Introduction
Higher temperature and high humidity weather is
common in the summer, and cardiovascular disease is associated with
this environment (1,2). A hot and humid environment is a type of
thermal stress on the body (3),
however, the effect of a thermal environment on patients with high
blood pressure remains unknown. Therefore, investigating the
pathophysiological effects of a high temperature and high humidity
environment on the body's cardiovascular system may be important in
improving the control and prevention of this type of disease.
Previous findings have revealed that thermal stress
induces apoptosis and causes vascular damage (4–6).
Caspase-3 is thought to be a key apoptosis indicator, its
activation indicates an irreversible stage of apoptosis (7). In the regulation of apoptosis, members
of the B-cell lymphoma 2 (Bcl-2) family serve key functions
(8). The Bcl-2 family can be divided
into two categories: One category is anti-apoptotic, and includes
Bcl-2, Bcl-xL, Bcl-2-like protein 2 (Bcl-2-L-2), Bcl-2-L-3 and cell
death protein 9; The other category of Bcl-2 proteins promotes cell
death, and includes Bcl-2-L-4 (Bax), Bcl-2-L-7, Bcl-xS, Bcl-2-L-8,
Bcl-2-interacting killer and BH3-interacting domain death agonist
(9). Increased Bax promotes cell
apoptosis, whereas increased Bcl-2 inhibits cell apoptosis
(10).
Besides apoptosis, vasoreactivity is the most basic
and direct indicator that reflects artery vascular function in the
body (11). Enhanced contractive
function is the primary symptom of a damaged blood vessel (12,13).
Increased vasoreactivity is a key mechanism for the development of
cardiovascular disease and is a prognostic indicator of arterial
health (14). Vasoreactivity of
blood vessels is increased by heat exposure (15), however, to the best of our knowledge,
this effect has not been investigated in a hypertensive state. The
aim of the current study was to investigate the effect of a thermal
environment on rats with hypertensive blood pressure. Apoptosis and
vasoreactivity of blood vessels was measured and changes in
vascular morphology were recorded.
Materials and methods
Animals
A total of 24 male Wistar-Kyoto (WKY) rats and 24
male spontaneously hypertensive rats (SHRs) (all 7 weeks old) were
provided by the Charles River Laboratories (Wilmington, MA, USA).
According to the experimental schedule, WKY rats were randomly
divided into three groups (n=8/group): Control group (WKY-CN), heat
exposure for 8 h group (WKY-8) and heat exposure for 24 h group
(WKY-24). SHR rats were randomly divided into three groups
(n=8/group): SHR-CN, SHR-8 and SHR-24. The WKY-CN and SHR-CN groups
were maintained at room temperature of 24°C with 55% relative
humidity, both the WKY-8 and WKY-24 groups were exposed to a high
temperature of 32°C at 65% relative humidity. Heat exposure was
performed in an artificial climate chamber (Qianjiang Instrument
& Equipment Co., Ltd., Hangzhou, China). Rats in the WKY-8 and
SHR-8 group received a fixed 8 h (9:00 a.m. to 5:00 p.m.) heat
exposure process each day, but were kept in the control conditions
(24°C, 55% humidity) when they weren't being exposed to heat; the
WKY-24 group was exposed to the hot environment all day. The SHR-8
and SHR-24 groups were received the same heat exposure. Food and
water were supplied ad libitum. Rats were housed in a 12-h
light/dark cycle (light 6:00 p.m. to 6:00 a.m.). Heat exposure
lasted for 7 days. The experimental procedures of the present study
were approved by the Animal Ethics and Use Committees of Ningxia
Medical University (Yinchuan, China), in accordance with the
guidelines of the Council of the Physiological Society of China.
The behavior and active state of rats were be monitored
carefully.
Weight and food consumption
Upon initiation of the heat exposure experiment, the
body weights of the rats were measured. During the experiment, food
consumption was recorded in each group daily. At the end of the
experiment, body weight was measured again.
Blood pressure
Prior to the experiment, systolic and diastolic
blood pressure were measured from the rat tails using a blood
pressure monitor (BP-2010A; Softron Biotechnology, Beijing, China),
and the data were obtained directly from the machine. At the end of
the experiment, blood pressure was measured again from the rat
tails.
Vasoreactivity
Following anesthesia, the rat chests were
immediately opened, and the thoracic aorta was removed and placed
into a paraffin platter filled with normal saline. Connective
tissue was cut off carefully; the vascular ring (4–5 mm wide) was
obtained by sectioning the thoracic aorta. Another section (5 mm)
of the thoracic aorta was harvested for hematoxylin and eosin
(H&E) staining. The rest of the thoracic aorta was submerged in
liquid nitrogen and stored at −80°C for subsequent reverse
transcription-quantitative polymerase chain reaction (RT-qPCR) and
western blotting analyses. The vascular ring was suspended in an
organ bath (DMT GmbH & Co., KG, Essen, Germany) containing 10
ml Krebs solution [ingredients (all mmol/l): Glucose 5.6, NaCl 10,
NaHCO3 24.8, KCl 4.6, CaCl2 2.5,
MgSO4 1.2, and KH2PO4 1.2]. The system was
ventilated with mixed gas of 95% O2 and 5%
CO2 continuously, and a constant temperature of 37°C was
maintained. Resting tension was adjusted to 1 g, and the ring was
balanced for 40 min, with Krebs solution replenished every 15 min.
Maximal contraction was established by the addition of 60 mM KCl.
After resting tension was stable, Krebs fluid was replaced and
basal tension was returned to 1 g. A cumulative concentration of
noradrenaline (Shanghai Harvest Pharmaceutical Co., Ltd., Shanghai,
China) (10−10-10−5M) was added to the bath
system, and contractive tension was recorded. The vascular tension
induced by NA (10−10-10−5M) was expressed as
a percentage of the maximal contraction tension range induced by
KCl (60 mM).
Morphological observation
A short part (5 mm) of the thoracic aorta was fixed
in 10% formalin for 12 h at 4°C, embedded in paraffin and sliced
into tissue sections (10 µm). Morphological changes of the thoracic
aorta were observed by HE staining (hematoxylin staining for 2 min
at 24°C; and eosin staining for 5 min at 24°C) using an Olympus
DP71 microscope (Olympus Corporation, Tokyo, Japan).
RT-qPCR analysis of caspase-3, Bcl-2
and Bax mRNA expression
Total RNA was extracted from the thoracic aorta
using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA), according to the manufacturer's protocol.
Complementary DNA (cDNA) was synthesized with a First-Strand cDNA
Synthesis kit (Thermo Fisher Scientific, Inc.). qPCR was carried
out using a Maxima SYBR-Green PCR kit (Thermo Fisher Scientific,
Inc.) with primers as listed in Table
I. Following an initial 10 min at 95°C, the PCR thermal cycling
program was performed as follows: 95°C for 15 sec, 60°C for 30 sec,
and extension at 72°C for 30 sec, for 40 cycles. At the end of the
reaction, melting curve analysis was performed to ensure the
specificity of the reaction. Relative gene expression levels were
determined using the 2−ΔΔCq method (11,12).
