Introduction
Cloacal exstrophy variants comprise a wide range of
disorders with four primary features: Omphalocele, bladder
exstrophy, an imperforate anus and spina bifida (1). The occurrence rate of cloacal exstrophy
variants is approximately 1/200,000–1/400,000 (2). No single environmental factor or
genetic defect in the etiology of cloacal exstrophy has been
identified (3,4). Many affected pregnancies are
terminated, while those that reach full term typically result in
infant mortality shortly after delivery (5,6). In most
countries, the disease is among the most severe congenital
anomalies, though increased survival rates have been observed with
improvements in neonatal care and surgical technique in countries
such as the USA (7,8). Prenatal differential diagnosis of
cloacal exstrophy from alternative urinary diseases is not well
studied. If the bladder is present, defects in the ventral wall may
not be visualized with prenatal ultrasound in certain conditions,
including oligohydramnios, and distinguishing cloacal exstrophy
from urorectal septum malformation sequence (URSMS) is challenging.
In order to improve the diagnosis of cloacal exstrophy, we describe
the misdiagnosis of a cloacal exstrophy variant as URSMS in a fetus
by ultrasound.
Case report
A 25-year-old woman (gravida, 4; para, 0; abortus,
2; ectopic, 1) was referred to Hubei Women and Children's Hospital
(Wuhan, Hubei) at 26 weeks of gestation due to oligohydramnios on
November 4, 2012. The patient reported vaginal bleeding that went
untreated at 50 days of gestation. She was not knowingly exposed to
teratogens prior to or during pregnancy and did not have a family
history of congenital disease. Sonography had been performed at
another hospital at 12 weeks of gestation and was normal.
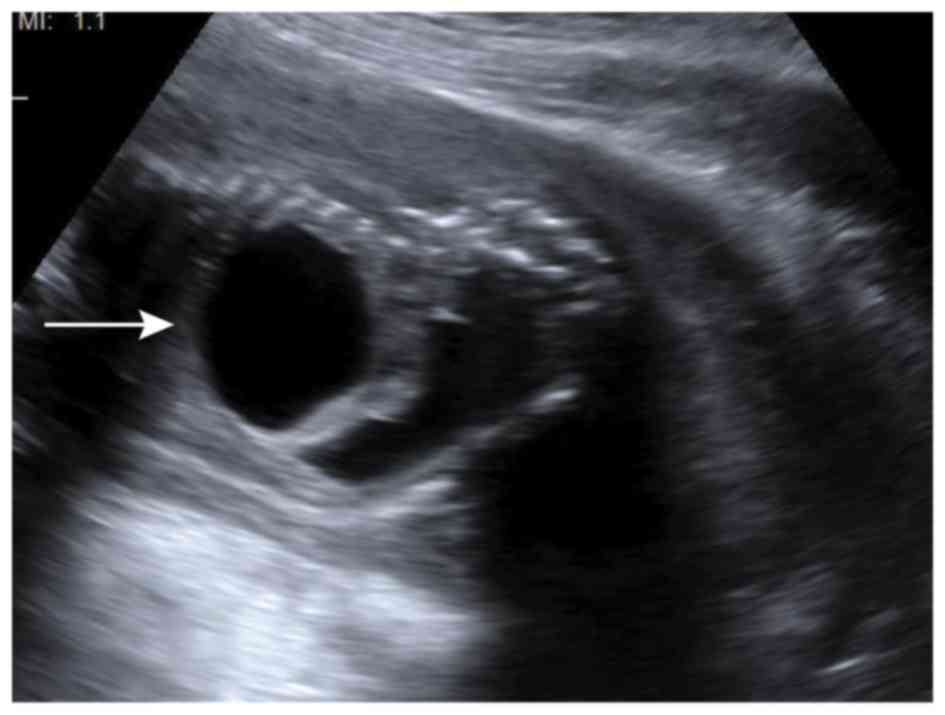
Conventional sonography revealed the fetus had a large of cyst
located on the right kidney (size, 2.1×2.0 cm; Fig. 1) and a left hypoplastic kidney (size,
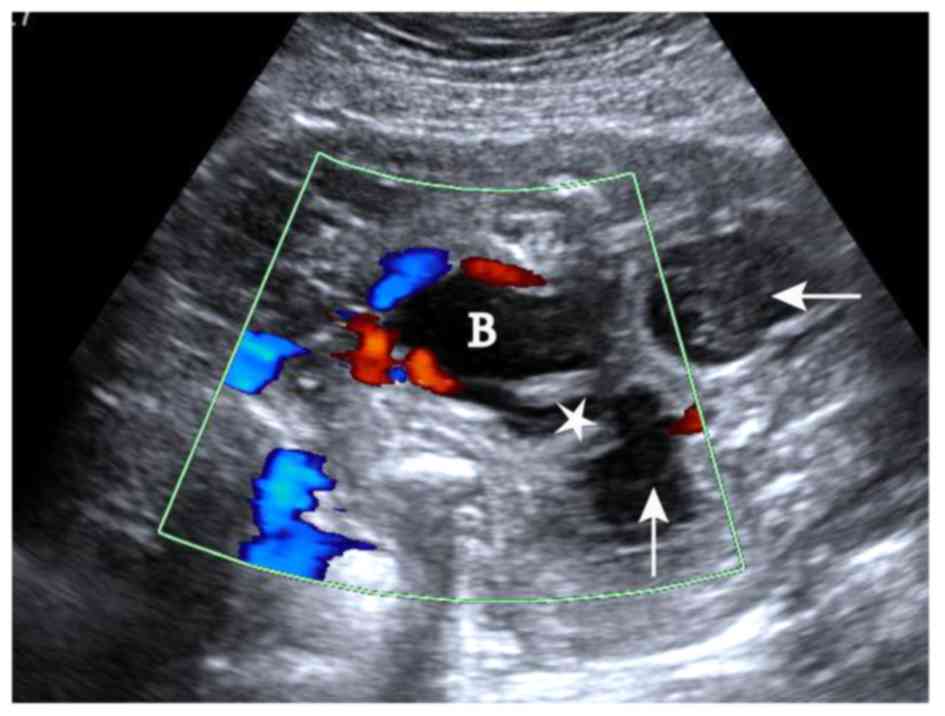
0.7×0.6 cm) with multiple cysts in the renal cortex (Fig. 2), dilated loops of the bowel with
blind endings, vesicointestinal fistula (Fig. 3), spinal scoliosis with a tethered
cord (Fig. 4), ambiguous genitalia
