Introduction
Infantile spasms are an age-specific epileptic
encephalopathy occurring in early infancy that are characterized by
epileptic spasms with neurodevelopmental regression and
electroencephalographic (EEG) features of hypsarrhythmia (1,2). The
incidence of infantile spasms is ~0.31 per 1,000 live births
(3,4). The average age of onset of infantile
spasms is 6 months (with a peak age of onset of 3–7 months), and
the prevalence is slightly higher in males (5,6).
Pathophysiological mechanisms underlying infantile
spasms remain elusive; two-thirds of patients have brain insults,
and >200 different etiologies have been found to be involved in
the pathogenesis of infantile spasms (7). Neonatal hypoglycemia is the most common
metabolic disorder during the neonatal period and is a recognized
trigger of infantile spasms (8–10).
Previous studies have found that neonatal hypoglycemia may result
in hypoglycemic neurological injuries, also known as neonatal
hypoglycemic brain injuries (11–16).
Udani et al examined the etiology of remote symptomatic
epilepsy with onset during the first 3 years of life and observed
that neonatal hypoglycemia was the most common etiology, with
spasms being the most common type of seizure (14).
Although hypoglycemic brain injury induces infantile
spasms, few cases of patients with neonatal hypoglycemia who
subsequently developed infantile spasms have been reported
(9,10). The present study describes the
clinical findings for 18 infants with neonatal-onset hypoglycemia
who later presented with infantile spasms, which suggest that
neonatal hypoglycemia is potentially associated with the subsequent
occurrence and development of infantile spasms during infancy.
Materials and methods
Patients
Data on 666 children with infantile spasms admitted
to the Chinese PLA General Hospital and Beijing Children's Hospital
affiliated with Capital Medical University (Beijing, China) from
January 2008 to October 2012 were retrospectively analyzed. The
study was approved by the Ethics Committee of the Chinese PLA
General Hospital. Written informed consent was obtained from all
patients included in the study.
Diagnosis of infantile spasms
The diagnostic criteria for infantile spasms were as
follows: i) the presence of epileptic spasms; ii) hypsarrhythmia or
modified hypsarrhythmia on EEG recordings (NicoletOne Ambulatory
EEG; Cardinal Health, Inc., Dublin, OH, USA) prior to treatment;
and iii) age of onset of the infantile spasms between 1 month and 2
years (1). Hypsarrhythmia was
characterized by EEG findings showing a chaotic background with
nearly continuous random asynchronous high-voltage slow waves and
spikes arising from multiple foci. Modified hypsarrhythmia was
defined as the presence of any of the following: Hypsarrhythmia
with increased interhemispheric synchronization, asymmetric
hypsarrhythmia, hypsarrhythmia with a consistent focus of abnormal
discharge, hypsarrhythmia with episodes of voltage attenuation, and
hypsarrhythmia with small spikes or sharp activity (17).
Diagnosis of neonatal
hypoglycemia
Neonatal hypoglycemia was confirmed by laboratory
results during the neonatal period based on a review of medical
records. Hypoglycemia was defined as a condition in which the whole
blood glucose concentration was <2.6 mmol/l (18).
Seizure analysis
Seizure semiology was analyzed based on clinical
history, contact with parents or caregivers, and video-EEG
recordings. All patients received long-term video-EEG recordings
and neuroradiological investigations following the onset of spasms
but prior to antiepileptic treatment. For the majority of patients,
magnetic resonance imaging (MRI; GE Signa EXCITE 1.5T MRI machine;
GE Healthcare Life Sciences, Chalfont, UK) of the brain was
repeated more than once to better clarify the tomography of
lesions. These retrospective data were collected by two of the
authors (Dr Shi and Dr Wang); the retrospective study protocol was
stringently followed so that no bias was introduced in this
process. The final brain MRI images were analyzed by two different
authors (Dr Tian and Dr Yao), who are experienced
neuroradiologists, in order to benefit from the optimum imaging
quality and to identify the precise extent of chronic brain
damage.
