Introduction
Diabetic foot wounds are a complication of diabetic
peripheral neuropathy and manifest as peripheral vascular lesions
in the lower limbs of patients with diabetes mellitus (1). Lesions may lead to lower limb
infection, ulcer formation and the destruction of deep tissue
(2). Diabetic foot wounds are prone
to relapse and wound healing is extremely slow; as such, clinical
treatments typically have poor outcomes, which may cause long-term
physical and mental suffering and financial hardship for the
patient (3). It has previously been
demonstrated that reduced absolute or relative levels of growth
factors may contribute to healing resistance in diabetic foot
wounds (4). The majority of research
has focused on mechanisms underlying the involvement of growth
factors in diabetic foot wound healing, whereas few clinic trials
have been performed to assess the efficacy of growth factor
treatments on diabetic foot wound healing (5). More rigorous and accurate randomized
controlled trials are required to investigate the clinical efficacy
of growth factors.
The clinical use of recombinant human epidermal
growth factor (EGF) and fibroblast growth factor (FGF) is common
(6). However, comparative studies of
the treatment effects of these growth factors alone or combined are
few. The aim of the present study was to investigate the effects of
EGF and acidic FGF (aFGF) factors on diabetic foot wound healing,
alone and in combination.
Materials and methods
Patients
A total of 199 patients with diabetic foot ulcers
were recruited at the Burn Treatment Center of the First Affiliated
Hospital of Nanchang University (Nanchang, China) between February
2015 and February 2017. All patients volunteered to participate in
the present study and provided written informed consent. The
present study has been approved by the Ethics Committee of the
First Affiliated Hospital of Nanchang University. Patient
demographics are presented in Table
I.
 | Table I.Basic information comparison of the
four included groups. |
Table I.
Basic information comparison of the
four included groups.
|
|
|
|
|
|
| Sex |
|---|
|
|
|
|
|
|
|
|
|---|
| Group | Case number | Diabetes mellitus
history (year) | Age | Wound
area/cm2 | Wound formation
Time/week | Male | Female |
|---|
| Combination group of
the growth factors | 50 | 12.67±3.96 | 61±5.31 | 3.6±0.5 | 12±0.53 | 26 | 24 |
| Human epidermal
growth factor group | 50 |
13±4.88 | 65±3.65 | 4.7±0.3 | 16±0.62 | 25 | 25 |
| Acidic fibroblast
growth factor group | 50 |
15±6.72 | 60±6.21 | 5.1±0.2 | 14±0.27 | 24 | 26 |
| Control group | 49 |
12±4.26 | 63±4.56 | 4.2±0.4 | 13±0.35 | 25 | 24 |
| P-value |
| >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
All patients met the following inclusion criteria:
Type II diabetes mellitus according to the World Health
Organization diagnostic criteria (7), wounds of grade II according to the
Wagner grading method (8) and wounds
located in the foot with good blood supply (or located at the toe
with limb salvage treatment required). The nutritional status of
enrolled patients was good (malnourished patients were given
underlying nutritional support before treatment). The exclusion
criteria were as follows: Presence of other serious complications,
other serious diseases, foot gangrene or severe ischemic necrosis
where amputation treatment was required.
Treatment groups
Patients were randomly divided into four groups: A
combination treatment group (EGF + aFGF; n=50), a recombinant human
EGF group (n=50), an aFGF group (n=50) and a normal saline control
group (n=49). The fasting blood glucose levels of all patients were
<11.1 mmol/l prior to wound treatment. Antibiotics (cftazidime,
administered via 1 g/12 h intravenous drip) were used to completely
control the infection. Antibiotics were used in all patients at the
same dosage for 3–7 days according to severity and were not used in
the trial following the administration of growth factor reagents
(beginning 3 days following the cessation of antibiotic treatment).
Therefore, antibiotics should not influence the results of the
present study. Debridement, cleaning and pathological granulation
removal were performed prior to the start of this experimental
study. EGF was provided by Shenzhen Watsin Genetech Co., Ltd.
(Shenzhen, China) and aFGF was provided by Shanghai Tenry
Pharmaceutical Co., Ltd. (Shanghai, China).
