Introduction
Acute multiple trauma is a common disease in clinic,
especially in emergency rescue, which will not only develop more
rapidly, but also greatly increase the mortality rate if it occurs
or is complicated by multiple organ dysfunction syndrome (MODS),
causing adverse effects on the prognosis (1). Numerous studies have shown that when
patients suffer from acute multiple trauma, the inflammation out of
control will lead to the occurrence of MODS, namely the unbalance
between inflammatory response system composed of immune
inflammatory cells and tissues and anti-inflammatory response
system, among which immune inflammatory cells play key roles
(2). At present, finding a detection
method that can predict MODS quickly and effectively is a common
problem (3,4). Many MODSs are developed from systemic
inflammatory response syndrome (SIRS); nuclear factor-κB (NF-κB) in
neutrophils is a mediator involved in the genetic transcription and
regulation of inflammatory factors, while interleukin-6 (IL-6) is
one of the common factors leading to inflammation (5). When the body is exposed to pathogenic
factors, a variety of cells in the body can be induced to produce
cytokines, such as macrophages and Kupffer cells. The most common
cytokines of MODS are tumor necrosis factor (TNF), IL, among which
TNF-α occupies a major position. The injection of high-dose TNF-α
into the human body can induce the occurrence of SIRS, eventually
leading to MODS (6,7). Therefore, the occurrence of MODS in
patients with acute multiple trauma was predicted in this study
through detecting the NF-κB, IL −6 and TNF-α levels in peripheral
blood, helping the clinical diagnosis and treatment.
Materials and methods
General data
A total of 70 patients diagnosed with severe
multiple trauma in Emergency Department of Sichuan Provincial
People's Hospital (Chengdu, China) from April 2014 to April 2016
were selected and retrospectively analyzed. The patients enrolled
were divided into the MODS group (n=25), including 18 males and 7
females with an average of 34.6±7.6 years old, and the non-MODS
group (n=45), including 28 males and 17 females with an average of
33.8±8.5 years old. The histories of drinking, smoking and chronic
diseases of all patients were collected. There were no
statistically significant differences in general data and past
medical history between the MODS and non-MODS groups (P>0.05),
and the data were comparable (Table
I). Inclusion criteria: patients diagnosed with severe multiple
trauma; patients aged above 14 years old; patients admitted within
6 h after trauma. Exclusion criteria: patients receiving
glucocorticoid or immunosuppressive therapy at admission; patients
aged below 14 years old; patients with severe liver or kidney
disease, heart disease, cardiogenic shock or cancer; pregnant
women; patients with incomplete clinical data or who quit halfway.
The study was approved by the Ethics Committee of Sichuan
Provincial People's Hospital (Chengdu, China) and written informed
consents were signed by the patients and/or guardians.
 | Table I.Comparisons of general data between
the two groups. |
Table I.
Comparisons of general data between
the two groups.
| Groups | n | Male/female | Age (years) | Drinking (n/%) | Smoking history
(n/%) | Chronic disease
history (n/%) |
|---|
| Non-MODS | 45 |
28/17 | 33.8±8.5 | 25 (55.6%) | 27 (60.0%) | 8 (17.8%) |
| MODS | 25 | 18/7 | 34.6±7.6 | 13 (52.0%) | 14 (56.0%) | 5 (20.0%) |
| P-value |
| 0.812 | 0.765 | 0.312 | 0.297 | 0.498 |
Methods
The injury severity scores (ISS), acute physiology
and chronic health evaluation II (APACHE II) scores, NF-κB, IL-6
and TNF-α levels in patients enrolled were detected at different
time-points (12, 24 and 48 h after admission). Peripheral venous
blood (8 ml) after anticoagulation was collected at different time
points, and the serum was separated and stored at −80°C for standby
application. 1) The level of NF-κB was detected via electrophoretic
mobility shift assay (EMSA). After specimen collection, the
nucleoprotein was extracted using the nucleoprotein extraction kit
provided by Active Motif (Carlsbad, CA, USA), and the activity of
nucleoprotein was detected via enzyme-linked immunosorbent assay
(ELISA). The optical density (OD) at the wavelength of 500 nm was
measured using the kit provided by Active Motif. 2) Detection of
IL-6 and TNF-α levels: The peripheral IL-6 and TNF-α specimens were
centrifuged at 1,800 × g for 20 min, and the upper-layer serum was
collected. The nucleoprotein was collected via ELISA and placed
into the solubilizing buffer; after incubation and washing for many
times, the goat anti-rabbit horseradish peroxidase (HRP)-labeled
polyclonal antibody (dilution, 1:1,000; cat no. 7074; Cell
Signaling Technology, Danvers, MA, USA) was added, and the mixture
was incubated and washed again. Finally, the IL-6 and TNF-α levels
were detected using the Bio-Rad 680 microplate reader provided by
Active Motif, and OD at the wavelength of 450 nm was measured. All
of the above indexes were measured by professional detection
physicians in strict accordance with the manufacturer's
instructions.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
19.0 software (SPSS, Inc., Chicago, IL, USA) was used for data
processing. Data were collected and presented as mean ± SD, ANOVA
was used for the comparison between multiple groups and the post
hoc test was the Least Significant Difference test. Multivariate
logistic regression analyses were performed for the factors with
statistically significant difference, and the area under the
receiver operating characteristic (ROC) curve (AUC) was calculated.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at admission between the two
groups
The peripheral serum was collected from patients at
12 h after admission to detect the serum NF-κB, IL-6 and TNF-α
levels. The ISS, APACHE II score, NF-κB, IL-6 and TNF-α levels in
the MODS group were higher than those in the non-MODS group, and
the differences were statistically significant (P<0.05)
(Table II).
