Introduction
Age-related macular degeneration (AMD) is the most
common cause of blindness in the elderly population (1). Accompanied by retinal pigment
epithelial detachment and macular hemorrhage, AMD is mainly caused
by regional perfusion disturbance of the central fovea-supplying
vessels and metabolite accumulation (2), which seriously affects the quality of
life of the elderly population. Many studies worldwide (3,4) have
found that vascular endothelial growth factor (VEGF) is directly
related to the occurrence of AMD and anti-VEGF drug treatment is an
important method for AMD. Anti-VEGF drugs can hinder the progress
of AMD, but exert limited effects on optimizing visual function
(5).
Photodynamic therapy (PDT) has been proved to be
effective in the treatment of neovascular AMD (6), but the expression of angiogenesis
factor increased after treatment, which may worsen the recovery of
visual acuity (7). A combined
treatment of anti-VEGF and PDT can break the limitation of a single
treatment and may become the recommended combined treatment method
in the future (8). This study uses
anti-VEGF drugs combined with PDT to treat patients with AMD with a
focus on changes in vision, visual field defects and hemodynamic
parameters of optical fundus blood vessels after treatment, and
thus, provided a reference basis for clinical treatment.
Materials and methods
Sample selection
Ninety-six cases (192 eyes) of patients that were
diagnosed with AMD at the The First Affiliated Hospital of
Zhengzhou University (Henan, China) from January 2013 to January
2016 were selected continuously. Inclusion criteria for the study
were: i) Diagnosis of macular degeneration through fundus
fluorescein angiography or optical coherence tomography (OCT); ii)
age ≥60 years; iii) being administered treatment for the first
time; iv) informed consent was obtained from patients and family
members; and v) complete clinical data. The exclusion criteria
were: History of eye trauma, surgical history and other retinal
diseases. According to therapeutic methods, patients were randomly
divided into teh observation and control groups, with 48 cases (96
eyes) in each group. The control group had 25 cases of males and 23
cases of females aged from 62 to 76 years with an average of
69.3±5.2 years. There were 31 cases of dry AMD and 17 cases of wet
AMD. Twenty cases of patients had comorbidity of hypertension and
10 cases had diabetes. The observation group was composed of 26
males and 22 females aged from 61 to 77 years, with an average of
69.5±5.6 years. There were 30 cases of dry AMD and 18 cases of wet
AMD. Twenty-two cases of patients had comorbidity with hypertension
and 8 cases had diabetes.
Therapeutic methods
The patients in control group were administered
anti-VEGF drug treatment, intravitreal injection of Lucentis at a
dose of 0.5 mg/0.05 ml. The injection was repeated once every other
month for 3 months.
The patients in the observation group were treated
with anti-VEGF drugs combined with PDT, with a dose of 6
mg/m2 verteporfin. Ten minutes after intravenous
injection, a laser [with a wavelength of 689 nm, an intensity of
600 mW·cm2 and an optical density (OD) of 50
J/cm2] was used to directly radiate the retinal lesion
area of patients through contact lens for 83 sec. The affected eyes
were kept out of the sun for 5 days after treatment. Lucentis (0.5
mg/0.05 ml) was administered through an intravitreal injection
within 3 days after PDT treatment. If bleeding was present, and
typical retina angiogenesis and retina hydrops continued to exist
in the re-examination after treatment, then intravitreal injection
of isodose Lucentis was administered again.
Observation indexes
The best corrected visual acuity was examined before
treatment as well as 1 week, 1 and 6 months after treatment. The
international standard visual acuity chart was used, according to
which improved vision meant that the corrected visual acuity
increased by over 2 lines, decreased vision meant that the
corrected visual acuity decreased by over 2 lines, and unchanged
vision meant that the vision change was within 1 line. For vision
<0.1, the change in vision of 0.02 was counted as 1 line.
