Introduction
Hypospadias is a condition where the urethra opens
on the underside of the penis with associated ventral penile
curvature, and it is the second most common genital birth defect in
boys, following cryptorchidism. The incidence of hypospadias is
~1:200–1:300 male births, and has doubled over the past three
decades. Hypospadias correction is one of the common surgical
procedures performed by pediatric urologists (1,2). The
initial diagnosis of hypospadias is typically made during physical
exam after birth, where boys with hypospadias are found to have a
ventral skin deficiency with a dorsal hood of foreskin and an
abnormally located meatus with varying degrees of ventral penile
curvature. The standard classification of hypospadias is based on
the location of the urethral meatus: distal, midshaft, or proximal.
For operative planning, many aspects of the hypospadias information
are taken into consideration: location of the meatus and the degree
of proximal spongiosal hypoplasia; quality of the urethral plate;
size of the glans and the depth of the navicular fossa; degree of
ventral skin deficiency and availability of the foreskin, and so
on. The most common early complications of hypospadias surgery
include urethral fistula, stricture and diverticulum dilatation
(3). Both the occurrences of
urethral fistula urethral stricture are related to the blood supply
of molding material for urethra reconstruction (4).
There are quite detailed research on blood supply of
normal penis, and the recognition towards prepuce vascular
distribution is relatively consistent (5). But quite limited research has been done
in prepuce vascular distribution in children with hypospadias,
especially in the Chinese. A correct recognition of prepuce
vascular distribution in child cases with hypospadias is very
important to understand the blood supply of molding urethra,
operative prognosis and surgical operation.
In this report, the authors generalized, analyzed
and summarized vascular distribution of vessel pedicle in children
with hypospadias through transmitting prepuce with cold light
illuminator, and carried out a prospective study to discuss the
blood supply of different vascular distribution types as well as
their relevance to short-term complications after operation.
Patients and methods
Patients
Our study received approval of the Ethics Committee
of Guangzhou Women and Childrens Medical Center (Guangzhou, China)
Affiliated to Capital Medical University (Beijing, China), and
informed consent was signed by the parents of the patients. This
study was conducted on primary cases with subcoronal, distal- or
mid-penile hypospadias and suitable for urethroplasty. Cases with
glanular, recurrent, or moderate-to-severe chordee were excluded
from the study. A total of 115 children with hypospadias undergoing
surgery at Beijing Children's Hospital affiliated to Capital
Medical University (Beijing, China), between October 20, 2010 and
March 2, 2011 were selected as the research objects (age range,
1–12 years; median age, 24 months; mean weight, 11.35 kg; mean
height, 87.20 cm). The surgeon was a pediatric urology surgery
specialist trained for >10 years with >15 years of experience
in hypospadias repair surgery. The surgical methods included
Duckett, ONLAY, Snograss, and MAGPI (meatal advancement and
glanuloplasty). Pedicled flaps of prepuce were cut for urethral
molding in Duckett and ONLAY (onlay island flap); peeled vascular
pedicle were to cover the new urethra in Snodgrass and MAGPI
(6).
