Introduction
Implant-related osteomyelitis is a significant
post-operation complication for orthopedic or orthopedic trauma
patients undergoing fracture fixation. Infections associated with
medical devices accounted for over 70% of all the orthopedic
infections (1), leading to infected
non-union or osteomyelitis with limited treatment options and a
heavy socio-economic impact (2).
Animal models are one of the most commonly used,
effective and valuable tools for research on implant-related
osteomyelitis. The model with intramedullary fixation proposed by
Worlock et al has been widely employed (3), but the intramedullary (IM) nail
described by Worlock lacks rotational stability, differing from
clinical cases where interlocking bolts are used (4).
In addition, at least 65% of all infections are
caused by the biofilm bacteria in the developed world (5,6).
Staphylococcal species are found to be the most prevalent
etiological agents of orthopedic infections, representing 75.3% of
all strains with S. aureus generally exhibiting the highest
prevalence (35.5% overall prevalence) (7). As a result of biofilm formation on the
implant surface, however, antibiotic treatment of the
staphylococcal species infections is often faced with failure
(8). The animal models of
osteomyelitis used to use planktonic bacterial cells as initial
inoculum, but with the advent of bacterial biofilm concept, the
limitation of planktonic bacterial inoculum and the important role
that biofilm bacteria play in osteomyelitis have been perceived
(9). Thus, a new model of
implant-related osteomyelitis has been proposed wherein a
well-established, mature biofilm is used as initial inoculum
instead of planktonic bacterial cells (10).
As a general rule, animal models should reflect the
clinical situation as much as possible for basic research on new
therapeutic options. Therefore, in order to improve the
above-mentioned problems, we aimed to establish a rabbit model of
osteomyelitis following plate fixation of femoral fracture with
initial inoculation by bacterial biofilm.
Materials and methods
Animals
A total of 24 male New Zealand White rabbits
(3.0–3.5 kg in weight; six months in average age) were randomly
divided into two groups. Group 2 (n=12) treated with biofilm served
as positive controls of infection and group 1 (n=12) treated
without biofilm as negative controls of infection. All animals were
kept in a single cage, supplied plenty food and water. All
operations were performed under good anesthesia. All procedures
performed in studies involving animals were in accordance with the
ethical standards of our institution's Institutional Animal Care
and Oversight Committee (Project SYXK No. 2015-0056, Southern
Medical University, Guangzhou, Guangdong, China).
Bacterial and implants
Staphylococcus aureus (ATCC 25923) was
provided by the Infectious Diseases Department of Nanfang Hospital;
316L stainless steel plates (35 mm in length, 6.5 mm in width and
2.0 mm in thickness) with 5 holes were used for fracture fixation.
Four screws (10 mm in length and 2.4 mm in diameter) were used to
fix each implant.
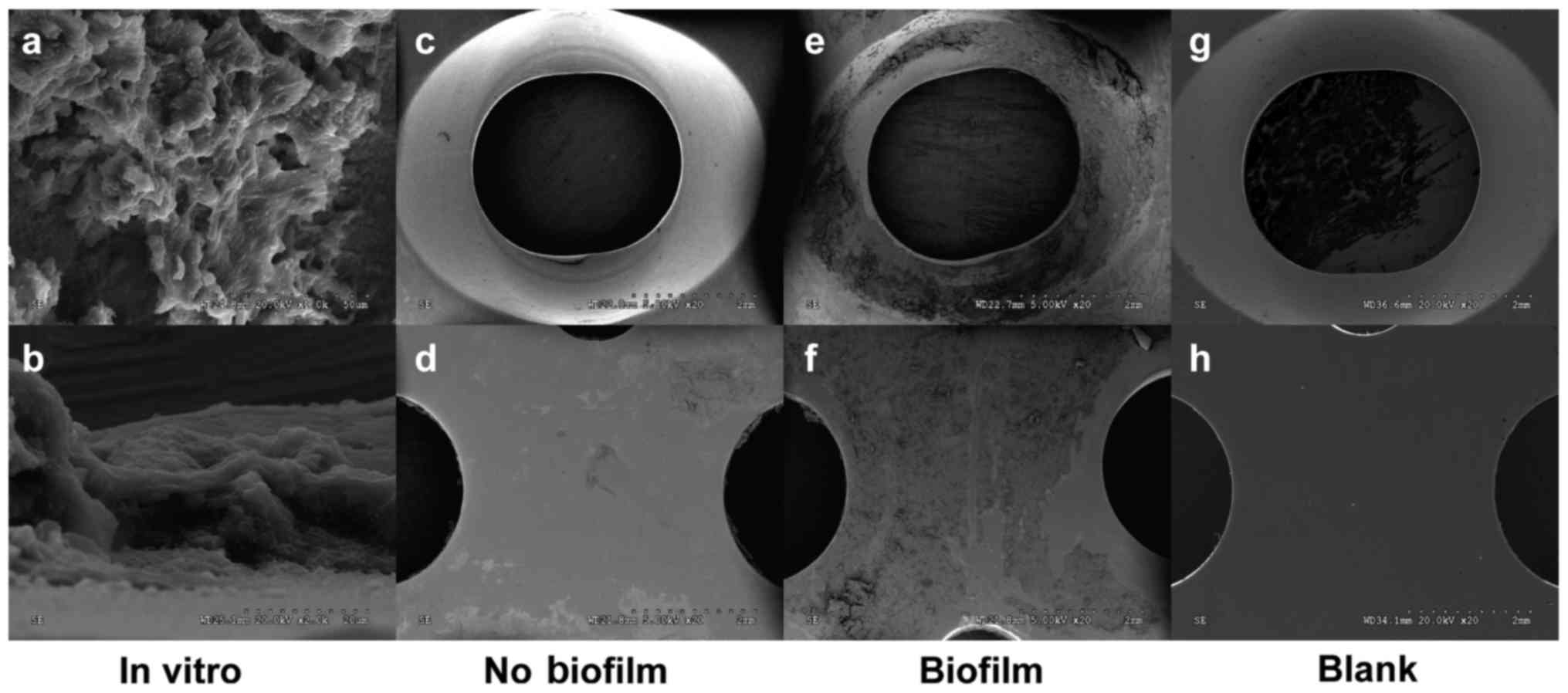
Biofilm growth
S. aureus was prepared by an overnight
culture in Luria-Bertani (LB) broth. Then the bacterial
concentration was adjusted to an OD600nm of 0.5,
corresponding to 108 CFU/ml by a microplate reader
(SpectraMax M5, Molecular Devices, USA). The concentration of S.
aureus in the inoculum and the OD suspension was confirmed by
colony forming unit (CFU) quantification of serially diluted
suspensions on agar. The bacterial suspension was then diluted
100-fold to 106 CFU/ml. Next, 5 ml of bacterial solution
and a piece of steel plate were placed into a 15 ml centrifuge
tube, and then the tube was incubated for 48 h at 37°C with shaking
(200 rpm) by a constant temperature shaking incubator. Finally, the
plate was taken out from the tube and washed 3 times with phosphate
buffer solution (PBS) to remove floating bacteria on the surface of
plate. The biofilm above the steel plate was observed by SEM
(Fig. 1).
