Introduction
Thromboangiitis obliterans and arteriosclerotic
occlusive disease are the most common ischemic diseases in lower
limbs, which, due to chronic ischemia and hypoxia in lower limbs,
are often accompanied by skin color changes (1) muscle atrophy and subcutaneous fat
disappearance, thus leading to fibrous connective tissue
hyperplasia (2) and eventually
resulting in osteoporosis ischemic neuritis and vasculitis. The
prolonged course of disease will aggravate tissue ischemia and
hypoxia and lead to ulcer or even gangrene (3). Traditional drug therapy cannot
fundamentally eradicate limb ischemia and hypoxia caused by
vascular lesions, so people are not satisfied with the treatment
results and eventually choose to be treated with amputation
(4).
Through Ilizarov transverse tibial bone transport
and microcirculation reconstruction technique, tibiae are formed
into movable bone flaps to be transversely transported
correspondingly, which repeatedly stimulates the regeneration of
tibial bone marrows (5), promotes
neovascularization and bone tissue formation, achieves the
reconstruction of peripheral blood circulation (6), so as to improve limb blood supply,
fundamentally eradicate the source of ischemic diseases in lower
limbs and promote blood circulation, thus playing a role in
clinical treatment (7). Although
certain clinical effects have been achieved after it is applied in
the treatment of diabetic foot, it has been applied in few studies
to the treatment of chronic ischemic diseases in lower limbs. To
make up for the above deficiencies, the clinical value of Ilizarov
transverse tibial bone transport and microcirculation
reconstruction technique in the treatment of chronic ischemic
diseases in lower limbs was mainly explored in the present
study.
Patients and methods
General data
A total of 90 patients with chronic ischemic
diseases in the lower limbs admitted to The First Affiliated
Hospital of Nanjing Medical University (Nanjing, China) from July
2015 to June 2017 were selected. All the patients were the
confirmed cases diagnosed through comprehensive examinations such
as clinical manifestation examination, biochemical tests and lower
limb vascular ultrasound, and all of them had symptoms such as
intermittent claudication, rest pain and lower limb ulcer or
gangrene. Before the inclusion, all the patients signed the
informed consent, and the study was approved by the Ethics
Committee of The First Affiliated Hospital of Nanjing Medical
University. Patients were aged 18-60 years old with no past history
of diseases. Patients combined with lower limb fractures, knee
dislocation, liver and kidney dysfunction, diabetes, coronary heart
disease, immune system diseases, systemic infection, malignant
tumors, mental illness, systemic immune system diseases were
excluded. Through a random number table, the patients were divided
into two groups with 45 patients each. In the observation group,
there were 25 males and 20 females, aged 18-60 years old with the
mean age of 53.2±1.8 years old; the course of disease endured 3
months to 1 year with the mean time of 5.1±0.3 months. In the
control group, there were 24 males and 21 females, aged 18-60 years
old with the mean age of 53.1±1.7 years old; the course of disease
endured 3 months to 1 year with the mean time of 5.0±0.3 months.
Differences in comparisons of sex, age, course of disease, the
diameters and blood flows of the femoral, popliteal, posterior
tibial and dorsalis pedis artery and dorsal foot skin temperature
were not statistically significant (Table I).
 | Table I.Comparisons of main artery diameter
and blood flow and dorsal foot skin temperature of lower limbs
between two groups of patients (mean ± SD). |
Table I.
