Introduction
Delayed pregnancy, pregnancy complications,
oligohydramnion, and placental dysfunction are common clinical
indications of labor induction (1).
Cervical ripening is an important indicator of timing labor
induction.
Methods promoting cervical ripening include drugs
such as oxytocin and prostaglandin preparations and mechanical
methods such as water sac. Dinoprostone is a kind of prostaglandin
E2 preparation, which should be locally applied and can
be slowly and continuously released, and it has been clinically
proven safe and effective (2). The
disadvantages include that it easily causes excessive uterine
stimulation and frequent uterine contractions, thus increasing the
probabilities of fetal distress in the uterus and amniotic fluid
contamination (3). The double
balloon catheter (Cook) is widely applied to promote cervical
ripening, but it is relatively more expensive (4). The main working principle of the
domestic single balloon catheter (disposable balloon cervical
dilator) is that balloon stresses in the catheter and cervix
stimulate the cervical canal such that the synthesis of local
cervix is accelerated and endogenous prostaglandins are released,
thus promoting cervical softening and ripening (5).
Labor induction in late-term pregnancy can
significantly increase the body's stress and inflammatory
responses, and the mechanical operation of a single balloon
catheter or dinoprostone chemical reaction can further exacerbate
the body's stress and inflammatory responses, thus affecting the
outcome of perinatal maternal pregnancy to a certain degree.
This study aimed to evaluate the application effect
of a single balloon catheter and dinoprostone on cervical ripening
in pregnant women in late-term pregnancy and their influences on
stress and inflammatory responses.
Patients and methods
Data from patients
A total of 160 pregnant women diagnosed with
late-term pregnancy in Affiliated Hospital of Jining Medical
University (Shandong, China) from January, 2016 to May, 2017, were
continuously selected. Inclusion criteria for the study were: i)
Patients with indications of labor induction but without history of
cervical surgery as well as internal and surgical complications.
ii) Patients with cervical Bishop score ≤6 points and with
responses in the test without stress. iii) Patients who
participated in this research, signed the informed consent and had
complete clinical data. Exclusion criteria for the study included
patients who suffered from premature ruptures of membranes, vaginal
infections, placenta previa or other abnormal pregnancies. The
study was approved by the Ethics Committee of The Affiliated
Hospital of Jining Medical University.
According to the order of admission, the random
number method was used to divide the patients into the control
group (n=80) and the observation group (n=80). The baseline data of
patients in the two groups were comparable (Table I).
 | Table I.Comparison of baseline data of
patients in the two groups. |
Table I.
Comparison of baseline data of
patients in the two groups.
| Group | Control group
(n=80) | Observation group
(n=80) | t/χ2 | P-value |
|---|
| Age (years old) | 25.3±4.4 | 24.9±4.2 | 0.195 | 0.867 |
| Pregnancy time
(week) | 38.5±2.3 | 38.9±2.6 | 0.098 | 0.946 |
| Reason for labor
induction [case (%)] |
|
| 1.133 | 0.769 |
| Delayed
pregnancy | 9 (11.25) | 6 (7.50) |
|
|
| Pregnancy
complications | 34 (42.50) | 36 (45.00) |
|
|
| Oligohydramnion | 30 (37.50) | 33 (41.25) |
|
|
| Placental
dysfunction | 7 (8.75) | 5 (6.25) |
|
|
| Bishop score | 3.4±0.5 | 3.3±0.4 | 0.065 | 0.957 |
Research methods
The research was completed by the same surgery,
midwifery and nursing teams. Patients in the control group received
the labor induction by administration of dinoprostone [dinoprostone
suppositories, 10 mg, H20090484; Controlled Therapeutics (Scotland)
Ltd., Glasgow, Scotland] at the vaginal vault. Specifically, the
bladder lithotomy position of pregnant women was disinfected, and
dinoprostone was inserted into the vaginal vault. The pregnant
women were horizontally laid at 90° and rested in a bed for 30 min.