Surgical procedure
Before surgery, the NZW rabbits were fasted for 12
h. They were anaesthetised using an intramuscular injection of 3%
pentobarbital sodium solution (1 ml/kg) in combination with
Xylazine Hydrochloride Injection (0.1 ml/kg).
The surgery was performed under strict aseptic
conditions. The surgical procedure for implant fixation was done
using a direct lateral approach to the middle femur as described
previously. After skin disinfection using povidone-iodine
(anerdian), a 3~4 cm long incision was made at the lateral aspect
of the middle right femur. Blunt separation was done along the
muscle gap to completely expose the femoral shaft. The pre-bent
plate (with or without biofilm, depending upon the animal group)
was rinsed with PBS 3 times and placed in front of the femoral
shaft and fixed with four screws. Then a fracture was created with
a 1 mm diameter wire saw at the area between the second and third
screws. The wound was rinsed with saline, closed in layers.
Postoperative monitoring extended until the animals could stand on
their own feet and eat and drink as well.
X-ray and micro-CT
X-rays of the femur were taken in all animals at day
0, 7, 14 and 21 post-surgery, to confirm the osteotomy and the
inflammatory changes of bone. After the animals were sacrificed and
the plates were removed on day 21 postoperatively, Micro-CT scan
was performed on the femur in order to observe and compare the
periosteal reaction, callus formation, osteolytic destruction and
absorption between the two groups.
Scanning electron micrography
(SEM)
After the animals were sacrificed on day 21, all the
plates were removed and washed 3 times with PBS. Six plates in each
group (group 1: 6 plates, group 2: 6 plates) were fixed with 2.5%
glutaraldehyde. After vacuum drying and sputter-coating with gold,
the specimens were assessed by a scanning electron microscope
operated (HITACHI S-3000N, Japan) at 5 kV. Through SEM, we directly
compared the biofilm growth on implant surface in the two
groups.
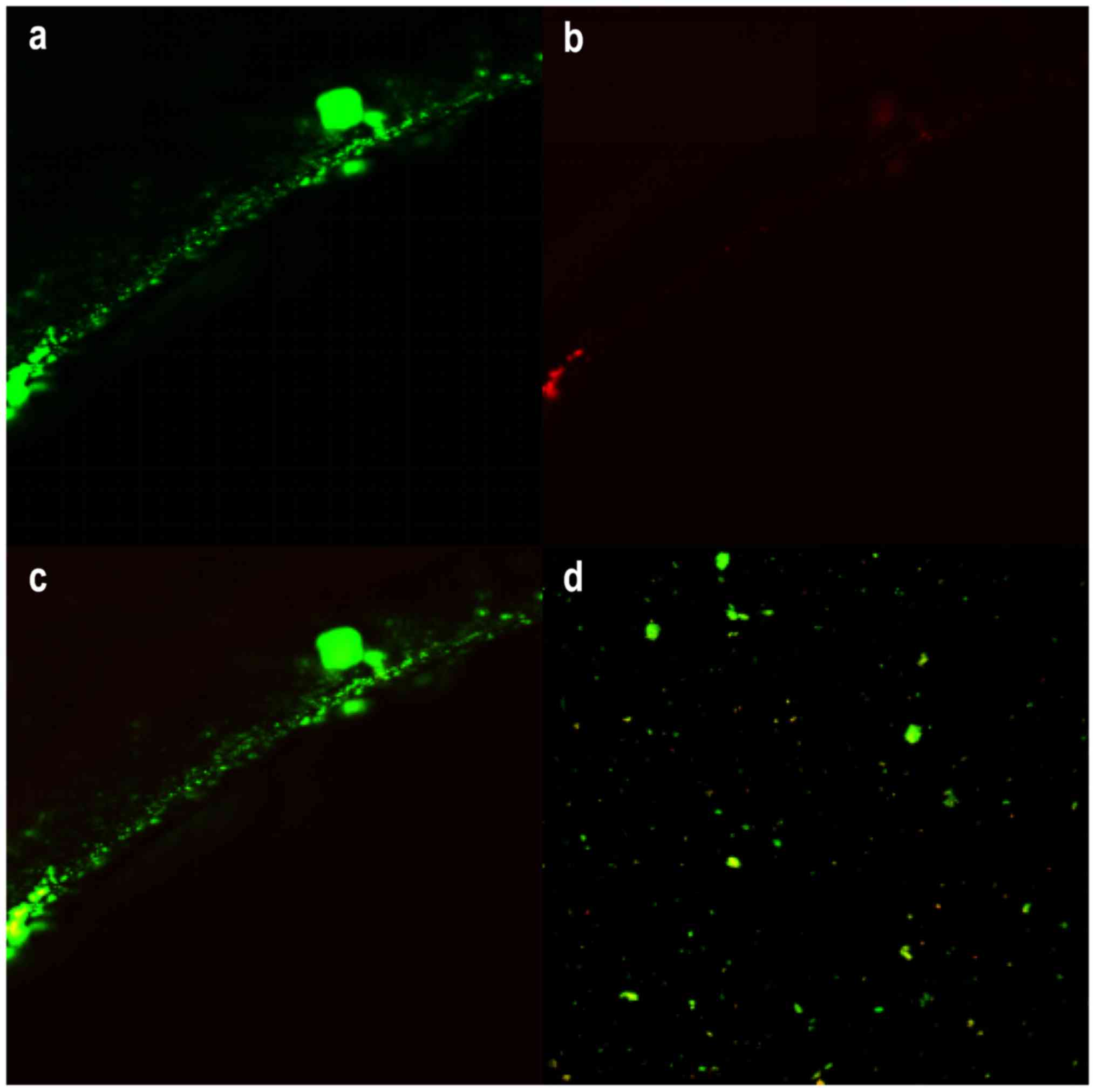
Confocal laser scanning microscopy
(CLSM)
The remaining plates (group 1: 6 plates, group 2: 6
plates) were subjected to bacterial semi-quantitative analysis
using LIVE/DEAD® Biofilm Viability Kit
(FilmTracer™, USA) by a confocal laser scanning
microscopy (Fluoview FV10i, Olympus). Ultrasonication was utilized
to release the bacteria in biofilms on the surface of the plate
(11). Directly after retrieval,
plates were placed in a 15 ml centrifuge tube containing 5 ml PBS.