Comparisons of main artery diameter
and blood flow and dorsal foot skin temperature of lower limbs
between two groups of patients (mean ± SD).
| Groups | Femoral artery
diameter (cm) | Popliteal artery
diameter (cm) | Posterior tibial
artery diameter (cm) | Dorsalis pedis artery
diameter (cm) | Femoral artery blood
flow (ml/min) | Popliteal artery
blood flow (ml/min) | Posterior tibial
artery blood flow (ml/min) | Dorsalis pedis artery
blood flow (ml/min) | Dorsal foot skin
temperature |
|---|
| Observation | 0.58±0.04 | 0.49±0.03 | 0.13±0.01 | 0.15±0.01 | 456.5±8.3 | 158.6±6.0 | 40.2±2.1 | 33.0±2.1 | 27.1±0.2 |
| Control | 0.59±0.04 | 0.48±0.03 | 0.13±0.01 | 0.15±0.01 | 456.1±8.3 | 159.1±5.9 | 40.3±2.0 | 33.1±2.0 | 27.2±0.3 |
| t or
χ2 | 1.186 | 1.342 | <0.001 | <0.001 | 0.229 | 0.399 | 0.231 | 0.231 | 1.861 |
| P-value | 0.239 | 0.183 | 1.000 | 1.000 | 0.820 | 0.691 | 0.818 | 0.818 | 0.007 |
Methods
Surgical methods in the observation group: Patients
in the observation group were treated with Ilizarov traverse tibial
bone transport and microcirculation reconstruction, during which
patients were in the supine position. The operation was performed
under the spinal anesthesia, and the incision was made at 15-18 cm
in the medial margin of the middle and lower tibia. The tibial
osteotomy distance was determined after the fascia was exposed by
blunt dissection. Generally, it is appropriate to set the length of
tibial osteotomy as 10-12 cm and width as 1.5-2.0 cm. The
periosteum was opened after being longitudinally cut in the middle
osteotomy area, so that the osteotomy area was completely exposed.
Then the bone cortex was cut using a pendulum saw to form the
active bone flap. An ~2 mm Schanz needle was inserted into the
upper and lower parts of the fenestrate bone flap, respectively,
for the traverse bone traction. Then two 4 mm Schanz needles were
inserted in a parallel direction into both ends of the tibia, and
the external fixation bracket was installed. Finally, two movable
transverse tractors were fitted on the external fixation bracket
and fixed with the traction needle. After operation, the hemostasis
was conducted, and wounds were sutured. Patients in the control
group were treated with percutaneous balloon angioplasty (PTBA)
mainly for the parts with ulcer and (or) gangrene. Treating the
femoral artery with PTBA improved and strengthened the lower limb
blood supply.
Observation indexes
Changes in the diameter and blood flow of lower limb
arteries in the paretic side after intervention were compared
between two groups of patients. Wound healing time and
disappearance time of pains in the two groups were counted. The
variation trends of dorsal foot skin temperature and the expression
area of vascular endothelial growth factors (VEGFs) at different
observation time-points in the two groups were compared so as to
know the improvement degree of clinical symptoms at 1 month after
operation in the two groups.
Evaluation methods
The diameter and blood flow of lower limb arteries
in the paretic side were detected using the Philips Hdiixe Doppler
blood vessel diagnostic apparatus with the probe frequency of 7-10
MHz. During the detection, patients were in the supine and prone
position, and the femoral, popliteal, posterior tibial and dorsalis
pedis artery were measured for detecting the artery inner diameter
and arterial stenosis. The diameter measurement position includes 1
cm away from the bifurcation proximal site of the femoral artery
and popliteal artery, 1 cm at the starting site of the posterior
tibial artery and 1 cm away from the distal junction site of the
ankle joint and the dorsalis pedis artery; the pain degree was
assessed with the visual analogue score as the standard, and the
total score ranged from 10 points (unbearable pain) to 0 point
(painless). The higher the score was, the higher the pain degree
would be. Rest pain refers to that people feel pain when the
affected limb is kept still, and rest pain score <3 points
indicates that clinical symptoms are improved. Disappearance time
of pains was examined with the score of rest pain and pain on
motion <3 points as the standard. The positive detection rate of
VEGFs was detected using enzyme-linked immunosorbent assay (the kit
was provided by Qingdao Wolsen Biotechnology Co., Ltd., Qingdao,
China), and its expression level was assessed using the HPIAS-1000
image analyzer. The main criterion for assessment was the ratio of
the area of positive substances in cells to the gray value in the
background.
