Introduction
Permanent eyeliner tattoo application is a cosmetic
periocular procedure that is increasing in popularity. However, it
may encounter technical complications, such as pigment fanning,
improper pigment placement, pigment migration and, on rare
occasions, functional damage of the eyelid margin (1,2). Diffuse
lamellar keratitis (DLK) is a common complication that may occur
following laser-assisted in situ keratomileusis (LASIK)
surgery, and is characterized by an inflammatory cellular response
at the interface (2). However,
limited cases of uveitis triggered by tattoo-related inflammation
have been reported (3). Furthermore,
little is known about ocular surface alterations and DLK resulting
from permanent eyeliner tattoo treatment.
To the best of our knowledge, the present case
report is the first to describe a case of DLK with late-onset,
occurring 10 years after LASIK surgery, which was triggered by
permanent eyeliner tattoo treatment. The objective in the present
case report is to alert ophthalmologists to this complication of
permanent eyeliner tattoo treatment as the popularity of this
cosmetic procedure increases. Topical steroid therapy, artificial
tears, autologous serum eye drops and timely surgical intervention
are suggested to be important treatment options for patients with
DLK.
Case report
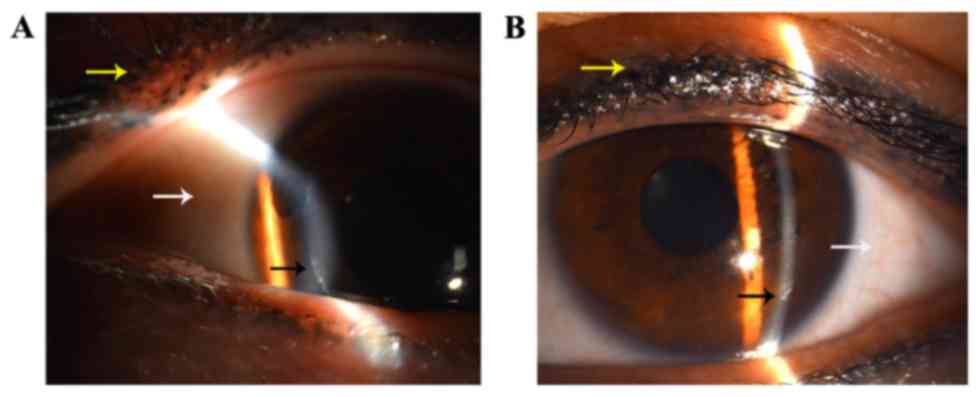
A 37-year-old Chinese woman developed pain and
severe foreign body sensation in both eyes 1 week after receiving
bilateral permanent eyeliner tattoo treatment (Fig. 1) and presented to the Department of
Ophthalmology, The First Hospital of Jilin University (Changchun,
China) in September 2015. The patient provided written informed
consent for her data to be used in this report. The patient's
ocular history indicated she had received bilateral LASIK surgery
10 years prior to the incident. The patient denied any recent
history of trauma and had no eye discomfort prior to the eyeliner
tattoo application. On examination, her best-corrected vision was
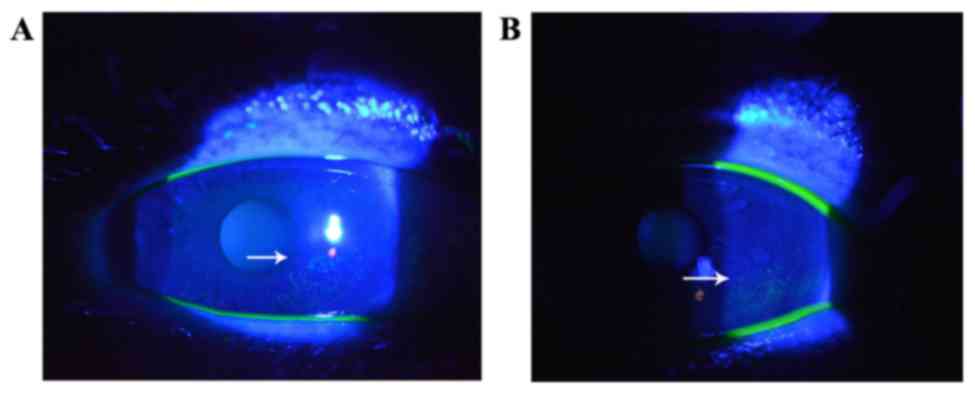
20/20 bilaterally. Slit-lamp biomicroscopy revealed mild
conjunctival congestion and punctate corneal epithelial erosions
(Fig. 2), and diffused fine granular
infiltrates precipitated around the edge of corneal flaps in both
eyes (Fig. 1). No inflammation in
the anterior chamber was observed. The remaining ophthalmic
examination was normal. Routine laboratory screening tests (routine
blood and urine tests, blood coagulation, liver function and kidney
function) were all within normal limits. The patient was diagnosed
with dry eye and DLK, and the patient was treated with topical 0.3%
tobramycin/0.1% dexamethasone, artificial tears and 20% autologous
serum three times per day.