Methods
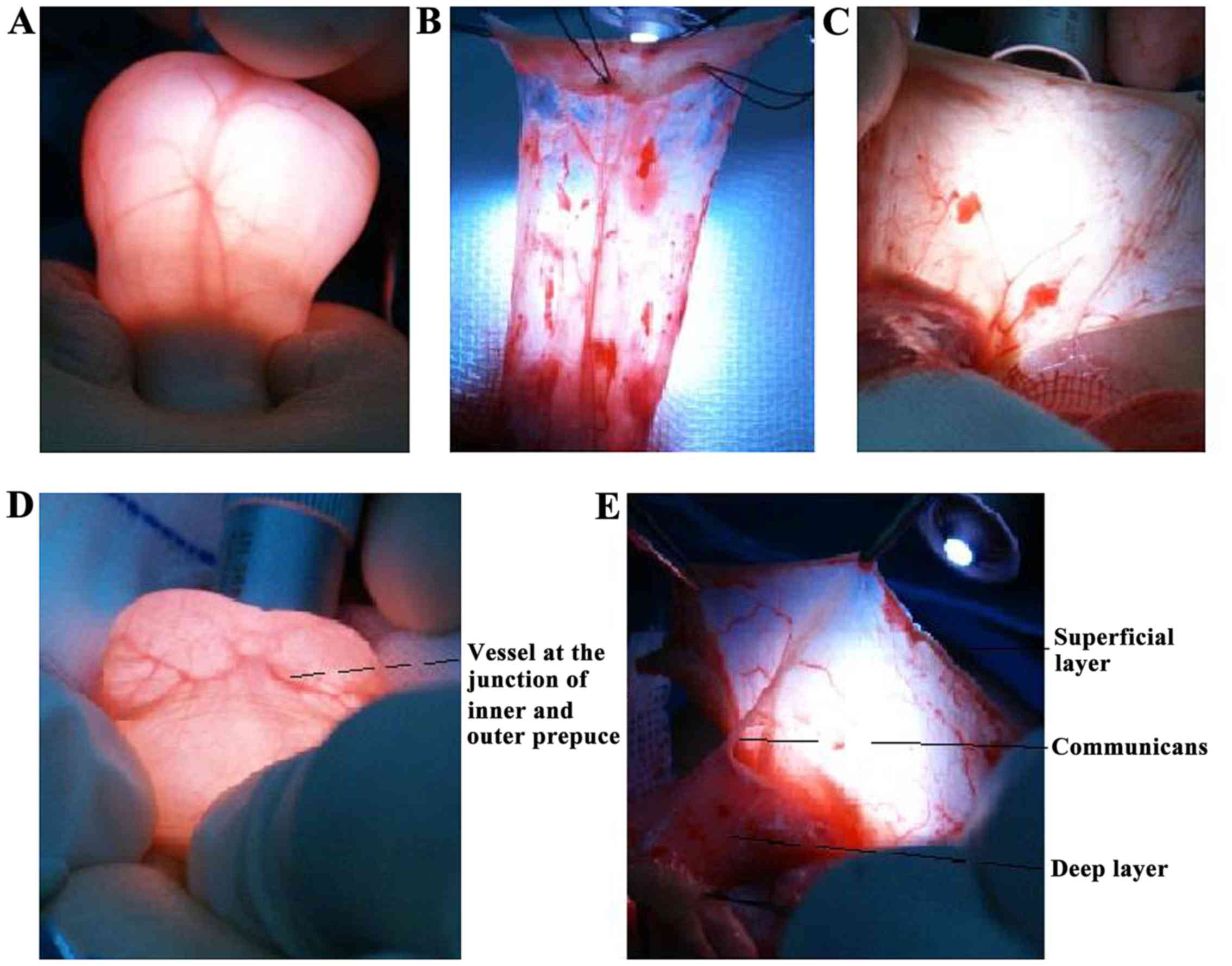
Endoscopic cold light source was used to
trans-illuminate the prepuce (before the operation), flap vascular
pedicle and residual prepuce skin (during the operation) (Fig. 1). All data were saved in the form of
photographs, and the distribution and number of blood vessels were
observed by two observers, then recorded and analyzed. Child
patients undergoing Duckett procedure were followed up for 1–5
months to understand the occurrence of complications considering
that the flap used in molding urethra by Duckett mostly depends on
the blood supply from pedicle blood vessels.
Statistical analysis
Data were analyzed by SPSS 19.0 software (IBM Corp.,
Armonk, NY, USA). Data were analyzed using the Chi-square test, and
differences between groups were considered significant at
P<0.05.
Results
Vascular distribution within the
vessel pedicle
The number and distribution of superficial vessels
within the prepuce varied, and there was no clear relationship
between the superficial and deep vessels of the prepuce. In terms
of the overall prepuce, the superficial vessels and deep vessels
were easily distinguishable (Fig.