Statistical analysis
SPSS 13.0 (SPSS, Inc., Chicago, IL, USA) was used in
this study. Measurement data were expressed as mean ± standard
deviation (mean ± SD), and the t-test was used for mean comparisons
between the two groups. χ2 test was used for ratio
comparisons. P<0.05 represented that the difference was
statistically significant.
Results
Comparison of the diameters of lower
limb arteries in the paretic side between the two groups after
intervention
After intervention, diameters of the femoral artery,
popliteal artery, posterior tibial artery and dorsalis pedis artery
of patients in the observation group were significantly larger than
those of patients in the control group (P<0.05) (Table II).
 | Table II.Comparison of the diameters of lower
limb arteries in the paretic side between the two groups (cm, mean
± SD). |
Table II.
Comparison of the diameters of lower
limb arteries in the paretic side between the two groups (cm, mean
± SD).
| Groups | Femoral artery | Popliteal artery | Posterior tibial
artery | Dorsalis pedis
artery |
|---|
| Observation | 0.72±0.08 | 0.60±0.05 | 0.23±0.01 | 0.21±0.01 |
| Control | 0.63±0.05 | 0.48±0.03 | 0.15±0.01 | 0.16±0.01 |
| t | 6.034 | 13.016 | 35.777 | 22.361 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 |
Comparison of the blood flow of lower
limbs in the paretic side between the two groups after
intervention