Results
Case selection
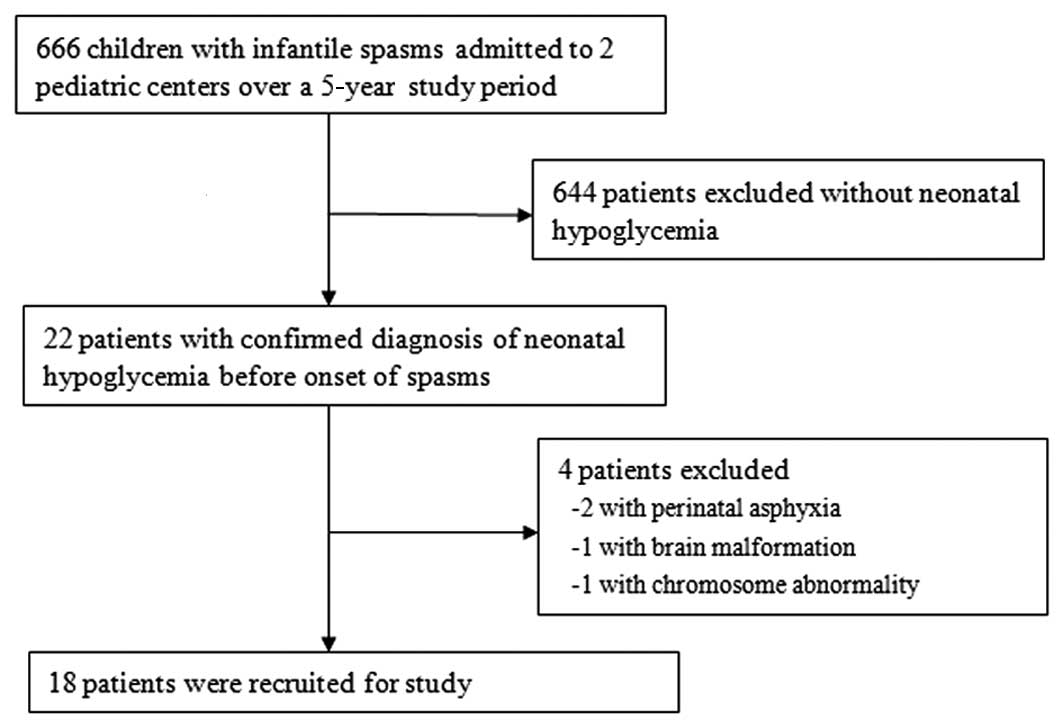
Among the 666 diagnosed cases of infantile spasm, 22
patients suffered from neonatal hypoglycemia with a whole blood
glucose concentration of <2.6 mmol/l during the neonatal period.
Among these 22 patients, 4 cases were excluded, comprising 2
patients who presented with perinatal asphyxia, 1 patient who had
brain malformations, and 1 patient who exhibited a chromosome
abnormality. These complications identified in the 4 patients might
have jointly contributed to the subsequent spasms. Among the
recruited 18 patients, there were 16 boys, and 2 girls. Seventeen
of the patients were full-term infants at birth, whereas one was
premature. Once the diagnosis of neonatal hypoglycemia was
confirmed, glucose was immediately supplemented intravenously. The
case selection process is presented in Fig. 1.
Risk factors
With regard to the risk factors of the 18 cases of
neonatal hypoglycemia, there were 6 cases with poor feeding, 5
cases with diabetic mothers, 3 cases afflicted by neonatal
swallowing syndrome, 1 preterm infant, and 3 cases with no clear
cause. All these subjects were confirmed to have neonatal
hypoglycemia at 1–4 days after birth. Neonatal seizures were
observed in 5/18 (27.8%) children prior to the development of
infantile spasms. The patients developed infantile spasms at a
range of 2 to 10 months (mean, 4.9 months) after the diagnosis of
neonatal hypoglycemia, which is consistent with previously reported
data (6). The detailed clinical data
on these 18 cases are presented in Table
I.
 | Table I.Clinical data on 18 patients with
infantile spasms after neonatal hypoglycemia. |
Table I.
