Introduction
Bisphosphonates (BPs) are synthetic analogues of
inorganic pyrophosphates, which act as potent inhibitors of
osteoclast-mediated bone resorption (1,2). This
type of drug is currently used in various pathological conditions,
including postmenopausal osteoporosis, hypercalcemia associated
with malignancy, lytic bone metastasis and other metabolic bone
diseases (3,4). The two most potent and widely used
nitrogen-containing BPs are zoledronate and alendronate, which
inhibit the intracellular mevalonate pathway (5,6). The
target protein of the nitrogen-containing BPs is considered to be
farnesyl diphosphate synthase, an important regulatory enzyme for
isoprenoid lipid production (6).
Certain isoprenoid lipids, including farnesyl
pyrophosphate and geranyl-geranyl pyrophosphosphate, serve an
important role in the prenylation and activation of small GTPases,
such as Ras, rhodopsin, Rac, Rab and cell division cycle 42
(7). In turn, the small GTPases
function as signaling proteins involved in the regulation of
osteoclast morphology, cytoskeleton arrangement, membrane ruffling,
trafficking and cell survival (8–11).
Currently, the resulting adverse effects from BP treatment are an
important issue. Although BPs are beneficial for several
pathological conditions of the bone, BP-related osteonecrosis of
the jaw (BONJ) has been reported (12). BONJ has been predominantly observed
in patients who underwent mechanical trauma, such as tooth
extraction, or were affected by periodontal disease, as well as
patients receiving corticosteroid treatment (1,13,14).
Despite the importance of the problem and numerous studies
investigating BONJ since 2004 (1,13,14),
BONJ etiology and pathophysiology remain largely unknown. Several
hypotheses have been proposed, including BP toxicity to oral
epithelium, altered wound healing following tooth extraction, high
turnover of the mandible and maxilla, oral biofilm formation,
infection and inflammation, suppression of angiogenesis and bone
turnover, and osteoblast death (15–19).
Our previous studies (20,21)
conducted on epithelial and bone tissue samples from patients with
BONJ demonstrated the presence of structural alteration of the
bone; furthermore, a decrease or absence of adhesion proteins,
sarcoglycans and integrins, was observed in the gingival epithelium
of patients with BONJ. Therefore, it was hypothesized that two
different pathogenic processes lead to BONJ: An indirect process,
from the oral mucosa to the bone, and a direct process, from the
bone to the mucosa (20,21).
ONJ is a complex disease that involves the
interaction of multiple tissues and cell types in response to local
wound healing; it is therefore difficult to replicate the disease
conditions in vitro. Various animal models replicating the
clinical, radiographic and histologic features of ONJ have been
developed in rats, mice and mini pigs (22–24). The
majority of these animal models underwent tooth extraction
following prolonged periods with high-dose BP treatment, suggesting
that BPs alter bone healing and lead to bone exposure. However, a
significant fraction of ONJ diseases occurs in the absence of tooth
extraction.
Therefore, the present study used a rat model to
observe the bone and gingiva during 45 days of zoledronate
treatment, without tooth extraction. The aim of the present
investigation was to analyze the changes that occur in the bone and
in the gingiva during treatment with BPs in order to determine the
mechanisms underlying the progression of bone osteonecrosis.
Furthermore, based on the two previous hypotheses the study also
aimed to determine which process, direct or indirect, leads to
BONJ.
Materials and methods
Animals
A total of 40 male Wistar rats (age, 7 weeks) were
purchased from Janvier Labs (Saint Berhevin, France). The rats were
housed in individual cages with bedding, and standard rat food and
tap water were available ad libitum for the duration of the
experimental period, unless otherwise noted. The rats were
maintained under a 12-h light/dark cycle at a constant temperature
of 22.0±0.6°C. The rat handling procedures were conducted in
accordance with the European Communities Council Directive of the
24th November 1986 (86/609/EEC). All experimental protocols were
approved by the Committee for Animal Care and Use at the University
of Messina (Messina, Italy). A total of 20 rats were treated with
intraperitoneal injections of 0.1 mg/kg zoledronate (Novartis
Pharmaceuticals Corporation East Hanover, NJ, USA) three times a
week, and an additional 20 rats were injected with saline as a
control. Doses and time schedules of drug administration were
designed according to previous studies (25,26).
After 7, 15, 30 and 45 days of treatment, 5 rats from each group
were sacrificed by paraformaldehyde (Sigma-Aldrich, St. Louis, MO,
USA) injection into the left ventricle of the heart, and their
mandibles were harvested and divided in two parts. One part was
used for scanning electron microscopy (SEM) and the second part was
used for histological and immunofluorescence analyses. In addition,
gingival epithelia biopsies were obtained and used for histological
and immunofluorescence analyses.
SEM
The tissue specimens were fixed with 2%
glutaraldehyde (Santa Cruz Biotechnology, Inc., Dallas, TX, USA) in
0.1 M phosphate buffer (Sigma-Aldrich) at pH 7.4 at room
temperature. The specimens were dehydrated through a gradual
increase in the concentration of ethanol and amyl acetate (1st
solution: 25% ethanol, 25% amyl acetate, 50% distilled water; 2nd
solution: 35% ethanol, 35% amyl acetate, 30% distilled water; 3rd
solution: 40% ethanol, 40% amyl acetate, 20% distilled water; 4th
solution: 45% ethanol, 45% amyl acetate, 10% distilled water and;
5th solution: 50% ethanol and 50% amyl acetate; Merck Millipore,
Darmstadt, Germany). Subsequently, the tissue specimens were dried
at critical-point in a Leica EM CPD030 Critical Point Dryer (Leica
Microsystems GmbH, Wetzlar, Germany) using liquid CO2.
The fractured surface of the mandible was mounted on stub supports
(Tousimis, Rockville, MD, USA) and platinum coated with a Plasma
Sciences CrC-100 Turbo-Pumped sputtering system (Electron
Microscopy Sciences, Hatfield, PA, USA), and observed using a
Phenom G2 Pro scanning electron microscope (Phenom-World B.V.,
Eindhoven, The Netherlands).
Histological analysis
Following perfusion, the tissue specimens were
post-fixed with 2% glutaraldehyde and 12.5% formaldehyde
(Sigma-Aldrich), and buffered in 0.1 M sodium cacodylate (pH 7.4;
Sigma-Aldrich) at room temperature for 4 h. Following rinses in 13
M phosphate buffer (pH 7.3), the tissue specimens were decalcified
in 4.13% ethylenediaminetetraacetic acid (pH 7.2; Hach Company,
Loveland, CO, USA) for 30 days, dehydrated in ethanol and embedded
in paraffin. Tissue sections (5 mm) were obtained using the Leica
RM2255 microtome (Leica Microsystems GmbH) and stained with
hematoxylin and eosin (H&E; Abbey Color, Philadelphia, PA, USA)
for 15 and 5 min, respectively, at room temperature.