The Bishop method was used to assess cervical ripening. The
emergence of labor, rupture of membranes, rigid and intense uterine
contraction, fetal distress in uterus, nausea and vomiting of
pregnant women and other reactions indicated that there was a need
to immediately remove the drug. If the cervix was not ripened 24 h
after dinoprostone was inserted, intravenous dropping of oxytocin
(1 ml: 5 units; National Medicine Permission no. H31020862;
Shanghai Pharma No. 1 Biochemical and Pharmaceutical Co., Ltd.,
Shanghai, China) could be combined. Patients with regular uterine
received a contraction response test to determine changes in the
fetal heart rate. As long as there was a regular uterine
contraction, drugs were discontinued, regardless of the state of
the cervix.
Patients in the observation group received labor
induction by domestic single balloon catheters (Jiangsu Aiyuan
Medical Technology Corp., Jiangsu, China). The lithotomy position
was disinfected, the cervix was exposed by bivalve speculum, and
the balloon catheter was inserted into the cervical canal to the
depth of approximately 10 cm using oval forceps without teeth.
Sterile saline (150 ml) was added using a syringe, and the end of
catheter was pasted with anti-allergy adhesive plasters. Pregnant
women were free to move; balloons came out on their own after the
natural labor, or were removed 12 h after the insertion. Finally,
the Bishop score was assessed.
Observation indicators
Cervical ripening (Bishop score), means of
pregnancy, the total stage of labor, maternal and child
complications, and Apgar scores of newborn infants at 1 min after
delivery in the two groups were compared, in which the Bishop score
was graded according to the following parameters: 0 point for the
opening size of the cervix equal to 0 cm, 1 point for 1–2 cm, 2
points for 3–4 cm and 3 points for 5–6 cm; 0 point for 0–30%
degraded cervical canals, 1 point for 40–50%, 2 points for 60–70%
and 3 points for 80–100%; 0 point for the station of presentation
part being −3, 1 point for −2, 2 points for −1-0 and 3 points for
+1-+2; 0 point for the cervical hardness being hard, 1 point for
medium-hard and 2 points for soft; 0 point for the orifice of the
uterus being the rear, 1 point for central position and 2 points
for forepart. The final score was the sum of each score.
The levels of cortisol (COR), norepinephrine (NE)
and β-endorphin (β-EP) were measured by radioimmunoassay at
prenatal and postpartum 12, 24 and 48 h. The levels of C-reactive
protein (CRP), interleukin-6 (IL-6) and tumor necrosis factor-α
(TNF-α) were measured by enzyme-linked immunosorbent assay (ELISA).
Radioimmunoassay reagents were purchased from Jiangsu Beyotime
Biotechnology Co., Ltd. (Jiangsu, China) and ELISA reagents were
purchased from Beijing Zhong Shan Golden Bridge Biological
Technology Co., Ltd. (Beijing, China). The detection was performed
3 times according to the procedures in the instructions, and the
average value was calculated.
Statistical methods
Statistical analysis was performed using Statistical
Product and Service Solutions (SPSS) 20.0 software (SPSS Inc.,
Chicago, IL, USA). The measurement data were expressed as mean ±
standard deviation. The independent sample t-test was used for
intergroup comparisons, and repeated-measures analysis of variance
or paired sample t-test (used for comparisons at two different
time-points, such as Bishop score) was used for comparisons at
different time-points. Enumeration data are represented as case or
(%), and the χ2 test was used for intragroup
comparisons. P<0.05 indicated that the difference was
statistically significant.
Results
Cervical Bishop score, the total stage
of labor and Apgar scores of newborn infants at 1 min after
delivery
Cervical Bishop scores in the two groups after
intervention were significantly higher than those before
intervention, and the score of the observation group was
significantly higher than that of the control group, and the
difference was statistically significant (P<0.05). The total
stage of labor of the observation group was significantly
shortened, and the Apgar score of the newborn infant at 1 min after
delivery was increased. The differences were statistically
significant (P<0.05) (Table
II).
 | Table II.Comparison of cervical Bishop score,
the total stage of labor and Apgar scores of newborn infants at 1
min after delivery. |
Table II.
