Introduction
In recent years, environmental and lifestyle
changes, as well as the increase in the aging population, have led
to a subsequent increase in the incidence rates of different
cardiovascular and cerebrovascular diseases (1). Chronic heart failure (HF) refers to the
weakening of myocardial contractility, in which the normal cardiac
output cannot be maintained due to chronic primary myocardial
disease, long-term high blood pressure or circulatory overload
(2). Chronic HF can involve the left
side, right side or whole heart (3).
Asymptomatic HF is a common disease and hospitalization cause in
elderly patients (4), which does not
present evident symptoms, but is the end-stage of various types of
heart disease. In HF, various body functions of the patients are
significantly impaired and the immune function decreases. Adverse
cardiac events frequently occur in patients with HF, and may result
in mortality. The survival rate of HF is low and the prognosis is
poor (5). Therefore, the development
of more effective medication is essential in order to improve the
function of various organs and the prognosis of patients.
Diuretics are an important, indispensable part of
the standard treatment for HF. These drugs can improve the clinical
symptoms of patients with HF, when combined with
angiotensin-converting enzyme inhibitors, angiotensin receptor
blockers and other drugs (6,7). However, diuretics may lead to various
adverse reactions, affecting the therapeutic efficiency of the
treatment. In addition, certain patients may refuse the use of
diuretics during the treatment. In such cases, the recurrence rate
of HF is high, with an increased number of re-hospitalized
patients, while the treatment efficiency can be reduced and a
longer course of treatment is required (8). Previous studies have shown that regular
long-term use of low-dose diuretics can improve the cardiac
function of patients. For instance, in the study by Cocco and Jerie
(9), the left ventricular ejection
fraction (LVEF) of patients increased following treatment with
diuretics, while the side effects and complications decreased.
Cystatin C (CysC) is a type of cysteine protease inhibitor. When
the renal function declines, CysC levels increase much earlier than
the levels of urea and creatinine. Therefore, the level of CysC can
be used in the evaluation and early prediction of changes in the
renal function (10,11). A decrease in the heart function of
patients has been shown to be accompanied by abnormal kidney
function (12). Therefore, improving
the cardiac function, renal function and prognosis of patients with
HF is crucial. Only a limited number of studies have reported the
effects of diuretics on the level of serum CysC and the prognosis
of patients with HF (13).
The aim of the present study was to analyze changes
in the LVEF and the levels of serum creatinine (Scr) and serum CysC
after long-term use of low-dose diuretics in patients with
asymptomatic chronic HF. In addition, the study investigated the
effects of long-term regular use of low-dose diuretics on the
prognosis, cardiac function classification, occurrence of adverse
reactions and complications in patients with asymptomatic chronic
HF.
Subjects and methods
Subjects
A total of 66 patients with asymptomatic chronic HF
who were admitted to the Henan University Huaihe Hospital (Kaifeng,
China) between January 2012 and January 2014 were enrolled in the
present study. The patients were randomly divided into the
observation (17 men and 16 women; age range, 45–78 years; mean age,
63.52±8.47 years) and control group (18 men and 15 women; age
range, 42–76 years; mean age, 63.15±8.82 years), with 33 patients
in each group. The study included patients who met the diagnostic
criteria for HF (14) and provided
informed consent. Patients with liver and/or kidney dysfunction,
pregnant or lactating patients, and patients complicated by other
severe cardiovascular diseases, cerebrovascular diseases or other
causes of severe arrhythmia were excluded from the study. The heart
function of patients was classified according to the New York Heart
Association (NYHA) functional classification (15). This study was conducted in accordance
with the declaration of Helsinki and with approval from the Ethics
Committee of Henan University Huaihe Hospital. Written informed
consent was obtained from all participants.
Treatment method
The patients were treated with
angiotensin-converting enzyme inhibitors (25 mg Captopril; Wanchang
Pharmaceutical Co., Ltd., Xi'an, China), β blockers (25 mg
Porpranolol; Baiyunshan Pharmaceutical Co. Ltd., Guangzhou, China)
and Digitalis (0.5 mg Lanatoside; Fuxing Pharmaceutical Co.,
Ltd., Shanghai, China) in the control group, which is routine
treatment for HF patients. Patients in the observation group were
treated with the same treatment as the control group, in addition
to 5–15 mg/day of the diuretic hydrochlorothiazide (Shanxi Yunpeng
Pharmaceutical Co., Ltd, Linfen, China; approval no. H14020796) for
long-term treatment, along with the same routine treatment as the
control group.