β-actin was used as an internal control.
 | Table I.Sequences of the oligo nucleotide
primers used for reverse transcription-quantitative polymerase
chain reaction analysis. |
Table I.
Sequences of the oligo nucleotide
primers used for reverse transcription-quantitative polymerase
chain reaction analysis.
| Gene | Direction | Sequence (5′-3′) | Bp | GenBank no. |
|---|
| Caspase-3 | Forward |
AGCTGGACTGCGGTATTGAG | 104 | NM_012922 |
|
| Reverse |
GGGTGCGGTAGAGTAAGCAT |
|
|
| Bcl-2 | Forward |
AGCCTGAGAGCAACCGAAC | 159 | NM_016993 |
|
| Reverse |
AGCGACGAGAGAAGTCATCC |
|
|
| Bax | Forward |
TTGCTACAGGGTTTCATCCAG | 145 | NM_017059 |
|
| Reverse |
TGTTGTTGTCCAGTTCATCG |
|
|
| β-actin | Forward |
CACCCGCGAGTACAACCTTC | 207 | NM_031144 |
|
| Reverse |
CCCATACCCACCATCACACC |
|
|
Protein expression levels of
caspase-3, Bcl-2 and Bax
Protein was extracted from the thoracic aorta using
a Total Protein Extraction kit for western blotting (KeyGen Biotech
Co., Ltd., Nanjing, China). The protein determination was completed
using the BCA method (KeyGen Biotech Co., Ltd.). Protein lysates
(100 µg) were separated by 12% SDS-PAGE (KeyGen Biotech Co., Ltd.)
run for 30 min at 80 V and 60 min at 120 V, followed by transferral
to polyvinylidene fluoride membranes (EMD Millipore, Billerica, MA,
USA). Following blocking with non-fat milk powder for 1 h at 24°C,
the membranes were incubated with primary antibodies for 2 h at
24°C. Primary antibodies used in the present study were as follows:
Rabbit monoclonal anti-Bax (1:5,000; cat no. ab32503), rabbit
monoclonal anti-Bcl-2 (1:2,000; cat no. ab136285), rabbit
monoclonal anti-Caspase-3 (1:500; cat no. ab4051) and rabbit
monoclonal anti-β-actin (1:1,000; cat no. 5632-1) (all from Abcam,
Cambridge, UK). Following washing with TBST three times for 5 min,
the membrane was incubated for 2 h at 24°C with secondary antibody
horseradish peroxidase-conjugated goat anti-rabbit IgG (1:2,000;
ZB-2301; ZSGB-Bio, Beijing, China). Membranes were subjected to an
enhanced chemiluminescence kit (Thermo Fisher Scientific, Inc.).
Western blot analysis was performed using an Amersham Imager 600
(GE Life Sciences, Chicaco, IL, USA).
Statistical analysis
Data were expressed as the mean ± standard
deviation. Statistical analyses were performed using SPSS version
17.0 software (SPSS, Inc., Chicago, IL, USA). Comparisons between
the means of numerous samples were evaluated by analysis of ANOVA,
and comparisons between the means of two samples were evaluated by
Fisher's least significant difference t-test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Weight and food consumption
Prior to heat exposure, all rats exhibited good
appetite, agility and activity levels. Rats were restless in the
evening. During thermal exposure, rats were tired and sleepy, and
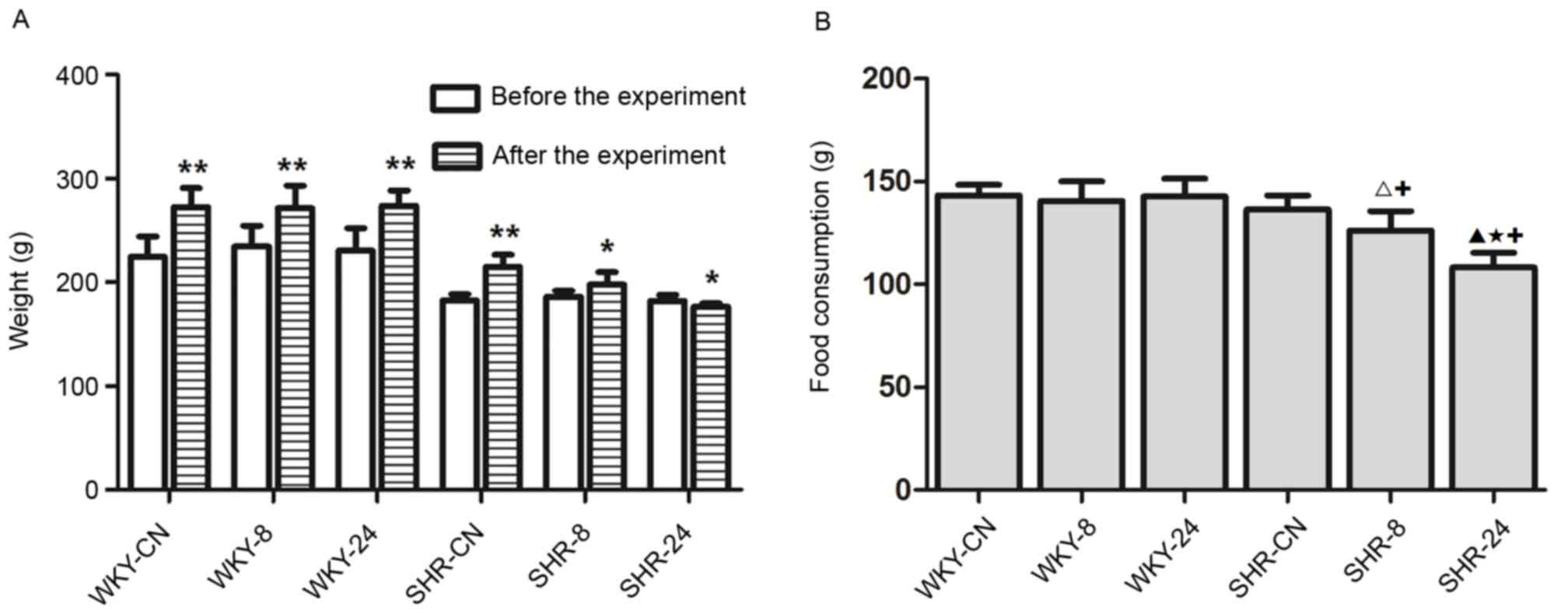
were observed to hide in the bedding material. As shown in Fig. 1A, the body weight of rats in each
group at the end of the experiment was significantly increased
compared with before the experiment (P<0.01 for all WKY groups
and SHR-CN; P<0.05 for SHR-8), except for rats in the SHR-24
group, which exhibited significantly reduced body weight compared
with before the experiment (P<0.05). There were no notable
differences in food consumption among the WKY groups (Fig. 1B). Food consumption was significantly
reduced in the SHR-8 and SHR-24 rats compared with SHR-CN
(P<0.05; Fig. 1B).