1A); however, the deep vessels were usually on or leaned
towards the middle line (Fig. 1A).
These blood vessels were later horizontally distributed at the
junction of the inner and outer prepuce (Fig. 1D). The deep layer of the superficial
fascia together with the skin at the junction of the inner and
outer prepuce constituted a peduncle island skin flap, and the
superficial layer of the superficial fascia supplied blood to the
remaining skin (Fig. 1B).
Occasionally, a ramus communicans was visible between the
superficial and deep layers of the superficial fascia or between
the superficial fascia and deep fascia (Fig. 1E).
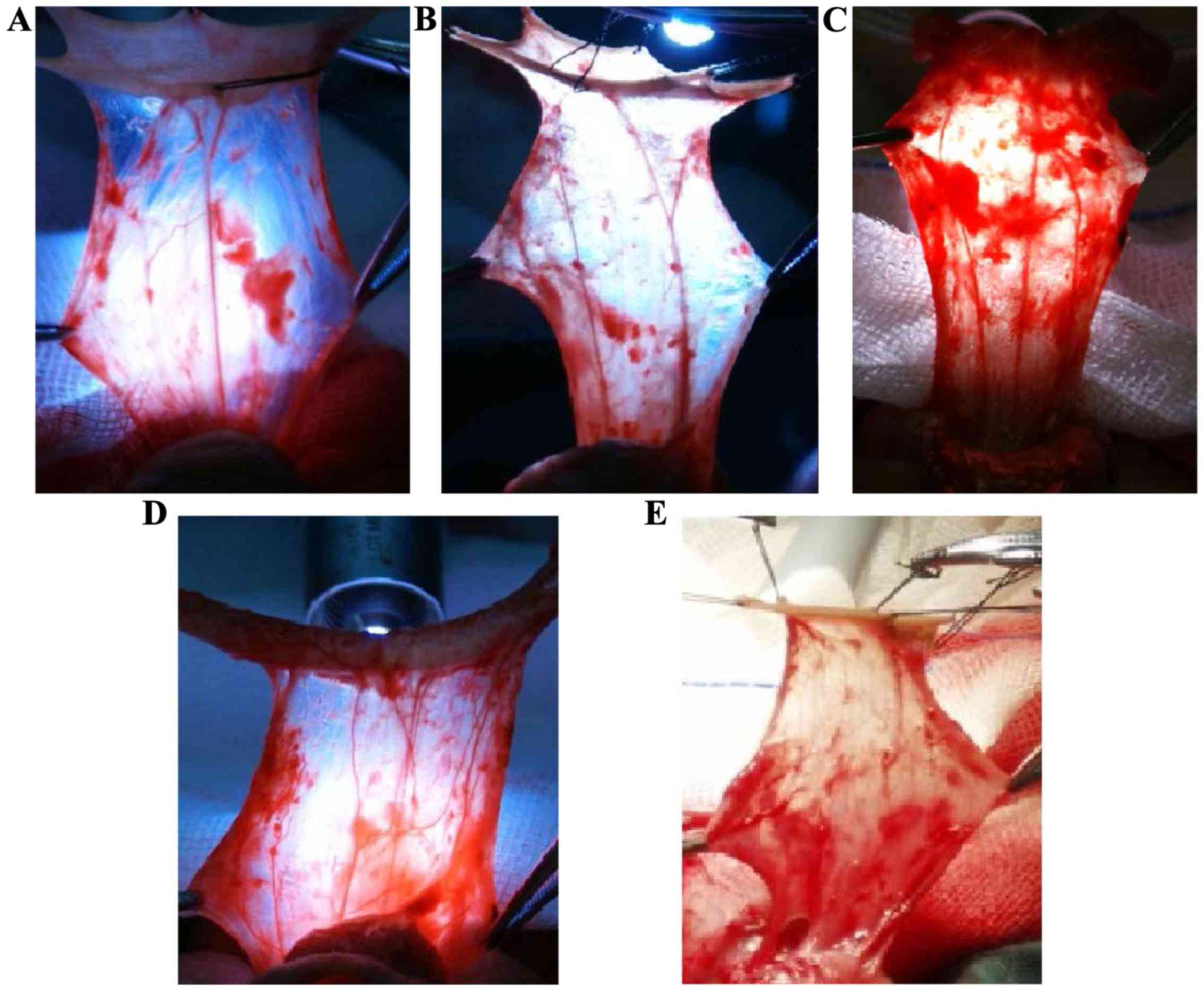
The vascular distribution and length of the vascular
pedicle (deep layer of the superficial fascia) were obviously
regular. When based on the number of predominant blood vessels, the
following four types of vascular pedicles were identified: i) one
blood vessel was predominant (Fig.
