Introduction
Splenogonadal fusion (SGF) is a rare congenital
malformation. The condition was first described in 1883, but fewer
than 200 cases have been reported to date (1). Only a few cases have been diagnosed
preoperatively, which were typically regarded as cryptorchidism,
testicular tumors or inguinal hernia, and accidentally determined
to be SGF after exposure of the inguinal canal during surgery
(2). This disease commonly leads to
a preoperative misdiagnosis of testicular cancer, causing testes to
be mistakenly removed in nearly a third of SGF cases (3,4). In
order to avoid these errors, increased awareness of the diagnosis
of and treatment for SGF therefore is required. In this case
report, we summarize our experiences of treating SGF and review the
literature to improve the understanding of this disease and provide
helpful suggestions for future treatment strategies.
Case report
A 4-year-old boy presented to the Department of
Pediatric Surgery, West China Hospital of Sichuan University
(Chengdu, China) with bilateral undescended testes from birth in
April 2013. Physical examination indicated that the bilateral
scrota were empty, the testes were also not present in the inguinal
region, and the patient's penis was normal. An ultrasound confirmed
that there were no testicular masses in the bilateral scrota and
inguinal regions. In accordance with the above clinical findings,
the patient was diagnosed with bilateral cryptorchidism, and
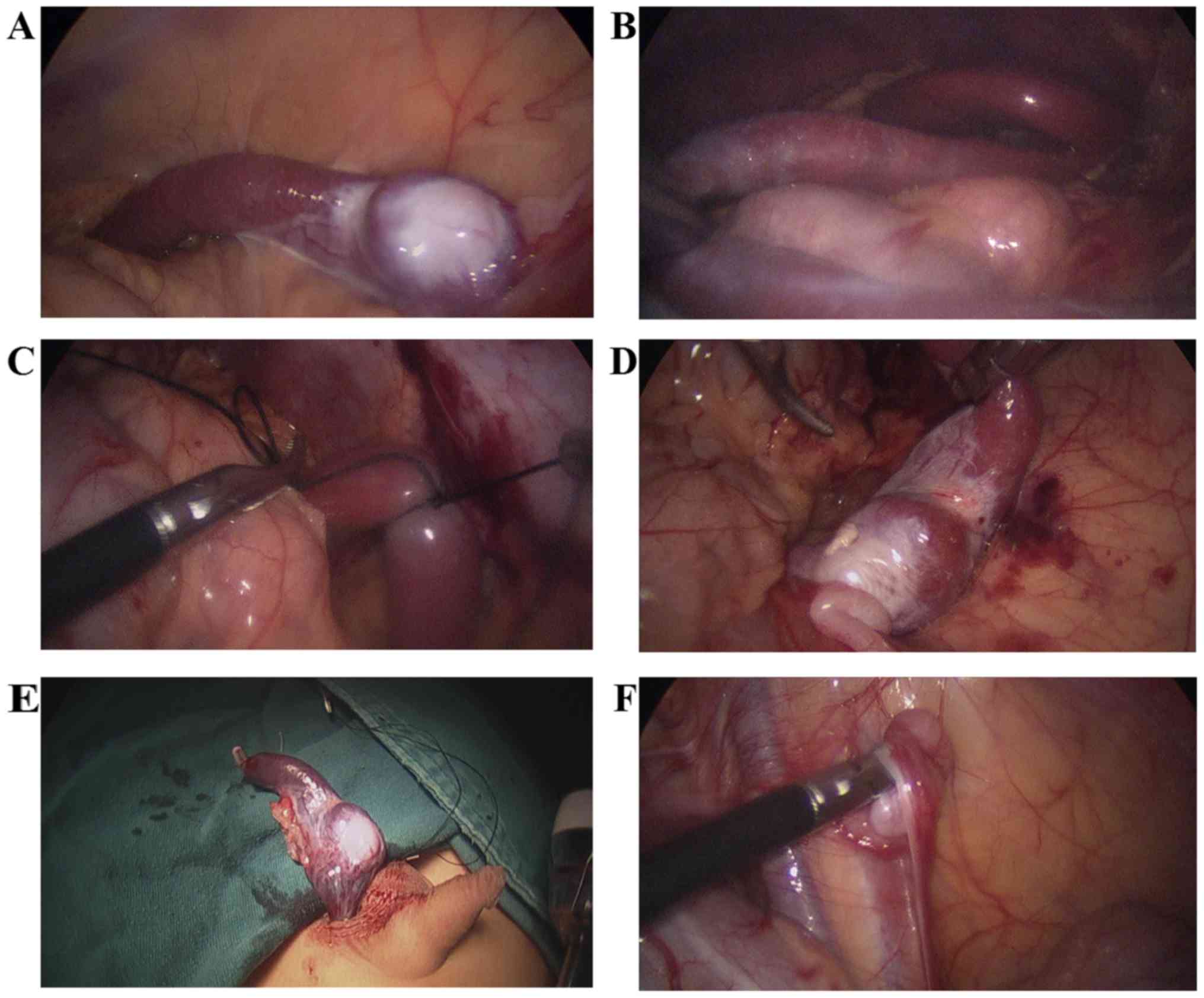
therefore laparoscopic gonad exploration was performed. Complete
abdominal exploration revealed gonad-like tissue connected with a
smooth, fleshy, brown, cord-like structure beside the left colon,
but left spermatic cord blood vessels were not observed. The
cord-like structure was connected to the spleen (which was normal),
and was approximately 5–6 cm long and 1.5 cm in diameter (Fig. 1A and B). The spleen cord was cut off
and the gonad-like tissues were pulled down into the scrotum
through the inguinal canal (Fig.