Blood pressure
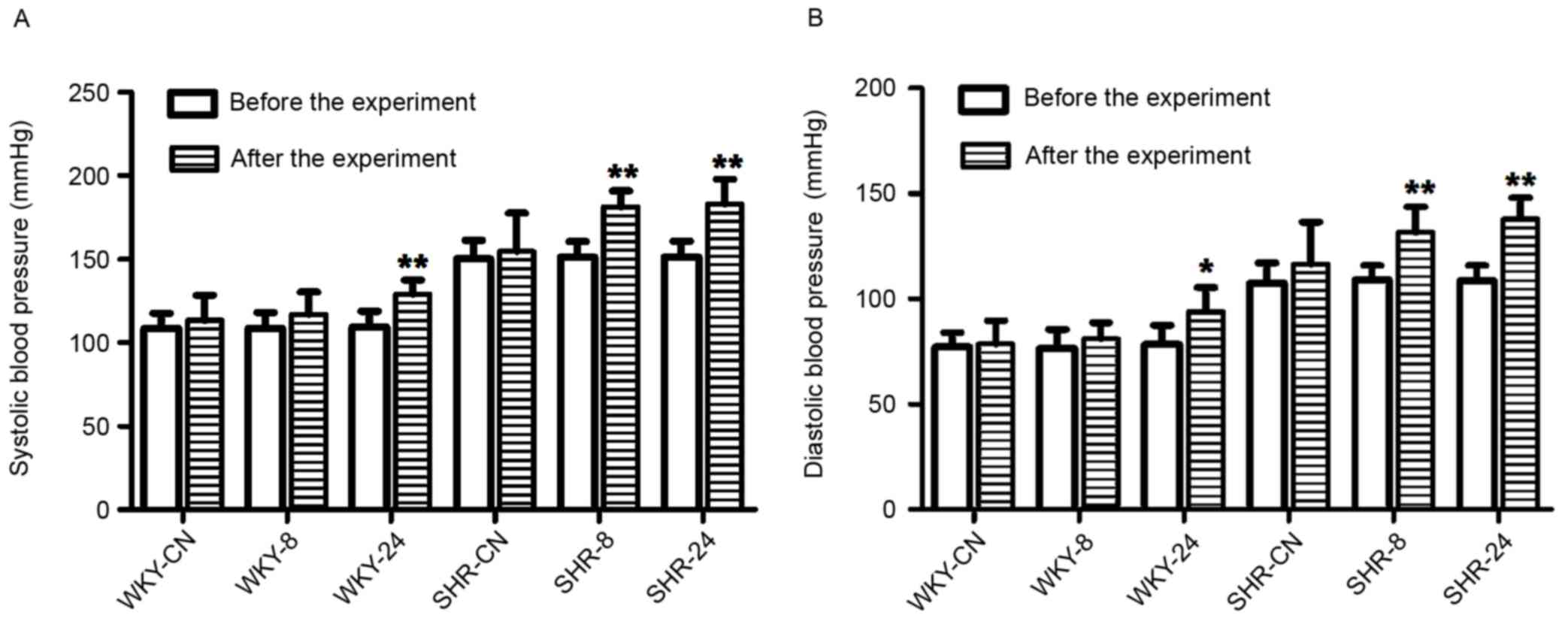
Experimental results demonstrated that rat blood
pressure was elevated in the high temperature and high humidity
environment compared with the room temperature environment
(Fig. 2). Following the experiment,
systolic blood pressure was significantly increased in the WKY-24,
SHR-8 and SHR-24 groups, as compared with before the experiment
(P<0.01; Fig. 2A). Diastolic
blood pressure was also significantly increased in the WKY-24
(P<0.05), SHR-8 (P<0.01) and SHR-24 (P<0.01) groups after
the experiment, as compared with before the experiment (Fig. 2B). As expected, systolic and
diastolic blood pressure in SHRs was higher than in WKY rats.
Vasoreactivity
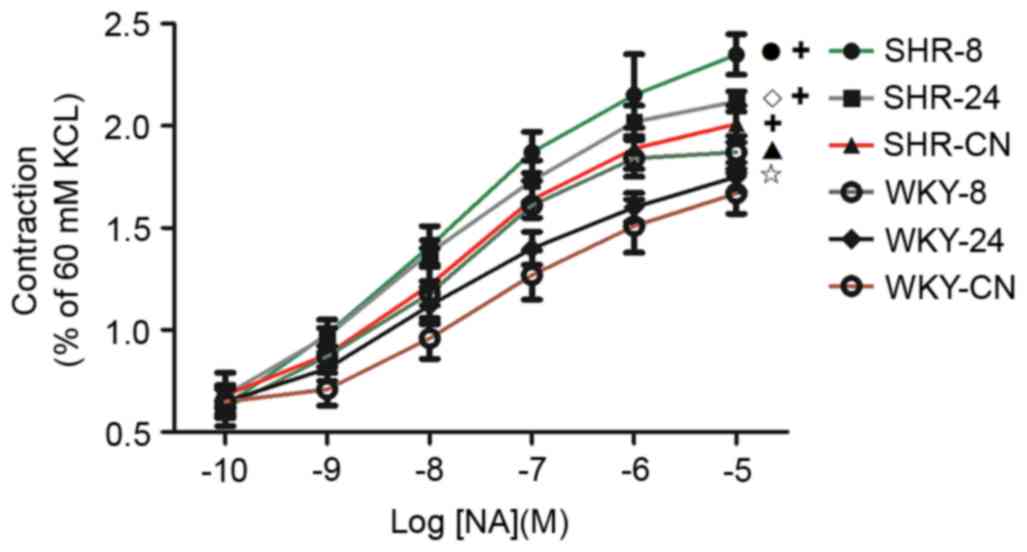
As shown in Fig. 3,
the contractile responses of thoracic aortic vascular rings to NA
in all groups increased as NA concentration increased.
Vasoreactivity in WKY-8 was significantly increased compared with
WKY-CN (P<0.01). Compared with the SHR-CN group, vasoreactivity
in the SHR-8 group was also significantly increased (P<0.01). In
both SHR and WKY groups, the increase in vasoreactivity in the 8
h-exposed group was significantly larger compared with the increase
in the 24 h-exposed group (P<0.05). Vasoreactivity in the SHR
groups was significantly increased compared with the corresponding
WKY groups (P<0.01).