Clinical data on 18 patients with
infantile spasms after neonatal hypoglycemia.
| Case no. | Gender | Age at onset of
spasms (months) | Birth status | Age at onset of NH
(days) | Neonatal
seizures | EEG results | Brain MRI
results |
|---|
| 1 | Male | 3 | Full term | 2 | No | Hypsarrhythmia | Bilateral corona
radiata and occipital abnormal signal intensity |
| 2 | Male | 8 | Preterm | 2 | No | Hypsarrhythmia | Bilateral centrum
semiovale abnormal signal intensity |
| 3 | Female | 5 | Full term | 3 | Yes | Modified
hypsarrhythmia | Bilateral
parieto-occipital cystic damage |
| 4 | Male | 4 | Full term | 3 | No | Hypsarrhythmia | Normal |
| 5 | Male | 4 | Full term | 2 | Yes | Hypsarrhythmia | Left occipital cystic
damage |
| 6 | Male | 3.5 | Full term | 3 | No | Hypsarrhythmia | Normal |
| 7 | Male | 6 | Full term | 2 | No | Hypsarrhythmia | Bilateral occipital
polycystic |
| 8 | Male | 2 | Full term | 2 | No | Modified
hypsarrhythmia | Normal |
| 9 | Male | 4 | Full term | 4 | Yes | Modified
hypsarrhythmia | Normal |
| 10 | Male | 7 | Full term | 3 | No | Hypsarrhythmia | Bilateral occipital
periventricular white matter abnormal signal intensity |
| 11 | Male | 4 | Full term | 2 | No | Hypsarrhythmia | Right
parieto-occipital cyst damage |
| 12 | Female | 10 | Full term | 1 | No | Hypsarrhythmia | Normal |
| 13 | Male | 5 | Full term | 3 | Yes | Hypsarrhythmia | Bilateral occipital
polycystic damage |
| 14 | Male | 6 | Full term | 4 | No | Modified
hypsarrhythmia | Normal |
| 15 | Male | 4 | Full term | 3 | No | Hypsarrhythmia | Normal |
| 16 | Male | 6 | Full term | 2 | No | Hypsarrhythmia | Bilateral
parieto-occipital cystic damage |
| 17 | Male | 4 | Full term | 2 | Yes | Modified
hypsarrhythmia | Bilateral
parieto-occipital and right temporal cystic damage |
| 18 | Male | 2 | Full term | 3 | No | Modified
hypsarrhythmia | Normal |
EEG results
The video-EEG results of these patients prior to
antiepileptic treatment were analyzed, and all 18 patients