Blood flows of the femoral artery, popliteal artery,
posterior tibial artery and dorsalis pedis artery of patients in
the observation group were significantly higher than those of
patients in the control group (P<0.05) (Table III).
 | Table III.Comparison of the blood flow of lower
limb arteries in the paretic side between the two groups after
intervention (ml/min, mean ± SD). |
Table III.
Comparison of the blood flow of lower
limb arteries in the paretic side between the two groups after
intervention (ml/min, mean ± SD).
| Groups | Femoral artery | Popliteal artery | Posterior tibial
artery | Dorsalis pedis
artery |
|---|
| Observation | 766.5±15.3 |
458.6±11.1 | 80.2±3.1 | 73.6±2.8 |
| Control | 698.8±12.7 | 323.2±5.9 | 53.5±2.0 | 43.1±2.5 |
| t | 21.533 | 68.123 | 45.773 | 51.389 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 |
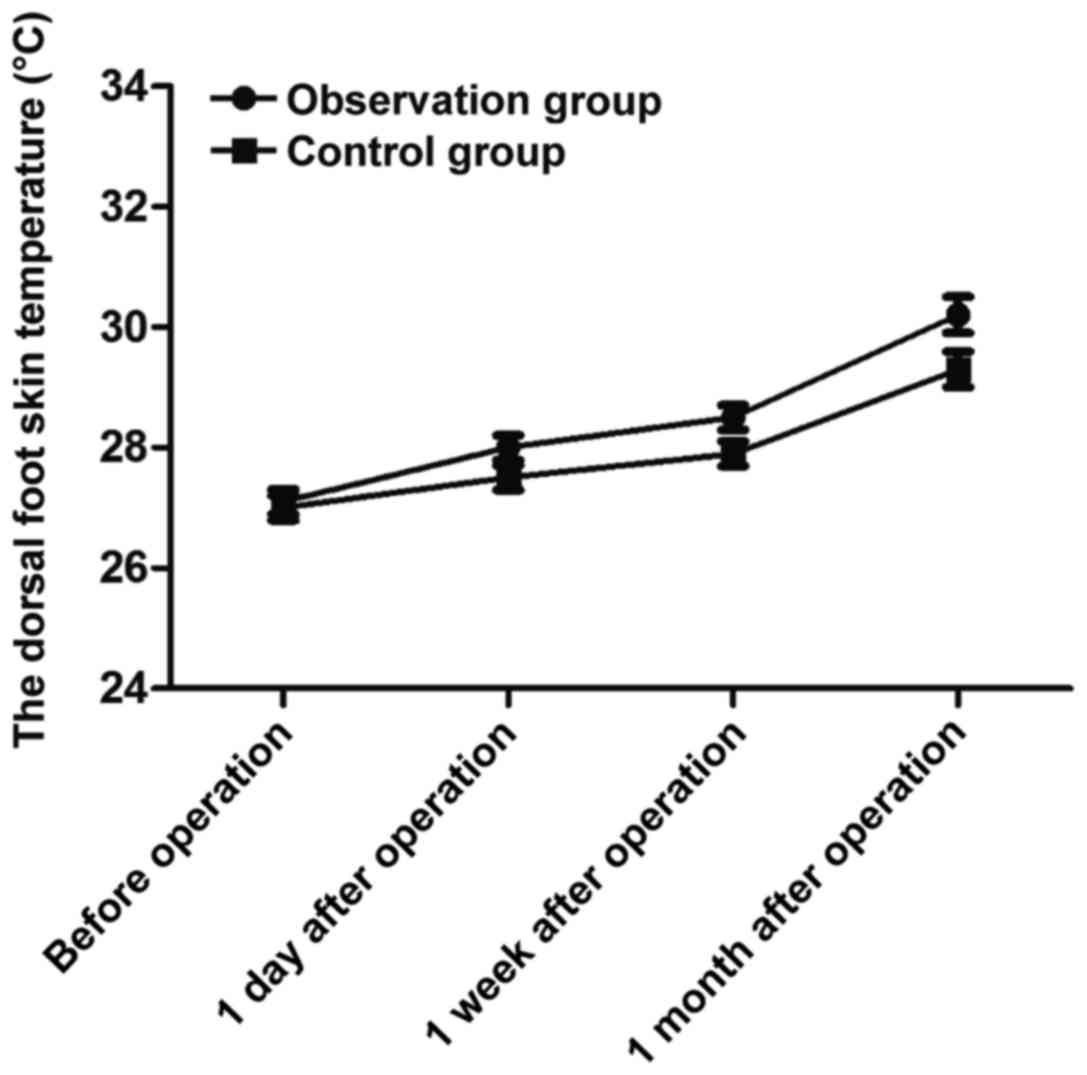
Comparison of the dorsal foot skin
temperature at different observation time-points between the two
groups
The dorsal foot skin temperature in the observation
group before operation (27.0±0.2°C) and at 1 day (28.0±0.2°C), 1
week (28.5±0.2°C), and 1 month (30.2±0.3°C) after operation was
significantly higher than that in the control group before
operation (27.0±0.2°C) and at 1 day (27.5±0.2°C), 1 week
(27.9±0.2°C) and 1 month (29.3±0.3°C) after operation (t=11.180,
13.416 and 13.416; P<0.001<0.05 in all comparisons) (Fig. 1).