Detection method
In order to evaluate the effect of the diuretic
treatment in HF patients, the LVEF, levels of Scr and serum CysC
and NYHA cardiac functional classification were determined, while
any adverse reactions and complications prior to and following the
diuretic treatment were recorded in the two groups. The LVEF, serum
CysC levels and Scr levels were detected in the patient serum at 1
day before the treatment, and at 1 week, 1 month, 3 months and 6
months after the treatment. A total of 5 ml fasting blood was
extracted from all participants, centrifuged at 4,000 × g at 4°C
for 10 min and stored at a constant temperature of −20°C. Next, the
level of serum CysC was detected using the latex enhanced
turbidimetric method (16), while
the level of Scr was detected using an enzymatic method (17). Scr detection kits were provided by
Nanjing Sen Beijia Biological Technology Co., Ltd. (Nanjing,
China). An ELx800 optical absorbance microplate reader (BioTek
Instruments, Inc., Winooski, VT, USA) was used to measure the
absorbance values at 570 nm. LVEF was detected using the HP Sonos
2000 ultrasonic diagnostic apparatus (Hewlett-Packard, Palo Alto,
CA, USA) and the ultrasonic probe frequency was 3.5–7 MHz. All
procedures were performed in strict accordance with the
manufacturer's instructions.
Evaluation method
NYHA functional classification (15) was determined according to the
activity degree of symptoms of induced by HF. The degree of cardiac
function damage is divided into the following four classes: Class
I, in which the patient suffers from heart disease, but daily
physical activity is not limited and does not cause excessive
fatigue, palpitations, shortness of breath or angina pectoris;
class II, in which the physical activity of patients with heart
disease is mildly restricted, with no symptoms at rest, while
general physical activity can cause excessive fatigue,
palpitations, shortness of breath or angina pectoris; class III, in
which heart disease causes significant restriction in physical
activity, with no symptoms at rest, while less than ordinary
physical activity can result in excessive fatigue, palpitations,
shortness of breath or angina pectoris; and class IV, in which the
patients with heart disease are unable to engage in any physical
activity, while the symptoms of HF appear at rest and discomfort is
aggravated subsequent to any physical activity.
Statistical analysis
All data were analyzed using SPSS version 17.0
software (SPSS Inc., Chicago, IL, USA). Quantitative data were
compared using the t test, while enumeration data were compared
with the χ2 test. P<0.05 was considered to indicate a
statistically significant difference.
Results
NYHA classification of patients
In the observation group, there were 2 cases with
NYHA class II, 23 cases with class III and 8 cases with class IV.
In the control group, there were 3 cases with NYHA class II, 23
cases with class III and 7 cases with class IV. No statistically
significant differences in the gender, age, NYHA cardiac functional
classification were observed between the two groups
(P>0.05).