 | Table II.Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at admission between the two
groups. |
Table II.
Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at admission between the two
groups.
| Groups | n | ISS | APACHE II score | NF-κB | IL-6 (µg/l) | TNF-α (ng/ml) |
|---|
| Non-MODS | 45 | 18.3±2.8 | 11.9±2.6 | 1.0±0.3 | 23.2±4.6 | 1.96±0.23 |
| MODS | 25 | 22.6±3.9 | 18.2±3.2 | 1.4±0.2 | 35.3±3.8 | 3.62±0.21 |
| P-value |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at different time points (12, 24 and
48 h after admission) between the two groups
The ISSs, APACHE II scores, NF-κB, IL-6 and TNF-α
levels in the MODS group at 12, 24 and 48 h after admission were
higher than those in the non-MODS group. These indexes were higher
at 24 h after admission than those at 12 h after admission, and
also higher at 48 h after admission than those at 24 h after
admission. The differences were statistically significant
(P<0.05) (Table III).
 | Table III.Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at different time-points after
admission between the two groups. |
Table III.
Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at different time-points after
admission between the two groups.
| Groups | n | ISS | APACHE II score | NF-κB | IL-6 (µg/l) | TNF-α (ng/ml) |
|---|
| Non-MODS | 45 |
| 12 h
after admission |
| 18.3±2.8 | 11.9±2.6 | 1.0±0.3 | 23.2±4.6 | 1.96±0.23 |
| 24 h
after admission |
| 21.6±3.2 | 14.2±3.1 | 1.2±0.2 | 26.5±4.9 | 2.22±0.32 |
| 48 h
after admission |
| 23.2±2.7 | 15.9±2.9 | 1.3±0.3 | 28.2±3.4 | 2.91±0.41 |
| MODS | 25 |
| 12 h
after admission |
| 22.6±3.9a | 18.2±3.2a | 1.4±0.2a | 35.3±3.8a |
3.62±0.21a |
| 24 h
after admission |
| 29.3±4.2a,b | 25.3±2.7a,b | 1.9±0.2a,b | 41.6±4.1a,b |
4.93±0.24a,b |
| 48 h
after admission |
| 36.5±3.6a,c | 29.9±2.3a,c | 2.3±0.3a,c | 49.3±3.7a,c |
5.71±0.31a,c |
Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at different time-points (12, 24 and
48 h after admission) between the deceased and survivor
The ISSs, APACHE II scores, NF-κB, IL-6 and TNF-α
levels in the deceased patients at 12, 24 and 48 h after admission
were higher than those in survivors. These indexes were higher at
24 h after admission than those at 12 h after admission, and also
higher at 48 h after admission than those at 24 h after admission.
The differences were statistically significant (P<0.05)
(Table IV).
 | Table IV.Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at different time-points after
admission between the deceased and survivor. |
Table IV.