The eye hemodynamic parameters used a color Doppler
ultrasound instrument (model iE33; Philips Medical Systems,
Andover, MA, USA) with the probe frequency of 11 MHz and sampling
volume of 2–3 mm. Patients were placed in a supine position with
slightly closed eyes. The probe slightly touched the upper eyelid
to conduct horizontal scanning. The dark area of the optic nerve
was displayed on the screen. The pulsed Doppler flow spectrum of
retrobulbar optic nerve bitamporal PCA was detected. The peak
systolic velocity (PSV) of the ophthalmic artery, arterial end
diastolic velocity (EDV), arterial resistance index (RI) and
pulsatility index (PI) were recorded. Central foveal thickness
(CFT) and visual field parameters were detected by OCT, including
the mean sensitivity (MS) within the central vision field scope of
10° as well as MS and mean defect (MD) within the scope of 4°.
Statistical analysis
The data in this study were analyzed using SPSS 23.0
(SPSS, Inc., Chicago, IL, USA) statistical software. Measurement
data are expressed as mean ± standard deviation after normality
test. Independent-samples t-test was applied. Analysis of variance
(ANOVA) was applied for repeated measures data. Enumeration data
were expressed as ratio and verified by χ2 test.
P<0.05 was considered to indicate a statistically significanct
difference.
Results
Comparison of vision improvement
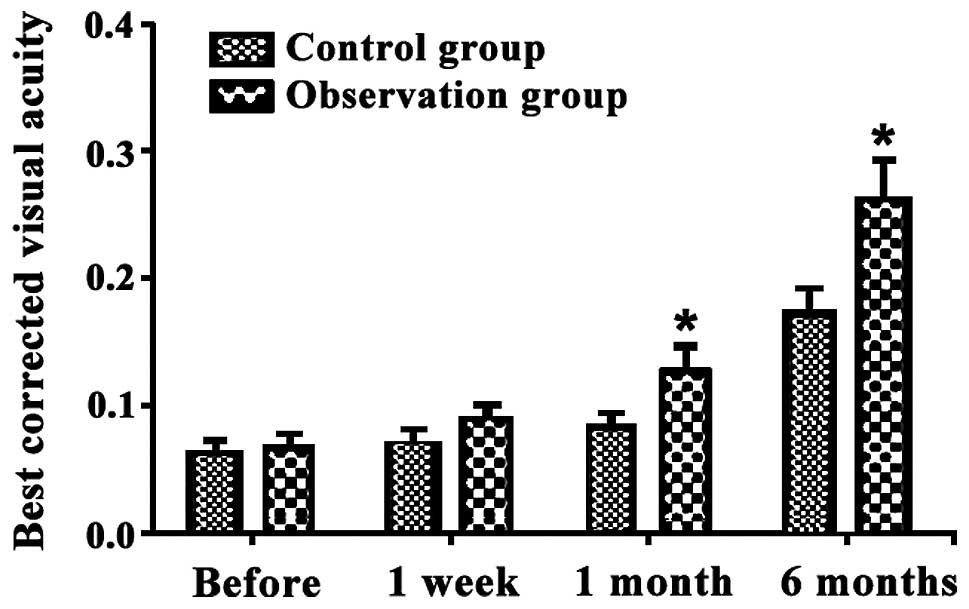
After treatment, the best corrected visual acuity of
patients in the two groups increased gradually. Within 1 and 6
months post-operation, the best corrected visual acuity of patients
in the observation group was significantly higher than that of the
control group. Differences were statistically significant
(P<0.05) (Fig. 1).
The ratio of vision improvement in observation group
was higher than that of control group within 1 and 6 months after
treatment, and the difference was statistically significant
(P<0.05) (Table I).
 | Table I.Comparison of vision improvement
within 1 and 6 months after treatment (cases, %). |
Table I.