Immunofluorescence
Non-colored sections of bone and gingiva (10 mm),
prepared during the histological analysis were deparaffinized twice
in xylene (5 min each; Sigma-Aldrich), hydrated twice in 100%
ethanol (3 min each), 95% ethanol (1 min), 90% ethanol (1 min) and
80% ethanol (1 min), and rinsed in distilled water. Pre-heating was
conducted in a MW 200 steamer (De'Longhi Appliances S.r.l, Treviso,
Italy) with a staining dish containing sodium citrate buffer
(Sigma-Aldrich) at 95–100°C.
To block non-specific sites and to make the
membranes permeable, the mandible and gingiva tissue sections were
pre-incubated with 1% bovine serum albumin and 0.3% Triton X-100
(both Sigma-Aldrich) in phosphate-buffered saline at room
temperature for 15 min. Next, the tissue sections were incubated
with primary antibodies at room temperature for 2 h. For the
mandible tissue sections, the following primary antibodies were
used: Rabbit polyclonal anti-receptor activator of nuclear
factor-κB (RANK; 1:150; sc-9072; Santa Cruz Biotechnology, Inc.) to
detect osteoclasts, and rabbit polyclonal anti-osteocalcin (1:200;
sc-30045; Santa Cruz Biotechnology, Inc.) to detect osteoblasts.
For gingival epithelia tissue sections, goat polyclonal
anti-ε-sarcoglycan (1:100; Santa Cruz Biotechnology, Inc.) was
used. Incubation with anti-RANK and anti-ε-sarcoglycan primary
antibodies was followed by incubation with Texas Red-conjugated
anti-goat (305-075-047) and Rhodamine Red-conjugated anti-rabbit
(711-295-152) IgG (heavy&light chains), respectively (1:100;
Jackson ImmunoResearch Laboratories, Inc., West Grove, PA, USA), at
room temperature for 1 h. Incubation with anti-osteocalcin antibody
was followed by incubation with fluorescein
isothiocyanate-conjugated anti-rabbit fluorochrome (1:100;
111-095-046; Jackson ImmunoResearch Laboratories, Inc.) at room
temperature for 1 h. The tissue samples were observed with a Zeiss
LSM 510 confocal microscope (Zeiss AG, Oberkochen, Germany)
equipped with an Argon laser (458 nm and 488 nm λ) and two HeNe
lasers (543 nm and 633 nm λ). All images were digitized at a
resolution of 8 bits into an array of 2,048×2,048 pixels. Optical
sections of the fluorescent tissue specimens were obtained at 488
nm λ, and 62/sec scanning shipped with ≥8 repetitions on average.
The detection pinhole was set for optimal resolution. Contrast and
brightness were established by examining the most brightly labelled
pixels and selecting settings that allowed clear visualization of
structural details while keeping the highest pixel intensities
~200. Digital images were cropped and figure montages prepared
using Adobe Photoshop 7.0 (Adobe Systems, Inc., San Jose, CA,
USA).
Results
BP treatment
The bone and gingiva tissue samples from all rats
were observed by H&E staining, SEM and immunofluorescence. No
differences were observed in the bone and gingiva tissue samples
after 7 and 15 days of zoledronate (0.1 mg/kg) treatment, as
compared with the control group. In addition, the results observed
after 7 days were similar to those observed after 15 days of
treatment. In the bone and gingiva tissue samples, several changes
were observed after 30 and 45 days of treatment, as compared with
the bone and gingiva tissue samples treated for 7 or 15 days, and
the control group. The results observed at 30 and 45 days of
treatment were similar. Based on these results, the tissue
specimens were described and compared in two groups, including the
7–15 and 30–45 groups, according to the number of days after
zoledronate treatment. No cases of necrosis or bone exposure were
observed.
SEM
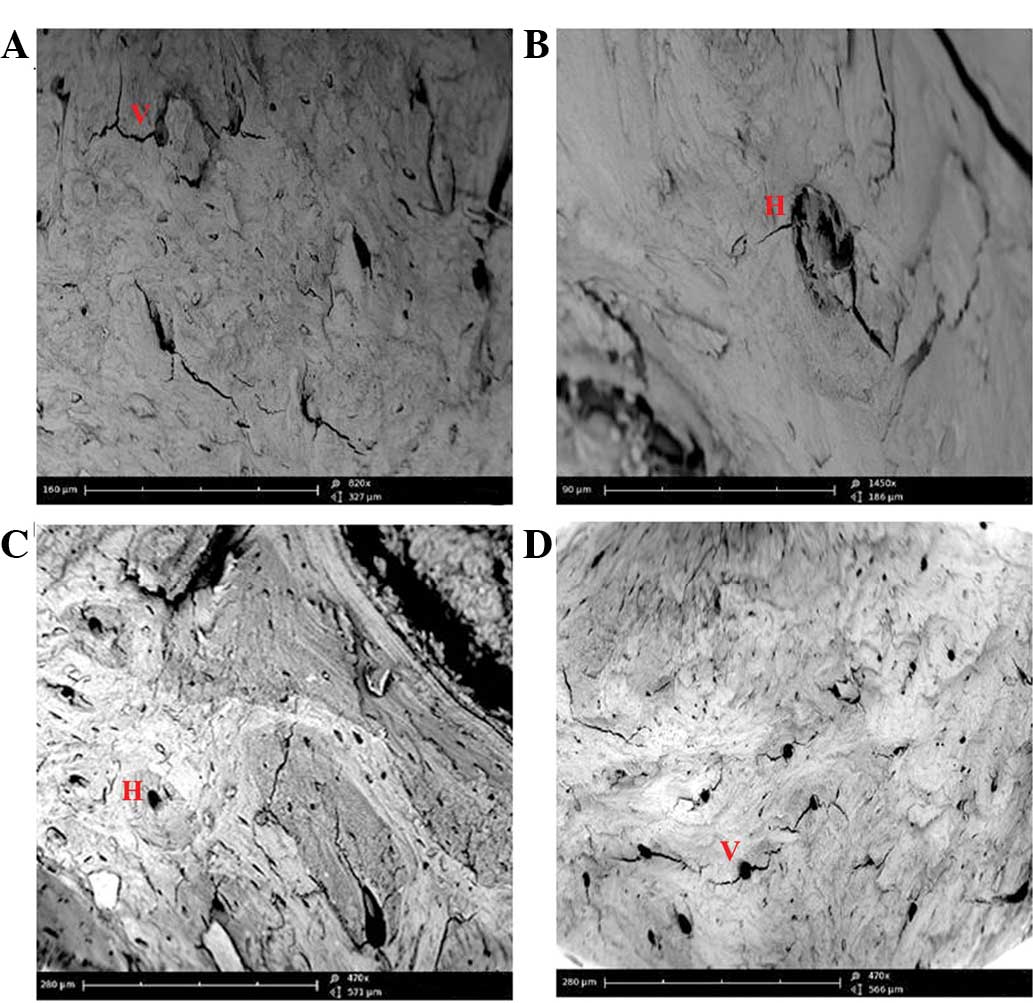
The images of the 7–15 group (Fig. 1) highlighted the presence of full
osteocytic lacunae, Haversian systems and Volkmann canals in the
cortical and trabecular alveolar bone regions. Conversely, images
of the 30–45 (Fig. 1) group showed
numerous empty osteocytic lacunae, which were particularly abundant
in the cortical bone. Empty Haversian systems and Volkmann canals
were also observed.