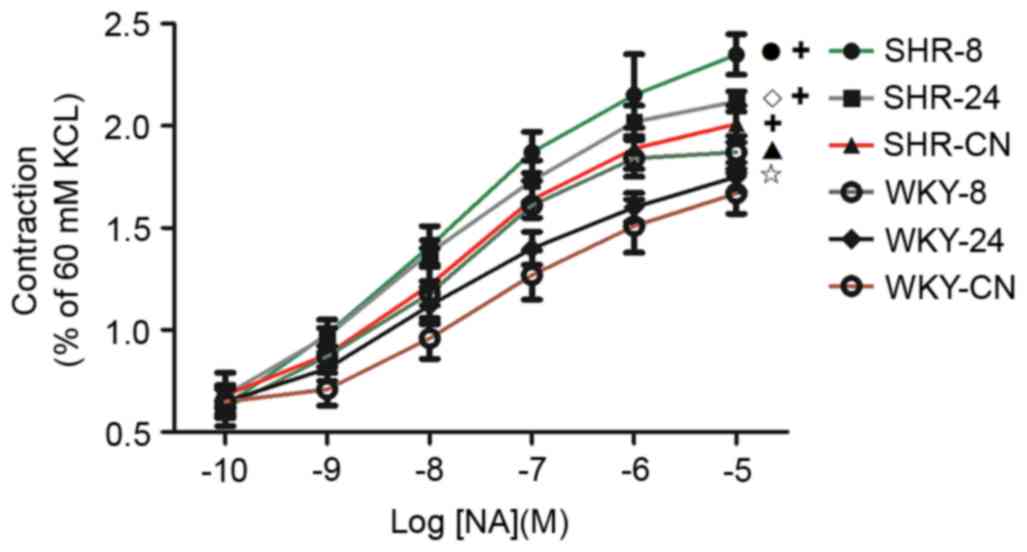 | Figure 3.Effect of a hot and humid environment
on vasoreactivity. Data are presented as the mean ± standard
deviation (n=8). •P<0.01, SHR-8 vs. SHR-CN;
◊P<0.05, SHR-24 vs. SHR-8; ▲P<0.01,
WKY-8 vs. WKY-CN; ✩P<0.05, WKY-24 vs. WKY-8;
+P<0.01, SHR vs. WKY. WKY, Wistar-Kyoto rats; SHR,
spontaneously hypertensive rats; CN, control; −8, heat exposure for
8 h; −24, heat exposure for 24 h; NA, noradrenaline. |
Morphological observation
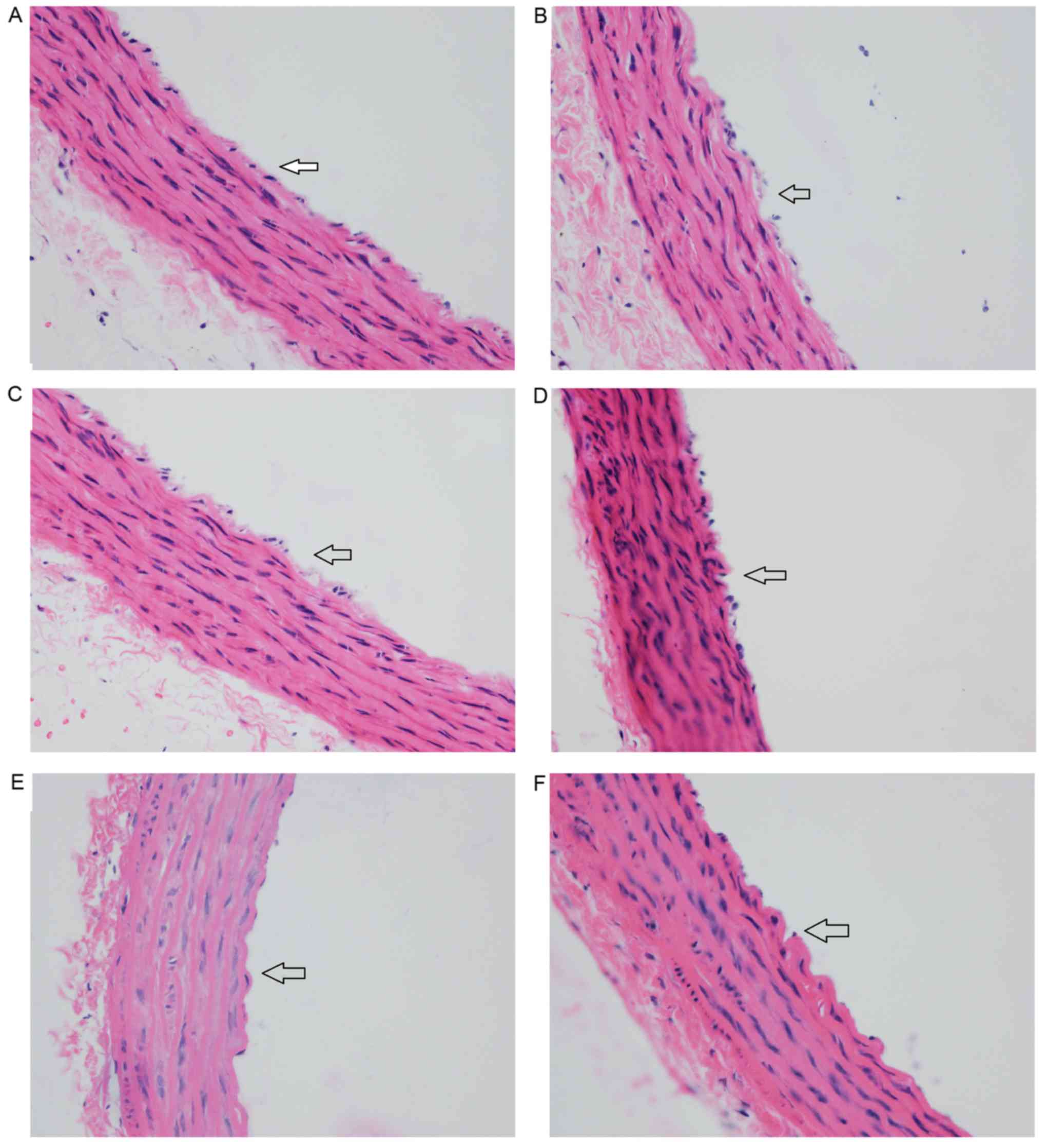
In the WKY-CN group, the intima of the aorta was
smooth with a single layer of endothelial cells (Fig. 4A). In the WKY-8 group, endothelial
cells detached and the endothelium was incomplete (Fig. 4B). In the WKY-24 group, endothelial
cells were connected loosely, and the endothelium was partly
missing (Fig. 4C), but the changes
were less notable than in the WKY-8 group. In the SHR groups, the
thoracic aorta was thicker and the arrangement of cells was
slightly more disordered than in the WKY groups. In the SHR-CN
group, the endothelial cells were mostly connected, and cells were
arranged closely in the intima, medial and outer membranes
(Fig. 4D). In the SHR-8 group, most
of the endothelial cells were lost, the vascular intima was
incomplete, some elastic fibers and collagen fibers were thicker,
and cell distribution was disorderly (Fig. 4E). Similar changes were observed in
the SHR-24 group (Fig. 4F), but
these were more severe in the SHR-8 group.