All the tubes were vortexed for 30 sec using a Vortex-Genie and
then subjected to sonication at 40 kHz in a ultrasound bath for 5
min, followed by additional vortexing for 30 sec. Ultrasonication
at this frequency and duration has previously been demonstrated not
to affect the viability of Staphylococcus aureus (12). The solution was centrifuged at 3,000
rpm for 5 min and the supernatant discarded. Then 200 µl of
staining solution was added into the solution. The sample was
incubated for 20–30 min at room temperature, protected from light.
After centrifugation by addition of 5 ml of PBS again, the
supernatant was discarded; the solution was subsequently mixed with
5 ml PBS and 300 µl of the solution was observed in a confocal dish
with CLSM finally. The images were processed by software (ImageJ)
and transformed into optical density or area for data analysis.
Histology
After Micro-CT, the femurs were cut according to the
length of the plate and decalcified with EDMA before being
dehydrated with increasing concentrations of ethanol and embedded
in paraffin. Transverse slices (4 µm) were made through the screw
holes in the bone and stained with Hematoxylin & Eosin (HE).
The sections were examined for inflammatory cells, necrotic tissue,
and bone destruction. Specific parameters were assessed on the
basis of a modified Smeltzer's grading scale (10). Each parameter was scored on a
five-point scale (0–4), with 4 representing the most severe
evidence. All individual sections were scored by an independent,
outside, blinded observer.
Statistical analysis
Histology scores obtained for each individual
parameter were averaged to obtain a composite score for each
rabbit. SPSS 20 (IBM, USA) was used for the statistical analyses.
The data were checked for homogeneity of variance using levene's
test. Differences between groups were determined by
independent-sample t test (Student's t test) for parametric
two-tailed significance. The significance level was determined at
P<0.05. Graphical representation of the data was performed in
GraphPad Prism 6 (GraphPad, USA).
Results
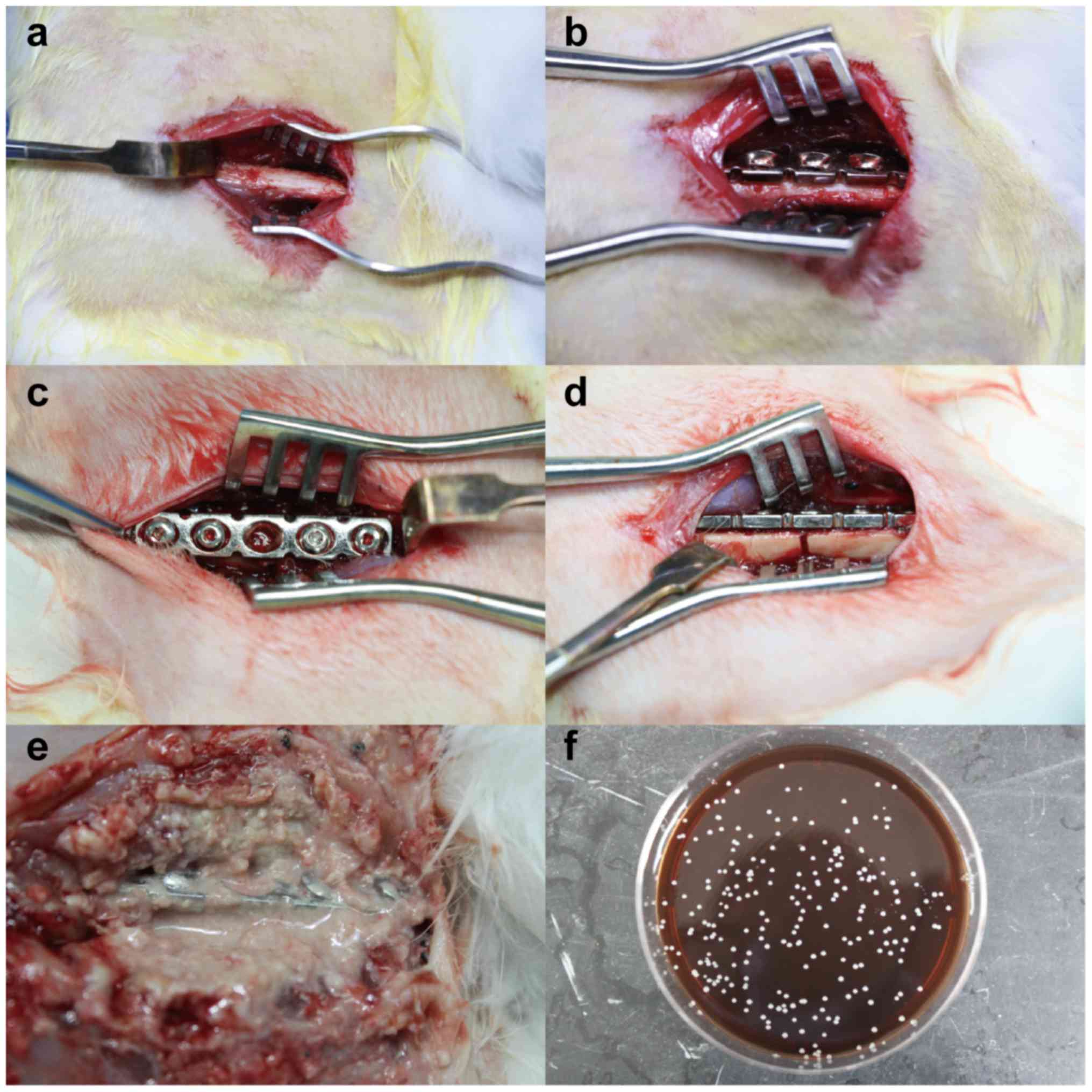
Clinical assessment
All animals were sacrificed at day 21 (Fig. 2). All animals in groups 2 showed
signs of soft tissue and bone infection with significant swelling,
pus formation and local tissue destruction (Fig. 2E). Three different points of the pus
were taken and painted on the agar plates. After cultured at 37°C
for 18 h, the plates on which colonies appeared were sent to a
clinical laboratory at Nanfang Hospital. Its automatic bacterial
identification instrument showed Staphylococcus aureus. Clear
instability of the plates and screws, a large amount of reactive
callus formation and no clinical fracture healing at the former
fracture site were observed in the 10 animals with biofilm
infected. In group 1 without biofilm all the animals showed stable
plate fixation with a moderate amount of healing callus.