Treatment methods
Patients were administered with growth factors
according to the manufacturer's recommended dosage. Patients in the
combination treatment group were treated with topical recombinant
human EGF at 40 IU/cm2 and aFGF at 40 AU/cm2.
Patients in the recombinant human EGF treatment group were treated
with topical recombinant human EGF at 40 IU/cm2.
Patients in the aFGF group were treated with topical aFGF 40
AU/cm2. For patients in the control group, the wound was
cleaned with normal saline only. Growth factors were dissolved in
normal saline and applied evenly to the surface of the lesions
prior to dressing application. Dressings were changed and
treatments were applied once per day for a total of 60 days.
Observation indices
The time required for wound healing at each stage
was recorded. The healing stage was determined by the percentage of
the wound healed and the degree of granulated tissue growth. Wound
healing percentage=[(initial wound area-corresponding time-point
wound area)/initial wound area] ×100. To assess the degree of
granulation, the following scoring system was used: No new
granulated tissue formation in the wound surface, grade 0. New
granulated tissue formation in the wound surface, grade 1.
Granulated tissue accounting for 50% of the total wound area, grade
2. Granulated tissue covering the entire wound area, grade 3. The
time taken to reach granulation grade 1, 2 and 3 in each group was
recorded for each patient. The time taken to reach 50 and 100%
healing were also recorded.
Statistical analysis
SPSS v18.0 (SPSS, Inc., Chicago, IL, USA) were used
for statistical analysis. Data were analyzed by two-way analysis of
variance followed by a post-hoc Student-Newman-Keuls q-test. Data
are presented as the mean ± standard deviation. P<0.05 was
considered to indicate a statistically significant difference.
Results
Patient demographics
According to the diagnostic criteria, 199 patients
with diabetic foot wounds classified as Wagner grade II were
enrolled in the present study. No patients withdrew or were lost to
follow-up and all are included in the analysis. No significant
differences were observed in diabetes mellitus history, age,
original wound surface area and duration of wound formation between
any of the groups (Table I).
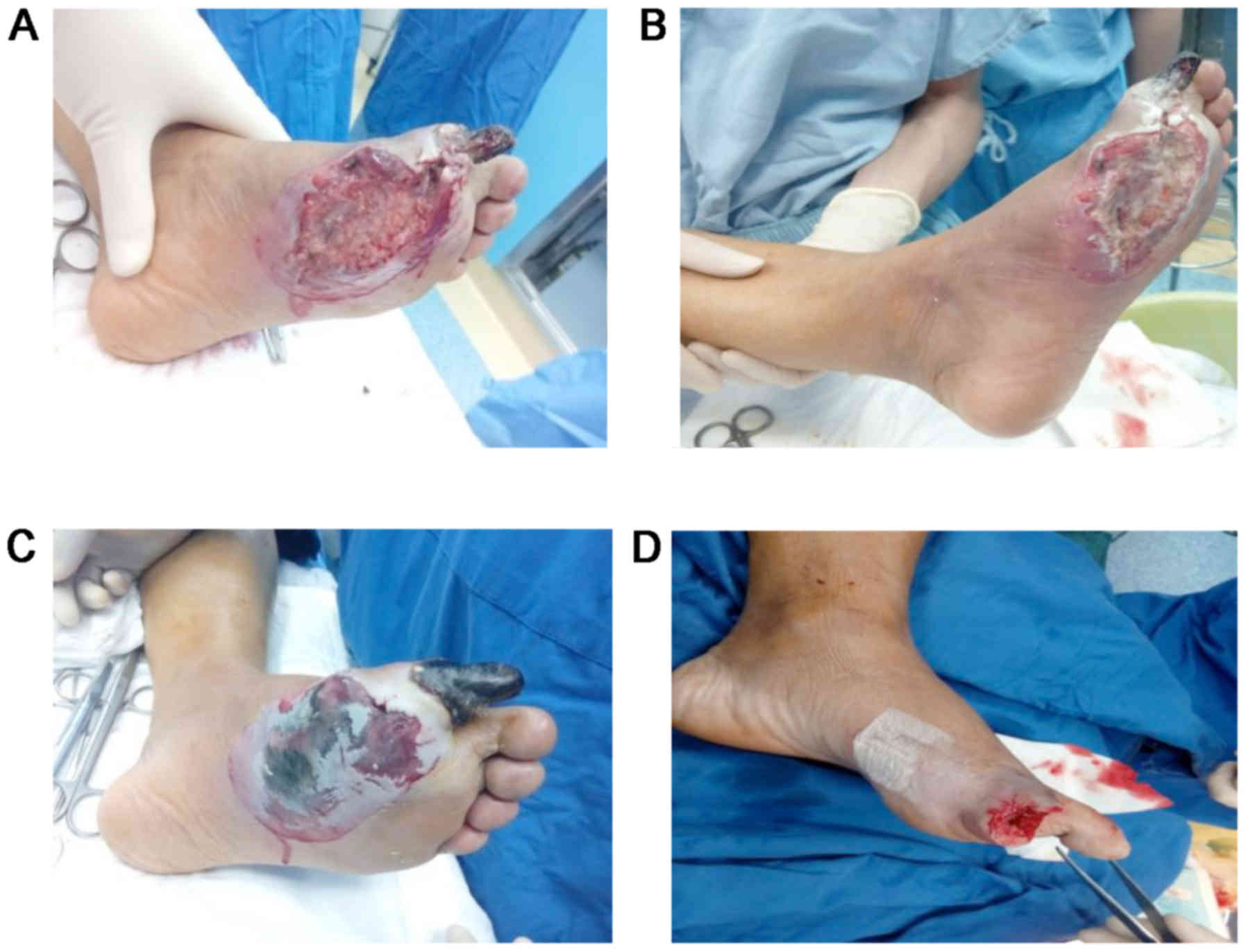
Wound healing
Wound healing initiation was observed in all groups
within 4 days of the start of treatment and no significant
difference was observed between groups (Fig. 1 and Table
II). However, 50% wound healing and complete wound healing were
achieved with significantly shorter treatment durations in the