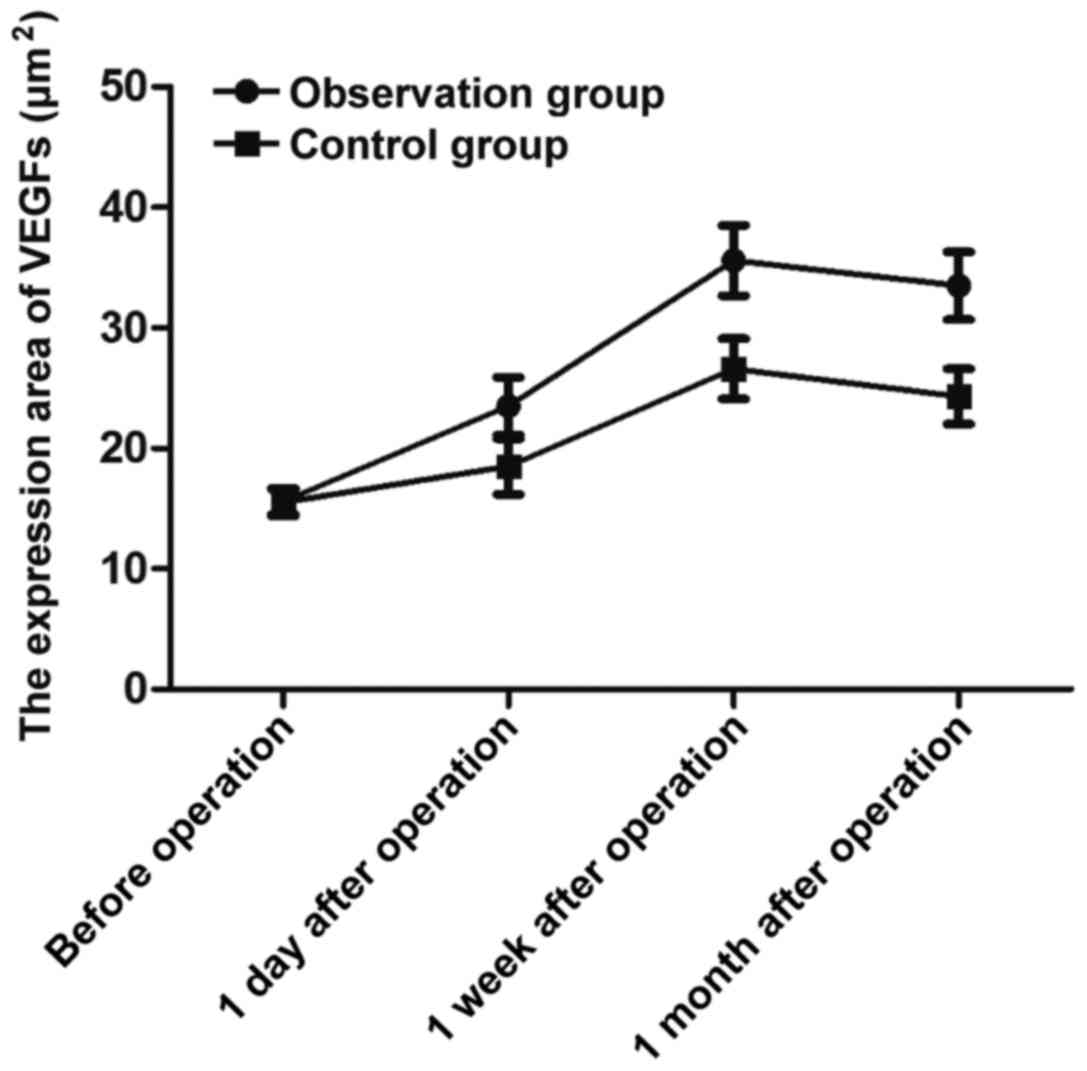
Comparison of the expression area of
VEGFs during intervention between the two groups
The expression area of VEGFs in the observation
group before operation (15.6±1.1 µm2) and at 1 day
(23.5±2.4 µm2), at 1 week (35.6±2.9 µm2) and
at 1 month (33.5±2.8 µm2) after operation was
significantly larger than that in the control group before
operation (15.5±1.1 µm2) and at 1 day (18.5±2.3
µm2), at 1 week (26.5±2.5 µm2) and at 1 month
(24.3±2.3 µm2) after operation (t=9.513, 14.866 and
16.058; P<0.001<0.05 in all comparisons) (Fig. 2).
Comparisons of wound healing time and
disappearance time of pains between the two groups
Wound healing time and disappearance time of pains
of patients in the observation group were earlier than those of
patients in the control group (P<0.05) (Table IV).
 | Table IV.Comparisons of wound healing time and
disappearance time of pains between the two groups (day, mean ±
SD). |
Table IV.