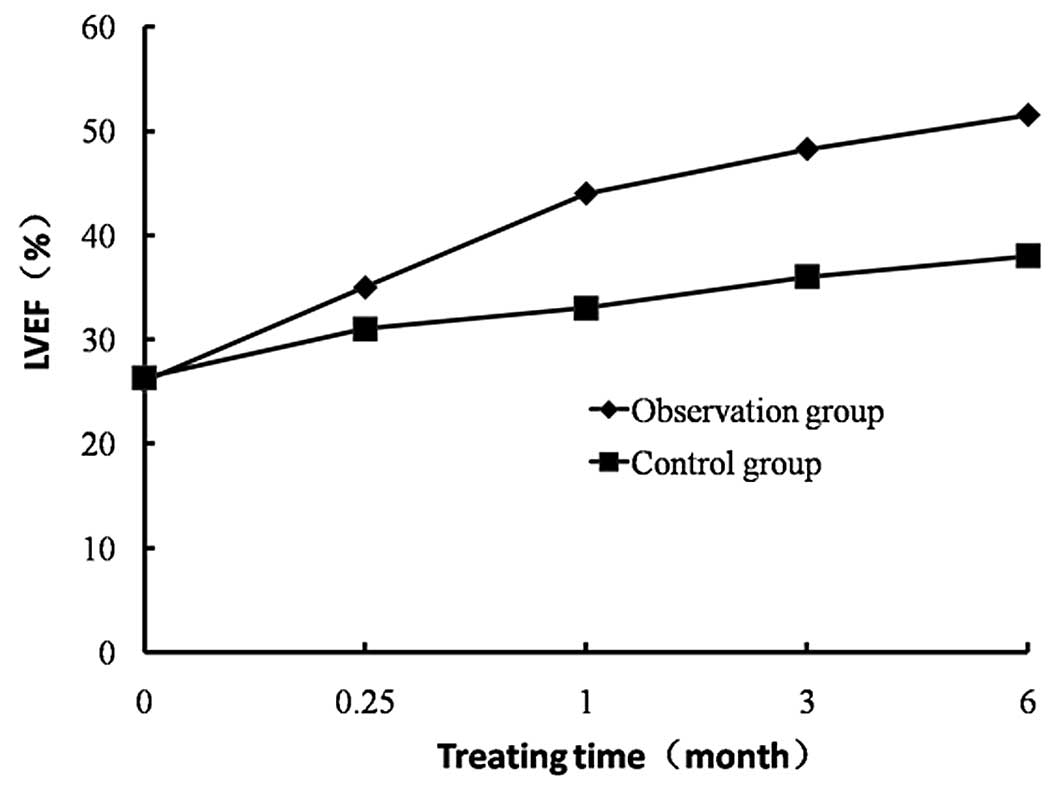
Comparison of LVEF, serum CysC levels
and Scr levels prior to and following treatment in the two
groups
LVEF, serum CysC levels and Scr levels prior to
diuretic treatment were compared between the two groups, and no
statistically significant difference was observed (P>0.05;
Table I). In the observation group,
LVEF after treatment for 1 week, 1 month, 3 months and 6 months
increased compared with the values prior to treatment. In addition,
the levels of serum CysC and Src in the observation group were
found to be decreased at these time points compared with the levels
prior to diuretic treatment. In the control group, LVEF increased
after treatment for 1, 3 and 6 months compared with the value prior
to treatment, whereas the levels of serum CysC and Scr decreased at
these time points compared to the levels prior to treatment.
Furthermore, LVEF values in the observation group after treatment
for 1, 3 and 6 months was higher compared with those in the control
group (P<0.05). The levels of serum CysC and Scr in the
observation group were lower at the aforementioned time points
compared with the levels in the control group, and the difference
was statistically significant (P<0.05; Table I; Figs.
1–3).
 | Table I.Comparison of LVEF, Scr levels and
serum CysC levels prior to and following diuretic treatment in the
two groups. |
Table I.
Comparison of LVEF, Scr levels and
serum CysC levels prior to and following diuretic treatment in the
two groups.