combination group compared with the control group (P<0.01;
Fig. 1 and Table II). Similar results were observed in
the EGF treatment group, with significantly shorter 50% and
complete wound healing durations compared with the control group
(P<0.05; Fig. 1 and Table II).
 | Table II.Treatment duration and for wound
healing. |
Table II.
Treatment duration and for wound
healing.
| Group | Wound healing
initiation time (days) | 50% wound surface
healing time (days) | Complete wound
healing time (days) |
|---|
| aFGF + EGF | 3.3±0.60 |
17.21±0.36b |
36.31±1.62b |
| EGF | 3.4±0.82 |
19.35±0.76a |
38.51±1.46a |
| aFGF | 3.5±0.78 | 22.42±0.86 | 41.83±1.78 |
| Normal control | 3.5±0.56 | 25.36±0.48 | 47.52±1.82 |
Granulated tissue maturation
No significant difference in the duration of
treatment required to achieve granulated tissue growth grade 1was
observed between groups (Table
III). However, granulated tissue growth grades 2 and 3 were
achieved with a significantly shorter treatment time in the
combination (P<0.01) and EGF (P<0.05) groups compared with
the control (Table III). No
significant differences in treatment time were observed between the
aFGF and control groups for any granulated tissue grade.
 | Table III.Treatment duration and granulated
tissue growth. |
Table III.
Treatment duration and granulated
tissue growth.
|
| Treatment duration
for granulated tissue growth (days) |
|---|
|
|
|
|---|
| Group | Grade 1 | Grade 2 | Grade 3 |
|---|
| aFGF + EGF | 3.61±0.72 |
10.23±0.57b |
26.19±1.35b |
| EGF | 3.83±0.63 |
11.65±0.71a |
28.31±1.68a |
| aFGF | 4.12±0.78 | 13.73±0.69 | 31.07±1.03 |
| Normal control | 3.94±0.22 | 16.27±0.61 | 37.21±1.27 |
Discussion
Diabetic foot wounds represent a refractory disease
that may be caused by multiple factors and the associated
pathophysiological processes are very complex. Diabetic foot refers
to pathological changes caused by chronic diabetes mellitus
(9) and typically manifests as
pathological changes to blood vessels and nerves in the lower limbs
(10). Infection of ulcers is common
and foot gangrene is the most serious complication associated with
diabetic foot (11–13). It is thought that decreased levels of
growth factors and their receptors in the diabetic foot result in
wounds that are resistant to healing (14). However, previous animal studies have
reported that growth factor therapy does not aid diabetic wound
healing in mice (15–18). Some studies have suggested that
decreased local growth factor activity, including growth factor
glycosylation, is responsible for delayed wound healing (19–21).
