Introduction
One-lung ventilation (OLV) is a common ventilation
method used in thoracic surgery (1).
A traditional double-lumen endotracheal tube is widely used in
thoracic surgery. In order to provide enough space for surgical
operation, the application of complete lung collapse is
recommended. This traditional ventilation method can cause an
imbalance in ventilation flow, thereby increasing the amount of
lung shunting and leading to hypoxemia (incidence rate of 9–27%)
(2); and the secondary lung injury
can occur. There are many studies on OLV, which are mostly limited
by reducing lung injury via changing ventilation strategy or
comparing the differences in lung injury caused by different lung
isolation tools (3–5), but there is no study on the correlation
between retaining the lung ventilation on operated side and lung
injury. With the development of visual minimally-invasive technique
of thoracic surgery, the prognosis of patients has attracted
increased attention under the condition of completing the precision
surgery (6,7). At the same time, the prognosis of
patients has been paid more attention (8,9). In this
study, a pulmonary sequestration tube device used to control the
shunt in lung was developed (China patent: CN205073462 U) (10). which can control the degree of lung
collapse during surgery while ensuing the surgical field; and the
partial lung ventilation can be retained, so as to improve the
prognosis of patients. From September 2015 to November 2016, the
effects of complete lung collapse and controlled lung collapse on
the pathology and physiology of lung were studied using the
ventilator.
Materials and methods
Animals and materials
Eighteen experimental dogs of either gender were
obtained from the Experimental Animal Center of Southern Medical
University (Guangzhou, China). The mean animal weight was 9.5–15.5
kg. Before experimentation, the dogs were fasted for 12 h without
water.
This study was approved by the Ethics Committee of
Southern Medical University (Guangzhou, China).
Animal model preparation and
grouping
After the peripheral veins were opened, 3%
pentobarbital sodium (30 mg/kg, Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany), fentanyl (2 µg/kg, Yichang Renfu
Pharmaceutical Co., Ltd.; Jiangxi, China) and cis-carbene sulfonate
(0.1 mg/kg) (Jiangsu Sinobiopharma Co., Ltd., Jiangsu, China) were
injected and the new single-lumen pulmonary sequestration tube was
inserted. An anesthesia machine (Datex-Ohmeda, Inc., Madison, WI,
USA) was used to control breathing. Sevoflurane was used to
maintain anesthesia. The oxygen concentration (FiO2) in
the inhalation gas was 100%, tidal volume was 10–15 ml/kg, and
respiratory rate was 12–16 times/min. A monitor (mindary BeneView
T8 China) was used to monitor and maintain PEtCO2 at
35–45 mmHg (1 kPa = 7.5 mmHg). During the experiment, the muscle
relaxation was maintained via intravenous injection of
cis-triptolulfonate. Limb electrocardiogram was monitored and a
temperature probe was inserted at 5 cm into the anus to monitor
rectal temperature. A blood oxygen saturation detection probe was
placed on the tongue to monitor oxygen saturation. During the
experiment, the rectal temperature was maintained at 37.5–38.5°C at
room temperature of 24–26°C and humidity of 67–73%.
The femoral tube was dislocated to monitor the mean
arterial pressure (MAP) and collect arterial blood. Femoral vein
cannulation was performed to inject lactic acid Ringer's solution
(8 ml·kg−1·h−1) using an infusion pump
(Berenger, Berlin, Germany). A Swan-Ganz floating tube (Edwards
Lifesciences, Irvine, CA, USA) was placed through right internal
jugular vein. The tube was embedded in the pulmonary artery to
monitor mean pulmonary arterial pressure (MPAP) and to collect
mixed venous blood.
After the preparation of animal model, TLV was
performed for 20 min and the dogs were randomly divided into 3
groups. The chest was opened between the fourth and fifth rib on
the right side, and right lung collapse was induced. Left lung OLV
was performed later. They were randomly divided into three groups
according to the degree of right lung collapse with 6 dogs in each
group: G1 group (100% collapse, complete right lung collapse), G2
group (90% collapse with 10% ventilation) and G3 group (50%
collapse with 50% ventilation). The catheter used in each group was
tested by aerodynamics at the factory, and the correspondence
between the lumen throughput and the minimum cuff pressure in the
tube wall was measured (Table I).
After OLV for 20 min, mixed venous blood and arterial blood were
extracted from the femoral artery and jugular vein prior to TLV
(T0), and at 30 (T1), 60 (T2), and 120 min (T3) after TLV for blood
gas analysis (11–14). The remaining venous blood and
arterial blood mixture was centrifuged (4°C, 2080 × g) for 12 min
to collect the supernatant to quantify inflammatory factors. The
supernatant was kept at −80°C before use. After OLV for 120 min,
two small lung tissue pieces were collected from the ventilated
side and the collapsed side, respectively. One lung tissue piece
was used to determine W/D and the other piece was fixed in 10%
formaldehyde solution for pathological examination.
 | Table I.Correspondence between lumen
throughput of intrapulmonary shunting balance tube and
intracapsular pressure in tube wall (mean ± SD)
cmH2O. |
Table I.
