Introduction
Infertility is currently a common disease in women
at childbearing age. With the acceleration of social processes, the
morbidity of infertility is increased gradually throughout the
world at present. In developed countries, 10–15% of couples suffer
from infertility (1). Common causes
of infertility include factors of male infertility, female
infertility, infertility in couples and unexplained infertility
(2–4), among which factors of female
infertility take up the most. Meanwhile, female infertility is
caused by the following definite reasons: Immune infertility, tubal
obstruction and ovulatory dysfunction (5,6). Zhong
et al (7), showed that in
vitro fertilization rates and embryo implantation rate was
significantly reduced in anti-thyroid antibody-positive patients.
At present, the number of infertile women in China is increased
year by year, which requires us to find more effective influence
indicators to judge and find out the causes of infertility in a
better way.
Materials and methods
General data
Objects of study: A total of 529 infertile females
that received treatments in The Affiliated Wuxi Maternity and Child
Health Care Hospital of Nanjing Medical University from January
2014 to January 2017 and complied with inclusion criteria were
selected for retrospective study. They were divided into positive
group (121 patients) and negative group (408 patients). The
patients were 22–43 years with an average age of 30.5±5.9. General
data of the patients, including age, height, body weight, initial
menstruation, duration of infertility, menstrual cycle, permanent
residence (city/village) and education background (university
degree or above/under university degree) are given in Table I. The present study was conducted in
accordance with the Declaration of Helsinki and was approved by the
Ethics Committee of The Affiliated Wuxi Maternity and Child Health
Care Hospital of Nanjing Medical University (Wuxi, China). All the
participants or their family members signed written informed
consent.
 | Table I.General data of 529 infertile female
patients. |
Table I.
General data of 529 infertile female
patients.
| Variables | Positive group
(n=121) | Negative group
(n=408) | P-value |
|---|
| Age (years) | 29.75±5.21 | 30.83±6.23 | 0.626 |
| Height (m) | 1.59±0.07 | 1.60±0.08 | 0.875 |
| Weight (kg) | 57.20±10.70 | 54.96±9.61 | 0.332 |
| Initial menstruation
(years) | 13.80±2.80 | 14.16±3.12 | 0.672 |
| Duration of
infertility (years) | 3.70±2.81 | 4.21±3.10 | 0.552 |
| Menstrual cycle
(days) | 27.95±13.21 | 28.21±14.43 | 0.745 |
| Permanent residence
(city/village) | 79/42 | 272/136 | 0.778 |
| Education background
(above/under)a, n | 69/52 | 229/179 | 0.861 |
Inclusion criteria: i) Married women at childbearing
age (20–49 years old); ii) patients complying with World Health
Organization (WHO) diagnostic criteria for female infertility:
females with sexual life; females without pregnancy or abortion;
females without pregnancy while no contraceptive measure was taken
within 1 year; iii) patients with normal thyroid function and
thyroid autoantibodies [thyroglobulin antibody (TG-Ab), thyroid
peroxidase antibody (TPO-Ab) and thyroid microsome antibody
(TM-Ab)]; iv) patients with positive TPO-Ab (a thyroid
autoantibody) and normal TG-Ab and TM-Ab. Patients meeting item i,
ii and iii were grouped into negative control group (negative group
for short), and those meeting item i, ii and iv into positive
simple TPO-Ab group (positive group for short).
Exclusion criteria: i) patients with a history of
diabetes, coronary heart disease, hyperlipidemia, hypertension,
diseases caused by hypothalamic or pituitary dysfunction, malignant
tumors, substantial lesions of organs such as liver and kidney,
etc.; and ii) patients with a history of thyroid diseases (whether
or not cured), patients with recent oral administration of drugs
that can affect thyroid function and blood lipid levels, patients
with a history of thyroid antibody positive.
Laboratory examinations
Venous blood was collected from all the included
infertile females on an empty stomach in the morning from the 2nd
day to the 4th day after menstruation to measure basal hormone
levels. The levels of human follicle stimulating hormone (hFSH),
estradiol (ESTRDL), progesterone (Prog), prolactin (PRL),
testosterone (TESTO) and human luteinizing hormone (hLH) in the
serum were measured by chemiluminescence method (Beijing Craymei
Biotech Co., Ltd., Beijing, China). All the items of blood drawing
were conducted by professional nurses, and relevant tests and
results were completed and judged, respectively by two specific
laboratory physicians.
Confirmation on causes of
infertility
The causes of female infertility were determined and
studied by inquiry of medical history, general gynecological
examination, detection of basal hormone levels, B-scan
ultrasonography, tubal and uterine lipiodol angiography (8), laparoscopy, hysteroscopy, surgical
pathologic examination and other ways. In addition, polycystic
ovarian syndrome (PCOS) was diagnosed as per industry standard of
the Ministry of Health (2011).
Comparisons of relative indicators
among groups
The correlation of positive simple TPO-Ab with the
diseases of infertility such as endometriosis (EMT), PCOS, tubal
obstruction and premature ovarian failure (POF) was compared. All
the patients were divided into three age groups (22–28, 28–35 and
35–42 years old) to analyze and compare the correlation of
infertility with positive simple TOP-Ab.
Statistical analysis
All the data were processed using SPSS v.20.0
software (IBM Corp., Armonk, NY, USA). The measurement data were
expressed as the mean ± standard deviation. Data between the two
groups was compared by t-test. Enumeration data was expressed as
percentages, and the Chi-square test was performed for data
analysis. P<0.05 was considered to indicate a statistically
significant difference.