Comparisons of ISS, APACHE II score,
NF-κB, IL-6 and TNF-α levels at different time-points after
admission between the deceased and survivor.
| Groups | n | ISS | APACHE II score | NF-κB | IL-6 (µg/l) | TNF-α (ng/ml) |
|---|
| Deceased | 19 |
| 12 h
after admission |
| 25.3±2.9a | 29.5±3.5a | 1.5±0.2a | 29.3±4.6a |
4.66±0.25a |
| 24 h
after admission |
| 26.5±2.6a,b | 32.3±4.1a,b | 1.8±0.2a,b | 35.3±3.9a,b |
4.93±0.31a,b |
| 48 h
after admission |
|
28.3±1.9a,c |
33.6±3.3a,c |
2.1±0.3a,c |
45.9±4.2a,c |
5.63±0.22a,c |
| Survivor | 51 |
| 12 h
after admission |
| 19.5±3.2 | 18.3±4.4 | 1.0±0.1 | 24.4±5.1 | 1.72±0.36 |
| 24 h
after admission |
| 20.8±2.9 | 19.6±3.9 | 1.2±0.2 | 26.3±4.4 | 2.74±0.29 |
| 48 h
after admission |
| 26.2±2.3 | 22.3±4.2 | 1.4±0.1 | 28.1±3.2 | 3.95±0.41 |
Multivariate logistic regression
analyses of influencing factors of MODS in patients with severe
multiple trauma
The analyses with ISS, APACHE II score, NF-κB, IL-6
and TNF-α levels as the independent variables, and whether MODS
occurred as the dependent variable showed that the ISS, APACHE II
score, NF-κB, IL-6 and TNF-α levels were not the risk factors of
MODS in patients with severe multiple trauma, and the differences
were not statistically significant (P>0.05) (Table V).
 | Table V.Multivariate logistic regression
analyses of influencing factors of MODS in patients with severe
multiple trauma. |
Table V.
Multivariate logistic regression
analyses of influencing factors of MODS in patients with severe
multiple trauma.
| Indexes | P-value | Odds ratio
(OR) | 95% confidence
interval (CI) |
|---|
| ISS | 0.823 | 0.919 | 0.659, 1.087 |
| APACHE II
score | 0.610 | 0.957 | 0.823, 1.316 |
| NF-κB | 0.463 | 3.562 | 0.314, 3.989 |
| IL-6 | 0.185 | 2.159 | 0.992, 4.024 |
| TNF-α | 0.366 | 1.944 | 0.765, 3.566 |
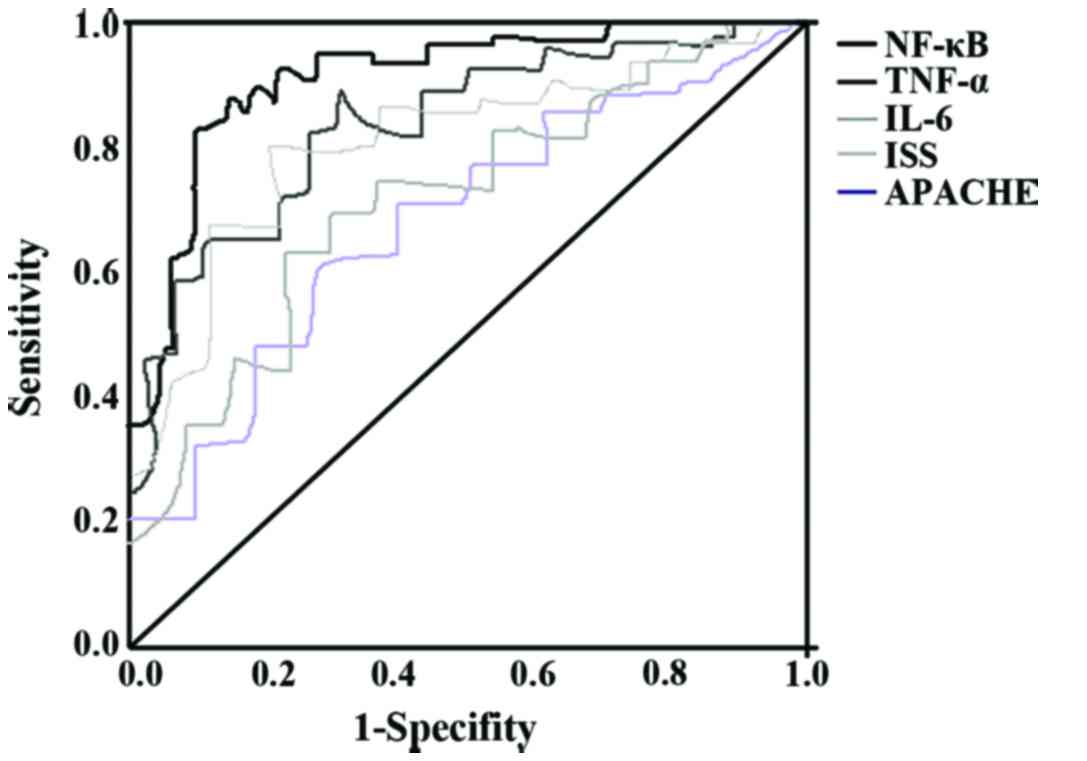
ROC curves
AUCs of ISS, APACHE II score, NF-κB, IL-6 and TNF-α
levels in predicting MODS were 0.598, (95% CI=0.483, 0.812), 0.664
(95% CI=0.614, 0.903), 0.796 (95% CI=0.699, 0.954), 0.835 (95%
CI=0.713, 0.095) and 0.803 (95% CI=0.705, 0.903), respectively; the
cut-off values were as follows: ISS >22 points; APACHE II score
>14 points; NF-κB >1.20; IL-6 >25.1 µg/l and TNF-α
>2.20 ng/ml. The sensitivities were 66.7, 75.2, 79.3, 83.7 and
86.0%, respectively, and the positive likelihood ratios were 2.12,
2.63, 3.51, 2.98 and 3.53, respectively, at the cut-off values
(Fig. 1).