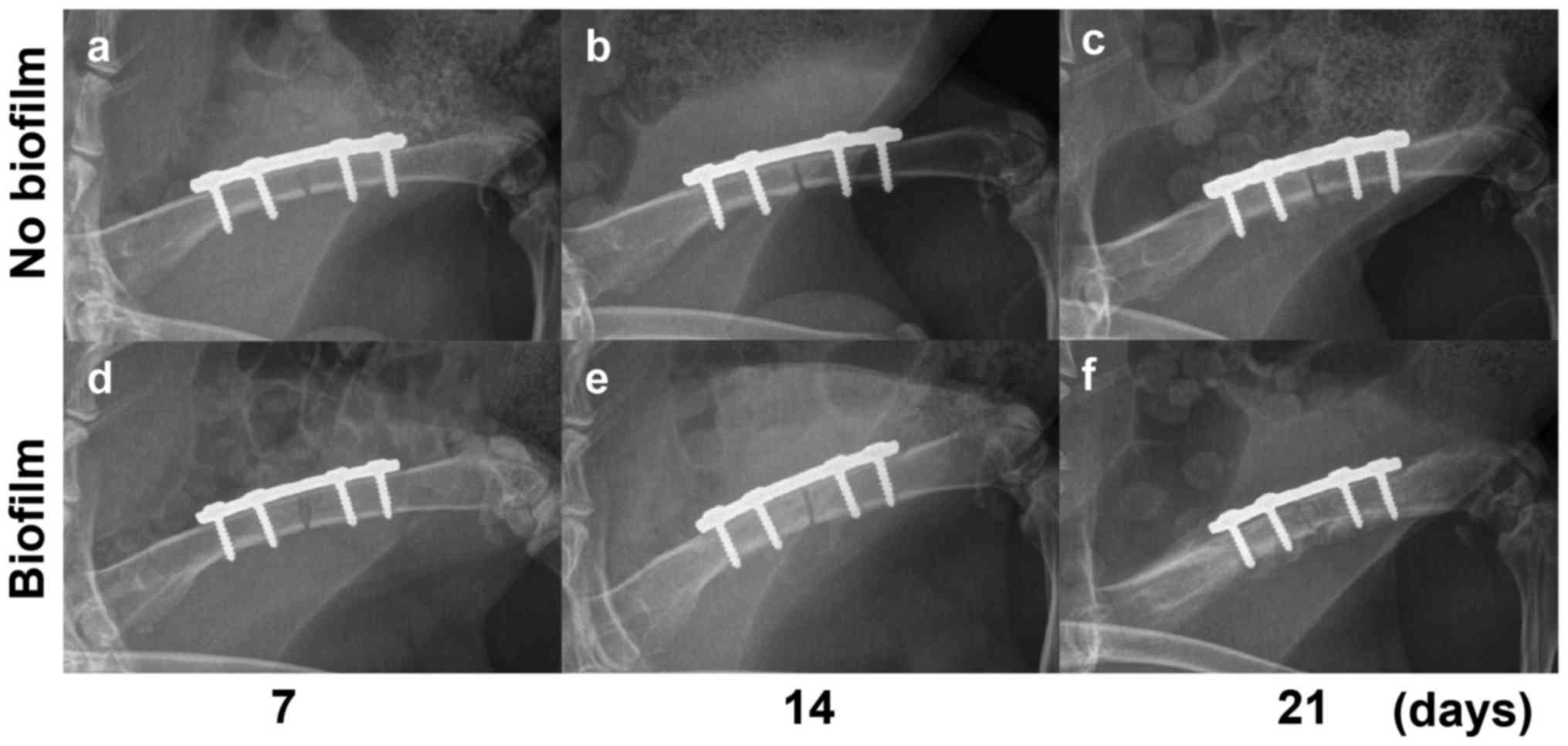
X-ray
The X-ray pictures showed stable internal fixation
without loosening on days 0 and 7, basically the same. The X-ray
results showed the rabbits without biofilm (group 1) had no
significant infection within 21 days, but only mild periosteal
reaction with no obvious infection at the third week (Fig. 3). Biofilm-infected rabbits (group 2)
showed only mild periosteal reaction on day 14 (Fig. 3E) which developed into diffuse
osteomyelitis in a week's time. On day 21, significant osteolysis
appeared around the implant in the rabbits of group 2 with severe
periosteal reaction away from the fracture (Fig. 3F).
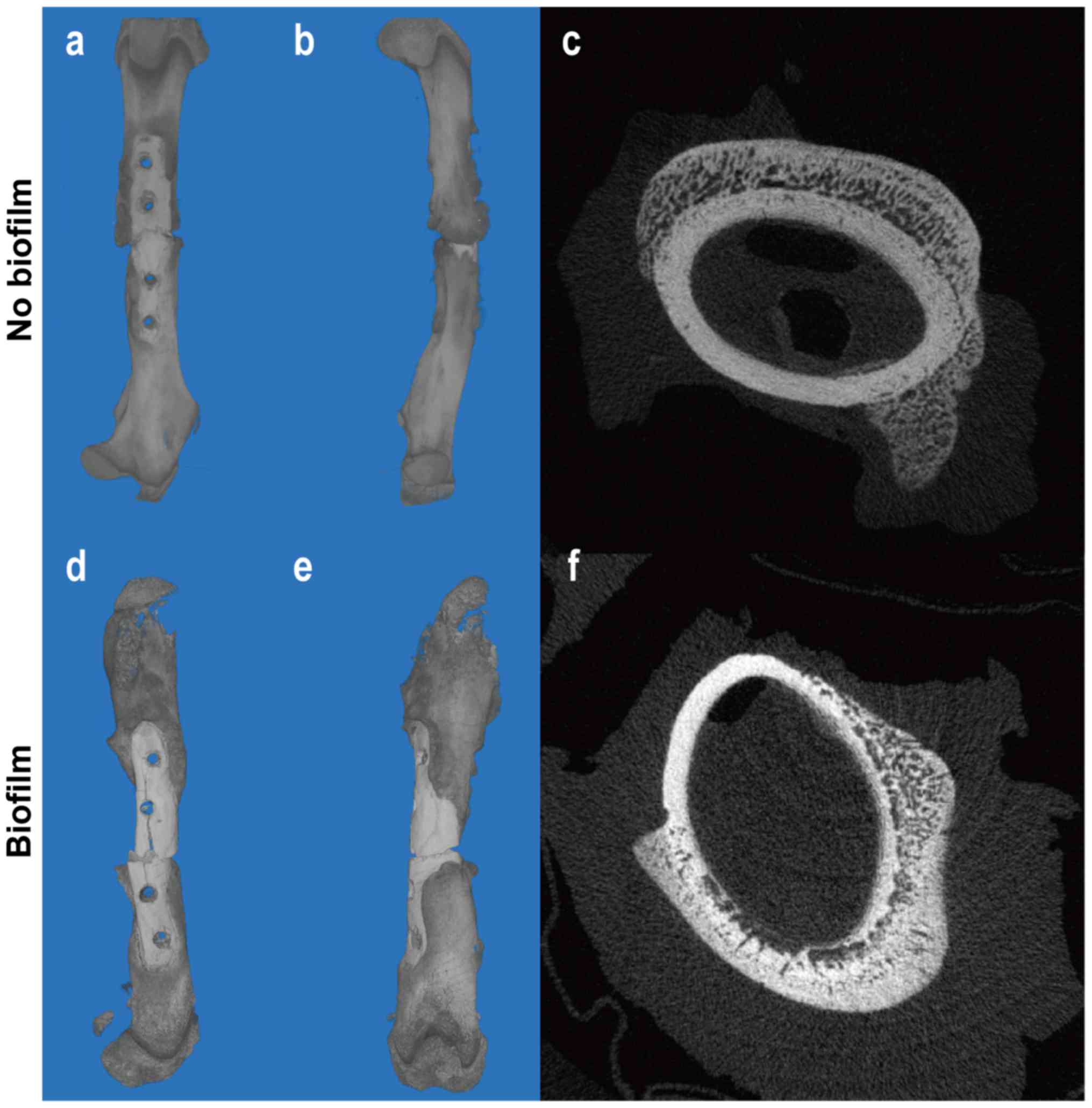
Micro-CT
In both infection and non-infection groups,
significant bone callus formation was observed (Fig. 4). In contrast to the control group
where the callus gathered around the fracture, the callus in the
infected group was far away from the fracture site [Fig. 4(a, b)]. This is because the severity
of inflammation varies from the proximal to the distal part of a
fracture. Studies have shown that inflammation at the distal part
of the fracture may be milder than that at the proximal part
(13), leading to more obvious
callus growth at the distal part. As we all know, the effect of
inflammation on the bone-formation is bi-directional. Mild
inflammatory response may stimulate osteogenesis while severe
inflammatory reaction inhibits or even destroys osteogenesis