exhibited abnormal EEG findings. The interictal EEG recordings of
12 patients (66.7%) revealed classical hypsarrhythmia, whereas
those of the other 6 patients (33.3%) exhibited modified
hypsarrhythmia.
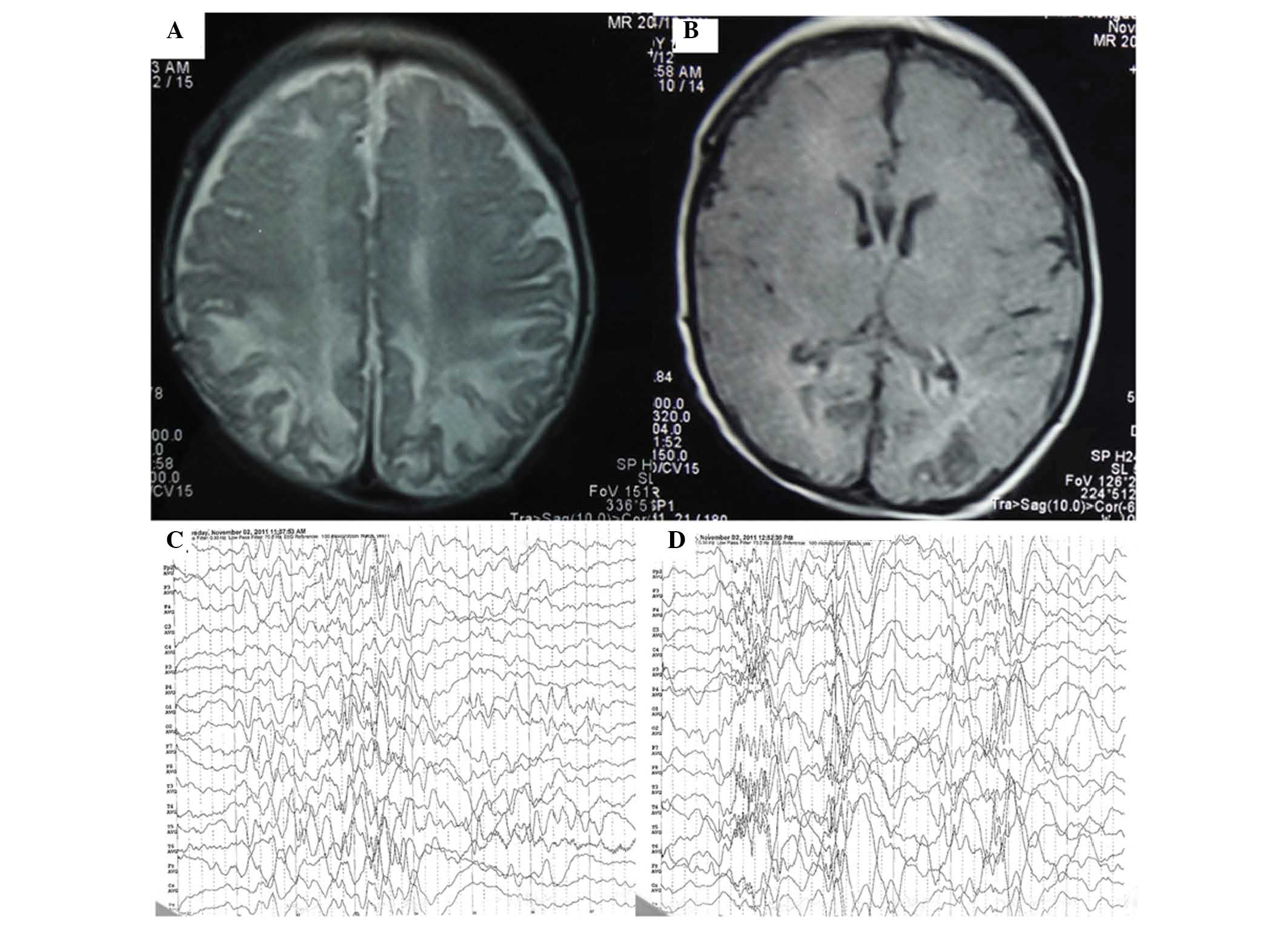
MRI examination
Upon brain MRI examination, 8 patients (44.4%) had
structurally normal brains. However, the images of the other 10
patients (55.6%) were abnormal, primarily showing disproportionate
involvement of the parietal and occipital cortices and sub-cortical
white matter lesions. In case 16, the brain MRI showed bilateral
parieto-occipital encephalomalacia foci (Fig. 2).
Discussion
Infantile spasms are an age-specific epileptic
syndrome associated with diverse etiological factors. Patients with
infantile spasms often have poor developmental outcomes. Extensive
and broad categories of etiologies, including prenatal, perinatal,
and postnatal insult, have been involved in the pathogenesis of
infantile spasms. Furthermore, almost any brain abnormality or
injury can potentially cause infantile spasms (7).
Neonatal hypoglycemic brain injury is a cause of
infantile spasms. However, few large systematic studies have been
conducted to characterize the association of neonatal hypoglycemic
brain injury with infantile spasms. The lack of glucose can
selectively impair multiple brain regions, including the
superficial cortex, dentate gyrus, hippocampus, and caudate
putamen; this impairment occurs through several putative
mechanisms, such as the release of excitatory neurotransmitter
(19), increased mitochondrial free
radical generation and initiation of apoptosis (20), activation of neuronal nicotinamide
adenine dinucleotide phosphate (NADPH) oxidase (21), and altered cerebral energetic
characteristics (22,23). In one study in which the etiology of
remote symptomatic epilepsy with onset during the first 3 years of
life was examined, it was observed that neonatal hypoglycemia was
the most common etiology, and infantile spasms were the most common
type of seizure (14).