Correspondence between lumen
throughput of intrapulmonary shunting balance tube and
intracapsular pressure in tube wall (mean ± SD)
cmH2O.
| Tube no. | 0% ventilation
(G1) | 10% ventilation
(G2) | 50% ventilation
(G3) |
|---|
| 1 | 30.4±1.1 | 24.8±2.1 | 18.8±3.0 |
| 2 | 28.7±0.8 | 23.1±3.1 | 18.0±2.5 |
| 3 | 29.4±1.2 | 22.6±1.0 | 17.5±1.7 |
| 4 | 24.1±0.3 | 19.5±2.4 | 15.6±1.8 |
| 5 | 25.7±0.9 | 20.1±1.7 | 17.8±1.7 |
| 6 | 27.4±0.4 | 22.8±0.6 | 16.2±1.4 |
| 7 | 29.5±1.3 | 22.2±1.5 | 17.8±1.5 |
| 8 | 31.4±0.4 | 25.7±1.9 | 19.4±2.4 |
| 9 | 28.7±1.0 | 23.4±1.6 | 17.7±2.9 |
| 10 | 35.1±1.3 | 27.4±0.8 | 21.8±1.5 |
| 11 | 30.5±2.1 | 24.1±0.9 | 19.8±2.2 |
| 12 | 33.0±2.2 | 26.0±3.9 | 22.3±2.2 |
| 13 | 27.8±1.9 | 21.8±2.0 | 19.7±1.9 |
| 14 | 32.3±1.1 | 27.6±1.5 | 23.2±2.1 |
| 15 | 30.0±0.9 | 24.8±2.7 | 18.8±2.6 |
| 16 | 26.3±1.5 | 22.4±3.4 | 17.0±3.4 |
| 17 | 28.1±1.9 | 21.6±2.4 | 18.1±1.7 |
| 18 | 26.9±0.6 | 20.4±1.1 | 17.4±1.2 |
Hemodynamic indicators
MAP, heart rate (HR) and MPAP were measured before
blood sample collection for the comparison of hemodynamic
stability.
Oxygenation indicators
Arterial blood was taken from the femoral artery at
20 min after TLV and at 30, 60 and 120 min after OLV. A Swan-Ganz
tube was used to collect mixed venous blood. Blood gas analyzer
(Nova Biomedical, Waltham, MA, USA) was used to measure the
arterial partial pressure of oxygen (PaO2), arterial
partial pressure of carbon dioxide (PaCO2), oxygen
saturation of arterial blood (SaO2), partial pressure of
oxygen in mixed venous blood (PvO2), and mixed venous
oxygen saturation (SvO2). The pulmonary shunt rate was
calculated according to the formula of the two-compartment model of
pulmonary blood flow distribution: Qs/Qt =
(Cc'O2-CaO2)/(Cc'O2-CvO2)
× 100%, where Cc'O2 is the blood oxygen content of
pulmonary capillary.
Lung wet/dry weight ratio (W/D)
After OLV for 20 min, the chest was opened and lung
tissue was collected and washed with saline (4°C). Connective
tissue was removed and filter paper was used to remove water on the
surface. The tissue was then placed in a clean and dry glass
bottle, accurately weighed and baked in an oven at 75°C for 24 h to
calculate the W/D and to assess the degree of lung tissue
edema.
Detection of serum TNF-α and IL-6
levels via ELISA
Frozen serum was allowed to defrost completely. The
TNF-α, ICAM-1 and IL-6 levels in serum were measured using ELISA
kits according to manufacturer instructions.
Pathological examination of lung
tissue
The middle lobe of the right lung was fixed in 10%
neutral formaldehyde for 24 h, followed by dehydration and paraffin
embedding. The tissue was cut into 4 µm-thick sections which were
stained via hematoxylin and eosin (H&E). The histopathological
changes of lung tissues were observed under light microscope
(Olympus, Tokyo, Japan) and scored according to four categories: i)
alveolar hyperemia, ii) hemorrhaging, iii) alveolar or vascular
wall neutrophil infiltration or aggregation, and iv) alveolar wall
thickening and/or hyaline membrane formation. Scoring was performed
on a 0–4 point scale according to the lesion severity; 0 point: no
lesions or very mild lesions; 1 point: mild lesions; 2 points:
moderate lesions; 3 points: severe lesions; 4 points: very severe
lesions. The sum of all scores was taken as the total score of
acute lung injury (ALI) (15).
Statistical analysis
Statistical Product and Service Solutions (SPSS)
19.0 software (IBM Corp., Armonk, NY, USA) was used for analysis,
and measurement data were expressed as mean ± SD; comparisons
between groups were performed using ANOVA and the post hoc test was
LSD test. P<0.05 indicates that the difference was statistically
significant.