(14). The cross-sectional images
showed although the two groups had callus formation outside the
cortex, destruction of the cortex dissolved occurred dramatically
in the infection group [Fig. 4(c,
f)].
Scanning electron micrography
Bacterial biofilm formed on the steel plate after 48
h culture in vitro; colonies of coccoid bacteria were
embedded in or under an extracellular matrix which was considered
as a bacterial biofilm (Fig. 1). The
same results were found in the biofilm-infected group, but the area
of biofilm was significantly increased. However, all the other
plates in the group without bacterial contamination were free of
biofilm formation.
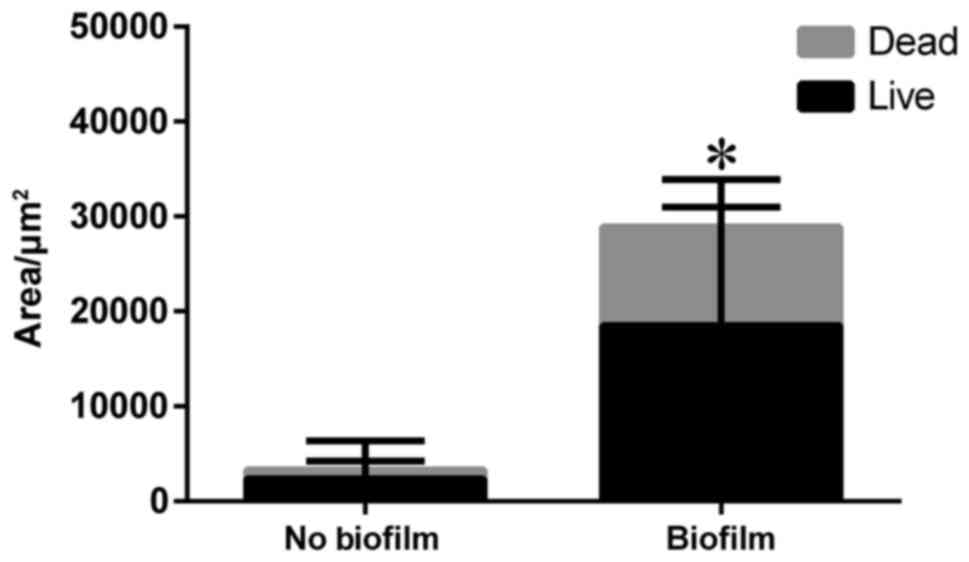
Confocal laser scanning
microscopy
LIVE/DEAD® Biofilm Viability Kit
(FilmTracer™, USA) utilizes mixtures of the
SYTO® 9 green fluorescent nucleic acid stain and the
red-fluorescent nucleic acid stain, propidium iodide. It allows
researchers to distinguish live and dead bacteria quickly, without
waiting for growth plate results. Because of the opaque steel
plate, only the edge of the screw hole could be observed to find
that live bacteria became green in fluorescence and dead red
(Fig. 5). Thus, we separated the
bacterial biofilm from the plate by ultrasonication to count the
area of the bacteria biofilm (Fig.
5D). There were evident statistical differences regarding the
biofilm area between the two groups (P<0.001) (Fig. 6).