H&E staining
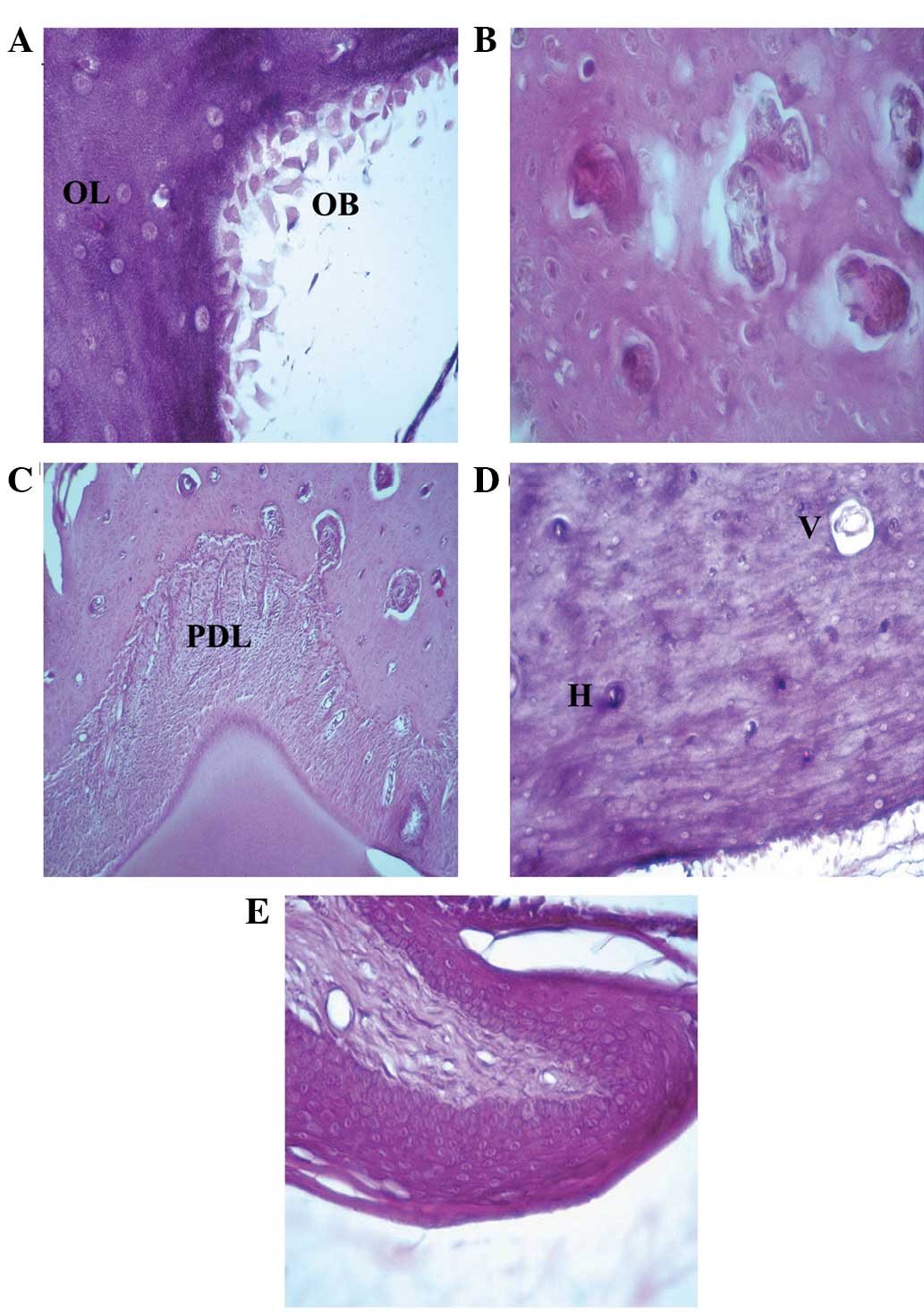
The mandibular bones after 7–15 days of zoledronate
treatment (Fig. 2) exhibited similar
characteristics to healthy bones, as evidenced by full osteocytic
lacunae, presence of osteoblasts at the mineralization sides, full
Howship's lacunae with osteoclastic rims, normal Haversian'
systems, and Volkmann's canals. The normal structure of surrounding
periodontal ligament and gingival mucosa were also observed.