Results
Comparison of hemodynamic indexes
There were no significant differences in MAP and HR
between groups at each time-point (P>0.05). MPAP of the G2 and
G3 groups at T1, T2 and T3 were significantly lower than those in
G1 group (P<0.05). No significant difference was found between
G2 and G3 groups (P>0.05, Table
II).
 | Table II.Comparison of hemodynamic parameters
among three groups of experimental dogs during OLV (mean ± SD). |
Table II.
Comparison of hemodynamic parameters
among three groups of experimental dogs during OLV (mean ± SD).
| Group | T0 | T1 | T2 | T3 |
|---|
| MAP (mmHg) |
| G1 | 129±10 |
113±14 | 118±5 | 115±3 |
| G2 | 128±11 | 120±7 |
126±17 | 118±9 |
| G3 | 131±10 | 125±7 | 123±8 | 120±6 |
| HR (time/min) |
| G1 | 195±13 |
182±15 | 178±5 | 185±9 |
| G2 | 203±10 |
185±16 | 177±9 | 171±8 |
| G3 | 199±13 | 179±8 | 171±5 | 177±6 |
| MPAP (mmHg) |
| G1 | 13.0±2.2 |
20.0±3.9a |
22.3±2.2a |
21.4±2.5a |
| G2 | 13.8±1.9 |
17.8±2.0a,b |
19.7±1.9a,b |
20.5±2.2a,b |
| G3 | 12.3±1.1 |
16.0±1.5a,b |
20.2±2.1a,b |
21.5±1.8a,b |
Oxygenation
Compared with the baseline values at T0,
PaO2 and PvO2 were significantly decreased at
all subsequent time-points (P<0.05). Qs/Qt was significantly
increased (P<0.05), and changes in PaCO2 levels were
not significant (P>0.05). Compared with those in G1 group, the
PaO2 of G2 and G3 groups was significantly increased at
T1, T2 and T3, while the Qs/Qt ratio was significantly decreased
(P<0.05). There were no significant differences in
PaCO2 and PvO2 between G1 and G2 or G3 groups
at any time points (P>0.05, Table
III).
 | Table III.Comparison of oxygenation indexes
among three groups of experimental dogs during OLV (mean ± SD). |
Table III.
Comparison of oxygenation indexes
among three groups of experimental dogs during OLV (mean ± SD).
| Group | T0 | T1 | T2 | T3 |
|---|
| PaCO2
(mmHg) |
| G1 | 40.1±2.1 | 41.3±1.2 | 39.6±3.5 | 37.1±2.3 |
| G2 | 38.3±3.4 | 40.6±2.8 | 42.3±2.0 | 39.4±3.1 |
| G3 | 41.9±1.9 | 42.9±3.2 | 40.8±2.7 | 39.7±2.2 |
| PaO2
(mmHg) |
| G1 | 419.1±9.7 |
107.6±12.6a |
173.4±11.7a |
189.3±15.2a |
| G2 | 426.2±17.2 |
158.9±13.8a |
237.0±18.3a |
258.6±20.2a |
| G3 | 410.5±13.5 |
162.3±19.9a |
258.0±20.1a |
261.8±16.5a |
| PvO2
(mmHg) |
| G1 | 60.1±2.5 |
44.9±3.7a |
49.6±2.1a |
50.9±3.1a |
| G2 | 64.8±1.8 |
51.3±2.6a |
55.0±2.8a |
54.3±2.7a |
| G3 | 62.2±2.1 |
53.7±2.8a |
54.8±1.1a |
53.6±1.6a |
| Qs/Qt (%) |
| G1 | 19.2±2.2 |
47.7±1.9a |
40.2±4.0a |
38.7±3.5a |
| G2 | 20.3±3.1 |
40.1±2.3a,b |
35.1±3.1a,b |
32.1±1.6a,b |
| G3 | 18.0±1.6 |
39.2±1.5a,b |
32.9±2.3a,b |
30.4±2.8a,b |
Changes in serum TNF-α, ICAM-1 and
IL-6 levels
Compared with the baseline values at T0, all three
groups showed significantly increased TNF-α levels at T1, T2 and T3
(P<0.05). TNF-α levels in G2 and G3 groups were significantly
lower at T1, T2 and T3 than those in G1 group (P<0.05) at the
corresponding time-points. No significant difference in TNF-α level
was found between G2 and G3 groups at any time-point (P>0.05). A
similar pattern was observed regarding ICAM-1 and IL-6 levels.
Compared with the baseline values at T0, ICAM-1 and IL-6 levels
were significantly increased at T1, T2 and T3 (P<0.05). ICAM-1
and IL-6 levels in G2 and G3 groups were significantly lower at T1,
T2 and T3 than those in G1 group (P<0.05) at the corresponding
time points. No significant differences in ICAM-1 and IL-6 levels
were found between G2 and G3 groups at any time point (P>0.05,
Table IV).
 | Table IV.Comparison of the effect of lung
collapse degree on inflammatory indexes in mixed arterial and
venous blood (mean ± SD). |
Table IV.