In the present study, wounds had begun to heal in
all groups following 3–4 days of treatment. However, as treatment
continued, healing was significantly faster in the EGF and
combination groups compared with the normal control. The time taken
for granulated tissue to reach Wagner grade 1 was also similar in
all groups, whereas grades 2 and 3 were achieved significantly
faster in the EGF and combination groups compared with the control.
In order to interpret these results, the mechanism by which growth
factors promote wound healing must be investigated.
The accumulation of necrotic tissue, severe
inflammation and a decrease in EGF release in a wound results in
local increases in sugar levels, non-enzymatic glycosylation and
advanced glycation end products (AGEs) (22). The increase in AGEs negatively
regulates cell proliferation, inflammatory reactions and granulated
tissue maturation (23), thereby
inhibiting the function of fibroblasts, vascular endothelial cells
and epidermal stem cells to delay wound healing. Several
large-sample randomized double-blind studies have been performed to
assess the effect of EGF treatment in diabetic foot ulcers
(14–17,24–27) and
it has previously been reported that the application of exogenous
EGF has a good curative effect in diabetic wounds (28).
Under normal physiological conditions, FGF binds to
a tyrosine kinase receptor, leading to signal transduction
(29) to stimulated fibroblasts and
vascular endothelial cells to move towards the site of trauma
(30). FGF and AGEs have the same
receptor binding sites, and so when the concentration of AGEs is
elevated (31) the function of FGF
is inhibited. Conversely, when local FGF is applied, the increase
of exogenous FGF (32) inhibits the
binding of AGEs to the tyrosine kinase receptor and accelerates
wound healing. A previous controlled trial treated diabetic foot
wounds with FGF alone (31) and the
results demonstrated that the use of exogenous FGF effectively
promoted wound healing (33).
Few studies have been performed to investigate the
effect of combined EGF and aFGF on diabetic foot wounds (32). Based on the mechanism by which growth
factors promote wound repair, the difficult healing of clinical
diabetic foot wounds can be explained by the following aspects: The
function of local microenvironment is changed such as strong
inflammatory response, necrotic tissues, and enhanced
glycosylation. Changes in the local microenvironment inhibit the
function of fibroblasts, endothelial cells and epidermal cells in
wound repair (34). When exogenous
growth factors are applied to necrotic tissue, the high level of
local AGEs results in competitive inhibition at the early stage of
wound healing, countering the curative effect of the growth factors
(35). In the later stages of would
healing, a sufficient amount of exogenous growth factors will have
entered the necrotic tissue, significantly increasing the local
growth factor concentration and outcompeting AGEs for binding
sites. As such, the effect of exogenous growth factors on wound
healing is more obvious with increased treatment time. Combined use
of EGF and aFGF results in a more rapid increase in local growth
factor concentration, accelerating the binding site competition
process and ultimately promoting cell proliferation. Combination
treatment may promote mitosis, signal transduction, endogenous
growth factor production and inflammatory cell chemotaxis of
fibroblasts. These processes all contribute to accelerating the
healing rate of the tissue (36).
The differences between EGF and aFGF treatment
remain unclear and a larger clinical investigation is required.
However, based on the present study it may be hypothesized that EGF
treatment is more effective than aFGF for treating diabetic foot
wounds. A possible reason for this difference is that diabetic foot
wound tissues release low levels of EGF and using exogenous growth
factors directly increases the concentration of EGF in the wound,
which may have a negative feedback effect on non-enzymatic
glycosylation to directly accelerate the process of tissue repair.
aFGF, on the other hand, is a competitive antagonist of AGEs and
therefore a high local concentration is required to improve wound
healing. As such, a longer treatment time is required to observe
the curative effects of aFGF compared with EGF (37–39).