Infantile spasms following exposure to neonatal
hypoglycemia are relatively rare and, to the best of our knowledge,
have been described in only two previous reports with a total of 6
patients (9,10). In the present study, the clinical,
biochemical, EEG, and neuroradiological characteristics of 18
patients with neonatal-onset hypoglycemia who subsequently
developed infantile spasms are reported. This case series suggests
that neonatal hypoglycemic brain injury could be an underlying
cause of infantile spasms later in the infancy period. The latency
period of infantile spasms following the onset of neonatal
hypoglycemia was 2–10 months in this case series, and epileptogenic
neutral circuits could be formed during this period. This finding
is consistent with previous observations that the duration of
latency between the onset of insult and the development of
infantile spasms is variable (9,24). This
temporal latency may be explained by the developmental
desynchronization hypothesis, which is that an insult results in
desynchronization of the development between the abnormal cortical
areas and the subcortical structures. This desynchronization
disrupts normal functional interactions and becomes increasingly
important as the brain matures, resulting in a functional deficit
that causes infantile spasms (25).
In our previous studies, which involved an animal
model of NMDA-induced stress and clinical epidemiological analysis,
it was found that prenatal adverse stress is associated with
infantile spasms (26,27). Shi et al (28) proposed a hypothesis (known as Zou's
hypothesis) of prenatal stress exposure for infantile spasms. This
hypothesis states that diverse etiological factors, for example,
brain dysplasia and inherited metabolic diseases, are the
foundations for the onset of infantile spasms, whereas adverse
stress occurring during the perinatal period causes the onset of
infantile spasms. Moreover, the mutual effects of these two aspects
may cause the occurrence of infantile spasms. A close association
exists between neonatal hypoglycemia and stress. Adverse perinatal
stress is an important cause of neonatal hypoglycemia (29,30). A
study conducted in newborn piglets has demonstrated that neonatal
hypoglycemia may also affect the functions of brain cells by
causing specific changes in the cerebral N-methyl-D-aspartate
receptor-associated ion channel, which may subsequently trigger
spasms (31).
With regard to the cause of the 18 cases of neonatal
hypoglycemia in the present study, the majority of these cases were
exposed to various risk factors, including a diabetic mother,
delayed feeding, neonatal swallowing syndrome and prematurity.
Delayed feeding may be one reason that some healthy term neonates
were hypoglycemic. Some newborns were not given formula milk or
sweet water in the few hours after birth, even if the mother's
breast milk was lacking because of the promotion of breastfeeding
by the government. Although hyperinsulinemic hypoglycemia has been
listed as an etiology of infantile spasms, the insulin levels for
those patients with neonatal hypoglycemia were not examined for the
patients in the present study.
In the present study, all 18 patients had abnormal
EEG findings with either classical or modified hypsarrhythmia.
Moreover, more than half of the patients (55.6%) presented abnormal
MRI results. Because of the complexity of a newborn's
circumstances, other factors that may dispose to brain injury, such
as asphyxia, premature birth, low birth weight and maternal factors
complicated the clinical case study. However, in 10 cases with MRI
anomalies, all showed occipital white matter damage, consistent
with hypoglycemic injury to susceptible parts of the brain
mentioned in the literature (16,23);
therefore, it was considered these MRI changes were mainly induced
by hypoglycemia. Previous studies have reported that structural and
functional cortical abnormalities in patients with infantile spasms
have a predilection for posterior brain areas (32,33). In
the present study, MRI neuroimaging principally showed a
disproportionate involvement of parietal and occipital cortices and
sub-cortical white matter lesions.
The significance of this study is that it provides
clinical evidence that neonatal hypoglycemic brain injury is an
important cause of infantile spasms. Whether timely treatment of
hypoglycemia will prevent the onset of infantile spasms and poor
developmental outcome is uncertain, but a better understanding of
the pathophysiological linking between neonatal hypoglycemia and
infantile spasms could result in the development of more effective
neuroprotective strategies. This study highlights the potential
risks of neonatal hypoglycemia, particularly in inadequately
treated patients, and it must be emphasized that close neurological
follow-up is important in children who suffer from neonatal
hypoglycemia.