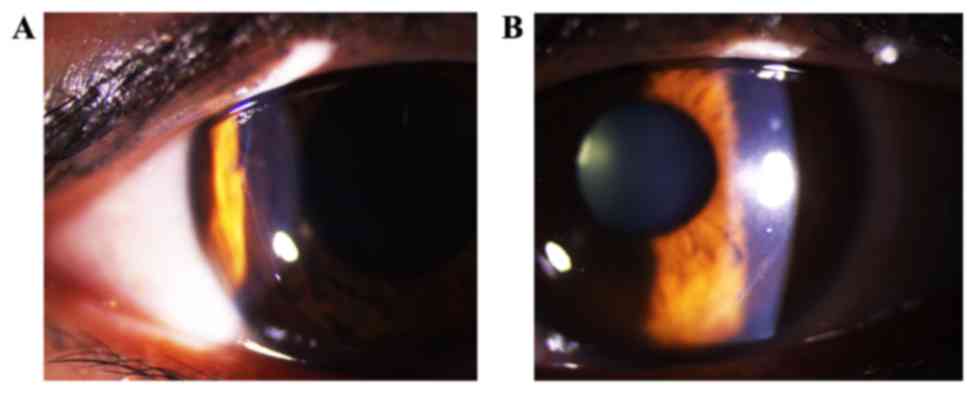
After 1 week of treatment, the punctate corneal
epithelial defects were resolved. However, epithelial ingrowth at
the corresponding corneal flap edge remained unchanged. Therefore,
the patient underwent surgery to remove the corneal epithelium
around the DLK lesion. Epithelial ingrowth at the corresponding
flap edge was no longer observed on the second postoperative day.
The topical steroidal medication (0.1% fluorometholone) was
gradually reduced over the next 3 weeks (three times a day for the
first week, twice a day for the second week, once a day for the
third week), while the artificial tears and autologous serum were
continued as before surgery. No recurrence of the disease was
detected during the 3-month observation period (Fig. 3).
Discussion
Permanent eyeliner tattoos have become increasingly
common; however, certain complications of such tattoos have been
reported in the ophthalmic literature (4). These include minor technical issues
such as misapplication of the pigment with resultant anterior
placement in the skin under the eyelashes, posterior placement in
mucocutaneous tissue, poor distribution of the pigment and pigment
fanning (4). More severe
complications, such as cilia loss, eyelid scarring and infections
have also been reported (4).
Permanent eyeliner tattoo application may cause instability of the
tear film and ocular surface disease through meibomian gland
dysfunction and loss (5). Therefore,
permanent eyeliner tattooing should be considered a risk factor for
ocular surface diseases. It has been suggested that a delayed
hypersensitivity reaction may occur secondary to localized immune
sensitization to a particular pigment (6). The association of DLK with permanent
eyeliner tattoo treatment is an unusual occurrence. To the best of
our knowledge, this is the first case report describing a case of
late-onset DLK, which was triggered by the application of a
permanent eyeliner tattoo.
DLK is a common complication of LASIK surgery, since
the creation of a flap provides a space in which cells are able to
accumulate (7). DLK is characterized
by diffused white, granular infiltrate around the edge of the
corneal flap (7) and typically
occurs within a few days after LASIK surgery. However, a previous
report described a case where DLK occurred 12 years after LASIK
surgery (8), although this is
considered to be extremely rare. The present case study is the
second case study to report late-onset DLK from LASIK surgery,
appearing 10 years after LASIK treatment. The findings of the
present case study and the previous study (8) indicate that DLK is able to manifest
after an extended period of time following LASIK surgery.