Comparison of cervical Bishop score,
the total stage of labor and Apgar scores of newborn infants at 1
min after delivery.
| Group | Bishop score | Total stage of labor
(min) | Apgar score |
|---|
| Control group
(n=80) | 10.9±1.8 | 460±80 | 9.3±0.4 |
| Observation group
(n=80) | 12.5±2.1 | 430±75 | 9.7±0.5 |
| t-value | 4.686 | 4.435 | 4.258 |
| P-value | 0.025 | 0.032 | 0.036 |
Means of pregnancy and
complications
The delivery rate of cesarean section in the
observation group was lower than that in the control group, the
overall incidence rate of perinatal complications was decreased,
and the differences were statistically significant (P<0.05)
(Table III).
 | Table III.Comparisons of means of pregnancy and
the incidence rate of complications [case (%)]. |
Table III.
Comparisons of means of pregnancy and
the incidence rate of complications [case (%)].
| Group | Cesarean section | Postpartum
hemorrhage | Precipitate
labor | Abnormal fetal heart
rate | Amniotic fluid
contamination | Neonatal
asphyxia | Total
complication |
|---|
| Control group
(n=80) | 20 (25.00) | 1 (1.25) | 7 (8.75) | 2 (2.50) | 2 (2.50) | 1 (1.25) | 13 (16.25) |
| Observation group
(n=80) | 9 (11.25) | 0 | 2 (2.50) | 1 (1.25) | 1 (1.25) | 0 | 4 (5.00) |
| χ2 | 5.096 |
|
|
|
|
| 5.331 |
| P-value | 0.024 |
|
|
|
|
| 0.021 |
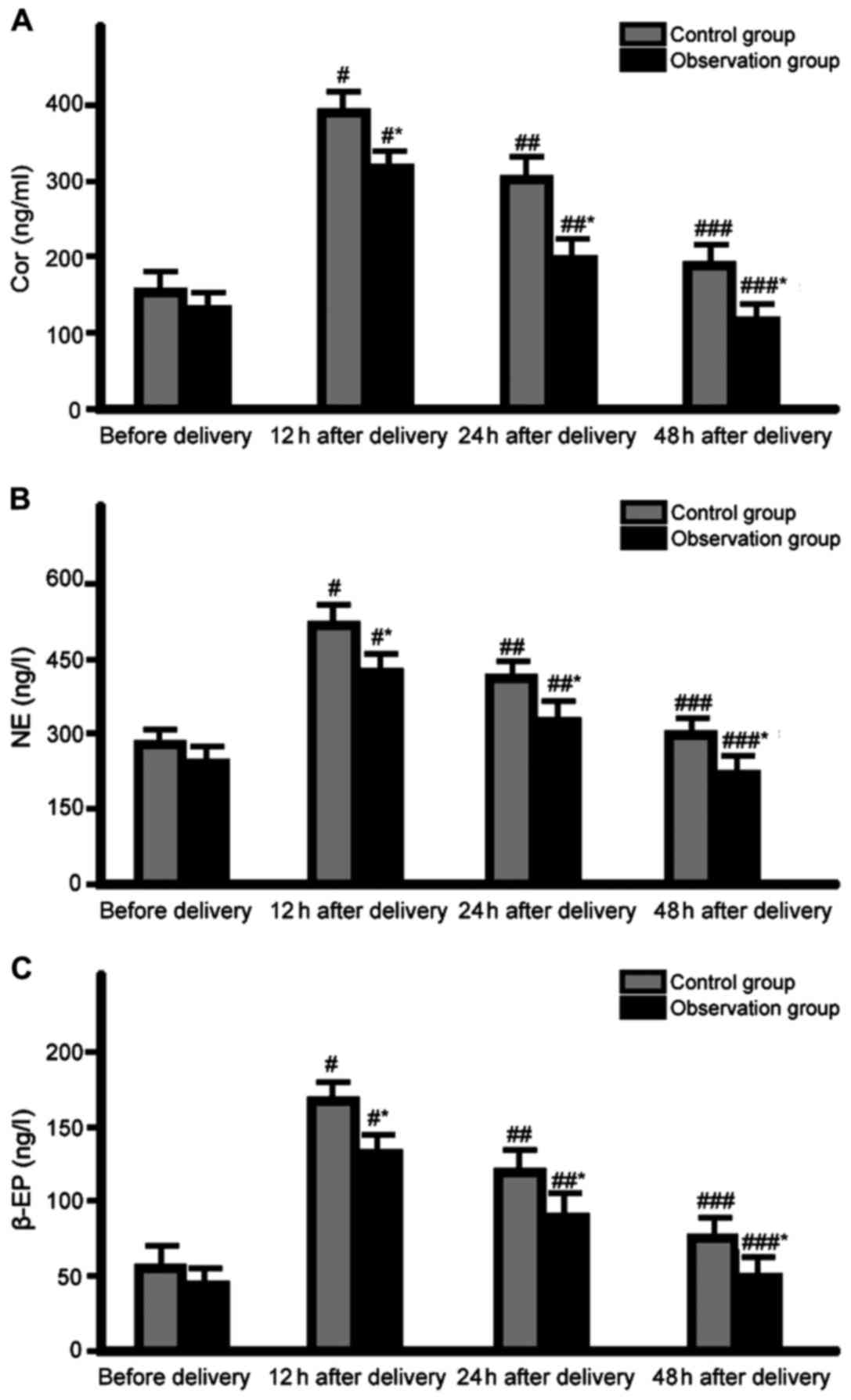
Comparison of stress responses
The levels of stress response markers at 12 h after