Acknowledgements
This study was supported by grants from the Major
State Basic Research Development Program (973 Program; grant no.
2012CB517903), the National Natural Science Foundation of China
(grant nos. 30770747, 30801249, 81071036 and 81211140048), the
Beijing Municipal Natural Science Foundation (grant nos. 7142150
and 7081002), the Capital Development Foundation of Beijing (grant
no. 2003-2037), the Capital Characteristic Clinical Application
Research Foundation (grant no. Z121107001012056), the Hygiene
Industry-Specific Research Projects of China (grant no. 200802074),
the Sanya Municipal Scientific and Technological Innovation Project
in Health Care (grant no. 2014YW41) and the Science and Technology
Special Fund for Social Development of Hainan Province (grant no.
2015SF05).
References
|
1
|
Pellock JM, Hrachovy R, Shinnar S, Baram
TZ, Bettis D, Dlugos DJ, Gaillard WD, Gibson PA, Holmes GL, Nordl
DR, et al: Infantile spasms: A US consensus report. Epilepsia.
51:2175–2189. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lux AL: Latest American and European
updates on infantile spasms. Curr Neurol Neurosci Rep. 13:3342013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pavone P, Striano P, Falsaperla R, Pavone
L and Ruggieri M: Infantile spasms syndrome, West syndrome and
related phenotypes: What we know in 2013. Brain Dev. 36:739–751.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Trevathan E, Murphy CC and Yeargin-Allsopp
M: The descriptive epidemiology of infantile spasms among Atlanta
children. Epilepsia. 40:748–751. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Go CY, Mackay MT, Weiss SK, Stephens D,
Adams-Webber T, Ashwal S and Snead OC III: Child Neurology Society;
American Academy of Neurology: Evidence-based guideline update:
Medical treatment of infantile spasms. Report of the Guideline
Development Subcommittee of the American Academy of Neurology and
the Practice Committee of the Child Neurology Society. Neurology.
78:1974–1980. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hrachovy RA and Frost JD Jr: Infantile
spasms. Handb Clin Neurol. 111:611–618. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Osborne JP, Lux AL, Edwards SW, Hancock E,
Johnson AL, Kennedy CR, Newton RW, Verity CM and O'Callaghan FJ:
The underlying etiology of infantile spasms (West syndrome):
Information from the United Kingdom infantile spasms study (UKISS)
on contemporary causes and their classification. Epilepsia.
51:2168–2174. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yu JY and Pearl PL: Metabolic causes of
epileptic encephalopathy. Epilepsy Res Treat.
2013:1249342013.PubMed/NCBI
|
|
9
|
Camurdan MO, Cinaz P, Serdaroğlu A, Bideci
A and Demirel F: Persistent hyperinsulinemic hypoglycemia
presenting with a rare complication: West syndrome. J Pediatr
Endocrinol Metab. 17:1465–1468. 2004.PubMed/NCBI
|
|
10
|
Kumaran A, Kar S, Kapoor RR and Hussain K:
The clinical problem of hyperinsulinemic hypoglycemia and resultant
infantile spasms. Pediatrics. 126:e1231–e1236. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rozance PJ: Update on neonatal
hypoglycemia. Curr Opin Endocrinol Diabetes Obes. 21:45–50. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Boardman JP, Wusthoff CJ and Cowan FM:
Hypoglycaemia and neonatal brain injury. Arch Dis Child Educ Pract
Ed. 98:2–6. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vijay K and Agarwal A: Neonatal
hypoglycemia resulting in occipital cerebral injury. Pediatr
Radiol. 40(Suppl 1): S1782010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Udani V, Munot P, Ursekar M and Gupta S:
Neonatal hypoglycemic brain-injury a common cause of infantile
onset remote symptomatic epilepsy. Indian Pediatr. 46:127–132.