and a lack of amniotic fluid in the fluid sac (Figs. 1–4).
The bladder was visible in the pelvis (Fig. 3) and the abdominal wall appeared
normal and without omphalocele. These findings suggested a
diagnosis of URSMS.
A fetal blood sample was obtained via cordocentesis
under ultrasonic guidance, and isolated umbilical cord blood cells
were cultured for 72 h, followed by G-banding karyotyping analysis
using a Metascan Karyotyping System (Imstar S.A., Paris, France).
The chromosomal phenotype was 46XY with a large Y. The family
decided to terminate the pregnancy after consulting an obstetrician
and pediatrician due to the poor prognosis of the abnormalities and
the lack of amniotic fluid. The abortus weighed 1,110 g and the
body was 37 cm long. A post-mortem examination revealed the absence
of the subcutaneous muscle layer in the infra-umbilicus, through
which the bowel was protruding. The abortus also exhibited an
imperforate anus, a bifid scrotum without a penis and a diastasic
pubic rami. Once the abdominal cavity of the abortus was opened, a
dilated bowel with blind endings and vesicointestinal fistula was
revealed. The jejuno-ileum and dilated colon were both reduced in
length at ~70 and ~10 cm long, respectively. Multiple cysts in the
left kidney and small ureters were present. Conversely, the right
kidney was enlarged and spherical-shaped. When the right kidney was
opened with a surgical knife, the cortex and medulla were
visualized and a large cystic cavity filled with yellow fluid was
observed laterally in the right kidney. The right ureter was
contorted and dilated. Both ureters terminated in the bladder.
X-rays revealed the vertebral fusion of lumbar vertebrae 4 and 5
with three sacral vertebrae visible without coccygeal vertebrae
(Fig. 5). Based on the findings from
the autopsy, the diagnosis was confirmed as cloacal exstrophy
variant.
All procedures performed in the present case study
involving human participants were approved and in accordance with
the ethical standards of The Ethics Committee of Hubei Women and
Children's Hospital and with the 1964 Helsinki declaration and its
later amendments or comparable ethical standards. Informed consent
was obtained from the parents of the fetus in the present case
study.