1C-E). A small incision was made in the scrotum skin to expose
the gonad-like tissue. A small piece of gonad-like tissue was
harvested for pathological examination. The result of pathological
examination demonstrated that the gonad-like tissue was a normal
testis. As a result, the spleen cord was resected and
Fowler-Stephens orchidopexy was implemented. The right testicle was
located in the right iliac fossa, 2 cm from the right deep inguinal
ring. The right spermatic cord was short and the testis exhibited
dysplasia. The right testicle was moved posteriorly and fixed by
single-stage laparoscopic Fowler-Stephens orchidopexy (Fig. 1F). Postoperatively, the patient
recovered well. At a 6-month follow-up in the Outpatient Department
of Pediatric Surgery, West China Hospital of Sichuan University
physical examination revealed that the right testis was normal;
however, the left scrotum demonstrated swelling and the internal
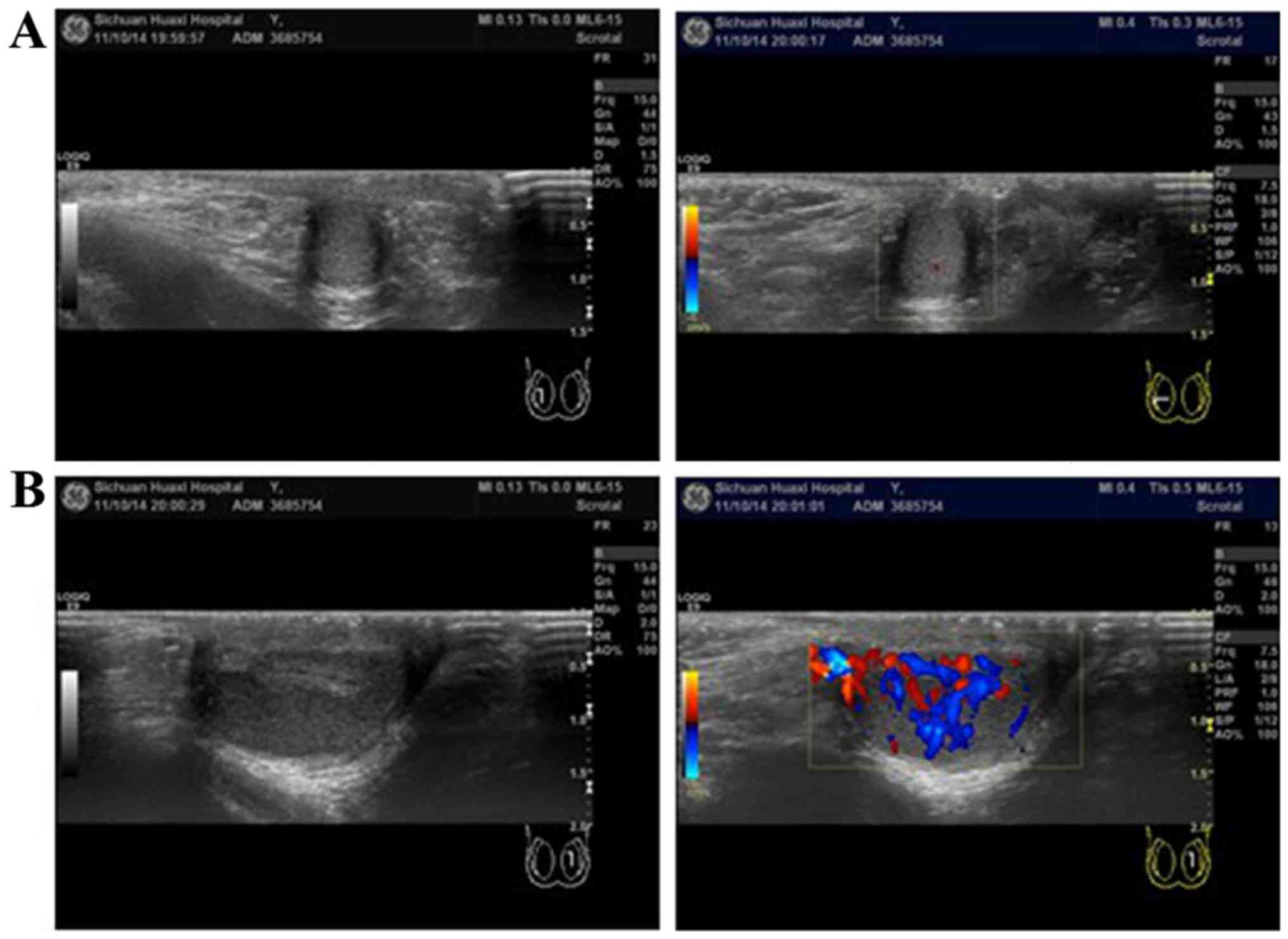
contents were hard. An ultrasound of this testicle indicated
non-uniform, splenic-like organization, with abundant blood flow
and a reduction in the testicular size (Fig. 2). We will continue to follow-up this
patient; if hyperplasia of the splenic tissue in the scrotum is
detected during a subsequent follow-up, a reoperation will be
performed. At one-year follow-up, the volume of splenic-like
organization was reduced but the testicular size did not exhibit
further atrophy, thus reoperation has not been performed. We will
continue to follow-up this patient.
Discussion
SGF is a rare congenital malformation, which was
first reported in 1883 by Bostroem (1,3) and
Pommer made a detailed report in 1889 (5). However, there have been fewer than 200
cases worldwide since the disease was first described (1). With regard to diagnoses, 70% of
patients are <20 years old when diagnosed and 50% are <10
years old. There are more male than female cases, at a ratio of
16.6:1 (6). In 1956, Putschar and
Manion (7) divided the disease into
two types: Continuous and discontinuous. Continuous type indicates
a cord-like tissue (spleen tissue or fibrous tissue) directly
connecting the gonad and spleen, whereas discontinuous type
indicates gonad tissue fused with ectopic accessory spleen but
there is no connection between the ectopic accessory spleen and
principal spleen (1,2,8). The
present case is an example of continuous SGF. Previous studies