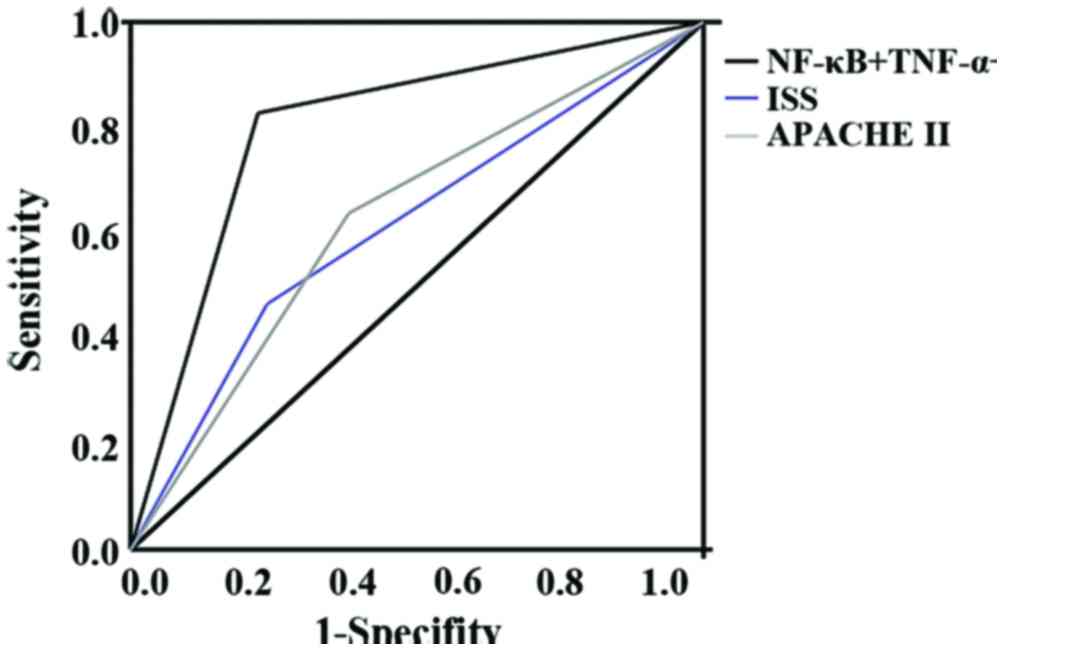
ROC curves of combined detection of
NF-κB, IL-6 and TNF-α levels and ISS and APACHE II score of
patients with severe multiple trauma in predicting MODS
AUCs of ISS >22 points and APACHE II score >14
points in predicting MODS were 0.598 (95% CI=0.483, 0.812) and
0.664 (95% CI=0.614, 0.903), which were lower than that of combined
detection of NF-κB >1.20; IL-6 >25.1 µg/l and TNF-α >2.20
ng/ml in peripheral blood in predicting MODS (0.853, 95% CI=0.659,
0.977). and the differences were statistically significant
(P<0.001) (Fig. 2).