2A); ⅱ) two blood vessels were predominant (Fig. 2B); ⅲ) numerous blood vessels (≥3)
were presented (Figs. 2C and D); and
ⅳ) no predominant blood vessel was presented (e.g., no definite
axial vessel displayed a network distribution) (Fig. 2E). All types of predominant vessels
were axially distributed, and then showed a transverse distribution
and formed numerous reticular lateral branches at the junction of
the inner and outer prepuce. The predominant vessels in the same
pedicle displayed no obvious difference in their development, and a
majority was symmetrically distributed along the middle line of the
pedicle. The patients were assigned to four different groups based
on their meatal location (Table I).
Next, the Chi-square test showed that the number of predominant
vessels was not directly related to the meatal location
(P=0.449).
 | Table I.The vascular distribution type data
for all groups according to their meatal location. |
Table I.
The vascular distribution type data
for all groups according to their meatal location.
| Vascular distribution
(type) | Glanular and
coronal | Penile | Penoscrotal | Perineal | Total | Rate (%) |
|---|
| 1 | 10 | 20 | 18 | 1 | 49 | 42.6 |
| 2 | 7 | 13 | 17 | 2 | 39 | 33.9 |
| Numerous | 4 | 5 | 6 | 4 | 19 | 16.5 |
| No predominant
vessels | 1 | 3 | 3 | 1 | 8 | 7 |
Follow-up
Eighty-three children were treated with Duckett
procedure. Seventy-nine of the children received follow-up and four
were lost to follow-up. The follow-up findings showed: i) eight
cases had urethral fistula and five cases had urethral stricture
(Table II); and ⅱ) the Chi-square
test showed that the number of predominant vessels was not
significantly related to urethral fistula (P=0.088) or stricture
(P=0.866) (Table II).
 | Table II.The occurrence of urethral fistula and
stricture by vascular distribution type in follow-up group. |
Table II.
The occurrence of urethral fistula and
stricture by vascular distribution type in follow-up group.
| Vascular distribution
pattern | Total no. of
follow-ups | No. of cases with
urethral fistula | No. of cases with
urethral stricture | Urethral fistula rate
(%) | Urethral stricture
rate (%) |
|---|
| 1 | 36 | 2 | 3 | 5.6 | 8.3 |
| 2 | 26 | 5 | 1 | 19.2 | 3.8 |
| Numerous | 14 | 0 | 1 | 0.0 | 7.1 |
| No predominant
vessels | 3 | 1 | 0 | 33.3 | 0.0 |
| Total | 79 | 8 | 5 | 10.1 | 6.3 |
Discussion
Surgery is the only curative treatment for
hypospadias. The frequently used Duckett surgical method (7) is ideal for achieving a one-step repair
of hypospadias accompanied by chordee of the penis. Duckett
procedure has been performed with increasing success at Beijing
Children's Hospital affiliated with the Capital Medical University
for ~30 years (8), and its most
common short-term complications are urethral fistula, stricture,
and diverticulum dilatation. The occurrence of urethral fistula and
stricture may result from local tissue ischemia and necrosis of the
molding material used for urethra reconstruction. Moreover,
preservation of blood supply to the island flap and remaining
prepuce skin may be a key factor for improving the success rate of
Duckett procedure and reducing the incidence of complications
(9–11). Therefore, an accurate assessment of
vascular distribution in the prepuce of children with hypospadias
may create the foundation for improving the success rate of
hypospadias treatment, and plays a critical role in preventing
postoperative urethral fistula and stricture.