indicate that the frequency of the two types is equal (5), but other studies suggest that the
frequency of discontinuous type SGF was lower than that of
continuous SGF (2,8,9).
The exact cause of SGF remains unknown, but it is
generally believed to occur prior to gonad decline, between 5–8
weeks of pregnancy (10). During
embryogenesis, the epithelial cells of the body cavity and the
intestinal cells form the spleen in the dorsal intestine.
Simultaneously, during rotation, the spleen is close to the gonads.
The rotation process may therefore lead to fusion of the two. The
gonads begin to decline at 8 weeks after gestation. If the gonad
and spleen are fused at this time, the partial splenic tissue
adhered to the gonad would descend with the gonads, so the splenic
tissue may appear in any location of the primordial gonad's descent
path, even in the inguinal canal or within the scrotum (8,10,11).
Almost all previous cases of SGF (98%) occurred on
the left side (2), often accompanied
by left cryptorchidism, short limb malformation and a small jaw. In
addition, it may also present as bilateral cryptorchidism,
hypospadias, anal malformation and diaphragmatic hernia (8,9,11). Complications occurring in continuous
type SGF are 5 times more frequent than in discontinuous type SGF
(8). Only a few cases have been
diagnosed preoperatively, usually due to cryptorchidism, testicular
tumors or inguinal hernia (4); most
are reported following exposure of the inguinal canal during
surgical treatment (2,3,11).
According to a previous study, approximately 30% of cases reporting
scrotal swelling are misdiagnosed as testicular tumors and result
in unnecessary orchiectomy (3). A
few cases have presented as emergencies, with symptoms such as
orchitis and testicular torsion or trauma. Hines and Eggum
(12) reported a case of intestinal
obstruction caused by the pressure of the splenic tissue in a
continuous type SGF patient. However, there have also been a few
cases diagnosed preoperatively by ultrasound, computed tomography
or magnetic resonance imaging (6,9,13). Most cases of SGF reported by such
imaging examination were continuous SGF, demonstrating a tubular
structure fused with the testicles (8,9,11). In the current case, the patient
presented with bilateral cryptorchidism but with no other
abnormalities. A clear diagnosis was not made prior to surgery.