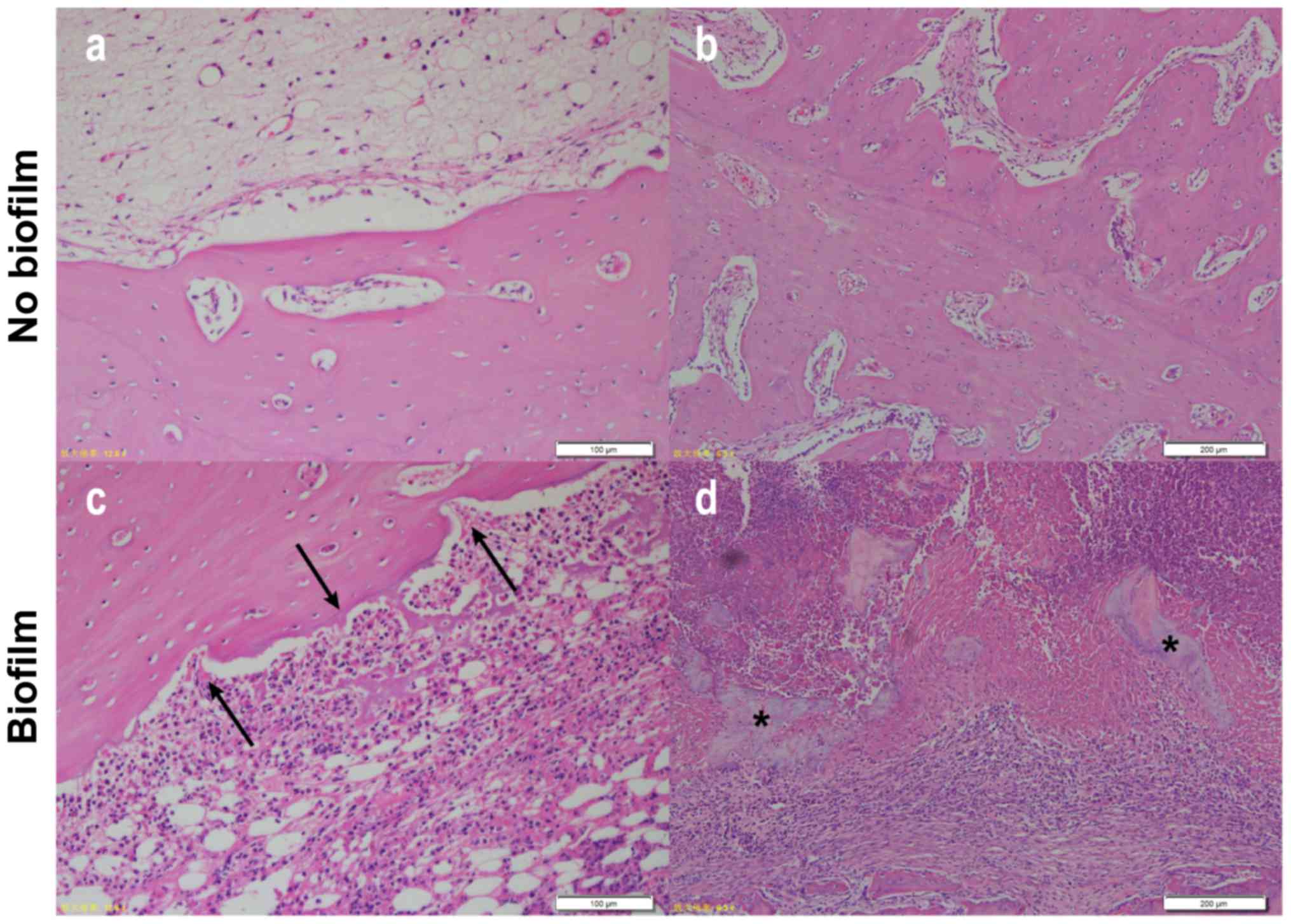
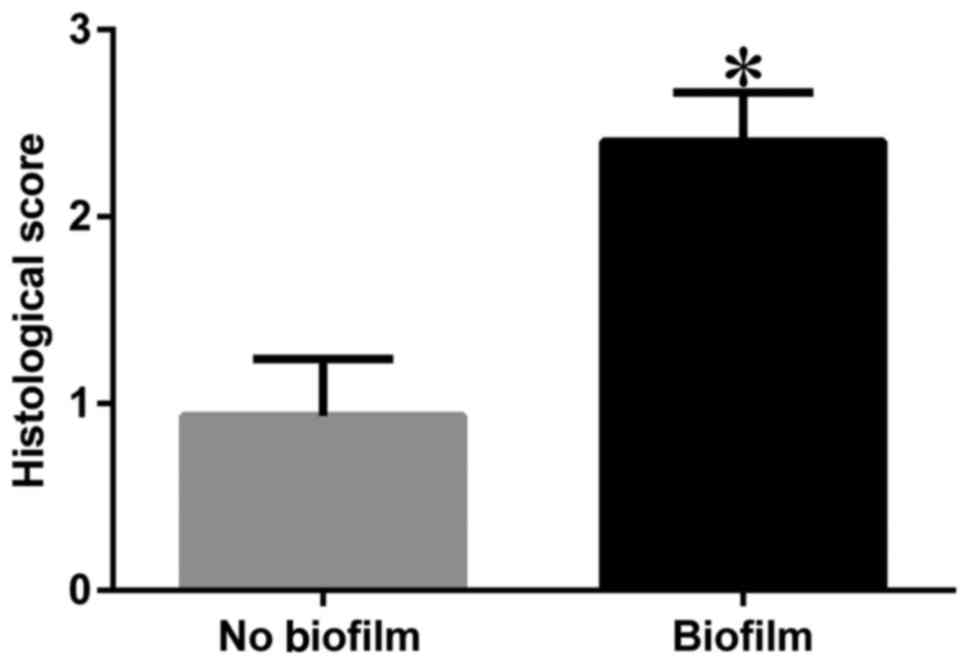
Histology
Sections stained with H&E showed an observable
difference between Group 1 and Group 2 rabbits. Cortical bone
growth and inflammatory response were not decisive indicators of
infection as the results suggested that they could be caused by
surgical trauma and infection; however, there was a notable
difference in the degree of response between the two groups in bone
morphology. Those that had infection showed a large amount of
inflammatory cell infiltration with signs of ‘moth eaten’ bone that
had jagged edges due to resorption/bacterial presence, whereas
those with a small amount of inflammatory cells due to surgical
trauma had little indication that resorption was occurring
(Fig. 7). More specifically,
scattered cell-free sequestrum was found in sections in the
infected group (Fig. 7D). The
histological scores of the two groups were significantly different
(P<0.001) (Fig. 8).
Discussion
The above experimental results demonstrate that all
the animals in the infection group presented with typical signs of
osteomyelitis and the difference between the experimental and
control groups was obvious. This animal model is stable,
reproducible and suitable for the study on treatment strategies for
osteomyelitis and antibacterial capacity of different materials,
and even suitable for observation of fracture healing. In addition
to improved repeatability and stability, our model also has an
advantage of reduced modeling time because it takes less time for
bacteria to proliferate and adhere to the surface of the plate and
form a mature biofilm in the presence of human body immune
reaction. In the present study, implant-related osteomyelitis
developed within 21 days in all the surviving rabbits in group 2
contaminated with biofilm bacterial inoculum, much sooner than 4–6
weeks reported by other relevant studies (3,15,16).
Since stability of internal fixation plays an
important role in reduction and fracture healing, the absence of
stability will have a negative effect on the outcomes of the
experiments using these animal models. Choice of steel plate
fixation may be a desirable solution to the absence of stability,
but most of the current animal models do not use internal fixation
with steel plate because osteotomy is not performed due to
insufficient rotational stability (17–20).
Currently, intramedullary fixation with a K-wire is widely used in
animal models of implant-related osteomyelitis (16). However, due to limitations in animal
size and equipment, such a fixation method apparently fails to
provide the stability required for fracture healing, and must have
an uncertain impact on the occurrence and development of infection.