Comparison of vision improvement
within 1 and 6 months after treatment (cases, %).
|
|
| 1 month after
treatment | 6 months |
|---|
|
|
|
|
|
|---|
| Groups | Eyes | Improved vision | Unchanged vision | Decreased vision | Improved vision | Unchanged vision | Decreased vision |
|---|
| Observation | 96 | 69 (71.9) | 20 (20.8) | 7 (7.3) | 82 (85.4) | 9 (9.4) | 5 (5.2) |
| Control | 96 | 50 (52.1) | 33 (34.4) | 13 (13.5) | 65 (67.7) | 21 (21.9) | 10 (10.4) |
| χ2
test |
|
| 8.022 |
|
| 8.433 |
|
| P-value |
|
| 0.018 |
|
| 0.015 |
|
Comparison of ocular hemodynamic
parameters
Detection through color Doppler ultrasound within 6
months after treatment showed that the PSV and EDV values of the
PCA of the observation group were higher than those of the control
group. The RI and PI values of the observation group were lower
than those of the control group. Differences were statistically
significant (P<0.05) (Table
II).
 | Table II.Comparison of ocular hemodynamic
parameter values after treatment. |
Table II.
Comparison of ocular hemodynamic
parameter values after treatment.
| Groups | PSV (cm/sec) | EDV (cm/sec) | RI | PI |
|---|
| Observation | 10.81±1.63 | 4.83±0.51 | 0.54±0.06 | 1.12±0.13 |
| Control | 8.34±0.92 | 3.92±0.41 | 0.63±0.07 | 1.31±0.17 |
| t-test | 4.383 | 4.293 | 5.012 | 5.172 |
| P-value | 0.035 | 0.037 | 0.027 | 0.023 |
Comparison of CFT and visual field
parameters
Within 6 months after treatment, the CFT value of
the observation group was lower than that of the control group. In
addition, the MS values of visual field parameter 10° and 4° of the
observation group were higher than those of the control group.
Finally, the absolute value of MD in the observation group was
lower than that of the control group. Differences were
statistically significant (P<0.05) (Table III).
 | Table III.Comparison of CFT and visual field
parameters. |
Table III.
Comparison of CFT and visual field
parameters.
| Groups | CFT (µm) | 10° MS (dB) | 4° MS (dB) | MD (dB) |
|---|
| Observation | 261.29±29.34 | 24.58±2.91 | 23.18±2.49 | −6.73±0.73 |
| Control | 295.47±32.15 | 21.17±2.64 | 20.35±2.63 | −10.14±0.92 |
| t-test | 5.342 | 5.495 | 5.124 | 5.372 |
| P-value | 0.020 | 0.018 | 0.024 | 0.019 |
Discussion
Lucentis can reduce the leakage of fundus choroidal
neovascularization (CNV) and alleviate macular edema, which lead to
notable effects in the maintenance of present vision acuity
(9). Treatment of neovascular AMD by
PDT can retard the central light loss caused by CNV (10).
The most visible clinical manifestation of AMD is
the diminution of vision. The best corrected visual acuity is a
reliable standard of measuring the eye function and vision of
patients. It is generally recognized that the higher the best
corrected visual acuity is, the better the holistic vision
conditions are (11). This study
concluded that the best corrected visual acuity of patients in the
two groups increased gradually after treatment, but the observation
group had a significantly higher improvement than the control group
within 1 and 6 months after operation. The proportion of vision
improvement in the observation group was higher than that of the
control group within 1 and 6 months, and the differences were
statistically significant. Thus, it can be discerned that anti-VEGF
drugs combined with PDT lead to significant therapeutic effects.
VEGF can cause damage to the function of the blood-retinal barrier,
and therefore, directly participates in the occurrence and
development of CNV which leads to macular oedema and visual
impairment. Intravitreal injection of Lucentis plays a role through
the inhibition of angiogenesis by drug use with high local
concentration (12). PDT leads to
the direct coagulation necrosis of CNV through the intravenous
injection of photosensitive drugs, which gather at a local part of
CNV and are activated by low intensity laser (13). Although anti-VEGF drugs can reduce
the formed CNV leakage, they lack targeting and cannot block CNV
completely (14). PDT can damage the
CNV framework that is insensitive to anti-VEGF drugs. Combined with
Lucentis, PDT can enlarge the CNV blocking degree and prevent any
further damage to vision (15). The
simple Lucentis intravitreal injection needs to be repeated many
times to achieve an ideal effect, during which it can result in
amotio retinae, increase of intra-ocular pressure, traumatic
cataracts and other ocular complications (16). After combination therapy, the times
of Lucentis injection decreases and the occurrence rate of ocular
complications decreases under the premise of inhibiting
neovascularization and protecting vision, which may be an important
reason for improving holistic therapeutic effects of patients
(17).