Comparisons of wound healing time and
disappearance time of pains between the two groups (day, mean ±
SD).
| Groups | Wound healing
time | Disappearance time of
pains |
|---|
| Observation | 15.3±0.6 | 12.1±0.5 |
| Control | 26.5±1.5 | 25.6±1.3 |
| t | 43.846 | 61.300 |
| P-value | <0.001 | <0.001 |
Comparison of the improvement degree
of clinical symptoms at 1 month after operation between the two
groups
At 1 month after operation, the improvement degree
of intermittent claudication, rest pain, lower limb ulcers or
gangrene among clinical symptoms in the observation group were
significantly higher than that in the control group (P<0.05)
(Table V).
 | Table V.Comparison of the improvement degree
of clinical symptoms at 1 month after operation between the two
groups (effective case/total case). |
Table V.
Comparison of the improvement degree
of clinical symptoms at 1 month after operation between the two
groups (effective case/total case).
| Groups | Intermittent
claudication | Rest pain | Lower limb ulcers or
gangrene |
|---|
| Observation | 39/45 | 44/45 | 38/45 |
| Control | 25/45 | 30/45 | 11/45 |
| χ2 | 10.601 | 12.846 | 32.658 |
| P-value | <0.001 | <0.001 | <0.001 |
Discussion
Lower limb ischemic disease is the most common cause
of lower limb dysfunction or even amputation in present clinical
practices. The incidence rate of the disease is high, and its
morbidity and mortality rate are in a certain degree, which will
significantly reduce the quality of life of patients and threaten
the safety of them (8). At present,
the clinical treatment includes conservative drug therapy and
minimally invasive vascular intervention, whose curative effects
have to be further improved, so patients have to receive surgical
treatments (9). Although Ilizarov
transverse tibial bone transport and vascular regeneration and
circulation reconstruction is still in the promotion stage
clinically, it has been widely recognized that the transport can
stimulate the regeneration of periosteum and tibial bone marrow
(10), thus promoting local
micro-arterial regeneration to reconstruct the mechanism of lateral
circulation network. In some studies, this technique has been
applied to the treatment of the diabetic foot (11), which achieves significant curative
effects with the advantages of minimal trauma, rapid postoperative
recovery and low treatment cost, and it can effectively reduce and
avoid the risk of amputation (12).
In this study, it was applied to the treatment of lower limb
ischemic diseases.
In the present study, comparisons of the diameter
and blood flow of lower limb arteries in the paretic side between
the two groups after intervention showed that compared with the
effect of expanding the femoral artery with PTBA, diameters and
blood flows of the femoral, popliteal, posterior tibial and
dorsalis pedis artery of patients after intervention in the
observation group were significantly larger than those of patients
in the control group, suggesting that the application of Ilizarov
traverse tibial bone transport and microcirculation reconstruction
to lower limb ischemic diseases can effectively expand the diameter
of main lower limb arteries and improve the blood flow. At the same
time, the analysis on the variation trends of dorsal foot skin
temperature and the expression area of VEGFs in the two groups at
different observation time-points manifested that dorsal foot skin
temperature at 1 day, 1 week and 1 month after operation in
patients in the observation group was significantly higher than
that in patients in the control group, and the expression area of
VEGFs was significantly larger than that in patients in the control
group, suggesting that the application of Ilizarov traverse tibial
bone transport and microcirculation reconstruction to lower limb
ischemic diseases can effectively elevate the lower limb
temperature, and the significantly increased expression level of
VEGFs promoting vascular regeneration contributes to the
revascularization of the lower limbs and improves clinical symptoms
of patients. Besides, comparisons of wound healing time and
disappearance time of pains between the two groups indicated that
wound healing time and disappearance time of pains in the
observation group were earlier than those in the control group,
suggesting that Ilizarov transverse tibial bone transport and
microcirculation reconstruction is of great significance for
promoting the healing of lower limb ulcer and (or) gangrene and
relieving lower limb pains. Finally, comparison of the improvement
degree of clinical symptoms at 1 month after operation between the
two groups revealed that the improvement degree of intermittent
claudication, rest pain and lower limb ulcers or gangrene in the
observation group was significantly higher than that in the control
group, suggesting that the application of Ilizarov traverse tibial
bone transport and microcirculation reconstruction to lower limb
ischemic diseases is of more significant clinical importance for
improving the clinical symptoms of patients than PTBA intervention
treatment.