Comparison of the effect of lung
collapse degree on inflammatory indexes in mixed arterial and
venous blood (mean ± SD).
| Inflammatory
index | Group | T0 | T1 | T2 | T3 |
|---|
| TNF-α (pg/ml) | G1 | 0.32±0.10 |
6.84±1.12a |
8.28±1.07a |
8.64±1.12a |
|
| G2 | 0.38±0.10 |
5.07±1.21a,b |
5.88±0.68a,b |
5.13±0.63a,b |
|
| G3 | 0.31±0.14 |
3.18±1.00a,b |
4.61±0.67a,b |
4.56±1.35a,b |
| ICAM-1 (ng/ml) | G1 | 7.14±1.05 |
20.45±0.96a |
30.81±1.04a |
36.33±0.60a |
|
| G2 | 7.21±1.24 |
15.74±1.44a,b |
18.57±0.46a,b |
20.00±0.65a,b |
|
| G3 | 7.51±1.20 |
9.92±0.98a,b |
13.45±0.53a,b |
14.62±0.43a,b |
| IL-6 (pg/ml) | G1 | 4.62±1.59 |
63.36±6.42a |
66.08±7.04a |
54.07±5.29a |
|
| G2 | 5.06±1.50 |
20.39±5.04a,b |
26.62±3.96a,b |
22.49±4.45a,b |
|
| G3 | 5.67±1.84 |
19.71±3.98a,b |
28.19±3.13a,b |
20.29±3.75a,b |
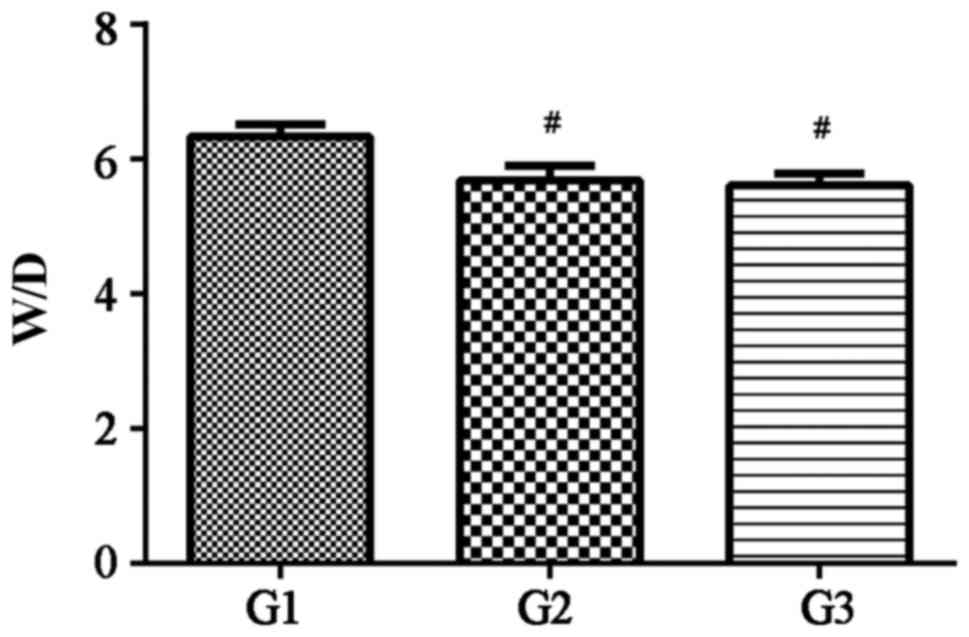
Lung W/D
W/D of lung in each group was as follows: G1 group:
6.33±0.55; G2 group: 5.69±0.67; G3 group: 5.61±0.56. W/D was
significantly decreased in G2 and G3 groups compared with that in
G1 group (P<0.05). No significant difference was found in W/D
between G2 group and G3 group (P>0.05, Fig. 1).