The distribution of vasculature in the normal
prepuce is well-known. It is generally believed that blood vessels
in the prepuce have two layers which can be easily separated. The
junction of the inner and outer prepuce has the most abundant blood
supply (12–15) and can serve as an island flap
(7,9,16–19).
This type of vascular distribution is the anatomic basis of Duckett
procedure, as it not only ensures blood supply to the flap, but
also prevents penis skin necrosis, which has been demonstrated once
again in this study.
Although Duckett procedure has been used for >30
years since its initial description, and the flap design takes the
vessel present in the foreskin into account. There has been no
significant improvement in the success rate of the procedure. The
lack of improved success is related to surgical skills,
postoperative management by the operator, and the medical
conditions of the operated children. However, some scholars argued
that the blood supply to a prepuce affected by hypospadias varies
greatly, and could be irregular. In other words, the actual factors
that directly affect blood flow to the prepuce, and the degrees of
variation in blood flow are not yet fully recognized and understood
(20). Perovic and Radojicic
(21) (2003) and Yucel et al
(22) (2004) studied vascular
distribution in hypospadias patients by using methods such as
trans-illumination with a cold light source, microscopic
observations after an injection of gelatin and Indian ink,
methylene blue injection, and 3-D computer reconstruction after
tissue sectioning. Both of those investigators identified four
types of prepuce vascular distribution: i) one predominant blood
vessel; ⅱ) two predominant blood vessels; ⅲ) two predominant blood
vessels with ramus communicans (H-like form); and ⅳ) no predominant
blood vessel (net-like form). They also demonstrated the accuracy
of data obtained by transillumination through the prepuce with a
cold light source. While our current study used the same cold light
method, the overall vascular distributions did not adhere to the
rules reported by Perovic and Radojicic (21) and Yucel et al (22). Furthermore, we found that vascular
distribution on the peduncle island skin flap was very regular. The
distribution law pertaining to blood vessels found in the deep
foreskin region as summarized in this study was similar to the
general blood vessel distribution law described by Cağrı Savas
et al (24). We suspect that
the latter law reflects the former law. This is because prior to
performing the transillumination test on foreskin with a cold light
source, normal saline was injected into the foreskin to cause
edema. This allowed superficial and deep vessels in the foreskin to
be displayed in a clear hierarchy to be easily identified (Fig 1A). As Cağrı Savas et al
(24) did not perform that step,
direct transillumination with a cold light source did not help to
distinguish between superficial and deep vessels. As a result,
Cağrı Savas et al (24)
observed the distribution of all superficial and deep vessels, and
the deep vessels were thicker than the superficial vessels. When
the foreskin was observed as a whole, deep vessel might have been
mistakenly identified as main vessels.