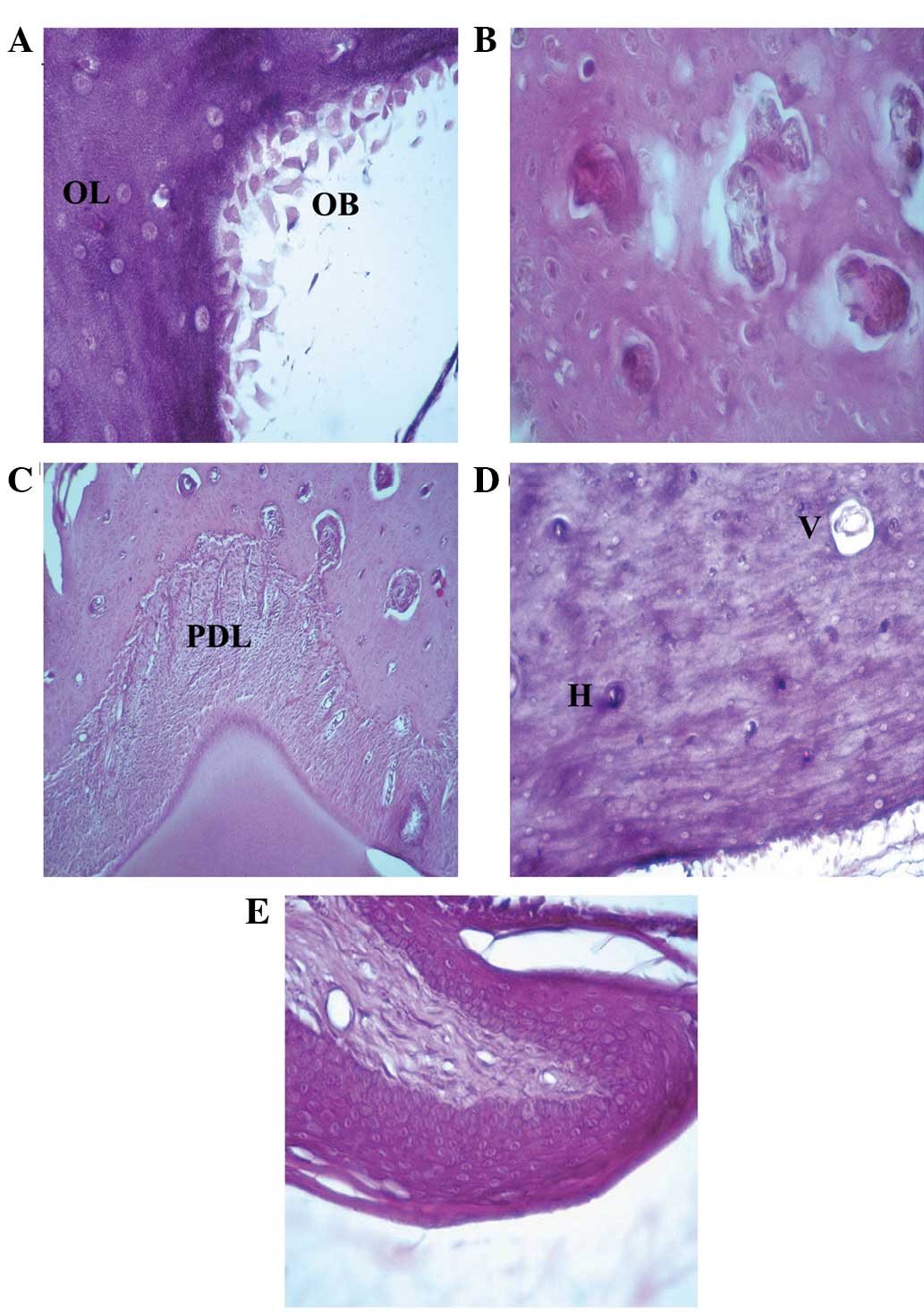 | Figure 2.Hematoxilin and eosin staining of the
rat mandibular bone and gingival epithelium after 7–15 days of
zoledronate treatment (0.1 mg/kg). (A) Osteoblasts at the rim side
of the cortical bone and full osteocytic lacunae were observed
(magnification, ×40). Hematoxylin and eosin staining also
demonstrated the presence of (B) full Howship's lacunae
(magnification, ×40), (C) normal periodontal ligament between the
tooth root and the bone (magnification, ×10) and (D) full Volkman's
and Haversian systems (magnification, ×20). (E) Normal gingival
epithelium structure (magnification, ×20). OB, osteoblast; OL,
osteocytic lacunae; PDL, periodontal ligament; V, Volkman's
systems; H, Haversian systems. |
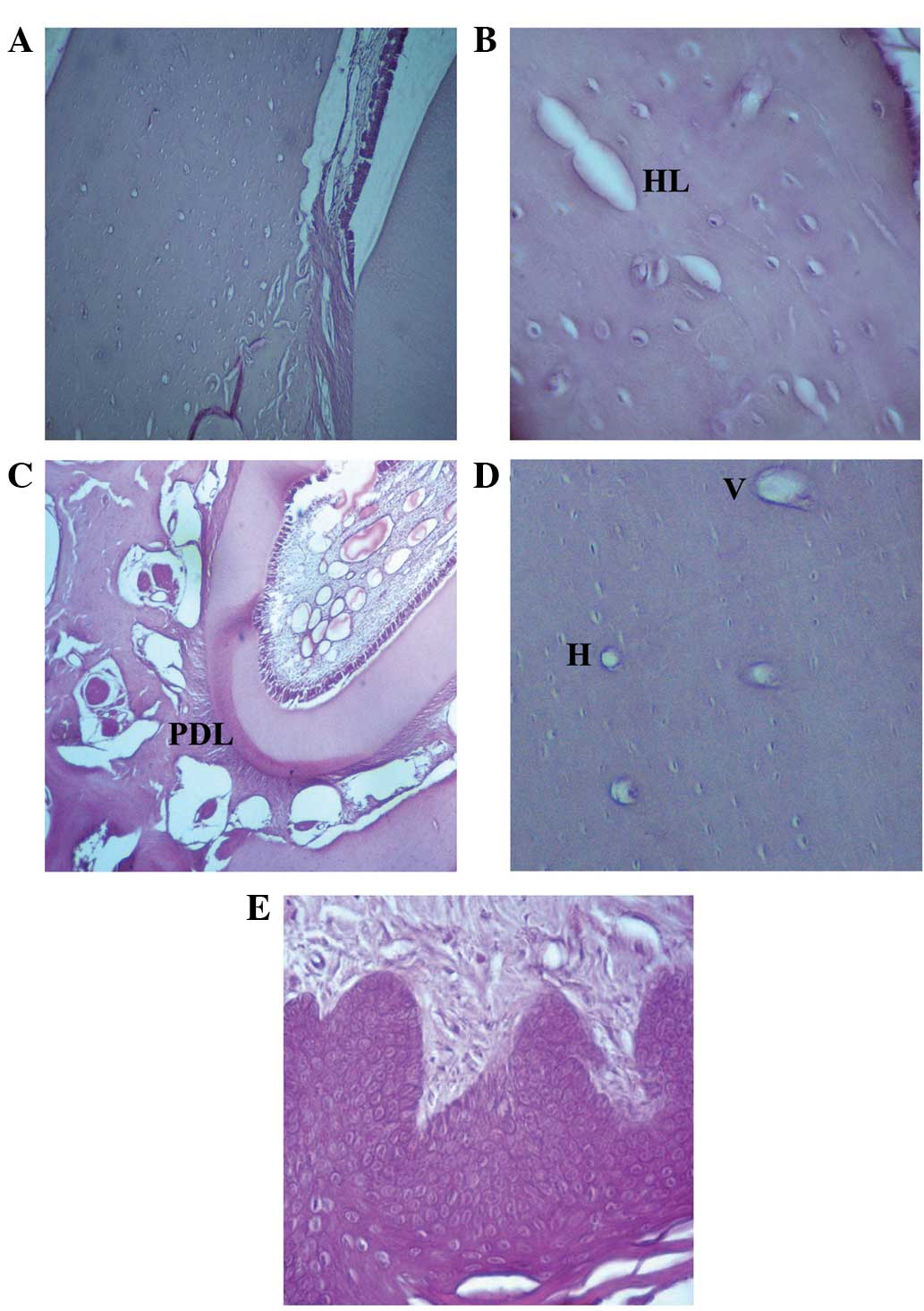
Mandibular bones after 30–45 days of zoledronate
treatment (Fig. 3) exhibited
structural modifications as evidenced by empty osteocytic lacunae,
which were particularly abundant in the cortical bone surrounding
the alveolar socket. The presence of empty Howship's lacunae,
Haversian systems and Volkmann canals was also noted. No
osteoblastic rims were observed in a wide area of bone surrounding
the tooth root region, as evidenced by the absence of osteoblasts
in the mineralized side. Occasionally, the surrounding tissue
samples exhibited altered structure, as evidenced by abnormal gaps
between the periodontal ligament and bone; however, the gingival
epithelium and connective tissue showed normal organization.