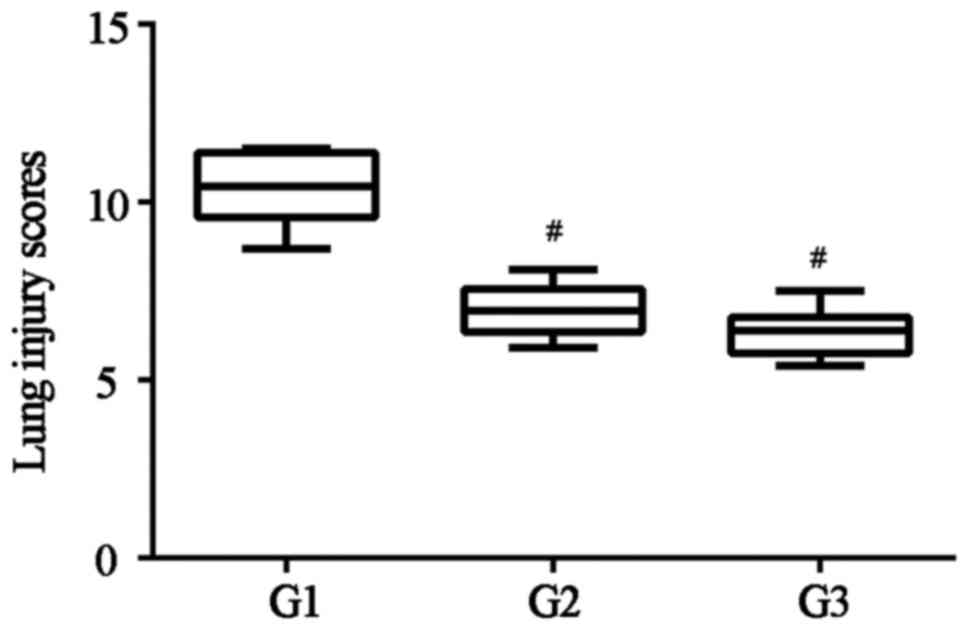
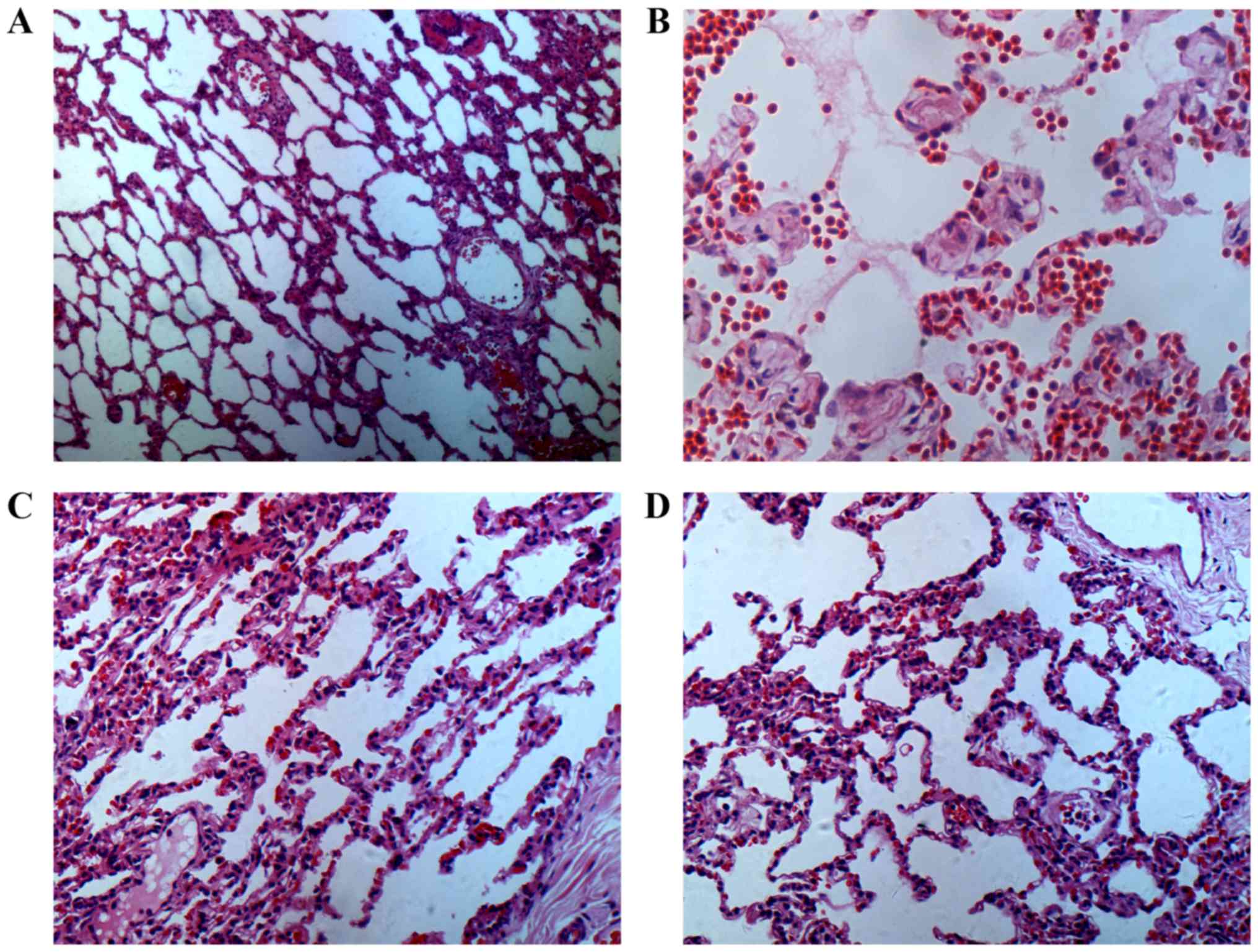
Histopathological examination of lung
tissues
The pathological examination of the collapsed side
(right lung) was as follows: The G1 group showed significant
changes in alveolar wall edema, pulmonary interstitial thickening,
vascular congestion, serious inflammatory cell infiltration and
alveolar structure damage. The alveolar structures of G2 and G3
groups were better than that in G1 group; the pulmonary
interstitial and alveolar cavity exudates and inflammatory cell
infiltration were significantly reduced compared with those in G1
group (Figs. 2 and 3).