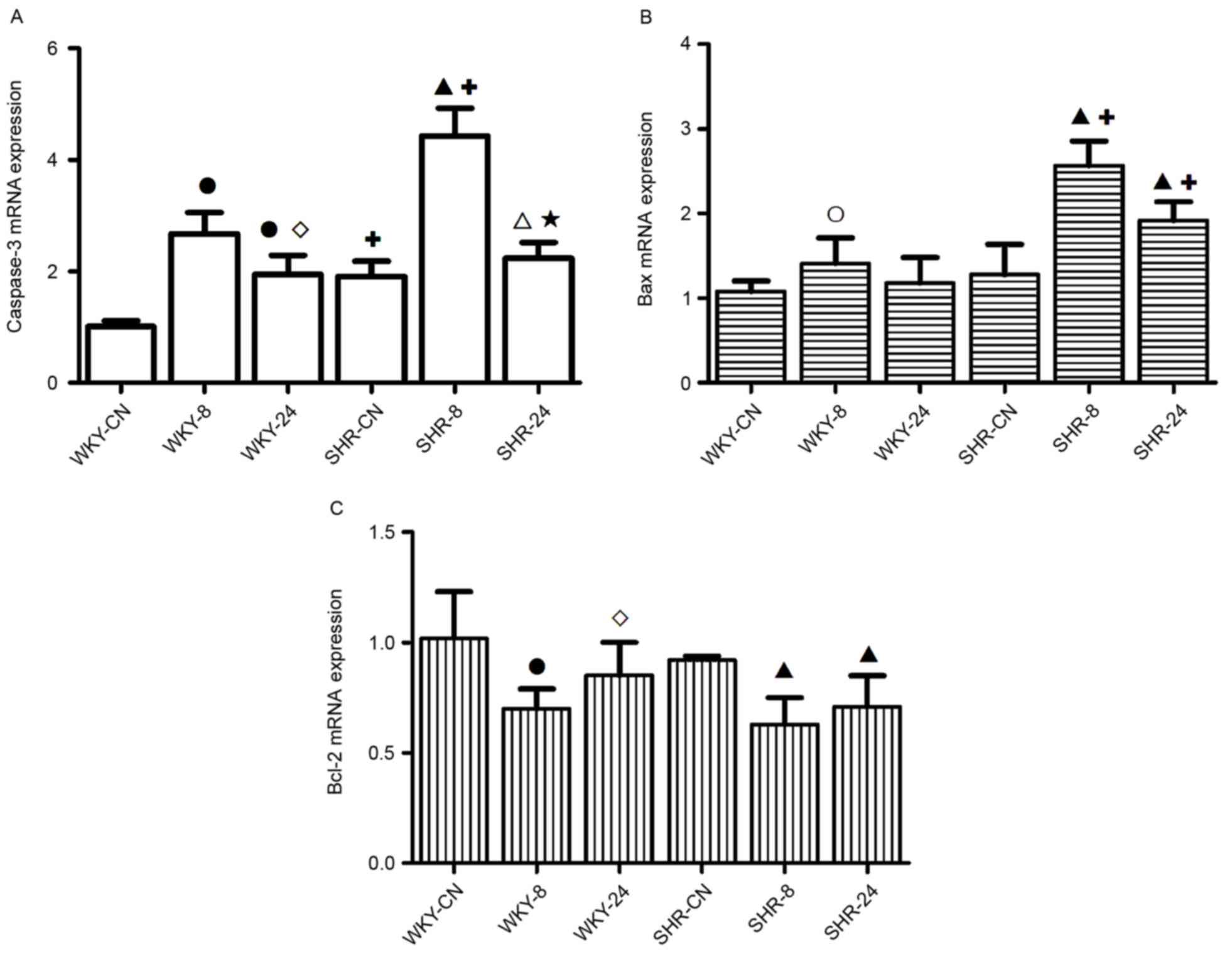
mRNA expression levels of caspase-3,
Bcl-2 and Bax
In the hot and humid environment, the expression
levels of apoptosis genes increased, and this increase was greater
under discontinuous thermal stimulation than with continuous
thermal stimulation (Fig. 5). mRNA
expression levels of caspase-3 in WKY-8 and WKY-24 were
significantly increased compared with WKY-CN (P<0.01; Fig. 5A). Compared with the SHR-CN group,
the mRNA expression level of Caspase-3 in the SHR-8 and SHR-24
groups was also significantly increased (P<0.01 and P<0.05,
respectively). Expression levels of caspase-3 in the SHR-CN and
SHR-8 groups were significantly increased compared with the
corresponding WKY groups (P<0.01). Compared with the 8 h-exposed
group, the increased expression level of caspase-3 in the 24
h-exposed group was weaker in both WKY and SHR groups (P<0.05,
P<0.01 respectively; Fig.
5A).
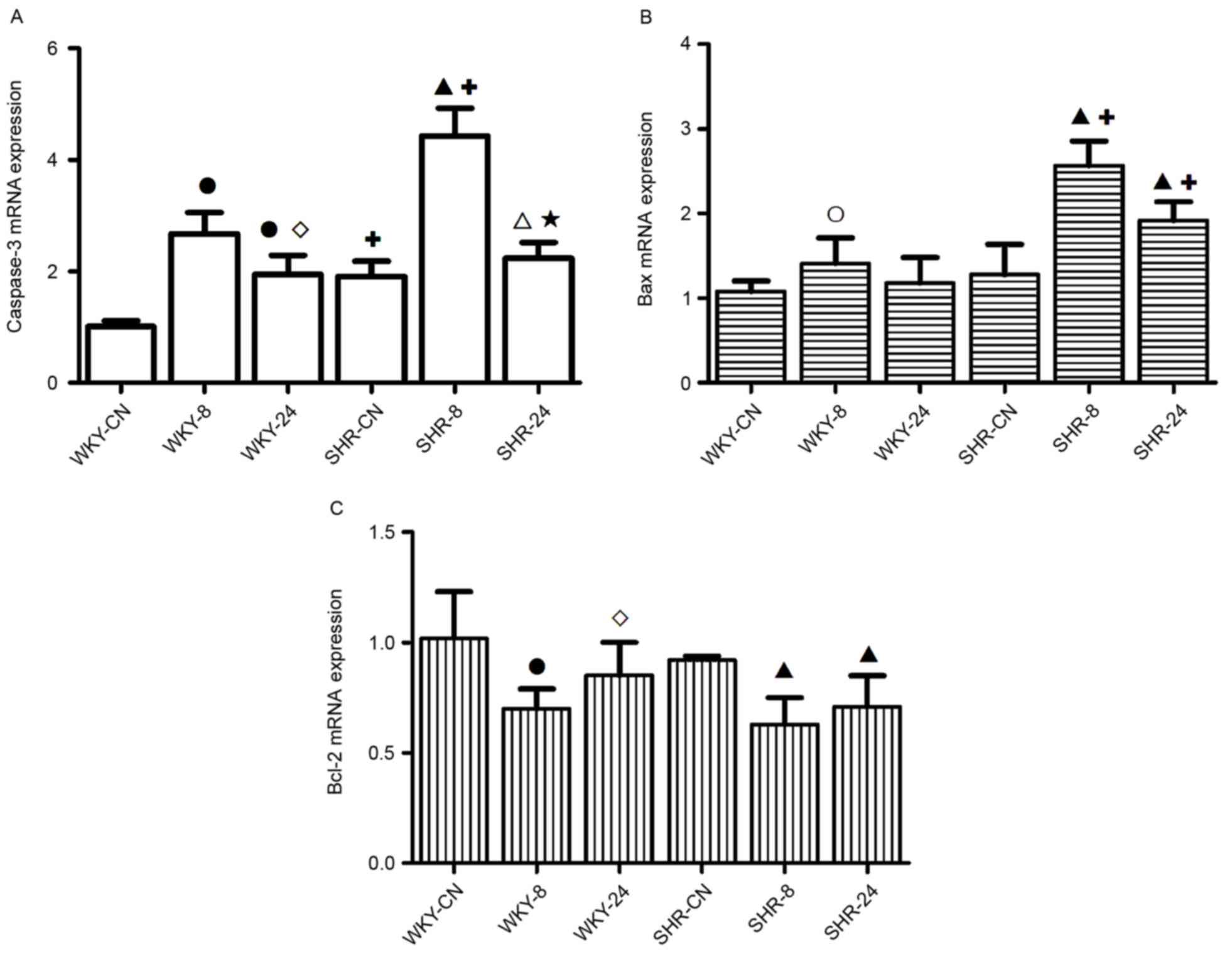 | Figure 5.Effect of a hot and humid environment
on the mRNA expression levels of (A) caspase-3, (B) Bax and (C)
Bcl-2. Data are presented as the mean ± standard deviation (n=8).