Regions of healthy bone were also observed in these samples.
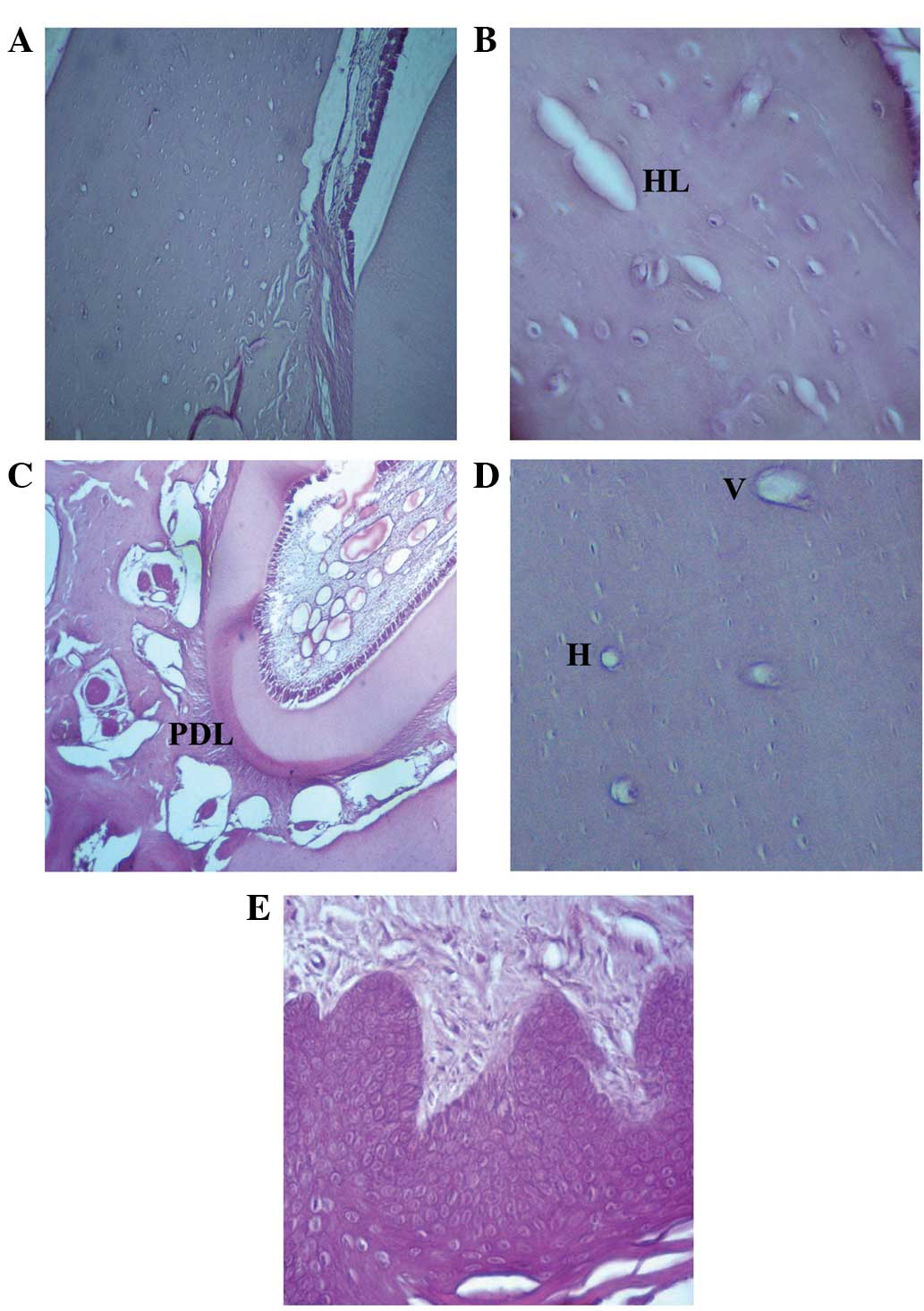 | Figure 3.Hematoxilin and eosin staining of the
rat mandibular bone and gingival epithelium following 30–45 days of
zoledronate treatment (0.1 mg/kg). (A) Osteoblasts at the rim side
of the cortical bone and empty osteocytic lacunae (magnification,
×10), as well as (B) Howship's lacunae (magnification, ×40) were
observed. Hematoxylin and eosin staining also demonstrated the
presence of (C) a detachment of the periodontal ligament from the
bone (magnification, ×20), as well as (D) empty Volkman's and
Haversian systems (magnification, ×20). (E) Normal gingival
epithelium structure (magnification, ×20). HL, Howship's lacunae;
PDL, periodontal ligament; V, Volkman's systems; H, Haversian
systems. |
Immunofluorescence
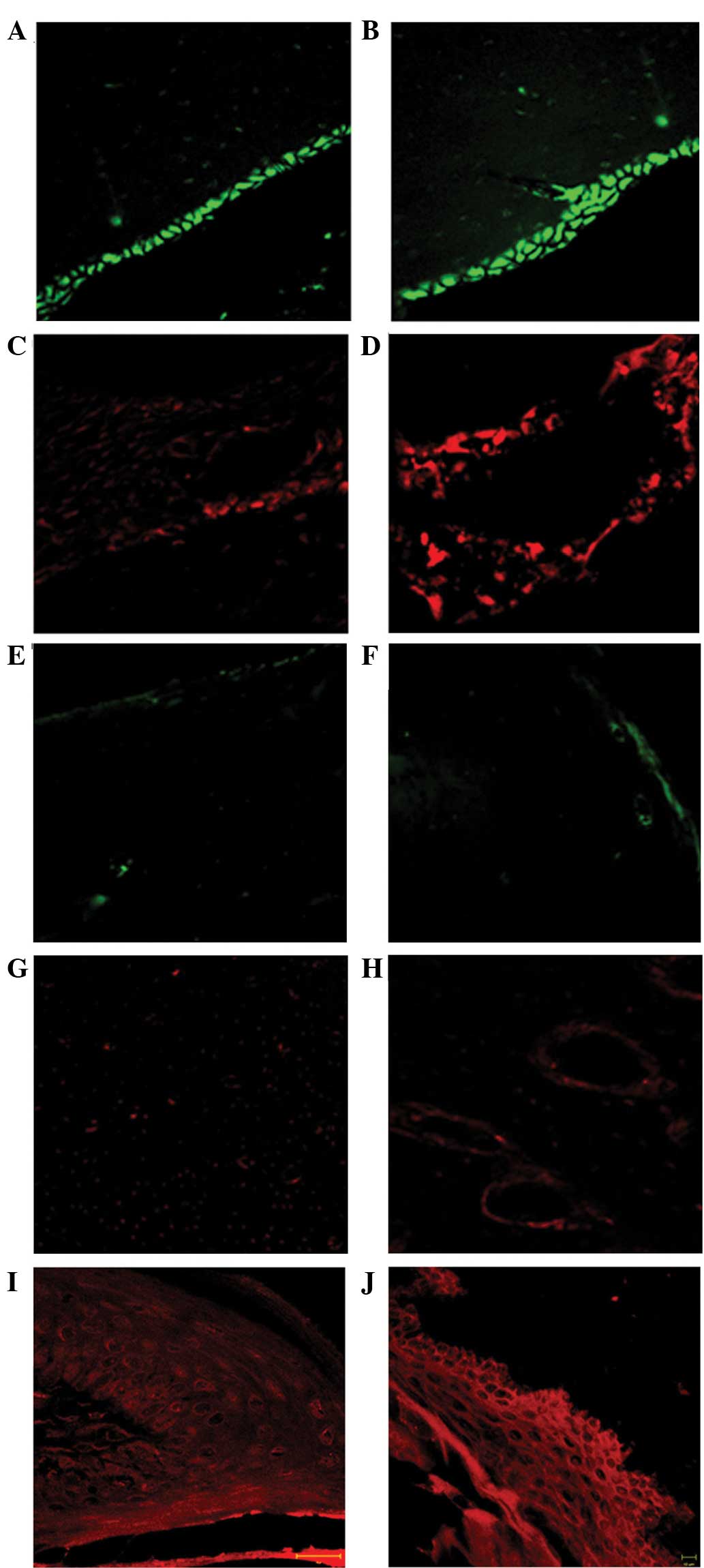
Immunofluorescence analysis of the 7–15 group
specimens (Fig. 4A–D) showed the
presence of osteoclasts and osteoblasts, as evidenced by the RANK
(red) and osteocalcin (green) markers, respectively. Osteoclasts
were detected in Howship's lacunae. Conversely, bone specimens in
rats treated with zoledronate for 30–45 days (Fig. 4E–H) exhibited a marked reduction in
osteoblast fluorescence, specifically in the cortical bone
surrounding the alveolar socket. Furthermore, the images showed a
weak osteoclast fluorescence pattern, and absence of fluorescence
in several Howship's lacunae. Immunofluorescence analysis of the
gingival epithelium demonstrated the presence of a uniform
distribution pattern of sarcoglycans (red channel) along the
epithelial layers in both the 7–15 and 30–45 groups (Fig. 4I and J, respectively).
Discussion
BP therapy is currently used to contrast several
bone pathological conditions, including multiple myeloma,
metastatic disease of the skeleton, Paget's disease of the bone and
osteoporosis (3,4). This type of drug inhibits osteoclast
bone resorption, thereby inhibiting loss of bone mass. It is well
established that a recognized side effect of BP is BONJ (12). The etiology and pathogenesis of BONJ
remain unclear, although several hypotheses have been proposed. It
was initially proposed that a hypoxic/ischemic signaling pathway
leads to BONJ, due to the anti-angiogenic properties of the drugs
(17,18). Currently, the most accredited
hypothesis suggests that the accumulation of BPs in the bone
inhibits osteoclast activity and their ability to maintain the bone
integrity (8–11). BPs also inhibit the regenerative
mechanisms underlying periodontal disease, tooth extraction and
invasive surgical treatment in the alveolar bone (13). BONJ has been predominantly observed
in patients who underwent surgical treatment, such as tooth
extractions or implant placement, or following traumatic events
(13,14). However, the lesions may also occur
spontaneously with no history of surgical procedures, trauma or
radiation therapy.
Our previous studies, conducted on intrasurgical
perilesional bone and gingiva tissue biopsies from patients with
BONJ, demonstrated the presence of bone structural modifications
with empty lacunae, absence of matrix and presence of unorganized
fibrillar structures (20,21). In the gingival epithelium a decrease