It has previously been reported that epidermis cell
proliferation is associated with age (40). Tiaka et al (35) suggested that diabetes, medical
history, age and foot blood perfusion may influence wound healing.
At the start of the present study, the baseline data of patients in
each group were compared and no significant differences were
observed. During treatment, patients were prescribed bed rest in
order to prevent differences in the load applied to the wounded
foot. The results of the present study demonstrate that growth
factors have good biological activity in that they promote the
growth of granulation tissue and that in combination with EGF and
aFGF treatment, they are important for angiogenesis and wound
repair. However, there were several limitations to the present
study. The results suggest that the combination of two growth
factors promotes wound healing, but the relationship between dosage
and healing effect was not investigated. Furthermore, a small
sample size was used and it could not be determined whether
individual factors, including sex, may affect the results. The
molecular mechanism by which growth factors promote wound healing
remains unclear and further research is required to explore
relevant signaling pathways and determine which factors influence
the efficacy of growth factor treatment.
In summary, the present study assessed the clinical
effect of growth factors as a treatment for diabetic foot wounds.
The results indicated that combined application of EGF and aFGF
effectively promotes wound healing. Diabetic foot wound healing
involves several pathological processes and so the treatment regime
used in the present study may need to be further improved. It could
be optimized based on further study of the pathogenesis of the
disease, as well as further evaluation of pharmacological agents,
treatment duration, dosage and route of administration (41). Using a combination of multiple growth
factors and dosages at different stages may improve the therapeutic
efficacy of growth factor treatment in diabetic foot wound. Further
studies are required to validate these findings.
Acknowledgements
The authors would like to thank Ms. Liao Kaili for
her support and encouragement.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JX designed the direction of research and
implemented it, collected clinical data and statistical analysis
and wrote the manuscript. DM collected clinical data and dressing
changes. GG conducted quality assessments and performed result
analysis. XL dressed and collected clinical data. ZF reviewed and
revised the manuscript and aided in communication for
publication.
Ethics approval and consent to
participate
The present study was approved by the ethics
committee of the First Affiliated Hospital of Nanchang University
and written informed consent was obtained from all patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Everett E and Mathioudakis N: Update on
management of diabetic foot ulcers. Ann NY Acad Sci. 1411:153–165.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Babaei V, Afradi H, Gohardani HZ, Nasseri
F, Azarafza M and Teimourian S: Management of chronic diabetic foot
ulcers using platelet-rich plasma. J Wound Care. 26:784–787. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dinh T, Tecilazich F, Kafanas A, Doupis J,
Gnardellis C, Leal E, Tellechea A, Pradhan L, Lyons TE, Giurini JM
and Veves A: Mechanisms involved in the development and healing of
diabetic foot ulceration. Diabetes. 61:2937–2947. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Demidova-Rice TN, Hamblin MR and Herman
IM: Acute and impaired wound healing: Pathophysiology and current
methods for drug delivery, part 2: Role of growth factors in normal
and pathological wound healing: Therapeutic potential and methods
of delivery. Adv Skin Wound Care. 25:349–370. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sridharan K and Sivaramakrishnan G: Growth
factors for diabetic foot ulcers: Mixed treatment comparison
analysis of randomized clinical trials. Br J Clin Pharmacol.
84:434–444. 2017. View Article : Google Scholar
|
|
6
|
Laiva AL, O'Brien FJ and Keogh MB:
Innovations in gene and growth factor delivery systems for diabetic
wound healing. J Tissue Eng Regen Med. May 8–2017.(Epub ahead of
print). PubMed/NCBI
|
|
7
|
Stern MP, Valdez RA, Haffner SM, Mitchell
BD and Hazuda HP: Stability over time of modern diagnostic criteria
for type II diabetes. Diabetes Care. 16:978–983. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wagner FW: Transcutaneous Doppler
ultrasound in the prediction of healing and the selection of
surgical level for dysvascular lesions of the toes and forefoot.