| Levels at each time
point | Observation
group | Control group | t test | P-value |
|---|
| Prior to
treatment |
|
|
|
|
| LVEF,
% | 25.45±4.92 | 26.02±4.22 | 0.25 | >0.05 |
| CysC,
mg/l | 6.42±2.14 | 6.39±2.66 | 0.18 | >0.05 |
| Scr,
µmol/l | 265.41±53.22 | 259.25±51.98 | 1.43 | >0.05 |
| After treatment for 1
week |
|
|
|
|
| LVEF,
% |
35.22±3.64a | 31.45±3.65 | 1.82 | >0.05 |
| CysC,
mg/l |
4.87±1.05a | 5.49±1.24 | 2.26 | >0.05 |
| Scr,
µmol/l |
185.69±46.88a | 192.84±48.72 | 2.17 | >0.05 |
| After treatment for 1
month |
|
|
|
|
| LVEF,
% |
43.55±4.26a |
33.68±4.75b | 2.62 | <0.05 |
| CysC,
mg/l |
3.26±0.59a |
4.18±0.88b | 3.54 | <0.05 |
| Scr,
µmol/l |
125.78±32.55a |
146.25±36.74b | 3.89 | <0.05 |
| After treatment for 3
months |
|
|
|
|
| LVEF,
% |
48.25±4.88a |
36.47±4.69b | 3.45 | <0.05 |
| CysC,
mg/l |
2.24±0.48a |
3.96±0.72b | 4.16 | <0.05 |
| Scr,
µmol/l |
98.41±21.59a |
123.55±23.72b | 4.87 | <0.05 |
| After treatment for 6
months |
|
|
|
|
| LVEF,
% |
50.86±5.22a |
38.22±5.12b | 4.28 | <0.05 |
| CysC,
mg/l |
1.65±0.26a |
2.84±0.53b | 5.27 | <0.05 |
| Scr,
µmol/l |
78.52±13.78a |
106.65±17.43b | 5.93 | <0.05 |
Comparison of NYHA class prior to and
following diuretic treatment in the two groups
The number of patients in each NYHA class prior to
treatment was not significantly different between the two groups
(P>0.05; Table IIA). The number
of patients with class I and II heart function in the two groups
increased following treatment, while the number of patients with
class III and IV cardiac function decreased. In the observation
group, the number of patients with cardiac function of class I and
II increased following treatment, whereas the number of patients
with cardiac function of class III and IV decreased following
treatment, when compared with that in the control group, and the
differences were statistically significant (P<0.05; Table IIB).
 | Table II.Comparison of NYHA cardiac function
classification prior to and following treatment in the two groups
(n, %). |
Table II.
Comparison of NYHA cardiac function
classification prior to and following treatment in the two groups
(n, %).
| A, Prior to
treatment |
|
|
|
|
|---|
|
|---|
| Parameter | Observation
group | Control group | χ2
test | P-value |
|---|
| Number of patients,
n | 33 | 33 | – | – |
| NYHA
classification, n (%) |
|
|
|
|
| Class
I | 0 (0.00) | 0 (0.00) | – | – |
| Class
II | 2 (6.06) | 3 (9.09) | 3.24 | >0.05 |
| Class
III | 23 (69.69) | 23 (69.69) | – | – |
| Class
IV | 8
(24.24) | 7
(21.21) | 1.42 | >0.05 |
|
| B, After treatment
for 6 months |
|
|
|
|
|
| Parameter | Observation
group | Control group | χ2
test | P-value |
|
| Number of patients,
n | 32 | 31 | – | – |
| NYHA
classification, n (%) |
|
|
|
|
| Class
I | 3
(9.38)a | 1
(3.23)b | 6.62 | <0.05 |
| Class
II | 9
(28.13)a | 4
(12.90)b | 7.84 | <0.01 |
| Class
III | 18
(56.25)a | 22
(70.97)b | 4.66 | <0.05 |
| Class
IV | 2
(6.25)a | 4
(12.90)b | 5.97 | <0.05 |
Comparison of prognosis in the two
groups
In the observation group, the number of patients
with improved prognosis increased after treatment for 6 months
compared with the control group (Table
III). In addition, the number of HF patients with deteriorated
prognosis, mortality or incidence of adverse prognosis were
significantly lower in the observation group, compared with those
in the control group following treatment for 6 months (P<0.05;
Table III). Thus, the results
indicated that treatment with low-dose diuretics improved the
prognosis of patients with HF.
 | Table III.Comparison of prognosis after
treatment for 6 months in the two groups (n=33 each group). |
Table III.
Comparison of prognosis after
treatment for 6 months in the two groups (n=33 each group).
| Prognosis | Observation
group | Control group | χ2
test | P-value |
|---|
| Improvement, n
(%) | 26 (78.79) | 20 (60.61) | 4.82 | <0.05 |
| Deterioration, n
(%) | 6
(18.18) | 11 (33.33) | 6.48 | <0.05 |
| Mortality, n
(%) | 1 (3.03) | 2 (6.06) | 6.25 | <0.05 |
| Incidence of
adverse prognosis, % | 21.21 | 39.39 | 4.82 | <0.05 |
Comparison of adverse reactions and
complications
The incidence of headaches, dizziness, anemia,
allergies, difficulty in breathing, hearing loss, and other adverse
reactions and complications was compared between the two groups,
with no statistically significant differences observed (P>0.05;
Table IV).
 | Table IV.Comparison of adverse reactions and
complications in the two groups (n=33 each group). |
Table IV.