delivery in the two groups reached the peak, and then decreased
(P<0.05). The levels of stress response markers at each
time-point after delivery in the observation group were
significantly lower than those in the control group, and the
difference was statistically significant (P<0.05) (Fig. 1).
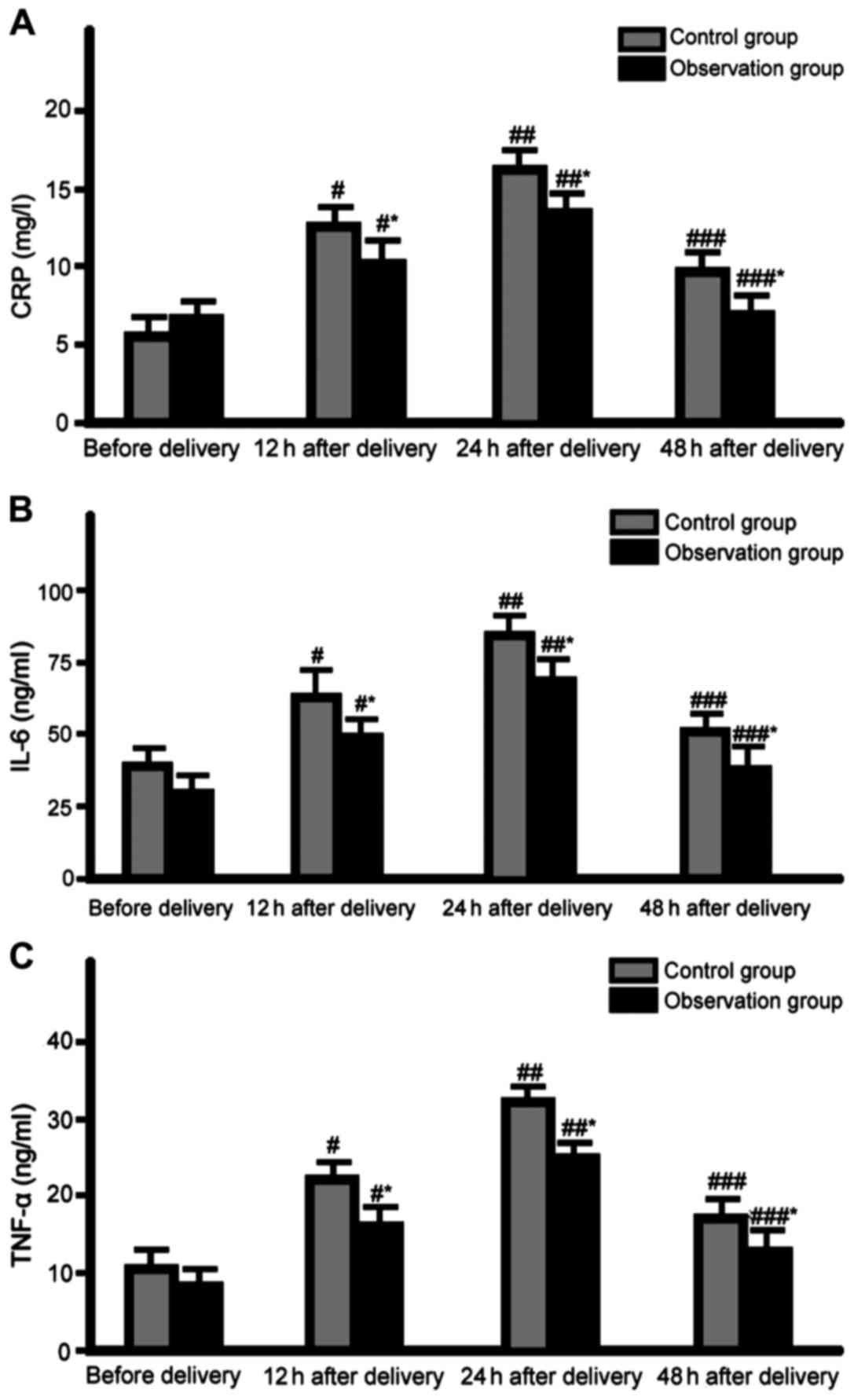
Comparison of inflammatory
responses
The levels of inflammatory response markers at 24 h
after delivery in the two groups reached the peak, and then
declined (P<0.05). The levels of inflammatory response markers
at each time-point after delivery in the observation group were
significantly lower than those in the control group, and the
difference was statistically significant (P<0.05) (Fig. 2).
Discussion
The study results showed that cervical ripening of
the observation group was significantly improved, the total stage
of labor was significantly shortened, the Apgar score of the
newborn infant at 1 min after delivery, and the delivery rate of
cesarean section and the incidence rate of perinatal complications
were decreased in the observation group. The levels of stress and
inflammatory responses at 12, 24 and 48 h after delivery in the
observation group were significantly lower than those in the
control group. Therefore, we believe that the single balloon
catheter promotes cervical ripening, improves pregnancy outcomes
and reduces stress and inflammatory responses in pregnant women in
late-term pregnancy, and is better than dinoprostone and has better
application and promotion values.
Previous findings (6–8) have
confirmed that the single balloon catheter produces mild mechanical
expansion by taking advantage of water sacs, stimulates endogenous
prostaglandin secretion, promotes cervical dilatation, stimulates
the release of oxytocins from local plexus of the cervix, assists
the expansion of the cervix and promotes the synthesis of cervical
tissue collagen and ripening. The single balloon catheter
significantly improves the comfort level of pregnant women, and can
also directly participate in the active stage, thus shortening the
total stage of labor and reducing the pain of delivery. The balloon
catheter is not restricted after insertion; thus, there is no need
for special observation. If abnormalities appear, it can be easily
removed at any time. Drugs are not required in the total stage, and
the catheter is easily accepted. It also shortens the hospital stay
and reduces hospital costs. Single balloon catheter may cause
relatively weaker cervical contraction, which does not affect the
rest, and its stage of labor is basically consistent with that of
normal labor. It has been reported that single balloon catheter can
cause reproductive tract infection after insertion; thus, strict
aseptic operation is imperative (9).