Yucel et al (22) reported that the frequency of a
net-like arterial system (no predominant blood vessel) was higher
in more severe hypospadiac prepuces; however, this phenomenon was
not observed in our current study (Table
I). Moreover, we verified the simplicity and practicability of
performing trans-illumination through the prepuce with a cold light
source. It is possible to observe the vascular distribution and
running of the prepuce in a clear and intuitive manner using this
method. Perovic and Radojicic (21)
reported that it is easier to create a peduncle island flap with a
good blood supply in patients with a predominant vessel. While
creating a peduncle island flap is not recommended for patients
without an axial predominant vessel, such patients can still be
treated with a stage operation. However, in our study, urethral
fistula and stricture showed no association with the number of
foreskin vascular pedicles, and there was no obvious difference in
the incidences of urethral fistula and stricture between patients
with and without vessels in the vessel pedicle. It is possible that
blood supply to the neourethra is not only determined by the
predominant blood vessel in the pedicle, but also by tissue
surrounding the neourethra and remaining foreskin. Moreover, tissue
surrounding the neourethra and the remaining foreskin might provide
sufficient blood supply for the neourethra. Free grafts have been
used to repair hypospadias for many years with a high success rate
(23). Therefore, it is not always
necessary to totally dissociate the vessel pedicle from foreskin
tissue to retain all of the blood vessels in the vessel pedicle;
instead, it is necessary to ensure that the vessels are not
damaged. Trans-illumination with a cold light source can help
surgeons to avoid vessel damage. Furthermore, the number of
predominant vessels should not be the basis for determining whether
to use a stage operation or a one-stage operation for hypospadias
repair.
Cağrı Savas et al (24) reported that microvessel density was
significantly decreased in hypospadiac children, and was negatively
correlated with the severity of the condition. This finding
suggests that blood supply to the neourethra or the occurrence of
postoperation complications may be associated with microvessel
density. Ceyhan et al (25)
studied this possibility, and reported that reduced preputial
microvessel density did not influence blood flow in cases of distal
hypospadias. However, the relationship between blood flow and
preputial microvessel density in other types of hypospadias (e.g.,
degrees III and IV) has not been investigated. Moreover, the
association between microvessel density and surgical results
(occurrence of complications) has not been reported, and requires
further study.
In conclusion, the deep blood vessel distribution of
prepuce in patient with hypospadias can be divided into four types.
There is no exact congruent relationship between the type of
vascularization and the meatal location. There are no significant
differences in blood supply of prepuce among the different types.
Vascularization of vessel pedicle has no exact relationship to
urethral fistula or stricture. This study further demonstrates the
anatomic basis of prepuce that Duckett surgery relies on. It is not
necessary to dissociate the vessel pedicle from foreskin too much
to keep all of the vessels in the vessel pedicle. Vascular
integrity should be ensured and trans-illumination with a cold
light source can help us to avoid vessel damage.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant
from funding agencies in the public, commercial, or not-for-profit
sectors.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZZ collected the general data of patients. ZZ and NS
performed the surgery. XM helped with statistical analysis. All
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Our study received approval of the Ethics Committee
of Guangzhou Women and Childrens Medical Center (Guangzhou, China),
and informed consent was signed by the parents of the patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nelson CP, Park JM, Wan J, Bloom DA, Dunn
RL and Wei JT: The increasing incidence of congenital penile
anomalies in the United States. J Urol. 174:1573–1576. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schnack TH, Poulsen G, Myrup C, Wohlfahrt
J and Melbye M: Familial coaggregation of cryptorchidism and
hypospadias. Epidemiology. 21:109–113. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
van der Horst HJ and de Wall LL:
Hypospadias, all there is to know. Eur J Pediatr. 176:435–441.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Westenfelder M: Treatment of hypospadias.
Urologe A. 31:333–341. 1992.(In German). PubMed/NCBI
|
|
5
|
Keays MA and Dave S: Current hypospadias
management: Diagnosis, surgical management, and long-term
patient-centred outcomes. Can Urol Assoc J. 11 Suppl 1:S48–S53.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Retik AB, Mandell J, Bauer SB and Atala A:
Meatal based hypospadias repair with the use of a dorsal
subcutaneous flap to prevent urethrocutaneous fistula. J Urol.
152:1229–1231. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Duckett JW Jr: Transverse preputial island
flap technique for repair of severe hypospadias. Urol Clin North
Am. 7:423–430. 1980.PubMed/NCBI
|
|
8
|
Zhang N, Zhang W, Sun N, Bai J, Tian J, Li
M, Song H and Huang C: Application of tubularized transverse
preputial island flap urethroplasty for the repair of hypospadias.