Although the precise mechanism of DLK has not been
fully elucidated, several possible etiologies, including peripheral
immune infiltrates, atopic disease, ocular inflammatory disease,
epithelial defects, bacterial endotoxins, chemicals or debris,
surgical gloves and meibomian gland secretions have been reported
(8,9). However, DLK resulting from permanent
eyeliner tattooing in a post-LASIK patient has not been reported
until now. Tattoo ink contains multiple coloring substances,
including copper, mercury, iron, chromium, titanium (10) and p-phenylenediamine (11), which may provoke delayed
hypersensitivity reactions (12).
Tattoo pigments are known to activate mast cells and may provoke
cellular lysis following phagocytosis (13). The histological appearance may vary
from diffused lymphohistiocytic infiltrate (14) to pseudolymphomatous reactions
(15), lichenoid reactions and
sarcoidal granulomas (16).
Intradermal injection of melanin, interphotoreceptor
retinoid-binding protein and S-antigen have been demonstrated to
produce severe posterior retinal uveitis (17). Cases of uveitis associated with
tattoo inflammation have also been described in the literature
(18–20). Tattoo-associated uveitis has been
reported to resolve following tattoo excision or immunosuppression
treatment with steroids, such as azathioprine or cyclosporine
(21), indicating that immune
reactions are involved in pigment-trigged uveitis. Although the
literature for allergic reactions as a risk factor of LASIK surgery
is limited, atopy has been suggested to be a patient-specific risk
factor for the development of DLK, a potentially severe side effect
following bilateral primary LASIK surgery (22). Previous studies have indicated that
DLK may be triggered by peripheral immune infiltrates (23,24).
Therefore, it is reasonable to postulate that the ink used in the
permanent eyeliner tattoo procedure in the present case included
chemicals that may provoke DLK. The underlying mechanism involved
may be regulated through activating a local immunoreaction
(25).
Although treatment recommendations for DLK have been
documented, no trials have determined the optimal treatments.
Mild-to-moderate inflammation is often treated with intensive
topical steroids, whereas severe inflammation is typically treated
by irrigating the interface and then administering intensive
topical steroids. Although the patient in the present case study
followed all of the doctor's instructions, the DLK did not improve.
Unresolved DLK may progress to disintegration of the flap, which
may lead to vision loss. Management of DLK includes lifting the
flap and reducing the inflammatory reaction by careful irrigation
of the bed and undersurface of the cap (22). In the present case, once the
epithelial debris of the lesion was surgically removed, DLK
improved markedly. The present findings indicate that when topical
steroids failed to treat DLK, timely surgical intervention combined
with topical steroids was a successful treatment. Artificial tears
and autologous serum were used as treatments in the present case.
Autologous serum has been demonstrated to be beneficial for corneal
epithelial recovery, and has been used to treat diseases of the
external eye, including keratoconjunctivitis sicca and persistent
epithelial defects (26).
In conclusion, the present case indicates that
permanent eyeliner tattoo treatment may serve as a potential
trigger of late-onset of DLK, which in the present patient occurred
10 years after LASIK surgery. Topical steroid therapy, artificial
tears, autologous serum eye drops and timely surgical intervention
are important factors to consider when treating patients with DLK.
Doctors should be aware of this complication associated with
permanent eyeliner tattoo treatment as the popularity of this
cosmetic procedure increases.
References
|
1
|
Hurwitz JJ, Brownstein S and Mishkin SK:
Histopathological findings in blepharopigmentation (eyelid tattoo).
Can J Ophthalmol. 23:267–269. 1988.PubMed/NCBI
|
|
2
|
Lin RT and Maloney RK: Flap complications
associated with lamellar refractive surgery. Am J Ophthalmol.