Clin Orthop Relat Res. 142:110–114. 1979.
|
|
9
|
Al-Rubeaan K, Al Derwish M, Ouizi S,
Youssef AM, Subhani SN, Ibrahim HM and Alamri BN: Diabetic foot
complications and their risk factors from a large retrospective
cohort study. PLoS One. 10:e01244462015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Naz I, Walters E, Akbari CM, Attinger CE
and Kim PJ: Noninvasive vascular assessment of lower extremity
wounds in diabetics: Are we able to predict perfusion deficits?
Surg Technol Int. 31:66–74. 2017.PubMed/NCBI
|
|
11
|
Gope ML and Gope R: Tyrosine
phosphorylation of EGF-R and PDGF-R proteins during acute cutaneous
wound healing process in mice. Wound Repair Regen. 17:71–79. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pastore S, Mascia F, Mariani V and
Girolomoni G: The epidermal growth factor receptor system in skin
repair and inflammation. J Invest Dermatol. 128:1365–1374. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schumacher B, Pecher P, Von Specht BU and
Stegmann T: Induction of neoangiogenesis in ischemic myocardium by
human growth factors: First clinical results of a new treatment of
coronary heart disease. Circulation. 97:645–650. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Simons M, Annex BH, Laham RJ, Kleiman N,
Henry T, Dauerman H, Udelson JE, Gervino EV, Pike M, Whitehouse MJ,
et al: Pharmacological treatment of coronary artery disease with
recombinant fibroblast growth factor-2: Double-blind, randomized,
controlled clinical trial. Circulation. 105:788–793. 2012.
View Article : Google Scholar
|
|
15
|
Eppler SM, Combs DL, Henry TD, Lopez JJ,
Ellis SG, Yi JH, Annex BH, Mccluskey ER and Zioncheck TF: A
target-mediated model to describe the pharmacokinetics and
hemodynamic effects of recombinant human vascular endothelial
growth factor in humans. Clin Pharmacol Ther. 72:20–32. 2013.
View Article : Google Scholar
|
|
16
|
Richardson TP, Peters MC, Ennett AB and
Mooney DJ: Polymeric system for dual growth factor delivery. Nat
Biotechnol. 19:1029–1034. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chen RR, Silva EA, Yuen WW, Brock AA,
Fischbach C, Lin AS, Guldberg RE and Mooney DJ: Integrated approach
to designing growth factor delivery systems. FASEB J. 21:3896–3903.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Marui A, Kanematsu A, Yamahara K, Doi K,
Kushibiki T, Yamamoto M, Itoh H, Ikeda T, Tabata Y and Komeda M:
Simultaneous application of basic fibroblast growth factor and
hepatocyte growth factor to enhance the blood vessels formation. J
Vasc Surg. 41:82–90. 2015. View Article : Google Scholar
|
|
19
|
Ghiasi Z, Gray T, Tran P, Dubielzig R,
Murphy C, McCartney DL and Reid TW: The effect of topical
Substance-P plus insulin-like growth factor-1 (IGF-1) on epithelial
healing after photorefractive keratectomy in rabbits. Transl Vis
Sci Technol. 7:122018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
An Y, Liu WJ, Xue P, Ma Y, Zhang LQ, Zhu
B, Qi M, Li LY, Zhang YJ, Wang QT and Jin Y: Autophagy promotes
MSC-mediated vascularization in cutaneous wound healing via
regulation of VEGF secretion. Cell Death Dis. 9:582018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saijo H, Kilpadi DV and Akita S:
Evaluation of the use of recombinant human basic fibroblast growth
factor in combination with negative pressure wound therapy with
instillation and dwell time in porcine full-thickness wound model.
Wound Repair Regen. Jan 12–2018.(Epub ahead of print).
|
|
22
|
Simmons CA, Alsberg E, Hsiong S, Kim WJ
and Mooney DJ: Dual growth factor delivery and controlled scaffold
degradation enhance in vivo bone formation by transplanted bone
marrow stromal cells. Bone. 35:562–569. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Basmanav FB, Kose GT and Hasirci V:
Sequential growth factor delivery from complexed microspheres for
bone tissue engineering. Biomaterials. 29:4195–4204. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Patel ZS, Young S, Tabata Y, Jansen JA,
Wong ME and Mikos AG: Dual delivery of an angiogenic and an
osteogenic growth factor for bone regeneration in a critical size
defect model. Bone. 43:931–940. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hutchings H, Ortega N and Plouet J:
Extracellular matrix-bound vascular endothelial growth factor
promotes endothelial cell adhesion, migration, and survival through
integrin ligation. FASEB J. 17:1520–1522. 2013. View Article : Google Scholar
|
|
26
|
Tsou R and Isik FF: Integrin activation is
required for VEGF and FGF receptor protein presence on human
microvascular endothelial cells. Mol Cell Biochem. 224:81–89. 2011.