Perioperative frozen pathological examination aids exclusion of the
possibility of testicular tumors and avoiding orchiectomy because
of misdiagnosis.
Following the development of laparoscopic
techniques, an increase of SGF diagnosis is expected. For children
with cryptorchidism, if laparoscopic exploration does not indicate
the presence of testicular tissue in the deep inguinal ring and
iliac fossa, the paracolic sulci should be investigated to prevent
misdiagnosis.
When SGF diagnosis is apparent but asymptomatic, the
necessity of surgery is controversial. SGF may not increase the
risk of testicular cancer, but SGF often associates with
cryptorchidism, a risk factor for testicular cancer; as a result,
SGF indirectly increases the risk of testicular tumors (2,4). To date
only 4 cases of patients with SGF and testicular tumors have been
reported, and all of these presented with merged cryptorchidism
(2). Therefore, for patients with
combined cryptorchidism, testicular descent fixation appears to be
the most appropriate therapeutic option. There is disagreement as
to whether the splenic tissue adhering to the testis should be
completely removed or not. Our team of surgeons hold the belief
that the tissue should not be completely eliminated, therefore this
protocol was followed. In the present case, it was suggested that
testicular blood supply would be affected if splenic tissue was
completely removed, so it was retained. At a 6-month follow-up, the
splenic tissue grew and the testicle became smaller. To the best of
our knowledge, whether splenic tissue hyperplasia causes
ipsilateral testicular atrophy is unknown. The currently described
patient may be subjected to a second surgery to resect splenic
tissue in the left scrotum. This has not yet occurred and the
patient is still being followed-up.
In conclusion, SGF is a rare disease, presenting
difficulty in diagnosis due to an absence of typical clinical
symptoms. This disease should be highlighted in order to avoid the
misdiagnosis of testicular tumors and performing unnecessary
orchiectomies; laparoscopic exploration is therefore helpful in
diagnosis and treatment of patients with high cryptorchidism, and
perioperative frozen pathological examination may help eliminate
differential diagnosis of testicular tumors.
Acknowledgements
This work was supported by the Sichuan Province
foundation (grant no 2017SZ0060) of the Science and Technology
Department of Sichuan Province.
References
|
1
|
Jayasundara JA, Vithana VH and Lamahewage
AK: A case of continuous-type splenogonadal fusion. Singapore Med
J. 54:e123–e124. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lopes RI, de Medeiros MT, Arap MA, Cocuzza
M, Srougi M and Hallak J: Splenogonadal fusion and testicular
cancer: Case report and review of the literature. Einstein (Sao
Paulo). 10:92–95. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Karaman MI and Gonzales ET Jr:
Splenogonadal fusion: Report of 2 cases and review of the
literature. J Urol. 155:309–311. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sountoulides P, Neri F, Bellocci R, Schips
L and Cindolo L: Splenogonadal fusion mimicking a testis tumor. J
Postgrad Med. 60:202–204. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carragher AM: One hundred years of
splenogonadal fusion. Urology. 35:471–475. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Varma DR, Sirineni GR, Rao MV, Pottala KM
and Mallipudi BV: Sonographic and CT features of splenogonadal
fusion. Pediatr Radiol. 37:916–919. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Putschar WG and Manion WC: Splenicgonadal
fusion. Am J Pathol. 32:15–33. 1956.PubMed/NCBI
|
|
8
|
Bosnalı O, Cici İ, Moralıoğlu S and
Cerrah-Celayir A: Continuous-typ esplenogonadal fusion: Report of a
rare case. Turk J Pediatr. 56:680–683. 2014.PubMed/NCBI
|
|
9
|
Keyik B, Yanik B, Conkbayir I, Tuygun C,
Kizilgoz V and Hekimoğlu B: Continuous-type splenogonadal fusion
associated with an ipsilateral testicular atrophy: Sonographic
findings. J Clin Ultrasound. 38:161–163. 2010.PubMed/NCBI
|
|
10
|
Le Roux PJ and Heddle RM: Splenogonadal
fusion: Is the accepted classification system accurate? BJU Int.
85:114–115. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chiaramonte C, Siracusa F and Li Voti G:
Splenogonadal fusion: A genetic disorder?-report of a case and
review of the literature. Urol Case Rep. 2:67–69. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hines JR and Eggum PR: Splenic-gonadal
fusion causing bowel obstruction. Arch Surg. 83:887–889. 1961.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Croxford WC, Pfistermuller KL, Scott F and
Pope AJ: Splenogonadal fusion presenting clinically and
radiologically as a seminoma. Urol Case Rep. 3:204–205. 2015.
View Article : Google Scholar : PubMed/NCBI
|