ALI score in each group: G1 group: 10.33±0.98
points; G2 group: 6.99±0.73 points; G3 group: 6.34±0.68 points.
Compared with that in G1 group, the ALI scores of G2 and G3 groups
were significantly reduced (P<0.05). There was no significant
difference in ALI score between G2 and G3 groups (P>0.05).
Discussion
OLV is a common ventilation method used in thoracic
surgery. The lumen diameter of the traditional double-lumen tube is
large and can cause damage to the glottis, throat edema and
postoperative hoarseness. After intubation tube, the
bronchofiberscope should be disconnected; otherwise, the
displacement or dislocation may occur when the position is
adjusted. During tube application, the lung is in a collapsed
state. Although it is beneficial for surgical operation, OLV can
cause lung collapse, which in turn leads to increased intrahepatic
shunt, hypoxia and high airway pressure in the healthy lung,
causing different degrees of lung injury later (16,17). In
this study, the controlled lung collapse based on the previous
study on lung injury was proposed for the first time. The tube of
controlling the shunt in the lung used in this study was
characterized by thinner lumen, thus effectively reducing the
airway damage. The size of sealing elements in the bronchial cavity
can be controlled by controlling intake air volume combined with a
pressure gauge to monitor internal pressure, which in turn controls
the collapse degree on the surgical side of lung while ensuring the
good surgical field. The ventilation on the surgical side of lung
can improve the re-expansion pulmonary edema and secondary acute
lung injury of patients during surgery, and improve oxygenation and
hemodynamic status of patients. The lower end of tracheal catheter
is porous and open, which needs no para-ventilation under general
anesthesia. The intubation has a high success rate, no need for
bronchofiberscope and large air flow, which can improve oxygenation
and control the intraoperative ventilation of patients more
precisely. It breaks through the traditional anesthesia method of
complete lung collapse on the operated side, and reduce the damage
of intubation tube to the bronchus. In particular, it can also
improve the quality of oxygenation and prognosis of patients with
chronic bronchitis and emphysema.
In this study, we found that PaO2 was
significantly decreased while Qs/Qt was significantly increased
(18) at 30 min during early-stage
OLV due to no ventilation, the presence of blood flow in the
collapsed lung and increased pulmonary shunting. PaO2
was gradually increased while Qs/Qt was gradually decreased at 1 h
after OLV, possibly due to the hypoxic pulmonary vasoconstriction
(HPV) response that causes lateral pulmonary artery contraction on
the collapsed side and increases the pulmonary vascular resistance.
With these changes, the blood flow is transferred to the ventral
side of lung, thereby improving the imbalanced
ventilation/perfusion ratio, reducing pulmonary shunting, and
maintaining normal PaO2 (19). In this study, the retention of
partial alveolar ventilation in the experimental group
significantly improved the shunt rate. At 1 h after OLV, the
pulmonary shunting was significantly better than that in τηε
complete collapse group, and the oxygenation condition was also
significantly improved.
The overexpansion of alveoli during mechanical
ventilation and the shear stress produced by repeated opening and
closing, as well as local lung collapse can induce lung
inflammatory responses and cause inflammation cascade initiation
(20,21). Pulmonary shunting, high airway
pressure, lung ischemia-reperfusion injury and ventilation
imbalance can damage alveolar capillary endothelium and stimulate
alveolar macrophages to release a large number of proinflammatory
mediators (22). Among the
proinflammatory mediators, TNF-α has anti-infection and immune
regulation functions, and it is one of the most important mediators
of early state inflammation, as it can induce other inflammatory
mediators and initiate inflammatory cascade reactions. ICAM-1 is an
important immunoinflammatory molecule that mediates the adhesion
reaction, which plays an important role in promoting the adhesion
of inflammatory site, controlling tumor deterioration and
metastasis and regulating the immune response. The expression of
ICAM-1 is important to the degree of tissue injurυ. IL-6 is the
strongest inflammatory mediator of the proinflammatory cytokines,
which is associated with the severity and duration of tissue damage
and can reflect the severity of inflammatory responses due to
surgical stress. In this study, controlled lung collapse and
partial ventilation significantly improved lung injury degree
during operation. TNF-α, ICAM-1 and IL-6 levels were gradually
increased over time in G1 group with complete lung collapse,
indicating that OLV causes immune inflammatory response and lung
injury. However, TTNF-α, ICAM-1 and IL-6 levels in G2 and G3 groups
were significantly lower than those in G1 group, suggesting that
partial ventilation of the collapsed lung can reduce the severity
of immune inflammatory reactions and protect lung tissue to a
certain extent, improving prognosis and accelerating postoperative
recovery.
