears as a diffuse
lesion with unclear boundary and exhibits venous congestive
infarction on radiological images. This is similar to that caused
by intracranial sinus thrombosis and venous thrombosis (13). Due to its rarity, elucidation of the
mechanisms underlying brainstem edema caused by TCCF has been
difficult. TCCF is not the only cause of brainstem edema, as
cavernous sinus dural arteriovenous fistula (CSDAVF) has also been
reported to cause brainstem edema (14,15). In
a retrospective study of 54 patients with CSDAVF, Miyamoto et
al (15) reported that the main
manifestation of venous congestive infarction was brainstem edema,
which was primarily caused by insufficient venous collaterals,
venous thrombosis, varicose, basilar venous hypoplasia and
increased venous flow; however, brainstem edema following TCCF is
not completely due to increased venous flow in the brainstem, as
venous congestion, although rare, can occur despite an increase in
venous flow in the superior and inferior petrosal sinus following
the entry of arterial blood into the cavernous sinus (5). Increased blood flow in the periphery of
the brainstem is therefore not the major cause of brainstem edema
following TCCF.
In all six previous cases with brainstem edema
caused by TCCF (Table I), thrombosis
in the superior petrosal sinus occurred. Although thrombosis in the
petrosal vein most commonly occurs in CSDAVF, thrombosis in the
superior petrosal sinus was also found in CSDAVF (15). Consistent with the literature, the
present case exhibited occlusion of the superior petrosal sinus on
DSA. When the superior petrosal sinus is occluded, high-flow
arterial blood mainly drains to the superior and inferior
ophthalmic veins, inferior petrosal sinus and pterygoid plexus,
thereby causing severe ophthalmic signs. The tributaries of the
superior petrosal sinus drain to the brainstem veins; when they are
occluded, the collaterals in the brainstem need to be
re-established via the venous plexus in the periphery of the
brainstem (16). In addition, small
veins that communicate with the cavernous sinus are enlarged and
drain the cavernous sinus. In the present case, the veins in front
of the brainstem were enlarged and drained to the basal vein of
Rosenthal. Ract et al (6)
reported that the edema in the brainstem and basal ganglion was
induced by drainage via the ulnar vein. Furthermore, following
occlusion of the superior petrosal sinus, drainage to the inferior
petrosal sinus increases, thus leading to impaired venous drainage
in the periphery of the brainstem and aggravation of the brainstem
edema. Besides occlusion of the superior petrosal sinus and
enlargement of the veins, hypoplasia of the basal vein of Rosenthal
was observed in cases with CSDAVF and TCCF with brainstem edema
(6,15). In combination, these findings suggest
that poor venous drainage may be a main cause of brainstem edema
with TCCF.
 | Table I.Summary of traumatic carotid-cavernous
fistula with brainstem edema. |
Table I.
Summary of traumatic carotid-cavernous
fistula with brainstem edema.
| Case no. | First author, year
(ref.) | Age in
years/gender | Location | Symptoms | Occlusion of the
superior petrosal sinus | Enlarged vein around
the brainstem | Treatment | Outcome |
|---|
| 1 | Turner, 1983
(2) | 81/F | Midbrain | Hemiparesis,
comatose | N/A | + | Not treated | Mortality |
| 2 | Teng, 1991 (3) | 36/M | Midbrain,
thalamus | Hemiparesis,
comatose | + | + | Transarterial balloon
embolization | Recovered |
| 3 | Teng, 1991 (3) | 26/M | Midbrain | Hemiparesis, facial
paralysis | + | + | Transarterial
balloon | Recovered |
| 4 | Murata, 2003
(4) | 49/F | Pons | Hemiparesis,
dysarthria, somnolence | + | + | Transarterial coil
embolization | Recovered |
| 5 | Bussière, 2009
(5) | 39/M | Pons | Drowsiness, facial
numbness, gait ataxia | + | + | Transarterial balloon
embolization | Recovered |
| 6 | Ract, 2014 (6) | 45/F | Brainstem, medial
side of the temporal lobe and basal ganglion | Hemiparesis,
dysarthria, comatose | + | + | Transarterial coil
embolization | Recovered |
| 7 | Present case | 51/F | Pons | Hemiparesis | + | + | Transarterial balloon
embolization | Recovered |
The cause of superior petrosal sinus occlusion in