or absence of sarcoglycan and integrin transmembrane proteins was
observed (20), proteins which have
a role in cell-cell and cell-matrix adhesion (27–29). In
addition, an increase in vascular endothelial growth factor
expression was observed (21). The
observation of structural alterations in the gingival epithelium
and bone suggested that BPs may act via two processes: A direct
process or an indirect process (21). In the direct process, BPs may act
directly on the bone to induce matrix necrosis, particularly in the
maxilla and mandibular bone due to their high levels of bone
remodeling from the constant stress of the masticatory forces
(21). In the indirect process,
drugs may induce epithelial modification and absence of cell-cell
and cell-matrix adhesion, which allows bacterial transit to the
bone in the oral region causing osteomyelitis (21).
The limitation of the aforementioned studies, as
well as of investigations on a human model, is the difficulty of
successful bone and gingiva tissue sample analysis prior to
necrosis. Therefore, it has yet to be established whether the
observed damage depends on necrotic or surgical events,
specifically in the case of the gingiva. The present study used a
rat experimental model in order to circumvent these problems.
Previous studies using rat models have already been conducted
(30,31), although the majority of these
replicate human clinical and histological features of BONJ by
investigating the mandibular bone or gingival epithelium following
tooth extraction, when bone necrosis has already begun.
A previous report described the bone and gingival
epithelium of rats prior to tooth extraction, demonstrating the
presence of structural alteration of the bone, as evidenced by
empty osteocytic lacunae and inflammation in the gingival mucosa
(22). However, the study used
histological techniques alone, and gingival inflammation was not
fully characterized.
In the present study, the rat mandibular bone and
gingiva were observed after 7, 15, 30 and 45 days of zoledronate
treatment without tooth extraction. The results, obtained by SEM,
hematoxylin and eosin staining, and immunofluorescence demonstrated
that the mandibular bone at 7 and 15 days of treatment exhibited
similar features to those of healthy bone. Only after 30 days of
treatment it was possible to observe structural alteration in large
surface areas of the bone, as evidenced by empty osteocytic
lacunae, and a marked reduction in the number of osteoblasts and
osteoclasts. According to a previous investigation, these
morphological features depend on molecular mechanisms underlying BP
inhibition of the mevalonate signaling pathway; BPs act by
preventing the prenylation and activation of small GTPases that are
essential for the bone-resorbing activity and survival of
osteoclasts (32). Furthermore,
another study suggested that BPs may also have toxic effects on
osteoblasts (19). It is known that
osteoblasts are important to osteoclast differentiation and
activation through the release of osteoclast-activating factors.
BPs may induce a reduction in osteoclasts and osteoblasts; in turn,
reduction of osteoblasts may inhibit bone-resorbing activity, and
the survival of osteoclasts may induce osteonecrosis.