The root cause of vision improvement of AMD lies in
the sealing of CNV and the recovery of haemodynamics of normal
ocular fundus (18). The results of
this study showed that when detected by color Doppler ultrasound
within 6 months after treatment, the PSV and EDV values of PCA of
the observation group were higher than those of control group. In
addition, the RI and PI values of observation group were lower than
those of the control group. The differences were statistically
significant. The choriocapillaris of the macular area are dominated
by PCA and the regional perfusion disturbance and CNV formation can
cause arteriosclerosis and disorders of the choroidea and retina
cycles (19). PSV reflects the
degree of angioplerosis and the intensity of blood supply; EDV
reflects the blood perfusion state at the distal end of tissue. The
higher the PSV and EDV are, the more sufficient the blood supply is
(20). RI and PI reflect the blood
flow resistance of blood vessels and are negatively related to
vascular compliance (21). The
results demonstrated that anti-VEGF drugs, combined with PDT, can
optimize blood flow state, which is the fundamental mechanism
behind vision changes in patients.
Poor blood supply of the macular area can directly
cause macular oedema, the increase of CFT as well as the decreased
visual acuity of the macular center and its vicinity (22). The results of this study showed that,
within 6 months after treatment, the CFT value of the observation
group was lower than that of the control group, the MS values of
visual field parameter 10° and 4° of the observation group were
higher than those of the control group, and the absolute value of
MD of the observation group was lower than that of control group.
The differences were statistically significant. It showed that the
improvement of blood supply to the macular area could alleviate
edema of the macular center and decrease CFT value; increased blood
supply to the macular area could also directly optimize retinal
function in order to improve visual acuity (23).
In conclusion, anti-VEGF drugs, combined with PDT,
can optimize the overall vision of patients with AMD, improve
hemodynamic parameters and reduce visual field defects, and may
therefore, be highly valuable in clinical application.
References
|
1
|
Cho HJ, Kim KM, Kim HS, Lee DW, Kim CG and
Kim JW: Response of pigment epithelial detachment to anti-vascular
endothelial growth factor treatment in age-related macular
degeneration. Am J Ophthalmol. 166:112–119. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ueda K, Zhao J, Kim HJ and Sparrow JR:
Photodegradation of retinal bisretinoids in mouse models and
implications for macular degeneration. Proc Natl Acad Sci USA.
113:6904–6909. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Novais EA, Badaró E, Hirai FE, Jorge FA,
Leal P, Farah ME and Rodrigues EB: Daily optical coherence
tomography examinations after first antivascular endothelial growth
factor injections: an interventional case series. J Ophthalmol.
2016:69718312016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Heimes B, Gunnemann F, Ziegler M,
Gutfleisch M, Spital G, Pauleikhoff D and Lommatzsch A: Compliance
of age related macular degeneration patients undergoing anti-VEGF
therapy: analysis and suggestions for improvement. Ophthalmologe.
6:Jun 6–2016.(In German) (Epub ahead of print).
|
|
5
|
Senra H, Ali Z, Balaskas K and Aslam T:
Psychological impact of anti-VEGF treatments for wet macular
degeneration-a review. Graefes Arch Clin Exp Ophthalmol. 4:12–13.