TCCF remains unclear. Since spontaneous occlusion of a bilateral
TCCF and spontaneous thrombosis of CCF following failed
transarterial balloon occlusion have been reported (17,18), we
speculate that stasis of venous flow and loss of venous pressure in
TCCF may lead to stasis of blood flow in the superior petrosal
sinus. Similar conditions have been reported in carotid-cavernous
dural arteriovenous fistula (19,20) and
in the ophthalmic vein following TCCF (21); therefore, thrombus formation due to
stasis of the venous flow likely contributes to occlusion of the
superior petrosal sinus in TCCF. Other factors may also contribute
to occlusion of the superior petrosal sinus, however, including
induction of thrombus formation by contrast agents either by
directly acting on endothelial cells or via the accumulation of
white and red blood cells. This may occur as a result of the
accumulation of contrasts in the cavernous sinus, since contrasts
do not induce thrombus formation in normal blood vessels (22,23). In
all six cases available with brainstem edema caused by TCCF,
brainstem edema and its associated symptoms occurred following the
use of contrast materials (2–6). In the
present case, there was mild brainstem edema on MRI during the use
of contrast materials, but the brainstem edema was aggravated
following the use of contrast materials. It is therefore possible
that the use of contrasts may lead to brainstem edema.
Brainstem edema caused by TCCF is associated with
venous congestion, which can be effectively treated with
transarterial coil or balloon embolization (Table I). Since ischemia and infarction do
not occur, the prognosis of TCCF with brainstem edema is similar to
that of brain edema caused by thrombosis of the intracranial venous
sinus (24). Five patients who were
treated with transarterial coil or balloon embolization achieved
satisfactory outcomes. In the present case, the hemiparesis and
brainstem edema disappeared with the transarterial balloon
embolization.
In conclusion, occlusion of the superior petrosal
sinus commonly occurs in TCCF, which can lead to poor venous
drainage in the brainstem. Increased venous pressure in the
superior petrosal sinus and clival venous plexus further blocks the
venous drainage in the brainstem, leading to brainstem edema and
its associated symptoms, such as hemiparesis. Use of contrasts for
angiography may aggravate the brainstem edema. Relief of brainstem
edema and brainstem edema-associated clinical symptoms can be
achieved with transarterial coil or balloon embolization of the
TCCF to reduce the drainage pressure in the brainstem veins.
References
|
1
|
Kato M, Ikegame Y, Toyoda I, Ogura S,
Kitajima H, Yoshimura S and Iwama T: Hemispheric laminar necrosis
as a complication of traumatic carotid-cavernous sinus fistula.
Neurol Med Chir (Tokyo). 49:26–29. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Turner DM, Vangilder JC, Mojtahedi S and
Pierson EW: Spontaneous intracerebral hematoma in carotid-cavernous
fistula. Report of three cases. J Neurosurg. 59:680–686. 1983.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Teng MM, Chang T, Pan DH, Chang CN, Huang
CI, Guo WY, Chen CC, Pang RG and Lee LS: Brainstem edema: An
unusual complication of carotid cavernous fistula. AJNR Am J
Neuroradiol. 12:139–142. 1991.PubMed/NCBI
|
|
4
|
Murata H, Kubota T, Murai M, Kanno H,
Fujii S and Yamamoto I: Brainstem congestion caused by direct
carotid-cavernous fistula - case report. Neurol Med Chir (Tokyo).
43:255–258. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bussière M, Lownie SP, Pelz DM and Nicolle
D: Direct carotid-cavernous fistula causing brainstem venous
congestion. J Neuroophthalmol. 29:21–25. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ract I, Drier A, Leclercq D, Sourour N,
Gabrieli J, Yger M, Nouet A, Dormont D, Chiras J and Clarençon F:
Extensive basal ganglia edema caused by a traumatic
carotid-cavernous fistula: A rare presentation related to a basal
vein of Rosenthal anatomical variation. J Neurosurg. 121:63–66.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de Keizer R: Carotid-cavernous and orbital
arteriovenous fistulas: Ocular features, diagnostic and hemodynamic
considerations in relation to visual impairment and morbidity.