Comparison of adverse reactions and
complications in the two groups (n=33 each group).
| Parameter | Observation
group | Control group |
|---|
| Headache and
dizziness, n | 1 | 1 |
| Anemia, n | 1 | 1 |
| Allergies, n | 2 | 1 |
| Difficulty in
breathing, n | 0 | 1 |
| Hearing loss,
n | 1 | 0 |
| Incidences of
adverse reactions | 15.15 | 12.12 |
| and complications,
%a |
|
|
Discussion
HF is frequently associated with asymptomatic left
ventricular dysfunction (18).
Patients normally present left ventricular systolic dysfunction
without evident symptoms of congestive HF. Asymptomatic HF often
occurs in the elderly population, severely affecting the patient's
health and quality of life, and may be life-threatening (19,20). The
incidence of HF in patients with cerebral vascular disease is high,
while cardiovascular and cerebral amplification effects may result
in alterations in the cardiac function of patients. In the early
stages of the disease, the patients often present no evident
symptoms. With time, the disease may develop or worsen into
dominant HF, which may lead to the occurrence of an adverse
prognosis (21,22); therefore, it is important to detect,
prevent and timely treat chronic HF at an early stage.
Diuretics are commonly administered for the
treatment of HF, since they can reduce the occurrence of sodium and
water retention through inhibition of tubular reabsorption of
sodium and chloride, thereby reducing the cardiac load in order to
improve heart function (23).
Asymptomatic chronic HF often develops into HF with evident
symptoms, having severe and even life-threatening effects on the
health of patients and resulting in the incidence of adverse
prognosis. Therefore, the timely and effective treatment of HF
patients is crucial. Serum CysC levels are altered with changes in
renal function, and thus can be used as an index for the early
detection of such changes (24).
There are few studies reporting the effect of low-dose diuretics on
renal function and prognosis (13,25).
Determination of the effect of long-term regular use of low-dose
diuretics on cardiac function, renal function and prognosis of
patients with asymptomatic HF may provide a strong clinical basis
for the improvement of prevention and prognosis, avoiding organ
damage.
The results of the present study showed that the
LVEF and heart function of patients with asymptomatic HF were
significantly reduced compared with normal levels, which was
consistent with the results of Parry et al (26). In addition, the levels of Scr, CysC
and other markers of renal function in patients with asymptomatic
chronic HF were significantly increased compared with normal levels
in the present study, suggesting that the renal function was
evidently damaged. Asymptomatic HF involves multiple systemic
organs prior to the appearance of evident symptoms, and thus its
early diagnosis and treatment are crucial. The mechanism of
abnormal cardiac and renal function in patients with asymptomatic
HF may be explained as follows: HF leads to long-term overload
compensatory work, which may cause significant cardiac damage,
reduce the heart function of patients and result in the reduction
of LVEF. Abnormalities in the heart function frequently lead to the
alteration of hemodynamics, affecting renal blood circulation,
which can result in the decline of renal function and the increase
of Scr and CysC levels (27). In the
present study, following treatment with long-term regular low-dose
diuretics, the LVEF of the patients with asymptomatic HF increased
consistently, while the levels of Scr and CysC continuously
declined throughout the treatment. The improvement in the heart and
renal function of the patients indicated that long-term regular
low-dose diuretic-based treatment was beneficial, improving the
organ function in patients with chronic HF.