Discussion
In the disease or severe trauma, failures of two or
more organs in the body consecutively or simultaneously are defined
as multiple organ failure (MOF). At present, more and more theories
argue that MODS, instead of MOF, is more reasonable and scientific
(8). Clinically, acute multiple
trauma is a common disease in emergency, often seriously
threatening the life of patients. There are also increasingly more
studies on severe multiple trauma, but there is a lack of more
accurate predictive indexes for severe multiple trauma or MODS
(9). After severe trauma, infection
or major surgery, the body will exhibit a significant acute
inflammatory reaction, thus causing abnormal inflammatory mediator
expression levels, among which inflammatory as well as
anti-inflammatory mediators are the most common (10). In particular, inflammatory and
anti-inflammatory mediators are in a relatively unstable state in
patients with severe multiple trauma (11), and the expression levels of
anti-inflammatory mediators are enhanced with the increase in
inflammatory mediators, showing balance and fluctuation between
inflammatory and anti-inflammatory mediators (12). In addition to the expression of
inflammatory mediators, more indexes are involved in the regulation
process of inflammatory mediators, which can indirectly reflect the
degree of inflammatory response (13). Many studies have shown that NF-κB is
an important regulatory factor in the inflammatory response
process, which in turn affects the expression disorder of
inflammatory mediators. Moreover, NF-κB activates the immune system
in the body via early activation, exhibiting SIRS (14); continuous attack and multiple organ
dysfunctions under stress state result in MODS (15). After activation, NF-κB enters
neutrophils and monocytes quickly, and specifically binds to gene
promoter and enhancer, which is expressed by cell regulatory
factors and promotes the synthesis and release of a large number of
inflammatory factors after binding and regulation, such as IL-6,
IL-8 and TNF-α. The most important factors stimulating the
synthesis of acute reactive protein in SIRS are IL-6 and TNF-α
(16,17).
In this study, the ISS, APACHE II score, NF-κB, IL-6
and TNF-α levels in the MODS group were higher than those in the
non-MODS group. With the prolongation of time, these indexes were
increased. The ISS, APACHE II score, NF-κB, IL-6 and TNF-α levels
in the deceased patients were obviously higher than those in
survivors. With the prolongation of time, these indexes were
increased, and the differences were statistically significant. It
can be seen that ISS and APACHE II score, or NF-κB, IL-6 and TNF-α
have great reference significance in the diagnosis of MODS.
However, the multivariate logistic regression analyses of
influencing factors of MODS in patients with severe multiple trauma
showed that the ISS, APACHE II score, NF-κB, IL-6 and TNF-α levels
were not the risk factors of MODS in patients with severe multiple
trauma. Besides, the ROC curves of combined detection of NF-κB,
IL-6 and TNF-α levels and ISS and APACHE II score of patients with
severe multiple trauma in predicting MODS revealed that AUCs of ISS
>22 points and APACHE II score >14 points in predicting MODS
were significantly lower than that of combined detection of NF-κB
>1.20. IL-6 >25.1 µg/l and TNF-α >2.20 ng/ml in peripheral
blood, suggesting that the combined detection of NF-κB, IL-6 and
TNF-α in peripheral blood of patients with severe multiple trauma
has important significance in predicting MODS (18).
The pathogenesis and pathophysiological process of
MODS are extremely complex, and the states of corresponding
inflammatory and anti-inflammatory mediators at different stages of
disease are different (19).
Maintaining the relative balance between inflammation and
anti-inflammation in human body is the most critical step in the
treatment of MODS. The detection of inflammation-related factors,
such as IL-6 and TNF-α, can reflect the autoreaction. Moreover, the
intervention in NF-κB activity can ultimately interfere in the
pathogenesis of MODS and improve the prognosis (20).
Acknowledgements
Not applicable.
Funding
The present study was supported by the Scientific
Research Projects of Health and Family Planning Commission of
Sichuan Province, China (grant no. 140088).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JZ wrote the manuscript and performed EMSA and
ELISA.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Sichuan Provincial People's Hospital (Chengdu, China) and written
informed consents were signed by the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The author declares that he has no competing
interests.
References
|
1
|
Fremont RD, Koyama T, Calfee CS, Wu W,
Dossett LA, Bossert FR, Mitchell D, Wickersham N, Bernard GR,
Matthay MA, et al: Acute lung injury in patients with traumatic
injuries: Utility of a panel of biomarkers for diagnosis and
pathogenesis. J Trauma. 68:1121–1127. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Davenport R and Brohi K: Fibrinogen
depletion in trauma: Early, easy to estimate and central to
trauma-induced coagulopathy. Crit Care. 17:1902013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Frink M, van Griensven M, Kobbe P, Brin T,
Zeckey C, Vaske B, Krettek C and Hildebrand F: IL-6 predicts organ
dysfunction and mortality in patients with multiple injuries. Scand
J Trauma Resusc Emerg Med. 17:492009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Matsuda N, Hattori Y, Takahashi Y,
Nishihira J, Jesmin S, Kobayashi M and Gando S: Therapeutic effect
of in vivo transfection of transcription factor decoy to NF-kappaB
on septic lung in mice. Am J Physiol Lung Cell Mol Physiol.