The results of the present study also demonstrated
the presence of empty Haversian and Volkman's canals. These
observations may be explained by the inhibitory effect of BPs on
angiogenesis (17,18), which is of particular interest since
ONJ lesions may result from ischemic changes to the tissues.
Conversely, another study suggested that BPs exerted a
dose-dependent effect on vascularization, and no anti-angiogenic
effect was observed with clinical dosing (33). Although several hypotheses have been
proposed, the anti-angiogenic mechanisms underlying the effects of
BPs remain to be elucidated, and further investigations are
required to identify specific markers of angiogenesis.
In two rats, detachment of the periodontal ligament
from the bone was observed. It has been demonstrated that
nitrogen-containing BPs, upon release from the jawbones in which
they previously accumulated, may have a cytotoxic effect on various
cells located around the jawbones (34). Furthermore, a decrease in osteoclast
activity was demonstrated to influence the differentiation of
periodontal ligament cells (35,36).
However, the data of the present study was not statistically
significant and, for this reason, the observations are not
attributable to the effect of BPs.
An important finding of the present report was the
absence of gingival epithelium lesions as evidenced by H&E
staining, which demonstrated the presence of a normal epithelial
structure. Furthermore, immunofluorescence showed that
α-sarcoglycan expression was present in all tissue specimens. The
sarcoglycan family includes six transmembrane glycoproteins that
have a role in cell-cell and cell-matrix adhesion (37–39).
Therefore, the presence of α-sarcoglycan indicated the absence of
structural and functional alteration in the gingival epithelium in
the 7–15 and 30–45 day treatment groups. The presence of structural
modifications of the bone but no gingival lesions further support
the hypothesis of a direct pathogenic event leading to BONJ.
Furthermore, the present study used an animal model to understand
which are the pathogenic events that occur in a short time frame of
BP treatment without spontaneous or surgically-induced
osteonecrosis. It is possible to speculate that this animal model
may replicate human conditions (BP treatment in the absence of
spontaneous or surgically-induced osteonecrosis). On this basis, it
is possible to consider the mandibular bones of patients treated
with BPs as bones which have lost healthy features. This state at
the early stage of BONJ was defined as stage 0 according to the
modified AAOMS criteria. A lost feature may be the regenerative
ability required following tooth extraction and invasive surgical
treatment of the alveolar bone, allowing bacterial infections and
necrotic bone exposure. This condition may be defined as the late
stage of BONJ, corresponding to stages 2 and 3 according to the
modified AAOMS criteria (40).
In conclusion, the present study aimed to analyze
the rat mandibular bone and gingival epithelium during 45 days of
zoledronate treatment without tooth extraction, in order to
determine the mechanisms underlying the progression of bone
osteonecrosis. The results of the present study demonstrated that,
after 30 and 45 days with low dose zoledronate treatment, the
mandibular bone underwent morphological changes that may predispose
the bone to necrosis when trauma is applied. Further studies should
focus on animal models to further investigate the role of BPs in
the development of BONJ, in order to develop a therapeutic
strategy.
Glossary
Abbreviations
Abbreviations:
|
BONJ
|
bisphosphonate-related osteonecrosis
of the jaw
|
|
ONJ
|
osteonecrosis of the jaw
|
|
PDL
|
periodontal ligament
|
References
|
1
|
Merigo E, Manfredi M, Meleti M, Guidotti
R, Ripasarti A, Zanzucchi E, D'Aleo P, Corradi D, Corcione L,
Sesenna E, et al: Bone necrosis of the jaws associated with
bisphosphonate treatment: A report of twenty-nine cases. Acta
Biomed. 77:109–117. 2006.PubMed/NCBI
|
|
2
|
Gutta R and Louis PJ: Bisphosphonates and
osteonecrosis of the jaws: Science and rationale. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 104:186–193. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Migliorati CA, Schubert MM, Peterson DE
and Seneda LM: Bisphosphonate-associated osteonecrosis of
mandibular and maxillary bone: An emerging oral complication of
supportive cancer therapy. Cancer. 104:83–93. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bertoldo F, Santini D and Lo Cascio V:
Bisphosphonates and osteomyelitis of the jaw: A pathogenic puzzle.
Nat Clin Pract Oncol. 4:711–721. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shipman CM, Rogers MJ, Apperley JF,
Russell RG and Croucher PI: Bisphosphonates induce apoptosis in
human myeloma cell lines: A novel anti-tumour activity. Br J
Haematol. 98:665–672. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Van Beek ER, Cohen LH, Leroy IM, Ebetino
FH, Löwik CW and Papapoulos SE: Differentiating the mechanisms of
antiresorptive action of nitrogen containing bisphosphonates. Bone.
33:805–811. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rogers MJ, Crockett JC, Coxon FP and
Mönkkönen J: Biochemical and molecular mechanisms of action of
bisphosphonates. Bone. 49:34–41. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hughes DE, MacDonald BR, Russell RG and
Gowen M: Inhibition of osteoclast-like cell formation by
bisphosphonates in long-term cultures of human bone marrow. J Clin
Invest. 83:1930–1935. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Löwik CW, van der Pluijm G, van der
Wee-Pals LJ, van Treslong-De Groot HB and Bijvoet OL: Migration and
phenotypic transformation of osteoclast precursors into mature
osteoclasts: The effect of abisphosphonate. J Bone Miner Res.
3:185–192. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fleisch H, Russell RG and Francis MD:
Diphosphonates inhibit hydroxyapatite dissolution in vitro and bone
resorption in tissue culture and in vivo. Science. 165:1262–1264.
1969. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Coxon FP, Helfrich MH, Van't Hof R, Sebti
S, Ralston SH, Hamilton A and Rogers MJ: Protein
geranylgeranylation is required for osteoclast formation, function
and survival: Inhibition by bisphosphonates and GGTI-298. J Bone
Miner Res. 15:1467–1476. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Marx RE: Pamidronate (Aredia) and
zoledronate (Zometa) induced avascular necrosis of the jaws: A
growing epidemic. J Oral Maxillofac Surg. 61:1115–1117. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Costa L, Lipton A and Coleman RE: Role of
bisphosphonates for the management of skeletal complications and
bone pain from skeletal metastases. Support Cancer Ther. 3:143–153.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mawardi H, Giro G, Kajiya M, Ohta K,
Almazrooa S, Alshwaimi E, Woo SB, Nishimura I and Kawai T: A role
of oral bacteria in bisphosphonate-induced osteonecrosis of the
jaw. J Dent Res. 90:1339–1345. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fournier P, Boissier S, Filleur S,
Guglielmi J, Cabon F, Colombel M and Clézardin P: Bisphosphonates
inhibit angiogenesis in vitro and testosterone-stimulated vascular
regrowth in the ventral prostate in castrated rats. Cancer Res.