○P<0.05 and ●P<0.01 vs. WKY-CN;
◊P<0.05, WKY-24 vs. WKY-8; ∆P<0.05 and
▲P<0.01 vs. SHR-CN; ★P<0.01, SHR-24 vs.
SHR-8; +P<0.01 vs. WKY. WKY, Wistar-Kyoto rats; SHR,
spontaneously hypertensive rats; CN, control; −8, heat exposure for
8 h; −24, heat exposure for 24 h; Bcl-2, B-cell lymphoma 2; Bax,
Bcl-2-like protein 4. |
Compared with WKY-CN, the Bax apoptosis gene was
significantly upregulated in WKY-8 (P<0.05; Fig. 5B). Compared with the SHR-CN group,
the expression levels of Bax in the SHR-8 and SHR-24 groups were
significantly increased (P<0.01). In the high temperature and
high humidity environment, the expression levels of Bax in the SHR
groups were significantly increased compared with the corresponding
WKY groups (P<0.01).
Under the high temperature and high humidity
conditions, the expression level of Bcl-2 in the WKY-8 group and
SHR groups was significantly decreased, as compared with the
respective controls (P<0.01; Fig.
5C). Compared with the WKY-8 group, the expression level of
Bcl-2 in the WKY-24 group was significantly increased (P<0.05;
Fig. 5C).
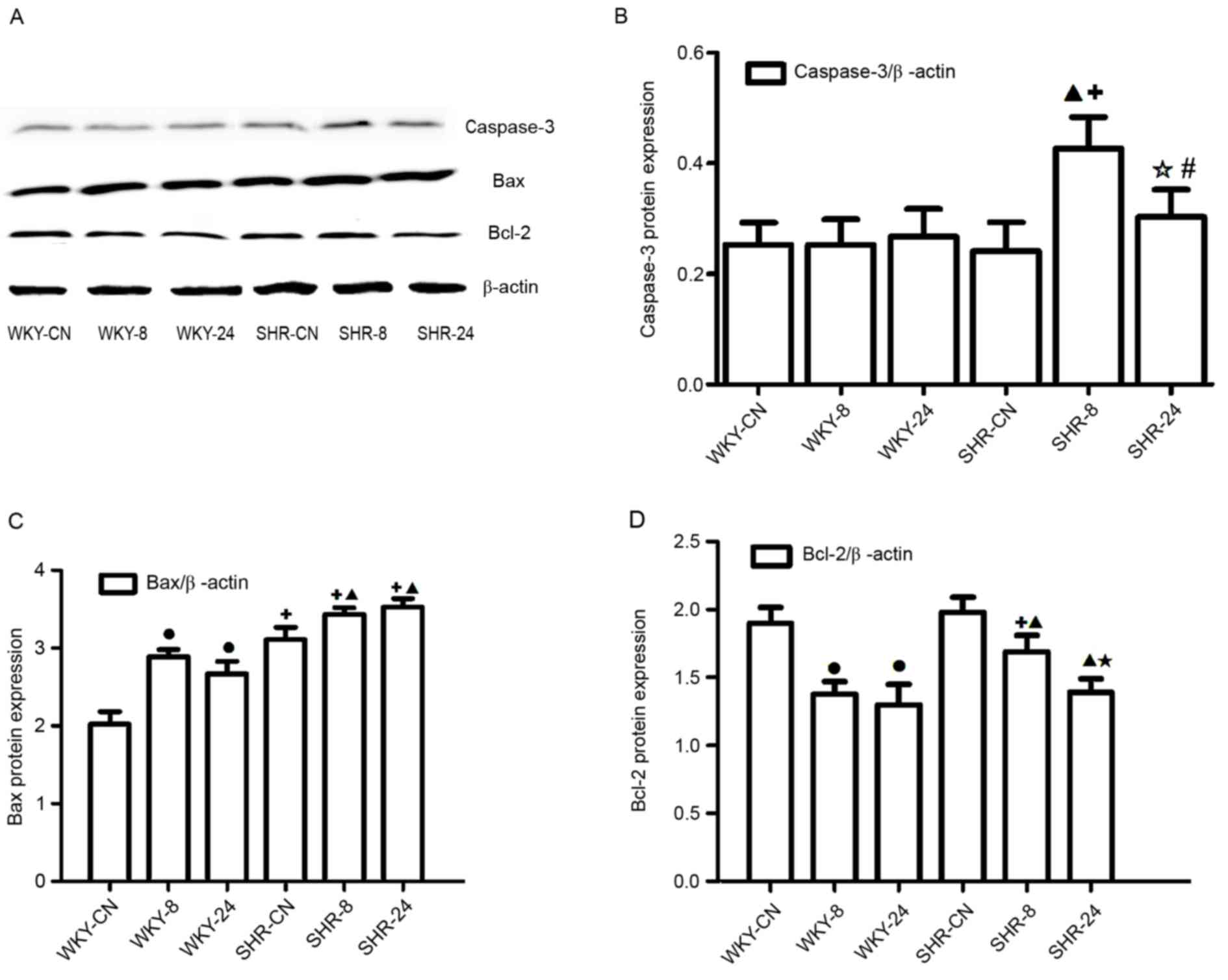
Protein expression levels of
caspase-3, Bcl-2 and Bax
Western blotting (Fig.