Discussion
The primary difference between the prenatal and
postnatal findings in the present case was that the omphalocele was
conspicuous through the thin membrane of skin due to the absence of
subcutaneous muscle postnatally, whereas the omphalocele was
invisible in utero. We speculated that the reason for the
difference in appearance was that the high pressure outside the
fetal abdominal cavity, which resulted from the lack of amniotic
fluid in the amniotic sac and limited space for the fetus,
prevented the bowels from protruding through the ventral abdominal
wall defect. Therefore, it was difficult to diagnose the present
case as a cloacal exstrophy variant based only on prenatal
knowledge of a spinal defect. As a result, a misdiagnosis of URSMS
was made due to the presence of defects in the internal and
external genitalia without omphalocele (9,10). There
is widespread agreement that the infra-umbilical wall defect is the
predominant difference between the two diseases as the accepted
mechanism of cloacal exstrophy is the failure of the primitive
streak mesoderm to extend into the infra-umbilical cloacal
membrane, resulting in the incomplete formation of the lower
abdominal wall and omphalocele (11,12).
To the best of our knowledge, the present report
presents the first description of cloacal exstrophy with no
amniotic fluid. The lack of amniotic fluid may have been caused by
the lack of orifices in the posterior and umbilical region. Nakano
et al (13) described a case
of cloacal exstrophy with normal amniotic fluid due to urachus in
the umbilical region. Another possible cause for the lack of
amniotic fluid may be due to the failure of fetal renal function
due to the renal hypoplasia. Hendren (14) previously reported a case where the
urinary system anomaly that accompanied cloacal exstrophy consisted
of crossed renal ectopia, horseshoe kidneys, an ectopic ureter,
ureteropelvic junction obstruction, dysplastic kidneys, megaureter
and a ureterocele.
The defining characteristic observed via prenatal
ultrasound and postnatal autopsy examination for the present case
was a non-exstrophic bladder, which is the predominant
characteristic used to distinguish cloacal exstrophy variant from
classic cloacal exstrophy (15).
Cloacal exstrophy involves a variety of abnormalities and to
achieve a superior analysis, understanding and treatment of the
disease, Manzoni et al (15)
proposed a systemic classification based on their experience with
34 patients. In the study, cloacal exstrophy was divided into the
following: Classic exstrophy (type I), which exhibits three
subclassifications (A-C) based on the position of the exstrophic
hemibladder relative to the everted bowel; and the cloacal
exstrophy variant (type II), which exhibits three
subclassifications (A-C) based on bladder variations, bowel
variations and mixed bladder-bowel variants. According to this
classification system, the present case is type IIA with a closed
bladder.
In addition, the present case featured bifid scrotum
and aphallia, similar to the cases reported by Nakano et al
(13) and Lakshmanan et al
(16). However, Lakshmanan, who is a
urologic surgeon, noted that the phallus was typically located in
the bladder rather than absent, a characteristic that may be
observed by pathologic examination. Lakshmanan et al
(16) indicated the importance for
surgeons to be aware of such variations in order to prevent the
inappropriate use of irrevocable measures, such as orchiectomy.
Similarly, a previous study demonstrated that undivided phallic
structures were shown to protrude either from the most caudal part
of the exstrophic area or from the short perineum via the
histopathological analysis of three cases with covered cloacal
exstrophy (17). Deficiencies in the
present case were the absence of pathological analysis of the
vesicle tissue and the limited experience of the pathologist
regarding cloacal exstrophy. Therefore, it was unknown whether the
phallus was absent or present as an intravesicle phallus, as in
previous cases (17,18). Finally, the present results
identified two testicles located laterally in the pelvic cavity via
autopsy examination, which is the most common anomaly of male
sexual development (19).
Furthermore, Meglin et al (20) reported that 5/7 males with cloacal
exstrophy were identified to exhibit cryptorchidism.
In conclusion, the present case indicated that
omphalocele with the cloacal exstrophy variant could not be
detected by ultrasound in utero due to the high pressure
outside the abdominal cavity caused by a lack of amniotic fluid and
limited space. Knowledge of this finding will aid medical
practitioners to make correct prenatal diagnoses. In addition, to
the best of our knowledge, the present study indicates the first
reported case of a cloacal exstrophy variant without amniotic fluid
in utero.
References
|
1
|
Carey JC, Greenbaum B and Hall BD: The
OEIS complex (omphalocele, exstrophy, imperforate anus, spinal
defects). Birth Defects Orig Artic Ser. 14:253–263. 1978.PubMed/NCBI
|
|
2
|
Hurwitz RS, Manzoni GA, Ransley PG and
Stephens FD: Cloacal exstrophy: A report of 34 cases. J Urol.