Orbit. 22:121–142. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rhoton AL Jr: The cavernous sinus, the
cavernous venous plexus and the carotid collar. Neurosurgery. 51 (4
Suppl):S375–S410. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fusco MR and Harrigan MR: Cerebrovascular
dissections: A review. Part II: Blunt cerebrovascular injury.
Neurosurgery. 68:517–530. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chang CM and Cheng CS: Late intracranial
haemorrhage and subsequent carotid-cavernous sinus fistula after
fracture of the facial bones. Br J Oral Maxillofac Surg.
51:e296–e298. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Asano T, Houkin K, Moriwaki T, Niiya Y and
Mabuchi S: Case of direct carotid-cavernous fistula presenting with
subarachnoid hemorrhage. No Shinkei Geka. 40:235–239. 2012.(In
Japanese). PubMed/NCBI
|
|
12
|
Ringer AJ, Salud L and Tomsick TA: Carotid
cavernous fistulas: Anatomy, classification and treatment.
Neurosurg Clin N Am. 16:279–295. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kalra VB, Malhotra A and Matouk CC:
Teaching neuroimages: Susceptibility-weighted MRI: First clue to
DAVF complicating sinovenous thrombosis. Neurology. 80:e2282013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Blanc R, Maia Barros AD, Brugieres P,
Meder JF and Gaston A: Cavernous sinus dural arteriovenous fistula
complicated by edematous cerebral lesions from venous etiology. J
Neuroradiol. 31:220–224. 2004.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Miyamoto N, Naito I, Takatama S, Shimizu
T, Iwai T and Shimaguchi H: Clinical and angiographic
characteristics of cavernous sinus dural arteriovenous fistulas
manifesting as venous infarction and/or intracranial hemorrhage.
Neuroradiology. 51:53–60. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Curé JK, Van Tassel P and Smith MT: Normal
and variant anatomy of the dural venous sinuses. Semin Ultrasound
CT MR. 15:499–519. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Churojana A, Chawalaparit O, Chiewwit P
and Suthipongchai S: Spontaneous occlusion of a bilateral post
traumatic carotid cavernous fistula. Interv Neuroradiol. 7:245–252.
2001.PubMed/NCBI
|
|
18
|
Uchino A, Takase Y, Koizumi T and Kudo S:
Spontaneous thrombosis of a high-flow carotid-cavernous fistula
after failed transarterial balloon occlusion. Interv Neuroradiol.
10:253–256. 2004.PubMed/NCBI
|
|
19
|
Sasaki H, Nukui H, Kaneko M, Mitsuka S,
Hosaka T, Kakizawa T, Kimura R, Nagaseki Y and Naganuma H:
Long-term observations in cases with spontaneous carotid-cavernous
fistulas. Acta Neurochir (Wien). 90:117–120. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Komiyama M, Nakajima H, Nishikawa M and
Kan M: Traumatic carotid cavernous sinus fistula: Serial
angiographic studies from the day of trauma. AJNR Am J Neuroradiol.
19:1641–1644. 1998.PubMed/NCBI
|
|
21
|
Iseki S, Ito Y, Nakao Y, Yamamoto T and
Mori K: Proptosis caused by partially thrombosed orbital varix of
the superior orbital vein associated with traumatic
carotid-cavernous sinus fistula - case report. Neurol Med Chir
(Tokyo). 50:33–36. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nishijima M, Iwai R, Horie Y, Oka N and
Takaku A: Spontaneous occlusion of traumatic carotid cavernous
fistula after orbital venography. Surg Neurol. 23:489–492. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Castillo M, Silverstein M, Hoffman JC Jr
and Barrow D: Spontaneous thrombosis of a direct carotid cavernous
sinus fistula: Confirmation by Gd-DTPA-enhanced MR. AJNR Am J
Neuroradiol. 10 (5 Suppl):S75–S76. 1989.PubMed/NCBI
|
|
24
|
Gupta RK, Bapuraj JR, Khandelwal N and
Khurana D: Prognostic indices for cerebral venous thrombosis on CT
perfusion: A prospective study. Eur J Radiol. 83:185–190. 2014.
View Article : Google Scholar : PubMed/NCBI
|