A recent study has confirmed that the effect of cervical single
balloon expansion in promoting cervical ripening is relatively
better, and it can effectively shorten the stage of labor and
improve the natural delivery rate with high safety (10). Cervical expansion of a single balloon
catheter has a higher natural labor rate and lower delivery rate of
cesarean section than that of the double balloon catheter,
rendering the former more suitable for clinically promoting
cervical ripening (11).
Both cesarean section and vaginal delivery are
traumatic stress response sources, which lead to abnormal
excitement of the maternal hypothalamus-pituitary-adrenal axis,
secretion of a large number of COR, NE and β-EP, regulate the body
stress response and participate in energy metabolism, body
temperature regulation and other physiological processes (12,13).
COR, NE and β-EP are important indicators of body stress responses
with high sensitivity (12). The
stress response not only improves maternal delivery power, but also
reduces postpartum immunity, which is an important reason for
puerperal infection and postpartum hemorrhage (13). At the same time, the maternal stress
response is maintained at peak level, which is also an important
risk factor for postpartum anxiety and depression (14). The peak levels of these indicators
appear at postpartum 12 h, which is consistent with the time of the
peak level of postpartum complications, suggesting that stress
responses play important roles in postpartum complications.
Inflammatory responses exist in the entire process of delivery. CRP
is a very sensitive indicator reflecting the level of inflammation
in the body, which can be rapidly increased in the early stage, and
its increased degree and duration are often closely associated with
disease severity and clinical prognosis (15). IL-6 is a key molecule for triggering
and promoting the cascade reaction of inflammation, a chemotactic
mediator of other inflammatory cells and a proinflammatory factor
of other inflammatory factors (16).
TNF-α is an inflammatory factor for regulating nuclear
transcription by the body. Extracellular signals activate TNF-α
activity, and then transfer it into the nucleus, mediate multiple
signal transduction pathways and affect the downstream target gene
transcription and target protein translation process to play
corresponding cytological roles (17). The peak level of inflammatory
responses appears at postpartum 24 h, suggesting that inflammatory
responses may be closely related to stress responses, and stress
responses may be driving powers of the persistent existence of
inflammatory responses (18).
In conclusion, the effect of a single balloon
catheter on promoting cervical ripening in the labor induction of
pregnant women in late-term pregnancy is more exact with high
safety. The deficiency of the study is that the sample size is
small. Consequently, clinical randomized controlled trials with a
larger size of samples are required for verification.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YC analyzed and interpreted the patient data, and
approved the final manuscript. MQ conceived and designed the study.
MQ and MJ were responsible for the data collection. MJ drafted and
revised the manuscript for important intellectual content. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Affiliated Hospital of Jining Medical University. Patients who
participated in this research, signed the informed consent and had
complete clinical data.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bakker R, Pierce S and Myers D: The role
of prostaglandins E1 and E2, dinoprostone, and misoprostol in
cervical ripening and the induction of labor: A mechanistic
approach. Arch Gynecol Obstet. 296:167–179. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim YM, Park JY, Sung JH, Choi SJ, Oh SY,
Roh CR and Kim JH: Predicting factors for success of vaginal
delivery in preterm induction with prostaglandin E2.
Obstet Gynecol Sci. 60:163–169. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hiersch L, Borovich A, Gabbay-Benziv R,
Maimon-Cohen M, Aviram A, Yogev Y and Ashwal E: Can we predict
successful cervical ripening with prostaglandin E2
vaginal inserts? Arch Gynecol Obstet. 295:1–349. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sayed Ahmed WA, Ibrahim ZM, Ashor OE,
Mohamed ML, Ahmed MR and Elshahat AM: Use of the Foley catheter
versus a double balloon cervical ripening catheter in pre-induction
cervical ripening in postdate primigravidae. J Obstet Gynaecol Res.
42:1489–1494. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kehl S, Weiss C and Rath W: Balloon
catheters for induction of labor at term after previous cesarean
section: A systematic review. Eur J Obstet Gynecol Reprod Biol.