127:129–136. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Saliba N, Owen ME and Beare N:
Tattoo-associated uveitis. Eye (Lond). 24:14062010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vagefi MR, Dragan L, Hughes SM,
Klippenstein KA, Seiff SR and Woog JJ: Adverse reactions to
permanent eyeliner tattoo. Ophthal Plast Reconstr Surg. 22:48–51.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee YB, Kim JJ, Hyon JY, Wee WR and Shin
YJ: Eyelid tattooing induces meibomian gland loss and tear film
instability. Cornea. 34:750–755. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sperry K: Tattoos and tattooing. Part II:
Gross pathology, histopathology, medical complications, and
applications. Am J Forensic Med Pathol. 13:7–17. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gritz DC: LASIK interface keratitis:
Epidemiology, diagnosis and care. Curr Opin Ophthalmol. 22:251–255.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kamiya K, Ikeda T, Aizawa D and Shimizu K:
A case of late-onset diffuse lamellar keratitis 12 years after
laser in situ keratomileusis. Jpn J Ophthalmol. 54:163–164. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhao J, He L, Yao P, Shen Y, Zhou Z, Miao
H, Wang X and Zhou X: Diffuse lamellar keratitis after
small-incision lenticule extraction. J Cataract Refract Surg.
41:400–407. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Slater DN and Durrant TE: Tattoos: Light
and transmission electron microscopy studies with X-ray
microanalysis. Clin Exp Dermatol. 9:167–173. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bourra H and Hassam B: Contact dermatitis
after black henna tattoo. Pan Afr Med J. 14:1542013.(In French).
PubMed/NCBI
|
|
12
|
Shavit I, Hoffmann Y, Shachor-Meyouhas Y
and Knaani-Levinz H: Delayed hypersensitivity reaction from black
henna tattoo manifesting as severe facial swelling. Am J Emerg Med.
26:515. e3–e4. 2008. View Article : Google Scholar
|
|
13
|
England RW, Vogel P and Hagan L: Immediate
cutaneous hypersensitivity after treatment of tattoo with Nd:YAG
laser: A case report and review of the literature. Ann Allergy
Asthma Immunol. 89:215–217. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Blumental G, Okun MR and Ponitch JA:
Pseudolymphomatous reaction to tattoos. Report of three cases. J Am
Acad Dermatol. 6:485–488. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Taaffe A, Knight AG and Marks R: Lichenoid
tattoo hypersensitivity. Br Med J. 1:616–618. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Goldstein AP: VII. Histologic reactions in
tattoos. J Dermatol Surg Oncol. 5:896–900. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Moschos MM and Guex-Crosier Y: Retinal
vasculitis and cystoid macular edema after body tattooing: A case
report. Klin Monbl Augenheilkd. 221:424–426. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mansour AM and Chan CC: Recurrent uveitis
preceded by swelling of skin tattoos. Am J Ophthalmol. 111:515–516.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
McElvanney AM and Sherriff SM: Uveitis and
skin tattoos. Eye (Lond). 8:602–603. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Barabasi Z, Kiss E, Balaton G and Vajo Z:
Cutaneous granuloma and uveitis caused by a tattoo. Wien Klin
Wochenschr. 120:182008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jacob J and Van Calster J: Skin tattoos
and the development of uveitis. Acta Ophthalmol. 91:e650–e652.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bielory BP and O'Brien TP: Allergic
complications with laser-assisted in-situ keratomileusis. Curr Opin
Allergy Clin Immunol. 11:483–491. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ambrósio R Jr, Periman LM, Netto MV and
Wilson SE: Bilateral marginal sterile infiltrates and diffuse
lamellar keratitis after laser in situ keratomileusis. J Refract
Surg. 19:154–158. 2003.PubMed/NCBI
|
|
24
|
Singhal S, Sridhar MS and Garg P:
Bilateral peripheral infiltrative keratitis after LASIK. J Refract
Surg. 21:402–404. 2005.PubMed/NCBI
|
|
25
|
Liao JC, Proia AD, Ely PH and Woodward JA:
Late-onset melanopenic hypomelanosis as a complication of cosmetic
eyeliner tattoo. J Am Acad Dermatol. 69:e144–e146. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Poon AC, Geerling G, Dart JK, Fraenkel GE
and Daniels JT: Autologous serum eyedrops for dry eyes and
epithelial defects: Clinical and in vitro toxicity studies. Br J
Ophthalmol. 85:1188–1197. 2001. View Article : Google Scholar : PubMed/NCBI
|