The principle of Ilizarov bone transport technique
is to repeatedly stimulate the tibial bone marrow, the mitosis of
vascular endothelial cells and tissue regeneration through the
tension-stress effect so as to reconstruct blood circulation and
avoid amputation (13). Fenestration
operation was conducted on the tibia, which effectively reduced the
bone pressure and relieved the occurrence of spasm in the small and
medium blood vessels, and it had great value for improving lower
limb pains, limb numbness and other symptoms (14). Meanwhile, the bone transport
effectively relieved rest pain and local swelling and improved the
skin color, which were considered to be related to the
reconstruction of new vessels in the lower limbs and the formation
of lateral circulation (15). In
addition, in combination with external fixation therapy (16), the bone transport could be repeatedly
adjusted and modified during treatment, thus contributing to better
microcirculation construction after the transport, while the both
sides of the end ring could be separated from the main rod at any
time, which was conducive to debridement, dressing change and wound
observation, and even to the reduction of complications such as
postoperative infection (17). In
order to improve the operation results, it was advised in this
study to avoid using the tourniquet and electric knife during
operation so as toavoid the stimulation and damage of iatrogenic
injuries to lower limb vessels (18). Besides, in the process of
fenestration operation on periosteum, the periosteum should be kept
integrated as much as possible, and it would be sutured at the end
of operation (19). In the process
of osteotomy, the protection of periosteum and bone marrow should
be strengthened (20).
In conclusion, Ilizarov traverse tibial bone
transport and microcirculation reconstruction in the treatment of
lower limb ischemic diseases effectively improves the blood supply
of lower limb arteries, enhances local vascular growth ability,
improves local temperature, relieves clinical symptoms and promotes
wound healing.
Acknowledgements
Not applicable.
Funding
Not funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
QZ and JZ designed the study and performed the
experiments, QZ, FG and HS collected the data, QZ and FG analyzed
the data, QZ and JZ prepared the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The First Affiliated Hospital of Nanjing Medical University
(Nanjing, China). All the patients signed the informed consent
Patient consent for publication
Not applicable.
Competing interests
All authors have no conflict of interest to
declare.
References
|
1
|
Wan J, Yang Y, Ma ZH, Sun Y, Liu YQ, Li GJ
and Zhang GM: Autologous peripheral blood stem cell transplantation
to treat thromboangiitis obliterans: Preliminary results. Eur Rev
Med Pharmacol Sci. 20:509–513. 2016.PubMed/NCBI
|
|
2
|
Osman W, Alaya Z, Kaziz H, Hassini L,
Braiki M, Naouar N and Ben Ayeche ML: Treatment of high-energy
pilon fractures using the ILIZAROV treatment. Pan Afr Med J.
27:1992017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hefny H, Elmoatasem EM, Mahran M, Fayyad
T, Elgebeily MA, Mansour A and Hefny M: Ankle reconstruction in
fibular hemimelia: New approach. HSS J. 13:178–185. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sala F, Thabet AM, Capitani P, Bove F,
Abdelgawad AA and Lovisetti G: Open Supracondylar-Intercondylar
fractures of the femur treatment with taylor spatial frame. J
Orthop Trauma. 31:546–553. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Popkov D: Guided growth for valgus
deformity correction of knees in a girl with osteopetrosis: A case
report. Strateg Trauma Limb Reconstr. 12:197–204. 2017. View Article : Google Scholar
|
|
6
|
Chaudhary MM: Infected nonunion of tibia.