138:1060–1064. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vlangos CN, Siuniak A, Ackley T, van
Bokhoven H, Veltman J, Iyer R, Park JM, Keppler-Noreuil K and
Keegan CE: Comprehensive genetic analysis of OEIS complex reveals
no evidence for a recurrent microdeletion or duplication. Am J Med
Genet A. 155A:1–49. 2011.PubMed/NCBI
|
|
4
|
Kosaki R, Fukuhara Y, Kosuga M, Okuyama T,
Kawashima N, Honna T, Ueoka K and Kosaki K: OEIS complex with
del(3)(q12.2q13.2). Am J Med Genet Part A. 135:224–226. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mallmann MR, Reutter H, Müller AM, Geipel
A, Berg C and Gembruch U: Omphalocele-exstrophy-imperforate
anus-spinal defects complex: Associated malformations in 12 new
cases. Fetal Diagn Ther. 41:66–70. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ben-Neriah Z, Withers S, Thomas M, Toi A,
Chong K, Pai A, Velscher L, Vero S, Keating S, Taylor G and
Chitayat D: OEIS complex: Prenatal ultrasound and autopsy findings.
Ultrasound Obstet Gynecol. 29:170–177. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Phillips TM, Salmasi AH, Stec A, Novak TE,
Gearhart JP and Mathews RI: Urological outcomes in the omphalocele
exstrophy imperforate anus spinal defects (OEIS) complex:
Experience with 80 patients. J Pediatr Urol. 9:353–358. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tiblad E, Wilson RD, Carr M, Flake AW,
Hedrick H, Johnson MP, Bebbington MW, Mann S and Adzick NS: OEIS
sequence-a rare congenital anomaly with prenatal evaluation and
postnatal outcome in six cases. Prenat Diagn. 28:141–147. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Escobar LF, Weaver DD, Bixler D, Hodes ME
and Mitchell M: Urorectal septum malformation sequence. Report of
six cases and embryological analysis. Am J Dis Child.
141:1021–1024. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chien JC, Chen SJ, Tiu CM, Chen YJ, Hwang
B and Niu DM: Is urorectal septum malformation sequence a variant
of the vertebral defects, anal atresia, tracheo-oesophageal
fistula, renal defects and radial dysplasia association? Report of
a case and a review of the literature. Eur J Pediatr. 164:350–354.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ambrose SS and O'Brien DP III: Surgical
embryology of the exstrophy-epispadias complex. Surg Clin North Am.
54:1379–1390. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Keppler-Noreuil KM: OEIS complex
(omphalocele-exstrophy-imperforate anus-spinal defects): A review
of 14 cases. Am J Med Genet. 99:271–279. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nakano Y, Aizawa M, Honma S and Osa Y:
Completely separated scrotum and vesicointestinal fistula without
exstrophy as a novel manifestation of aphallia: A case report.
Urology. 74:1303–1305. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hendren WH: Cloacal malformations:
Experience with 105 cases. J Pediatr Surg. 27:890–901. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Manzoni GA, Ransley PG and Hurwitz RS:
Cloacal exstrophy and cloacal exstrophy variants: A proposed system
of classification. J Urol. 138:1065–1068. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lakshmanan Y, Bellin PB, Gilroy AM and
Fung LC: Antenatally diagnosed cloacal exstrophy variant with
intravesical phallus in a twin pregnancy. Urology. 57:11782001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
van der Putte SC, Spliet WG and Nikkels
PG: Common (‘classical’) and covered cloacal exstrophy: A
histopathological study and a reconstruction of the pathogenesis.
Pediatr Dev Pathol. 11:430–442. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Arunachalam P, Pillai SB and Sridhar DC:
Classical cloacal exstrophy with intravesical phallus. J Pediatr
Surg. 47:E5–E8. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Phillips TM: Spectrum of cloacal
exstrophy. Semin Pediatr Surg. 20:113–118. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Meglin AJ, Balotin RJ, Jelinek JS, Fishman
EK, Jeffs RD and Ghaed V: Cloacal exstrophy: Radiologic findings in
13 patients. AJR Am J Roentgenol. 155:1267–1272. 1990. View Article : Google Scholar : PubMed/NCBI
|