2009.PubMed/NCBI
|
|
15
|
Montassir H, Maegaki Y, Ogura K, Kurozawa
Y, Nagata I, Kanzaki S and Ohno K: Associated factors in neonatal
hypoglycemic brain injury. Brain Dev. 31:649–656. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Termote B, Verswijvel G, Gelin G and
Palmers Y: Neonatal hypoglycemic brain injury. JBR-BTR. 91:116–117.
2008.PubMed/NCBI
|
|
17
|
Jain P, Sharma S and Tripathi M: Diagnosis
and management of epileptic encephalopathies in children. Epilepsy
Res Treat. 2013:5019812013.PubMed/NCBI
|
|
18
|
Harris DL, Weston PJ, Signal M, Chase JG
and Harding JE: Dextrose gel for neonatal hypoglycaemia (the Sugar
Babies Study): A randomised, double-blind, placebo-controlled
trial. Lancet. 382:2077–2083. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Papagapiou MP and Auer RN: Regional
neuroprotective effects of the NMDA receptor antagonist MK-801
(dizocilpine) in hypoglycemic brain damage. J Cereb Blood Flow
Metab. 10:270–276. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ballesteros JR, Mishra OP and McGowan JE:
Alterations in cerebral mitochondria during acute hypoglycemia.
Biol Neonate. 84:159–163. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Suh SW, Gum ET, Hamby AM, Chan PH and
Swanson RA: Hypoglycemic neuronal death is triggered by glucose
reperfusion and activation of neuronal NADPH oxidase. J Clin
Invest. 117:910–918. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Imai T, Kondo M, Isobe K, Itoh S and
Onishi S: Cerebral energy metabolism in insulin induced
hypoglycemia in newborn piglets: In vivo 31P-nuclear
magnetic resonance spectroscopy. Acta Paediatr Jpn. 38:343–347.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wong DS, Poskitt KJ, Chau V, Miller SP,
Roland E, Hill A and Tam EW: Brain injury patterns in hypoglycemia
in neonatal encephalopathy. AJNR Am J Neuroradiol. 34:1456–1461.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Guggenheim MA, Frost JD Jr and Hrachovy
RA: Time interval from a brain insult to the onset of infantile
spasms. Pediatr Neurol. 38:34–37. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Frost JD Jr and Hrachovy RA: Pathogenesis
of infantile spasms: A model based on developmental
desynchronization. J Clin Neurophysiol. 22:25–36. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shang NX, Zou LP, Zhao JB, Zhang F and Li
H: Association between prenatal stress and infantile spasms: A
case-control study in China. Pediatr Neurol. 42:181–186. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zou LP, Zhang WH, Wang HM, Zen M, Chen K
and Mix E: Maternal IgG suppresses NMDA-induced spasms in infant
rats and inhibits NMDA-mediated neurotoxicity in hippocampal
neurons. J Neuroimmunol. 181:106–111. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shi XY, Zou LP, Yang G and Ding YX:
Prenatal stress exposure hypothesis for infantile spasms. Med
Hypotheses. 78:735–737. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Nold JL and Georgieff MK: Infants of
diabetic mothers. Pediatr Clin North Am. 51:619–37. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Najati N and Saboktakin L: Prevalence and
underlying etiologies of neonatal hypoglycemia. Pak J Biol Sci.
13:753–756. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
McGowan JE, Zanelli SA, Haynes-Laing AG,
Mishra OP and Delivoria-Papadopoulos M: Modification of glutamate
binding sites in newborn brain during hypoglycemia. Brain Res.
927:80–86. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chugani HT, Shewmon DA, Shields WD, Sankar
R, Comair Y, Vinters HV and Peacock WJ: Surgery for intractable
infantile spasms: Neuroimaging perspectives. Epilepsia. 34:764–771.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hamano S, Tanaka M, Kawasaki S, Nara T,
Horita H, Eto Y and Kohno S: Regional specificity of localized
cortical lesions in West syndrome. Pediatr Neurol. 23:219–224.
2000. View Article : Google Scholar : PubMed/NCBI
|