Indian J Orthop. 51:256–268. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pobloth AM, Schell H, Petersen A,
Beierlein K, Kleber C, Schmidt-Bleek K and Duda GN: Tubular
open-porous β-tricalcium phosphate polycaprolactone scaffolds as
guiding structure for segmental bone defect regeneration in a novel
sheep model. J Tissue Eng Regen Med. May 8–2017.(Epub ahead of
print). doi: 10.1002/term.2446.2017.
|
|
8
|
Ertürk C, Altay MA, Altay N, Öztürk IA,
Baykara İ, Sert C and Işıkan UE: The effect of 2 different surgical
methods on intracompartmental pressure value in tibial shaft
fracture: An experimental study in a rabbit model. Ulus Travma Acil
Cerrahi Derg. 23:85–90. 2017.PubMed/NCBI
|
|
9
|
Zak L and Wozasek GE: Tibio-talo-calcaneal
fusion after limb salvage procedures-A retrospective study. Injury.
48:1684–1688. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xu J, Zhong WR, Cheng L, Wang CY, Wen G,
Han P and Chai YM: The combined use of a neurocutaneous flap and
the ilizarov technique for reconstruction of large soft tissue
defects and bone loss in the tibia. Ann Plast Surg. 78:543–548.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mukhopadhaya J and Raj M: Distraction
osteogenesis using combined locking plate and Ilizarov fixator in
the treatment of bone defect: A report of 2 cases. Indian J Orthop.
51:222–228. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Simpson AH, Keenan G, Nayagam S, Atkins
RM, Marsh D and Clement ND: Low-intensity pulsed ultrasound does
not influence bone healing by distraction osteogenesis: A
multicentre double-blind randomised control trial. Bone Joint J.
99-B:494–502. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Iliopoulos E, Morrissey N, Cho S and
Khaleel A: Outcomes of the Ilizarov frame use in elderly patients.
J Orthop Sci. 22:783–786. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mudiganty S, Daolagupu AK, Sipani AK, Das
SK, Dhar A and Gogoi PJ: Treatment of infected non-unions with
segmental defects with a rail fixation system. Strateg Trauma Limb
Reconstr. 12:45–51. 2017. View Article : Google Scholar
|
|
15
|
Mongon MLD, Ribera FC, de Souza AMA,
Sposito AL, Belangero WD and Livani B: Pedicled sensate composite
calcaneal flap in children with congenital tibial pseudoarthrosis.
J Pediatr Orthop. 37:e271–e276. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hamahashi K, Uchiyama Y, Kobayashi Y and
Watanabe M: Delayed methicillin-resistant Staphylococcus
aureus-induced osteomyelitis of the tibia after pin tract
infection: Two case reports. J Med Case Reports. 11:232017.
View Article : Google Scholar
|
|
17
|
Sivakumar R, Mohideen MG, Chidambaram M,
Vinoth T, Singhi PK and Somashekar V: Management of large bone
defects in diaphyseal fractures by induced membrane formation by
masquelet's technique. J Orthop Case Rep. 6:59–62. 2016.PubMed/NCBI
|
|
18
|
Górski R, Żarek S, Modzelewski P, Górski R
and Małdyk P: Stress fractures of tibia treated with ilizarov
external fixator. Ortop Traumatol Rehabil. 18:337–347. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rohilla R, Siwach K, Devgan A, Singh R,
Wadhwani J and Ahmed N: Outcome of distraction osteogenesis by ring
fixator in infected, large bone defects of tibia. J Clin Orthop
Trauma. 7 Suppl 2:201–209. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Aktuglu K, Günay H and Alakbarov J:
Monofocal bone transport technique for bone defects greater than 5
cm in tibia: Our experience in a case series of 24 patients.
Injury. 47 Suppl 6:S40–S46. 2016. View Article : Google Scholar : PubMed/NCBI
|