Due to the imbalance of ventilation/perfusion ratio
in OLV, hypoxemia is caused, triggering the production the release
of a large number of inflammatory mediators, increasing the
pulmonary capillary permeability (23) and increasing the lung water content
on the collapsed side, ultimately leading to acute lung injury
(ALI). The main pathological changes are extensive pulmonary
inflammation, neutrophil aggregation, pulmonary interstitial edema,
damaged pulmonary capillary endothelial cell, alveolar epithelial
cell integrity, and penetration of protein-rich fluids into
alveolar cavities. In this study, at 2 h after complete lung
collapse, the dogs in G1 group showed significant hypoxemia,
pulmonary edema and lipid peroxidation. Through pathological
observation, alveolar wall edema, pulmonary interstitial thickening
and serious inflammatory cell infiltration in alveolar cavities,
and damaged alveolar structure were found. Our experiment
successfully proved that the partial retention of collapsed lung
ventilation can significantly improve oxygenation, reduce W/D of
lung tissues and decrease plasma inflammatory factor levels without
affecting the visual field. These results suggest that the
controlled lung collapse can alleviate acute lung injury in
experimental dogs to a certain extent.
In this study, the physiological indicators and
inflammatory indicators in G2 and G3 groups were very similar, and
there were usually no statistically significant differences in
statistical analysis. The reasons may be that the current data
measured are insufficient to produce the statistically significant
differences due to the small sample size, so it is needed to
further increase the sample size. In addition, there was partial
alveolar ventilation in the two groups, but the maximum
experimental time was set to only 2 h, so there was no significant
difference yet due to the short time. Therefore, the time and
sample size should be increased for further study.
In this study, we confirmed that a new type of lung
sequestration tube can control the degree of lung collapse during
OLV in thoracotomy. The partial retention of collapsed lung
ventilation can significantly improve the intraoperative
oxygenation, thereby reducing lung injury caused by OLV during
surgery without affecting the visual field. Further studies are
still needed to explore whether this new type of tube can reduce
the burden on other organs when used to protect the lung.
Acknowledgements
Not applicable.
Funding
This study was supported by Guangdong Province
Science and Technology Planning projects: 00174990166341080,
2016B090918111, 701253476268, 2014A020212583 and Horizontal fund
project (SZLB201218) (SZMR20120918)(JSLY20130118), China patent
number ZL2015 2.0247672.2; ZL2017 3 0099023 7; ZL2017 3
0098968.7.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GL, HW and XLu analyzed and interpreted the patient
data, and GL drafted the manuscript. XM, MX, PX, MY and XuY
performed the experiment and participated in the design of the
study. YW, XiY and AZ participated in the analysis and discussion
of the data. RL and JT were responsible for the collection of the
data and the follow-up management of the patients. XLi and YZ were
responsible for the statistical analysis of the data. JX was
devoted to designing the methods and revising the manuscript
critically for important intellectual content. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Southern Medical University (Guangzhou, China).
Patient consent for publication
Not applicable.
Competing interests
Two authors of this study (JX and MX) are among the
inventors of the patent CN205073462. According to Article 24 of the
Intellectual Property Law of People's Republic of China and Article
60 of Chapter VII of the Patent Law of the People's Republic of
China, the patent holders have permitted the authors to use the
pulmonary sequestration tube device described in this patent, where
the use is limited to projects for non-profit research.
References
|
1
|
Bernasconi F and Piccioni F: One-lung
ventilation for thoracic surgery: Current perspectives. Tumori.
103:495–503. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Seo JH, Cho CW, Hong DM, Jeon Y and Bahk
JH: The effects of thermal softening of double-lumen endobronchial
tubes on postoperative sore throat, hoarseness and vocal cord
injuries: A prospective double-blind randomized trial. Br J
Anaesth. 116:282–288. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lohser J and Slinger P: Lung injury after
one-lung ventilation: a review of the pathophysiologic mechanisms
affecting the ventilated and the collapsed lung. Anesth Analg.