2016.
|
|
6
|
Arias L, Gómez-Ulla F and Ruiz-Moreno JM:
Ranibizumab in monotherapy and combined with photodynamic therapy
for retinal angiomatous proliferation. Clin Ophthalmol. 10:861–869.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wu B, Li J, Lin H and Wu H: Different
strategies for the treatment of age-related macular degeneration in
China: an economic evaluation. J Ophthalmol. 2016:76898622016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Scherer KM, Bisby RH, Botchway SW and
Parker AW: New approaches to photodynamic therapy from type I, II
and III to type IV using one or more photons. Anticancer Agents Med
Chem. 13:17–18. 2016.
|
|
9
|
Catchpole T, Daniels T, Perkins J and
Csaky KG: Method development to quantify Bv8 expression in
circulating CD11b+ cells in patients with neovascular
age-related macular degeneration (nvAMD) exhibiting anti-VEGF
refractoriness. Exp Eye Res. 148:45–51. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Otsuji T, Sho K, Tsumura A, Koike N,
Nishimura T and Takahashi K: Three-year results of a modified
photodynamic therapy procedure (Ironing PDT) for age-related
macular degeneration patients with large lesions. Clin Ophthalmol.
10:431–436. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Arnold JJ: Age-related macular
degeneration: anti-vascular endothelial growth factor treatment.
BMJ Clin Evid. 24:07012016.
|
|
12
|
Uzun S and Pehlivan E: Comparison of
intravitreal aflibercept and ranibizumab injections on subfoveal
and peripapillary choroidal thickness in eyes with neovascular
age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol.
2:15–16. 2016.
|
|
13
|
Teper SJ, Nowinska A, Pilat J and Wylegala
E: Photodynamic therapy in VEGF inhibition
non-responders-pharmacogenetic study in age-related macular
degeneration assessed with swept-source optical coherence
tomography. Photodiagn Photodyn Ther. 13:108–113. 2016. View Article : Google Scholar
|
|
14
|
Lee JP, Park JS, Kwon OW, You YS and Kim
SH: Management of acute submacular hemorrhage with intravitreal
injection of tenecteplase, anti-vascular endothelial growth factor
and gas. Korean J Ophthalmol. 30:192–197. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Newman DK: Photodynamic therapy: current
role in the treatment of chorioretinal conditions. Eye (Lond).
30:202–210. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
MacDonald DA, Martin J, Muthusamy KK, Luo
JK, Pyles E, Rafique A, Huang T, Potocky T, Liu Y, Cao J, et al:
Aflibercept exhibits VEGF binding stoichiometry distinct from
bevacizumab and does not support formation of immune-like
complexes. Angiogenesis. 19:389–406. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Colombeau L, Acherar S, Baros F, Arnoux P,
Gazzali AM, Zaghdoudi K, Toussaint M, Vanderesse R and Frochot C:
Inorganic nanoparticles for photodynamic therapy. Top Curr Chem.
370:113–134. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shahin M, Gad MA and Hamza W: Impact of
intravitreal triamcinolone acetonide versus intravitreal
bevacizumab on retrobulbar hemodynamic in patients with diabetic
macular edema. Cutan Ocul Toxicol. 33:49–53. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Toklu Y, Cakmak HB, Raza S, Anayol A, Asik
E and Simşek S: Short-term effects of intravitreal bevacizumab
[Avastin®] on retrobulbar hemodynamics in patients with
neovascular age-related macular degeneration. Acta Ophthalmol.
89:e41–e45. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mete A, Saygili O, Mete A, Bayram M and
Bekir N: Effects of intravitreal bevacizumab (Avastin) therapy on
retrobulbar blood flow parameters in patients with neovascular
age-related macular degeneration. J Clin Ultrasound. 38:66–70.
2010.PubMed/NCBI
|
|
21
|
Sakalar YB, Senturk S, Yildirim M,
Keklikci U, Alakus MF and Unlu K: Evaluation of retrobulbar blood
flow by color doppler ultrasonography after intravitreal
ranibizumab injection in patients with neovascular age-related
macular degeneration. J Clin Ultrasound. 41:32–37. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Koizumi H, Kano M, Yamamoto A, Saito M,
Maruko I, Kawasaki R, Sekiryu T, Okada AA and Iida T: Short-term
changes in choroidal thickness after aflibercept therapy for
neovascular age-related macular degeneration. Am J Ophthalmol.
159:627–633. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Smith RT: New understanding of age-related
macular degeneration through quantitative autofluorescence. JAMA
Ophthalmol. 134:824–826. 2016. View Article : Google Scholar : PubMed/NCBI
|