6A) indicated that the Caspase-3 protein level increased in the
SHR-8 group when compared with the SHR-CN group (Fig. 6B); the protein levels of caspase-3 in
the SHR-24 was significantly decreased compared with the SHR-8
group (P<0.01; Fig. 6B), there
were no notable differences among the WKY groups, however, the
caspase-3 level was elevated in both SHR-8 and SHR-24 groups than
in WKY-8 and WKY-24 groups (P<0.01, P<0.05; Fig. 6B). In the high temperature and
humidity environment, protein expression levels of Bax were
significantly increased, as compared with the control, respectively
(P<0.01; Fig. 6C), whereas Bcl-2
protein expression levels were significantly decreased compared
with the control in both types of rat (P<0.01; Fig. 6D), and compared with the SHR-8 group,
the protein level of Bcl-2 in the SHR-24 group was significantly
decreased, the decreased level of Bcl-2 in SHR-8 was weaker than in
the WKY-8 group (P<0.01; Fig.
6D). These results were broadly consistent with the mRNA
analysis.
Discussion
The present study investigated the effects of a hot
and humid environment on thoracic aorta damage in SHR. The results
of the present study revealed increased expression of Caspase-3 and
Bax, and reduced expression of Bcl-2 in a hot and humid
environment. Morphological observation of the thoracic aorta and
detection of vasoreactivity also indicated that the structure and
function of blood vessels was altered by the hot and humid
environment. Adverse effects on the rats' weight, diet and blood
pressure were also observed. According to these results, thoracic
aorta damage was more severe when rats were in a discontinuous
thermal environment, as compared with a continuous one.
In recent decades, the burden of cardiovascular
disease has increased to become a major public health problem
requiring urgent prevention and treatment strategies (16). The effect of a continuous high
temperature environment on health has been studied both in China
and abroad (17). High temperature
affects the body's blood dynamics and endocrine system (18), the amount of blood near the surface
of the body is increased, and the blood supplied to the heart is
relatively reduced under high temperature conditions, leading to
cerebral ischemia and hypoxia (19).
Meanwhile, the human body sweats under high temperature, which
results in loss of water and thickening of the blood, which are
dangerous factors in the occurrence of hypertension disease
(20). However, the effect of high
temperature environment on hypertension remains unclear.
In the present study, SHRs were used as the disease
model. The effect of a high temperature and humid environment was
investigated in these rats by measuring indices associated with
apoptosis, in order to investigate the corresponding changes in
blood vessels in hypertensive rats and the underlying
pathophysiological mechanisms. Along with high temperature
(5), high humidity also affects
blood dynamics by affecting heat dissipation, therefore, rats were
exposed to high temperature and high humidity conditions together.
The results revealed that food intake was slightly reduced in the
hot and humid environment in SHRs. The activity of rats was reduced
during the day. The SHR-24 group exhibited a decrease in body
weight over the course of the experiment. Furthermore, blood
pressure was increased in both WKY rats and SHRs in the 24-h heat
exposure group, however, 8-h heat exposure only increased blood
pressure in the SHRs, no elevation of blood Untitled-18pressure was
observed in WKY rats after 8-h exposure. This indicated that the
SHRs were more sensitive to a thermal environment compared with WKY
rats.
Vasoreactivity is one of the most basic and direct
indices used to assess artery blood vessel function (21). Enhanced contractive function is the
primary characteristic of a damaged blood vessel (22). In the present study, vasoreactivity
of the thoracic aorta indicated that contractive function was
enhanced in the hot and humid environment. Morphological
observation of the thoracic aorta revealed that the structure was
altered by exposure to a hot and humid environment. The most marked
difference was the lack of endothelium. Endothelium-dependent
vasodilatation is important in regulating the function of the aorta
(23), therefore the loss of the
endothelium may affect contractive function.
Apoptosis describes the programmed death of a cell
as part of its natural growth and development (24). Apoptosis has a key regulatory
function in the body, and can be induced by stress, such as free
radicals, hypoxia, blood deficiency or high temperature (25). Caspase-3 is thought to be an
important apoptosis indicator, its activation results in an
irreversible stage of apoptosis (26). In the process of cell apoptosis,
Bcl-2 and Bax have critical functions, increased Bax promotes cell
apoptosis, whereas increased Bcl-2 inhibits cell apoptosis
(27). The present study
demonstrated a hot and humid environment elevates the expression of
caspase-3 and Bax, whereas Bcl-2 was reduced, the elevation of
caspase-3 and Bax were more obvious in SHR rats while the
downregulation of Bcl-2 was more stronger in WKY rats. These
results suggested that cell apoptosis was induced by the hot and
humid environment. The loss of the endothelium may have been
associated with the increased number of apoptotic cells, thus
resulting in an altered organizational structure of blood vessels.
This may also affect the function of blood vessels. The SHR rats
were more sensitive to the hot and humid environment.
Heat acclimation, a conserved phenotypic adaptive
response to the prolonged transfer to a higher ambient temperature,
confers protection against acute heat stress and delays thermal
injury (28). The heat acclimation
process may strengthen the body to heat tolerance and make blood
vessels dilate (29). High
temperature and humidity environments are a type of stimulation.
When rats are housed in this environment for a long time, the body
may gradually adapt to this type of stimulation, and a variety of
disorders in the body will also move gradually toward the normal
value (30). However, it is
difficult to restore to the normal condition. Therefore, prior to
the end of the present experiment, rats (WKY-24 and SHR-24) in the
high temperature and humidity environment for 7 days had begun to
enter the heat acclimation process. However, due to the
discontinuous cold and hot stimulation, WKY-8 and SHR-8 rats
remained in a state of stress and therefore found it difficult to
enter the heat acclimation process. This might be the reason why 8
h-exposure induced more significant damage to the blood vessel.
Therefore, the present study concluded that intermittent heat
stress was more harmful than the continuous heat stress to blood
vessels.
In conclusion, apoptosis in the thoracic aorta was
increased under hot and humid conditions, this may be related to
the altered organizational structure and increased contractive
function of thoracic aorta. The disturbance of structure and
function on thoracic aorta was more notable in rats with
spontaneous hypertension under heat stress. The blood vessel was
more sensitive to intermittent heat stress than the continuous heat
stress. Besides, increased apoptosis may also have occurred
elsewhere in the body, affecting the rats' body weight, which
requires further experiments to confirm this.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant no. 81560052) and the Ningxia
Natural Science Foundation Key Project (grant nos. NZ13055 and
NZ16065) and West China Top Class Discipline Project in Basic
Medical Science, Ningxia Medical University (grant no.
2017016).
References
|
1
|
Hausfater P, Doumenc B, Chopin S, Le
Manach Y, Santin A, Dautheville S, Patzak A, Hericord P, Mégarbane
B, Andronikof M, et al: Elevation of cardiactroponin I during
non-exertional heat-related illnesses in the contextof a heatwave.
Crit Care. 14:R992010. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li G, Zhou M, Cai Y, Zhang Y and Pan X:
Does temperature enhance acute mortality effects of ambient
particle pollution in Tianjin City, China. Sci Total Environ.