This may lead to unsatisfactory experimental results, no matter
osteotomy is performed or not. Moreover, in clinic, surgeons
usually prefer plate fixation to intramedullary fixation for
patients with open fracture who still have a high possibility of
infection despite thorough debridement. Taking the above aspects
into account, the present study chose plate fixation to provide
stability of fracture, instead of intramedullary fixation. We
didn't create a fracture before pre-bent plate was fixed, due to
the difficulty of anatomical reduction, higher surgical failure
rate, as well as higher mortality of animals. Besides, although the
tibia is mainly utilized in the open fracture models (3,16,21), the
femoral shaft was selected as the location for plate fixation in
the present study because in anatomical morphology the rabbit
femoral shaft is flat with little pre-arch, unlike the triangular
prism of the tibia.
Most animal models of osteomyelitis primarily use an
initial inoculum of planktonic bacterial cells (15,19,22,23),
with an expectation that these planktonic cells will attach to the
surface of medical devices or to the surrounding tissue and
subsequently form a biofilm. However, according to Williams et
al (9), there may be three major
limitations which may accompany the use of bacteria in animal
models of osteomyelitis. (1)
Planktonic bacterial cells are more likely to be cleared by the
immune system than biofilm bacteria, and immune systems of animals
are innately more powerful than those of humans. (2) Planktonic bacteria are more susceptible
to antibiotics than cells residing in biofilm. >1,000 times of
the minimum inhibitory concentration are required to treat biofilm
infections (24). (3) The possibility exists for planktonic
bacteria to be diluted by animal body fluids, which may result in
insufficient concentration to attach to tissue or medical devices.
When we model osteomyelitis and perform early intervention with
antibiotics, the above limitations may lead to inconsistent
results, affecting the repeatability of infection development as
well as the effect of antibiotic treatment.
Since animal models with good reproducibility and
stability are designed to solve clinical problems, they should
simulate clinical settings as closely as possible. The
osteomyelitis animal model is an artificial confrontation between
the host immune system and bacterial virulence. The pure cultures
that have proven so valuable in the laboratory are virtually absent
in nature: >99.9% of bacteria exist in heterogeneous communities
called biofilms (25). As they can
form on nearly every surface, the bacteria on them, rather than
floating bacteria, are in action when contamination occurs. Animal
models inoculated with floating bacteria still need a process of
biofilm formation, but host immunity will have a strong resistance
to this process. This is the reasons why this modeling method is
unstable. Low concentrations of bacterial suspensions are not
sufficient to overcome host immunity, but high concentrations are
likely to overwhelm the host immunity completely, leading to high
mortality. In order to overcome these defects, we avoided
destructing host immunity by inoculating a biofilm on the surface
of an in vitro steel plate. We believe that the biofilm
bacteria which are in a relatively dormant state will not cause a
violent confrontation with host immunity so that the host has
enough time to get adapted to the gradual escalation of bacterial
virulence.
It has to be noticed that our method for quantifying
bacteria is not by conventional bacterial culture but by combining
CLSM with ImageJ software. This was because many studies confirmed
unsatisfactory effect of bacterial culture on the biofilm (1). The positive rate of traditional culture
is low and bacteria wrapped in the biofilm cannot be cultured. The
first method of semi-quantitative determination of biofilm was
developed by Christensen et al, measuring the absorbance of
biofilm stained with crystal violet (26). After continuous improvement,
spectrophotometry has become a widespread method for biofilm
evaluation, but the scarce specificity still limits its application
(27).
Despite the improvements, we also have shortcomings
in our study. As a result of the absence of comparison with the
inoculation of floating bacteria, we can not get a definite result
about any difference with this model between planktonic vs. biofilm
inocula, which is a serious deficiency in our study. We will
continue to explore their differences in our further study.
Although SEM is one of the most important tools to observe the
structure of bacterial biofilm, it can be used to observe only the
surface but not the internal composition and structure. Currently,
no objective measurements are available to distinguish the stages
of biofilm formation. This is indeed a limitation that is worth
exploring. Identifying early and mature biofilms and comparing them
with floating bacteria will be a chief concern of our future study.
Since the concern of this present study was to establish a novel
animal model with biofilms as initial inoculation to explore the
feasibility to improve the stability and repeatability of a
currently conventional animal model of osteomyelitis, but not to
compare the intervention factors for fracture fixation, we did not
establish an intramedullary fixation as another control group.
Moreover, Long-axial Multiplanar Reconstruction (MPR) images are
better and more realistic to show the callus and osteomyelitis than
three-dimensional reconstruction. Besides, our model only involved
biofilm as initial inoculum of S. aureus after plate fixation. In
fact, the occurrence and development of osteomyelitis is related to
a number of factors, such as material of the plate, species of the
bacterium, virulence of the bacterium and immune status of the
host. Although it appears that S. aureus will still be the primary
pathogen for osteomyelitis for a long time, the effect of other
pathogens should not be ignored, such as S. epidermidis, P.
aeruginosa and polymicrobial ones. Different bacteria may lead to
changes in the pathophysiology, making the experimental results
varied.
CLSM is one of the most sensitive and specific
methods for analysis of biofilm structures, and for determination
of bacterial survival as well. However, limited by the confocal
microscopy (Fluoview FV10i, Olympus) we used, most areas of the
steel plate could not be observed, except for the edges irradiated
by the laser. Therefore, we used ultrasonic method, as previously
mentioned, to remove the biofilm from the plates before we
performed a semi-quantitative analysis with CLSM. However, our CLSM
remains a very worthwhile attempt; some scientists have made it
possible to measure biomass volume with CLSM improved by computer
technology (28). We hope to make up
for this shortcoming in the future experiment.
Conclusion
The results show that we have successfully
established a rabbit model of infection after open fracture
fixation. We believe that our model is an improvement of the
previous model. The primary benefit of this model lies in its
stability and repeatability, and its good simulation of clinical
conditions as well. It can be used to replace traditional models,
but does not seem to have a very direct impact on how to improve
clinical care and patient outcomes. However, when the stability and
repeatability is improved, our new model helps to produce more
accurate experimental results, though the effects of our improved
model are not obvious at present. We hope that this animal model
could be verified and further improved by more studies.
Acknowledgements
The authors thank Professor Liang and all the staff
in the Key Laboratory of Bone and Cartilage Regenerative Medicine,
Nanfang Hospital of Southern Medical University. This work was
supported by the National Natural Science Foundation of China
[grant nos. 2016B090913004/201508020035].