287:L1248–L1255. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Moraes LA, Piqueras L and Bishop-Bailey D:
Peroxisome proliferator-activated receptors and inflammation.
Pharmacol Ther. 110:371–385. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cuzzocrea S, Pisano B, Dugo L, Ianaro A,
Maffia P, Patel NS, Di Paola R, Ialenti A, Genovese T, Chatterjee
PK, et al: Rosiglitazone, a ligand of the peroxisome
proliferator-activated receptor-γ, reduces acute inflammation. Eur
J Pharmacol. 483:79–93. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Marshall JC, Cook DJ, Christou NV, Bernard
GR, Sprung CL and Sibbald WJ: Multiple organ dysfunction score: A
reliable descriptor of a complex clinical outcome. Crit Care Med.
23:1638–1652. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Damiani P and Burini G: Fluorometric
determination of nitrite. Talanta. 33:649–652. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dougnac A, Riquelme A, Calvo M, Andresen
M, Magedzo A, Eugenin E, Marshall G and Gutiérrez M: Study of
cytokines kinetics in severe sepsis and its relationship with
mortality and score of organic dysfunction. Rev Med Chil.
129:347–358. 2001.(In Spanish). PubMed/NCBI
|
|
10
|
Stegmaier J, Kirchhoff C, Kanz KG, Mayer
V, Landes J, Euler E, Mutschler W and Biberthaler P: Analysis of
NF-kappaB nuclear translocation in PMN-neutrophils of major trauma
patients in the early post-traumatic period: A pilot study. World J
Surg. 30:2142–2151. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhao E, Wang L and Wen Q: Fasudil
hydrochloride differentiates bone marrow mesenchymal stem cells
into neurons via notch signaling. Neural Regen Res. 5:814–819.
2010.
|
|
12
|
Pacary E, Legros H, Valable S, Duchatelle
P, Lecocq M, Petit E, Nicole O and Bernaudin M: Synergistic effects
of CoCl(2) and ROCK inhibition on mesenchymal stem cell
differentiation into neuron-like cells. J Cell Sci. 119:2667–2678.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pacary E, Petit E and Bernaudin M:
Concomitant inhibition of prolyl hydroxylases and ROCK initiates
differentiation of mesenchymal stem cells and PC12 towards the
neuronal lineage. Biochem Biophys Res Commun. 377:400–406. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Collison LW, Workman CJ, Kuo TT, Boyd K,
Wang Y, Vignali KM, Cross R, Sehy D, Blumberg RS and Vignali DA:
The inhibitory cytokine IL-35 contributes to regulatory T-cell
function. Nature. 450:566–569. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Neunaber C, Zeckey C, Andruszkow H, Frink
M, Mommsen P, Krettek C and Hildebrand F: Immunomodulation in
polytrauma and polymicrobial sepsis - where do we stand? Recent Pat
Inflamm Allergy Drug Discov. 5:17–25. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Marti L, Cervera C, Filella X, Marin JL,
Almela M and Moreno A: Cytokine-release patterns in elderly
patients with systemic inflammatory response syndrome. Gerontology.
53:239–244. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li J, Li NP, Gu YF, Yang X, Lu XB, Cong
JN, Ling Y, Tang JA, Yuan XY and Wang H: Dynamic activity of
NF-kappaB in multiple trauma patients and protective effects of
ulinastain. Chin J Traumatol. 14:354–358. 2011.PubMed/NCBI
|
|
18
|
Yadav K, Zehtabchi S, Nemes PC, Miller AC,
Azher M, Durkin H and Sinert R: Early immunologic responses to
trauma in the emergency department patients with major injuries.
Resuscitation. 80:83–88. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shih HC, Huang MS and Lee CH:
Polymorphonuclear cell priming associated with NF-κB activation in
patients with severe injury is partially dependent on macrophage
migration inhibitory factor. J Am Coll Surg. 211:791–797. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li R, Zijlstra JG, Kamps JA, van Meurs M
and Molema G: Abrupt reflow enhances cytokine-induced
proinflammatory activation of endothelial cells during simulated
shock and resuscitation. Shock. 42:356–364. 2014. View Article : Google Scholar : PubMed/NCBI
|