409:1811–1817. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yibin JI, Liping P and Jun W: Assessment
of thermal comfort for aircraft cabin environment. J Safety
Environment. 15:306–309. 2015.
|
|
4
|
Shi YJ, Yu JR, Cen XN, Zhu Q and Ren HY:
Influence of HSP70 on combined method of hyperthermia and
immunologic effector cells to treat cancer. Beijing Da Xue Xue Bao.
37:175–178. 2005.(In Chinese). PubMed/NCBI
|
|
5
|
Pathapati RM, Kumar Rajesh M, Chirra BR,
Buchineni M, Sujith TR, Devaraju SR and Naidu MUR: Acute effects of
two angiotensin receptor blockers on vascular hemodynamics,
arterial stiffness and oxidative stress in patients with mild to
moderate hypertension: An open label parallel group study. ISRN
Vascular Med. 2013:52013. View Article : Google Scholar
|
|
6
|
Manning EP and Wilson B: Dehydration in
extreme temperatures while conducting stability and support
operations in a combat zone. Mil Med. 172:972–976. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
John K, Rösner I, Keilholz U, Gauler T,
Bantel H and Grünwald V: Baseline caspase activity predicts
progression free survival of temsirolimus-treated head neck cancer
patients. Eur J Cancer. 51:1596–1602. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu Y, Zheng Q, Wu H, Guo X, Li J and Hao
S: The effects of rapamycin on expression ratio of Bax/Bcl-2 and
the expression of activated caspace-3 in different types of tumor
cells. Tumor. 33:138–145. 2013.
|
|
9
|
Anvekar RA, Asciolla JJ, Missert DJ and
Chipuk JE: Born to be alive: A role for the BCL-2 family in
melanoma tumor cell survival, apoptosis, and treatmen. Front Oncol.
1:pii:000342011. View Article : Google Scholar
|
|
10
|
Zhang SD, Shan L, Li W, Li HL and Zhang
WD: Isochamaejasmin induces apoptosis in leukemia cells through
inhibiting Bcl-2 family proteins. Chin J Nat Med. 13:660–666.
2015.PubMed/NCBI
|
|
11
|
Li GH, Katakura M, Maruyama M, Enhkjargal
B, Matsuzaki K, Hashimoto M and Shido O: Changes of
noradrenaline-induced contractility and gene expression in aorta of
rats acclimated to heat in two different modes. Eur J Appl Physiol.
104:29–40. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim Y, Kim J, Kim M, Baek W and Kim I:
Effect of heat shock on the vascular contractility in isolated rat
aorta. J Pharmacol Toxicol Methods. 42:171–174. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Morimoto T, Miki K, Nose H, Itoh T and
Yamada S: Changes in vascular compliance during hyperthermia. J
Thermal Biol. 9:149–151. 1984. View Article : Google Scholar
|
|
14
|
Crandall CG and González-Alonso J:
Cardiovascular function in the heat-stressed human. Acta Physiol
(Oxf). 199:407–423. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Guanghua LI, Zhao N, Yang M, Zhao Z, Luo Y
and Osamu S: Effects of heat exposure during fixed time on thoracic
aorta contractility in rats. Academ J Second Military Med Univ.
34:291–294. 2013.
|
|
16
|
Liu X, Cui Y, Yang Y and Li L: Study on
neuroendocrine mechanism of occurrence of cerebral infarction in
hypertension rats induced by soaring temperature. Progress Modern
Biomedicine. 8:1428–1431. 2011.
|
|
17
|
Brazaitis M and Skurvydas A: Heat
acclimation does not reduce the impact of hyperthermia on central
fatigue. Eur J Appl Physiol. 109:771–778. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Haiyan Y, Liu Y, Wuxing Z and Daoyi L:
Influence of outdoor temperature on the indoor environment and
thermal adaptation in Chinese residential buildings during the
heating season. Energy Buildings. 116:133–140. 2016. View Article : Google Scholar
|
|
19
|
Maglara AA, Vasilaki A, Jackson MJ and
McArdle A: Damage to developing mouse skeletal muscle myotubes in
culture: Protective effect of heat shock proteins. J Physiol.
548:837–846. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhao Z, Yang M, Zhao N, Liu H, Dong J and
Li G: Influence of Lycium barbarum polysaccharides on
thoracic aortic vascular reactivity and free radical metabolism at
high temperature in exhaustive exercise rats. J Ningxia Med Univ.
35:481–484. 2013.
|
|
21
|
Laurent S, Cockcroft J, Van Bortel L,
Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C,
Wilkinson I and Struijker-Boudier H: European Network for
Non-invasive Investigation of Large Arteries: Expert consensus
document on arterial stiffness: Methodological issues and clinical
applications. Eur Heart J. 27:2588–2605. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Swierblewska E, Hering D, Kara T, Kunicka
K, Kruszewski P, Bieniaszewski L, Boutouyrie P, Somers VK and
Narkiewicz K: An independent relationship between muscle
sympathetic nerve activity and pulse wave velocity in normal
humans. J Hypertens. 28:979–984. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhao Z, Luo Y, Li G, Zhu L, Wang Y and
Zhang X: Thoracic aorta vasoreactivity in rats under exhaustive
exercise: Effects of Lycium barbarum polysaccharides
supplementation. J Int Soc Sports Nutr. 10:472013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Salvesen GS and Ashkenazi A: Snapshot:
Caspases. Cell. 147:476.e12011. View Article : Google Scholar
|
|
25
|
Jonestone RW, Ruefli AA and Lowe SW:
Apoptosis: A link between cancer genetics and chemotherapy. Cell.
108:153–164. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang LI, Liu F, Luo Y, Zhu L and Li G:
Effect of acute heat stress on adrenocorticotropic hormone,
cortisol, interleukin-2, interleukin-12 and apoptosis gene
expression in rats. Biomed Rep. 3:425–429. 2015.PubMed/NCBI
|
|
27
|
Li Z, Zhao J, Li Q, Yang W, Song Q, Li W
and Liu J: KLF4 promotes hydrogen-peroxide-induced apoptosis of
chronic myeloid leukemia cells involving the bcl-2/bax pathway.
Cell Stress Chaperones. 15:905–912. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Horowitz M: From molecular and cellular to
integrative heat defense during exposure to chronic heat. Comp
Biochem Physiol A Mol Integr Physiol. 131:475–483. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Horowitz M, Eli-Berchoer L, Wapinski I,
Friedman N and Kodesh E: Stress-related genomic responses during
the course of heat acclimation and its association with
ischemic-reperfusion cross-tolerance. J Appl Physiol (1985).
97:1496–1507. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Schwimmer H, Gerstberger R and Horowitz M:
Heat acclimation affects the neuromodulatory role of AngII and
nitric oxide during combined heat and hypohydration stress. Brain
Res Mol Brain Res. 130:95–108. 2004. View Article : Google Scholar : PubMed/NCBI
|