References
|
1
|
Arciola CR, Campoccia D, Ehrlich GD and
Montanaro L: Biofilm-based implant infections in orthopaedics. Adv
Exp Med Biol. 830:29–46. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Metsemakers WJ, Kuehl R, Moriarty TF,
Richards RG, Verhofstad MH, Borens O, Kates S and Morgenstern M:
Infection after fracture fixation: Current surgical and
microbiological concepts. Injury. Sep 11–2016.(Epub ahead of
print). View Article : Google Scholar
|
|
3
|
Worlock P, Slack R, Harvey L and Mawhinney
R: An experimental model of post-traumatic osteomyelitis in
rabbits. Br J Exp Pathol. 69:235–244. 1988.PubMed/NCBI
|
|
4
|
Reizner W, Hunter JG, O'Malley NT,
Southgate RD, Schwarz EM and Kates SL: A systematic review of
animal models for Staphylococcus aureus osteomyelitis. Eur Cell
Mater. 27:196–212. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Donné J and Dewilde S: The challenging
world of biofilm physiology. Adv Microb Physiol. 67:235–292. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Costerton JW: Cystic fibrosis pathogenesis
and the role of biofilms in persistent infection. Trends Microbiol.
9:50–52. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Montanaro L, Speziale P, Campoccia D,
Ravaioli S, Cangini I, Pietrocola G, Giannini S and Arciola CR:
Scenery of Staphylococcus implant infections in orthopedics. Future
Microbiol. 6:1329–1349. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Trampuz A and Zimmerli W: Diagnosis and
treatment of infections associated with fracture-fixation devices.
Injury. 37 Suppl 2:S59–S66. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Williams DL and Costerton JW: Using
biofilms as initial inocula in animal models of biofilm-related
infections. J Biomed Mater Res B Appl Biomater. 100:1163–1169.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Williams DL, Haymond BS, Woodbury KL, Beck
JP, Moore DE, Epperson RT and Bloebaum RD: Experimental model of
biofilm implant-related osteomyelitis to test combination
biomaterials using biofilms as initial inocula. J Biomed Mater Res
A. 100:1888–1900. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Trampuz A, Piper KE, Jacobson MJ, Hanssen
AD, Unni KK, Osmon DR, Mandrekar JN, Cockerill FR, Steckelberg JM,
Greenleaf JF and Patel R: Sonication of removed hip and knee
prostheses for diagnosis of infection. N Engl J Med. 357:654–663.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Monsen T, Lövgren E, Widerström M and
Wallinder L: In vitro effect of ultrasound on bacteria and
suggested protocol for sonication and diagnosis of prosthetic
infections. J Clin Microbiol. 47:2496–2501. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rochford ET, Sabaté Brescó M, Zeiter S,
Kluge K, Poulsson A, Ziegler M, Richards RG, O'Mahony L and
Moriarty TF: Monitoring immune responses in a mouse model of
fracture fixation with and without Staphylococcus aureus
osteomyelitis. Bone. 83:82–92. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Glass GE, Chan JK, Freidin A, Feldmann M,
Horwood NJ and Nanchahal J: TNF-alpha promotes fracture repair by
augmenting the recruitment and differentiation of muscle-derived
stromal cells. Proc Natl Acad Sci USA. 108:1585–1590. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kishor C, Mishra RR, Saraf SK, Kumar M,
Srivastav AK and Nath G: Phage therapy of staphylococcal chronic
osteomyelitis in experimental animal model. Indian J Med Res.
143:87–94. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Odekerken JC, Arts JJ, Surtel DA,
Walenkamp GH and Welting TJ: A rabbit osteomyelitis model for the
longitudinal assessment of early post-operative implant infections.
J Orthop Surg Res. 8:382013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Moriarty TF, Campoccia D, Nees SK, Boure
LP and Richards RG: In vivo evaluation of the effect of
intramedullary nail microtopography on the development of local
infection in rabbits. Int J Artif Organs. 33:667–675.
2010.PubMed/NCBI
|
|
18
|
Norden CW: Experimental osteomyelitis. I.
A description of the model. J Infect Dis. 122:410–418. 1970.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shiels SM, Bedigrew KM and Wenke JC:
Development of a hematogenous implant-related infection in a rat
model. BMC Musculoskelet Disord. 16:2552015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Arens S, Kraft C, Schlegel U, Printzen G,
Perren SM and Hansis M: Susceptibility to local infection in
biological internal fixation. Experimental study of open vs
minimally invasive plate osteosynthesis in rabbits. Arch Orthop
Trauma Surg. 119:82–85. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Alt V, Lips KS, Henkenbehrens C, Muhrer D,
Cavalcanti Oliveira MC, Sommer U, Thormann U, Szalay G, Heiss C, et
al: A new animal model for implant-related infected non-unions
after intramedullary fixation of the tibia in rats with fluorescent
in situ hybridization of bacteria in bone infection. Bone.
48:1146–1153. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Svensson S, Trobos M, Hoffman M, Norlindh
B, Petronis S, Lausmaa J, Suska F and Thomsen P: A novel soft
tissue model for biomaterial-associated infection and
inflammation-Bacteriological, morphological and molecular
observations. Biomaterials. 41:106–121. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
dos Reis JA Jr, de Carvalho FB, Trindade
RF, de Assis PN, de Almeida PF and Pinheiro AL: A new preclinical
approach for treating chronic osteomyelitis induced by
Staphylococcus aureus: In vitro and in vivo study on photodynamic
antimicrobial therapy (PAmT). Laser Med Sci. 29:789–795. 2014.
View Article : Google Scholar
|
|
24
|
Gnanadhas DP, Elango M, Janardhanraj S,
Srinandan CS, Datey A, Strugnell RA, Gopalan J and Chakravortty D:
Successful treatment of biofilm infections using shock waves
combined with antibiotic therapy. Sci Rep. 5:174402015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wimpenny J, Manz W and Szewzyk U:
Heterogeneity in biofilms. FEMS Microbiol Rev. 24:661–671. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Christensen GD, Simpson WA, Younger JJ,
Baddour LM, Barrett FF, Melton DM and Beachey EH: Adherence of
coagulase-negative staphylococci to plastic tissue culture plates:
A quantitative model for the adherence of staphylococci to medical
devices. J Clin Microbiol. 22:996–1006. 1985.PubMed/NCBI
|
|
27
|
Vassena C, Fenu S, Giuliani F, Fantetti L,
Roncucci G, Simonutti G, Romanò CL, De Francesco R and Drago L:
Photodynamic antibacterial and antibiofilm activity of RLP068/Cl
against Staphylococcus aureus and Pseudomonas aeruginosa forming
biofilms on prosthetic material. Int J Antimicrob Agents. 44:47–55.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Drago L, Agrappi S, Bortolin M, Toscano M,
Romanò C and De Vecchi E: How to study biofilms after microbial
colonization of materials used in orthopaedic implants. Int J Mol
Sci. 17:2932016. View Article : Google Scholar : PubMed/NCBI
|