62:6538–6544. 2002.PubMed/NCBI
|
|
16
|
Kobayashi Y, Hiraga T, Ueda A, Wang L,
Matsumoto-Nakano M, Hata K, Yatani H and Yoneda T: Zoledronic acid
delays wound healing of the tooth extraction socket, inhibits oral
epithelial cell migration and promotes proliferation and adhesion
to hydroxyapatite of oral bacteria, without causing osteonecrosis
of the jaw, in mice. J Bone Miner Metab. 28:165–175. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Khokher MA and Dandona P: Diphosphonates
inhibit human osteoblast secretion and proliferation. Metabolism.
38:184–187. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
De Ponte FS, Favaloro A, Siniscalchi EN,
Centofanti A, Runci M, Cutroneo G and Catalfamo L: Sarcoglycans and
integrins in bisphosphonate treatment: Immunohistochemical and
scanning electron microscopy study. Oncol Rep. 30:2639–2646.
2013.PubMed/NCBI
|
|
19
|
Siniscalchi Nastro E, Cutroneo G,
Catalfamo L, Santoro G, Allegra A, Oteri G, Cicciù D, Alonci A,
Penna G, Musolino C, et al: Immunohistochemial evaluation of
sarcoglycans and integrins in gingival epithelium of multiple
myeloma patients with bisphosphonate-induced osteonecrosis of the
jaw. Oncol Rep. 24:129–134. 2010.PubMed/NCBI
|
|
20
|
Senel FC, Duman Kadioglu M, Muci E,
Cankaya M, Pampu AA, Ersoz S and Gunhan O: Jaw bone changes in rats
after treatment with zoledronate and pamidronate. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 109:385–391. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Su J, Feng M, Han W and Zhao H: The
effects of bisphosphonate on the remodeling of different irregular
bones in mice. J Oral Pathol Med. 44:638–648. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pautke C, Kreutzer K, Weitz J, Knödler M,
Münzel D, Wexel G, Otto S, Hapfelmeier A, Stürzenbaum S and Tischer
T: Bisphosphonate related osteonecrosis of the jaw: A minipig large
animal model. Bone. 51:592–599. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pytlik M, Kaczmarczyk-Sedlak I, Sliwiński
L, Janiec W and Rymkiewicz I: Effect of concurrent administration
of alendronate sodium and retinol on development of changes in
histomorphometric parameters of bones induced by ovariectomy in
rats. Pol J Pharmacol. 56:571–579. 2004.PubMed/NCBI
|
|
24
|
Kapitola J, Zák J, Lacinová Z and Justová
V: Effect of growth hormone and pamidronate on bone blood flow,
bone mineral and IGF-I levels in the rat. Physiol Res. 49(Suppl 1):
S101–S106. 2000.PubMed/NCBI
|
|
25
|
O'Ryan FS and Lo JC:
Bisphosphonate-related osteonecrosis of the jaw in patients with
oral bisphosphonate exposure: Clinical course and outcomes. J Oral
Maxillofac Surg. 70:1844–1853. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ruggiero SL, Carlson ER and Assael LA:
Comprehensive review of bisphosphonate therapy: Implications for
the oral and maxillofacial surgery patient. J Oral Maxillofac Surg.
67(Suppl 5): S12009. View Article : Google Scholar
|
|
27
|
Arco A, Favaloro A, Gioffrè M, Santoro G,
Speciale F, Vermiglio G and Cutroneo G: Sarcoglycans in the normal
and pathological breast tissue of humans: An immunohistochemical
and molecular study. Cells Tissues Organs. 195:550–562. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hynes RO: Integrins: Versatility,
modulation and signaling in cell adhesion. Cell. 69:11–25. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Trimarchi F, Favaloro A, Fulle S, Magaudda
L, Puglielli C and Di Mauro D: Culture of human skeletal muscle
myoblasts: Timing appearance and localization of
dystrophin-glycoprotein complex and vinculin-talin-integrin
complex. Cells Tissues Organs. 183:87–98. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Cankaya AB, Erdem MA, Isler SC, Demircan
S, Soluk M, Kasapoglu C and Oral CK: Use of Cone-Beam Computerized
Tomography for Evaluation of Bisphosphonate-Associated
Osteonecrosis of the Jaws in an Experimental Rat Model. Int J Med
Sci. 8:667–672. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ali-Erdem M, Burak-Cankaya A, Cemil-Isler
S, Demircan S, Soluk M, Kasapoglu C and Korhan-Oral C: Extraction
socket healing in rats treated with bisphosphonate: Animal model
for bisphosphonate related osteonecrosis of jaws in multiple
myeloma patients. Med Oral Patol Oral Cir Bucal. 16:879–883. 2011.
View Article : Google Scholar
|
|
32
|
Murakami H, Takahashi N, Sasaki T, Udagawa
N, Tanaka S, Nakamura I, Zhang D, Barbier A and Suda T: A possible
mechanism of the specific action of bisphosphonates on osteoclasts:
Tiludronate preferentially affects polarized osteoclasts having
ruffled borders. Bone. 17:137–144. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Biver E, Vieillard MH, Cortet B, Salleron
J, Falgayrac G and Penel G: No anti-angiogenic effect of clinical
dosing regimens of a single zoledronic acid injection in an
experimental bone healing site. Bone. 46:643–648. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tanaka Y, Nagai Y, Dohdoh M, Oizumi T,
Ohki A, Kuroishi T, Sugawara S and Endo Y: In vitro cytotoxicity of
zoledronate (nitrogen-containing bisphosphonate: NBP) and/or
etidronate (non-NBP) in tumour cells and periodontal cells. Arch
Oral Biol. 58:628–637. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lustosa-Pereira A, Garcia RB, de Moraes
IG, Bernardineli N, Bramante CM and Bortoluzzi EA: Evaluation of
the topical effect of alendronate on the root surface of extracted
and replanted teeth. Microscopic analysis on rats' teeth. Dent
Traumatol. 22:30–35. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lekic P, Rubbino I, Krasnoshtein F,
Cheifetz S, McCulloch CA and Tenenbaum H: Bisphosphonate modulates
proliferation and differentiation of rat periodontal ligament cells
during wound healing. Anat Rec. 247:329–340. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yoshida M and Ozawa E: Glycoprotein
complex anchoring dystrophin to sarcolemma. J Biochem. 108:748–752.
1990.PubMed/NCBI
|
|
38
|
Ervasti JM and Campbell KP: A role for the
dystrophin-glycoprotein complex as a transmembrane linker between
laminin and actin. J Cell Biol. 122:209–231. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Campbell KP: Three muscular dystrophies:
Loss of cytoskeleton-extracellular matrix linkage. Cell.
80:675–679. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
American Association of Oral and
Maxillofacial Surgeons (AAOMS): Office Anesthesia Evaluation Manual
(8th). AAOMS, Rosemont, IL, USA: 1899–1900. 2011.
|