The underlying mechanism through which long-term
regular use of low-dose diuretics elevate LVEF and decrease the
levels of Scr and serum CysC may be as follows: A low dose of
diuretics can have a long-term positive effect on the kidneys,
inhibit the overactivation of the rennin-angiotensin-aldosterone
system in patients with asymptomatic HF, and alleviate the symptoms
of HF. Furthermore, low-dose diuretic treatment effectively
inhibits the reabsorption of sodium and chloride in the glomerulus
in order to decrease their levels in the body, while it also
reduces the occurrence of sodium and water retention, reduces the
cardiac preload in order to improve heart function, and improves
the LVEF. The improvement of cardiac function can also reduce, to a
certain extent, the effects of HF on hemodynamics, improving the
renal circulation and function, and reducing the levels of Scr,
CysC and other associated indexes of renal function (28). Following treatment with long-term
low-dose diuretics, a higher number of patients with asymptomatic
HF exhibited improved HF-related symptoms compared with the control
patients, while the number of patients with worsened disease or
mortality due to renal failure reduced. In addition, the heart
function classification of patients increased and the prognosis was
evidently improved, following diuretic treatment. Furthermore, the
incidence of adverse reactions and complications (including
headache, dizziness, anemia, allergies, breathing difficulties and
hearing loss) did not increase in patients treated with diuretics,
compared with the control patients. Due to the short observation
time in the present study, the interval between heart and renal
function detection was longer, while a large number of factors
affected the heart function, renal function and prognosis.
Therefore, the effect of low-dose diuretics on patients with
asymptomatic chronic HF should be investigated further in an
in-depth study with longer observation time.
In conclusion, long-term low-dose diuretic treatment
effectively improved the heart function, renal function and
prognosis in patients with asymptomatic chronic HF. Furthermore,
this treatment did not increase the occurrence of adverse reactions
and complications. Thus, administration of low-dose diuretics is an
effective treatment for asymptomatic chronic HF.
References
|
1
|
Orth-Gomér K: Psychosocial and behavioral
aspects of cardiovascular disease prevention in men and women. Curr
Opin Psychiatry. 20:147–151. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Berezin AE, Kremzer AA, Samura TA and
Martovitskaya YV: Circulating endothelial-derived apoptotic
microparticles in the patients with ischemic symptomatic chronic
heart failure: Relevance of pro-inflammatory activation and
outcomes. Int Cardiovasc Res J. 8:116–123. 2014.PubMed/NCBI
|
|
3
|
Maughan D and Toth M: Discerning primary
and secondary factors responsible for clinical fatigue in
multisystem diseases. Biology (Basel). 3:606–622. 2014.PubMed/NCBI
|
|
4
|
Lang NN, Wong CM, Dalzell JR, Jansz S,
Leslie SJ and Gardner RS: The ease of use and reproducibility of
the Alere™ Heart Check System: A comparison of patient and
healthcare professional measurement of BNP. Biomark Med. 8:791–796.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Armstrong C: ACCF and AHA release
guidelines on the management of heart failure. Am Fam Physician.
90:186–189. 2014.PubMed/NCBI
|
|
6
|
Nativi-Nicolau J, Ryan JJ and Fang JC:
Current therapeutic approach in heart failure with preserved
ejection fraction. Heart Fail Clin. 10:525–538. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Imamura T, Kinugawa K, Ohtani T, Sakata Y,
Higo T, Kinugawa S, Tsutsui H, Sunagawa K and Komuro I: Assessment
of quality of life during long-term treatment of tolvaptan in
refractory heart failure: Design and rationale of the AQUA-TLV
study. Int Heart J. 55:264–267. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rad EM and Assadi F: Management of
hypertension in children with cardiovascular disease and heart
failure. Int J Prev Med. 5(Suppl 1): S10–S16. 2014.PubMed/NCBI
|
|
9
|
Cocco G and Jerie P: Comparison between
ivabradine and low-dose digoxin in the therapy of diastolic heart
failure with preserved left ventricular systolic function. Clin
Pract. 3:e292013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pitt B, Pfeffer MA, Assmann SF, Boineau R,
Anand IS, Claggett B, Clausell N, Desai AS, Diaz R, Fleg JL, et al:
Spironolactone for heart failure with preserved ejection fraction.
N Engl J Med. 370:1383–1392. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
De Vecchis R, Esposito C and Ariano C:
Efficacy and safety assessment of isolated ultrafiltration compared
to intravenous diuretics for acutely decompensated heart failure: A
systematic review with meta-analysis. Minerva Cardioangiol.