Zhonghua Xiaoerwaike Zazhi. 31:757–760. 2010.(In Chinese).
|
|
9
|
Duckett JW: HypospadiasCampbell's Urology.
Walsh PC, Gittes RF, Perlmutter AD and Stamey TA: 2. 5th edition.
W.B. Saunders Co.; Philadelphia, PA: pp. 1969–1999. 1986
|
|
10
|
Retik AB and Borer JG:
HypospadiasCampbell's Urology. Walsh PC, Retik AB, Vaughan ED and
Wein AJ: 8th edition. W.B. Saunders Co.; Philadelphia, PA: pp.
2284–2353. 2002
|
|
11
|
Duckett JW Jr: The island flap technique
for hypospadias repair. Urol Clin North Am. 8:503–511.
1981.PubMed/NCBI
|
|
12
|
Juskiewenski S, Vaysse Ph, Moscovici J,
Hammoudi S and Bouissou E: A study of the arterial blood supply to
the penis. Anat Clin. 4:101–107. 1982. View Article : Google Scholar
|
|
13
|
Grossman JA, Caldamone A, Khouri R and
Kenna DM: Cutaneous blood supply of the penis. Plast Reconstr Surg.
83:213–216. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang F and Chen Z: Applied anatomy in
urethroplasty by penile flap with external pudendal artery. J Pract
Aesthetic Plast Surg. 13:236–237. 2002.
|
|
15
|
Chan IH and Wong KK: Common urological
problems in children: Prepuce, phimosis, and buried penis. Hong
Kong Med. J22:263–269. 2016.
|
|
16
|
Buckley J and McAninch J: Distal penile
circular fasciocutaneous flap for complex anterior urethral
strictures. BJU Int. 100:221–231. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Quartey JKM: Anatomy and blood supply of
the urethra and penisUrethral Reconstructive Surgery. Schreiter F
and Jordan GH: Springer; Berlin, Heidelberg: pp. 11–17. 2006,
View Article : Google Scholar
|
|
18
|
Brandes SB: Vascular anatomy of genital
skin and the urethra: Implications for urethral reconstruction. In:
Urethral Reconstructive SurgeryCurrent Clinical Urology. Humana
Press; pp. 9–18. 2008
|
|
19
|
Jiang XZ, Yang JF, Zeng Q, Wan B and He
LY: Transverse preputial island flap technique (Ducketts procedure)
forhypospadias repair: a report of 356 cases. Zhonghua Nan KeXue.
17:622–624. 2011.(In Chinese).
|
|
20
|
Mylchreest E, Cattley RC and Foster PM:
Male reproductive tract malformations in rats following gestational
and lactational exposure to Di(n-butyl) phthalate: An
antiandrogenic mechanism? Toxicol Sci. 43:47–60. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Perovic SV and Radojicic ZI:
Vascularization of the hypospadiac prepuce and its impact on
hypospadias repair. J Urol. 169:1098–1101. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yucel S, Guntekin E, Kukul E, Karaguzel G,
Ciftcioglu A, Melikoglu M and Baykara M: Comparison of hypospadiac
and normal preputial vascular anatomy. J Urol. 172:1973–1976;
discussion 1976. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hendren WH and Horton CE Jr: Experience
with 1-stage repair of hypospadias and chordee using free graft of
prepuce. J Urol. 140:1259–1264. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cağrı Savaş M, Kapucuoğlu N, Gürsoy K and
Başpınar S: The microvessel density of the hypospadiac prepuce in
children. J Pediatr Urol. 7:162–165. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ceyhan L, Savas Cagri M, Baspinar S, Duman
L and Büyükyavuz BI: The correlation between preputial blood flow
and microvessel density in distal hypospadias: A prospective
clinical study. J Pediatr Urol. 10:103–106. 2014. View Article : Google Scholar : PubMed/NCBI
|