View Article : Google Scholar
|
|
27
|
Li B, Davidson JM and Guelcher SA: The
effect of the local delivery of platelet-derived growth factor from
reactive two-component polyurethane scaffolds on the healing in rat
skin excisional wounds. Biomaterials. 30:3486–3494. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Silva AK, Richard C, Bessodes M, Scherman
D and Merten OW: Growth factor delivery approaches in hydrogels.
Biomacromolecules. 10:9–18. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sakiyama-Elbert SE and Hubbell JA:
Development of fibrin derivatives for controlled release of
heparin-binding growth factors. J Control Release. 65:389–402.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhang X, Ding X, Lin X, Yang P and Lin K:
Clinical observation of recombinant human epidermal growth factor
combined with lipoic acid in the treatment of diabetic foot. Chin
Pharm. 27:4147–4149. 2016.(In Chinese).
|
|
31
|
Johnson NR and Wang Y: Controlled delivery
of heparin-binding EGF-like growth factor yields fast and
comprehensive wound healing. J Control Release. 166:124–129. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bae IH, Park JW and Kim DY: Enhanced
regenerative healing efficacy of a highly skin-permeable growth
factor nanocomplex in a full-thickness excisional mouse wound
model. Int J Nanomedicine. 9:4551–4567. 2014.PubMed/NCBI
|
|
33
|
Loot MA, Kenter SB, Au FL, van Galen WJ,
Middelkoop E, Bos JD and Mekkes JR: Fibroblasts derived from
chronic diabetic ulcers differ in their response to stimulation
with EGF, IGF-I, bFGF and PDGF-AB compared to controls. Eur J Cell
Biol. 81:153–160. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Nie K, Li P, Zeng X, Sun G, Jin W, Wei Z,
Wang B, Qi J, Wang Y and Wang D: Clinical observation of basic
fibroblast growth factor combined with topical oxygen therapy in
enhancing burn wound healing. Chin J Rep Rec Surg. 6:643–646.
2010.(In Chinese).
|
|
35
|
Tiaka EK, Papanas N, Manolakis AC and
Maltezos E: The role of nerve growth factor in the prophylaxis and
treatment of diabetic foot ulcers. Int J Burns Trauma. 1:68–76.
2011.PubMed/NCBI
|
|
36
|
Sheridan MH, Shea LD, Peters MC and Mooney
DJ: Bioabsorbable polymer scaffolds for tissue engineering capable
of sustained growth factor delivery. J Control Release. 64:91–102.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chen RR and Mooney DJ: Polymeric growth
factor delivery strategies for tissue engineering. Pharm Res.
20:1103–1112. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhu XH, Wang CH and Tong YW: In vitro
characterization of hepatocyte growth factor release from PHBV/PLGA
microsphere scaffold. J Biomed Mater Res A. 89:411–423. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Pepper MS, Ferrara N, Orci L and Montesano
R: Potent synergism between vascular endothelial growth factor and
basic fibroblast growth factor in the induction of angiogenesis in
vitro. Biochem Biophys Res Commun. 189:824–831. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hamann Jimenez MC, Tator CH and Shoichet
MS: Injectable intrathecal delivery system for localized
administration of EGF and FGF-2 to the injured rat spinal cord. Exp
Neurol. 194:106–119. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Yang HS, Shin J, Bhang SH, Shin JY, Park
J, Im GI, Kim CS and Kim BS: Enhanced skin wound healing by a
sustained release of growth factors contained in platelet-rich
plasma. Exp Mol Med. 43:622–629. 2011. View Article : Google Scholar : PubMed/NCBI
|