204:44–50. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Salim R, Zafran N, Nachum Z, Garmi G,
Kraiem N and Shalev E: Single-balloon compared with double-balloon
catheters for induction of labor: A randomized controlled trial.
Obstet Gynecol. 118:79–86. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Alfirevic Z, Keeney E, Dowswell T, Welton
NJ, Medley N, Dias S, Jones LV, Gyte G and Caldwell DM: Which
method is best for the induction of labour? A systematic review,
network meta-analysis and cost-effectiveness analysis. Health
Technol Assess. 20:1–584. 2016. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol
BW, Irion O and Boulvain M: Mechanical methods for induction of
labour. Cochrane Database Syst Rev. Mar 14–2012.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Husain S, Husain S and Izhar R: Oral
misoprostol alone versus oral misoprostol and Foley's catheter for
induction of labor: A randomized controlled trial. J Obstet
Gynaecol Res. 43:1270–1277. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Policiano C, Pimenta M, Martins D and
Clode N: Efficacy and safety of foley catheter balloon for cervix
priming in term pregnancy. Acta Med Port. 30:281–284. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Duro Gómez J, Garrido Oyarzún MF,
Rodríguez Marín AB, de la Torre González AJ, Arjona Berral JE and
Castelo-Branco C: Vaginal misoprostol and cervical ripening balloon
for induction of labor in late-term pregnancies. J Obstet Gynaecol
Res. 43:87–91. 2017. View Article : Google Scholar
|
|
12
|
Vrachnis N, Malamas FM, Sifakis S,
Tsikouras P and Iliodromiti Z: Immune aspects and myometrial
actions of progesterone and CRH in labor. Clin Dev Immunol.
2012:9376182012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li YY, Yin ZY, Li S, Xu H, Zhang XP, Cheng
H, Du L, Zhou XY and Zhang B: Comparison of transvaginal surgery
and methotrexate/mifepristone-combined transcervical resection in
the treatment of cesarean scar pregnancy. Eur Rev Med Pharmacol
Sci. 21:2957–2963. 2017.PubMed/NCBI
|
|
14
|
Florio P, Romero R, Chaiworapongsa T,
Kusanovic JP, Torricelli M, Lowry PJ and Petraglia F: Amniotic
fluid and umbilical cord plasma corticotropin-releasing factor
(CRF), CRF-binding protein, adrenocorticotropin, and cortisol
concentrations in intraamniotic infection and inflammation at term.
J Clin Endocrinol Metab. 93:3604–3609. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jagielska I, Kazdepka-Ziemińska A, Janicki
R, Fórmaniak J, Walentowicz-Sadłecka M and Grabiec M: Evaluation of
the efficacy and safety of Foley catheter pre-induction of labor.
Ginekol Pol. 84:180–185. 2013.(In Polish). PubMed/NCBI
|
|
16
|
Eleje GU, Ezugwu EC, Eke AC, Eleje LI,
Ikechebelu JI, Ezebialu IU, Obiora CC, Nwosu BO, Ezeama CO, Udigwe
GO, et al: Accuracy of a combined insulin-like growth
factor-binding protein-1/interleukin-6 test (Premaquick) in
predicting delivery in women with threatened preterm labor. J
Perinat Med. Feb 25–2017.(Epub ahead of print). View Article : Google Scholar
|
|
17
|
Castillo-Castrejon M, Meraz-Cruz N,
Gomez-Lopez N, Flores-Pliego A, Beltrán-Montoya J, Viveros-Alcaráz
M and Vadillo-Ortega F: Choriodecidual cells from term human
pregnancies show distinctive functional properties related to the
induction of labor. Am J Reprod Immunol. 71:86–93. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bollapragada S, Youssef R, Jordan F, Greer
I, Norman J and Nelson S: Term labor is associated with a core
inflammatory response in human fetal membranes, myometrium, and
cervix. Am J Obstet Gynecol. 200:104.e1–104.e11. 2009. View Article : Google Scholar
|