62:131–146. 2014.PubMed/NCBI
|
|
12
|
Mpe MT, Klug EQ, Silwa KS, Hitzeroth J and
Smith DA: Heart failure society of South Africa (HeFSSA)
perspective on the European society of cardiology (ESC) 2012
chronic heart failure guideline. S Afr Med J. 103(9 Suppl 2):
660–667. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Verbrugge FH, Nijst P, Dupont M, Reynders
C, Penders J, Tang WH and Mullens W: Prognostic value of glomerular
filtration changes versus natriuretic response in decompensated
heart failure with reduced ejection. J Card Fail. 20:817–824. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Seronde MF, Laribi S, Collins SP, Deye N,
Logeart D, Plaisance P, Cohen-Solal A and Mebazaa A: Heart failure
diagnosis in acute conditions has high agreement with inpatient
diagnosis. Eur J Emerg Med. Feb 23–2015.(Epub ahead of print).
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Miller-Davis C, Marden S and Leidy NK: The
New York Heart Association Classes and functional status: What are
we really measuring? Heart Lung. 35:217–224. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Uemura O, Ushijima K, Nagai T, Yamada T,
Hayakawa H, Nabeta Y, Shinkai Y, Koike K and Kuwabara M: Reference
serum cystatin C levels in Japanese children. Clin Exp Nephrol.
14:453–456. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang X, Xu G, Li H, Liu Y and Wang F:
Reference intervals for serum creatinine with enzymatic assay and
evaluation of four equations to estimate glomerular filtration rate
in a healthy Chinese adult population. Clin Chim Acta.
412:1793–1797. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Moukarbel GV and Solomon SD: Treatment of
asymptomatic left ventricular dysfuntion. Curr Treat Options
Cardiovasc Med. 10:476–485. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rami K: Aggressive salt and water
restriction in acutely decompensated heart failure: is it worth its
weight in salt? Expert Rev Cardiovasc Ther. 11:1125–1128. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lee KK, Shilane D, Hlatky MA, Yang J,
Steimle AE and Go AS: Effectiveness and safety of spironolactone
for systolic heart failure. Am J Cardiol. 112:1427–1432. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hasenfuß G, Edelmann F and Wachter R:
Recommendations for the treatment of heart failure: What's new?
Internist (Berl). 54:1141–1151. 2013.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ferreira JP, Santos M, Almeida S, Marques
I, Bettencourt P and Carvalho H: Tailoring diuretic therapy in
acute heart failure: Insight into early diuretic response
predictors. Clin Res Cardiol. 102:745–753. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Vaduganathan M, Marti CN, Georgiopoulou
VV, Kalogeropoulos AP and Butler J: Classification of patients
hospitalized for heart failure. Heart Fail Clin. 9:277–283. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Frankenstein L, Katus HA, Grundtvig M,
Hole T, de Blois J, Schellberg D, Atar D, Zugck C and Agewall S:
Norwegian Heart Failure Registry steering committee: Association
between spironolactone added to beta-blockers and ACE inhibition
and survival in heart failure patients with reduced ejection
fraction: A propensity score-matched cohort study. Eur J Clin
Pharmacol. 69:1747–1755. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ng TM, Hshieh S, Chan CY and Elkayam U:
Clinical experience with low-dose continuous infusion of furosemide
in acute heart failure: Assessment of efficacy and safety. J
Cardiovasc Pharmacol Ther. 17:373–381. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Parry HM, Doney AS, Palmer CN and Lang CC:
State of play of pharmacogenetics and personalized medicine in
heart failure. Cardiovasc Ther. 31:315–322. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
O'Dell KM, Kalus JS, Kucukarslan S and
Czerska B: Nesiritide for secondary pulmonary hypertension in
patients with end-stage heart failure. Am J Health Syst Pharm.
62:606–609. 2005.PubMed/NCBI
|
|
28
|
Chen HH, Martin FL, Gibbons RJ, Schirger
JA, Wright RS, Schears RM, Redfield MM, Simari RD, Lerman A,
Cataliotti A and Burnett JC Jr: Low-dose nesiritide in human
anterior myocardial infarction suppresses aldosterone and preserves
ventricular function and structure: A proof of concept study.
Heart. 95:1315–1319. 2009. View Article : Google Scholar : PubMed/NCBI
|