121:302–318. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Falzon D, Alston RP, Coley E and
Montgomery K: Lung isolation for thoracic surgery: From inception
to evidence-based. J Cardiothorac Vasc Anesth. 31:678–693. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Clayton-Smith A, Bennett K, Alston RP,
Adams G, Brown G, Hawthorne T, Hu M, Sinclair A and Tan J: A
comparison of the efficacy and adverse effects of double-lumen
endobronchial tubes and bronchial blockers in thoracic surgery: A
systematic review and meta-analysis of randomized controlled
trials. J Cardiothorac Vasc Anesth. 29:955–966. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bendixen M, Jørgensen OD, Kronborg C,
Andersen C and Licht PB: Postoperative pain and quality of life
after lobectomy via video-assisted thoracoscopic surgery or
anterolateral thoracotomy for early stage lung cancer: A randomised
controlled trial. Lancet Oncol. 17:836–844. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Guerrero WG and González-Rivas D:
Multiportal video-assisted thoracic surgery, uniportal
video-assisted thoracic surgery and minimally invasive open chest
surgery-selection criteria. J Vis Surg. 3:562017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brat K, Tothova Z, Merta Z, Taskova A,
Homolka P, Vasakova M, Skrickova J, Sramek V, Olson LJ and Cundrle
I Jr: Resting end-tidal carbon dioxide predicts respiratory
complications in patients undergoing thoracic surgical procedures.
Ann Thorac Surg. 102:1725–1730. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Magee MJ, Herbert MA, Tumey L and Prince
SL: Establishing a dedicated general thoracic surgery subspecialty
program improves lung cancer outcomes. Ann Thorac Surg.
103:1063–1069. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xiao JF, Xiang B, Xiao M, Su L and Deng M:
10 years, controlled lungs balance air-separation pulmonary
isolation catheter, CN205073462 U, ZlL2015 2 0247672.2, 5050843.
The data filed: 22-04-2015. The data issued: 02-03-2018.
|
|
11
|
Ludwig C, Morand P, Schnell J and Stoelben
E: Preserving middle lobe to improve lung function in
non-small-cell lung cancer. Asian Cardiovasc Thorac Ann.
17:153–156. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ichinose J, Kohno T and Fujimori S:
Video-assisted thoracic surgery for metachronous lung cancer. Kyobu
Geka. 63:969–972. 2010.(In Japanese). PubMed/NCBI
|
|
13
|
Cai HB, Li YX and Li Z: Short term
curative effect of video assisted thoracoscopic lobectomy for
early-stage lung cancer. Indian J Cancer. 51 Suppl 2:e37–e41.
2015.PubMed/NCBI
|
|
14
|
Xie D, Wang H, Fei K, Chen C, Zhao D, Zhou
X, Xie B, Jiang L, Chen Q, Song N, et al: Single-port
video-assisted thoracic surgery in 1063 cases: A single-institution
experience. Eur J Cardiothorac Surg. 49 Suppl 1:i31–i36. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sinclair SE, Kregenow DA, Lamm WJ, Starr
IR, Chi EY and Hlastala MP: Hypercapnic acidosis is protective in
an in vivo model of ventilator-induced lung injury. Am J Respir
Crit Care Med. 166:403–408. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Potočnik I, Novak Janković V, Šostarič M,
Jerin A, Štupnik T, Skitek M, Markovič-Božič J and Klokočovnik T:
Antiinflammatory effect of sevoflurane in open lung surgery with
one-lung ventilation. Croat Med J. 55:628–637. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chai XQ, Ma J, Xie Y-H, Wang D and Chen
KZ: Flurbiprofen axetil increases arterial oxygen partial pressure
by decreasing intrapulmonary shunt in patients undergoing one-lung
ventilation. J Anesth. 29:881–886. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Choi YS, Bae MK, Kim SH, Park JE, Kim SY
and Oh YJ: Effects of alveolar recruitment and positive
end-expiratory pressure on oxygenation during one-lung ventilation
in the supine position. Yonsei Med J. 56:1421–1427. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tojo K, Goto T and Kurahashi K: Protective
effects of continuous positive airway pressure on a nonventilated
lung during one-lung ventilation: A prospective laboratory study in
rats. Eur J Anaesthesiol. 33:776–783. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jin Y, Zhao X, Li H, Wang Z and Wang D:
Effects of sevoflurane and propofol on the inflammatory response
and pulmonary function of perioperative patients with one-lung
ventilation. Exp Ther Med. 6:781–785. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
García-de-la-Asunción J, García-del-Olmo
E, Perez-Griera J, Martí F, Galan G, Morcillo A, Wins R, Guijarro
R, Arnau A, Sarriá B, et al: Oxidative lung injury correlates with
one-lung ventilation time during pulmonary lobectomy: A study of
exhaled breath condensate and blood. Eur J Cardiothorac Surg.
48:e37–e44. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ding N, Wang F, Xiao H, Xu L and She S:
Mechanical ventilation enhances HMGB1 expression in an LPS-induced
lung injury model. PLoS One. 8:e746332013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Helenius IT, Dada LA and Sznajder JI: Role
of ubiquitination in Na,K-ATPase regulation during lung injury.
Proc Am Thorac Soc. 7:65–70. 2010. View Article : Google Scholar : PubMed/NCBI
|