Results
Comparisons of BMI and basal hormone
levels in the serum between the two groups
A total of 529 infertile females were included in
this study. The differences in body mass index (BMI) and basal
hormone levels (hFSH, ESTRD, Prog, PRL, TESTO and hLH) had no
statistical significance (P>0.05; Table II).
 | Table II.Comparisons of BMI and basal hormone
levels in the serum between the two groups. |
Table II.
Comparisons of BMI and basal hormone
levels in the serum between the two groups.
| Variables | Positive group | Negative group | P-value |
|---|
| Age (years) | 29.75±5.21 | 30.83±6.23 | 0.626 |
| BMI (kg/m2) | 24.68±3.67 | 24.21±3.82 | 0.782 |
| hFSH (mIU/ml) | 7.56±2.20 | 7.23±1.96 | 0.725 |
| ESTRDL (pg/ml) | 36.20±21.43 | 37.76±28.51 | 0.631 |
| Prog (ng/ml) | 0.79±0.63 | 0.82±0.58 | 0.599 |
| PRL (ng/ml) | 14.92±8.24 | 14.88±9.01 | 0.838 |
| TESTO (ng/dl) | 44.53±19.25 | 47.79±21.98 | 0.721 |
| hLH (mIU/ml) | 3.29±1.96 | 3.38±2.11 | 0.824 |
Comparison of incidence rates of
diseases of infertility between the two groups
The comparison of menstruation between the two
groups of patients showed no statistical significance (P>0.05).
The incidence rates of tubal obstruction and POF in the positive
group were lower than those in the negative group, but the
differences between the two groups were not significant
(P>0.05). However, the differences in the incidence rates of EMT
and PCOS between the two groups of females were significant
(P<0.05), and the incidence rate of PCOS was relatively
significant in females with positive simple TPO-Ab (P<0.001;
Table III).
 | Table III.Comparison of incidence rates of
diseases of infertility among 529 infertile females. |
Table III.
Comparison of incidence rates of
diseases of infertility among 529 infertile females.
|
| Positive group
(n=121) | Negative group
(n=408) |
|
|
|---|
|
|
|
|
|
|
|---|
| Disease | n | % | n | % | χ2 | P-value |
|---|
| Irregular
menstruation | 25 | 20.7 | 65 | 15.9 | 1.479 | 0.224 |
| Tubal
obstruction | 19 | 15.7 | 89 | 21.8 | 2.145 | 0.143 |
| EMT | 34 | 28.1 | 76 | 18.6 | 5.083 | 0.024 |
| POF | 12 | 9.9 | 43 | 10.5 | 0.039 | 0.844 |
| PCOS | 45 | 37.1 | 79 | 19.4 | 16.527 | <0.001 |
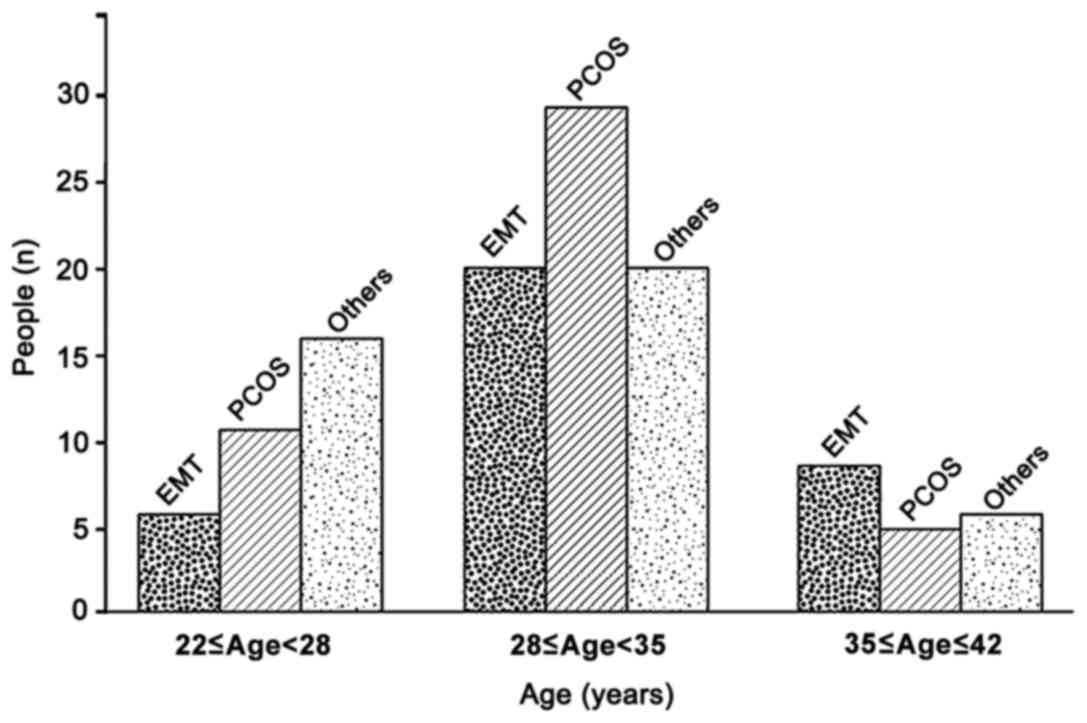
Comparisons of the number of patients
with EMT, PCOS among different age groups
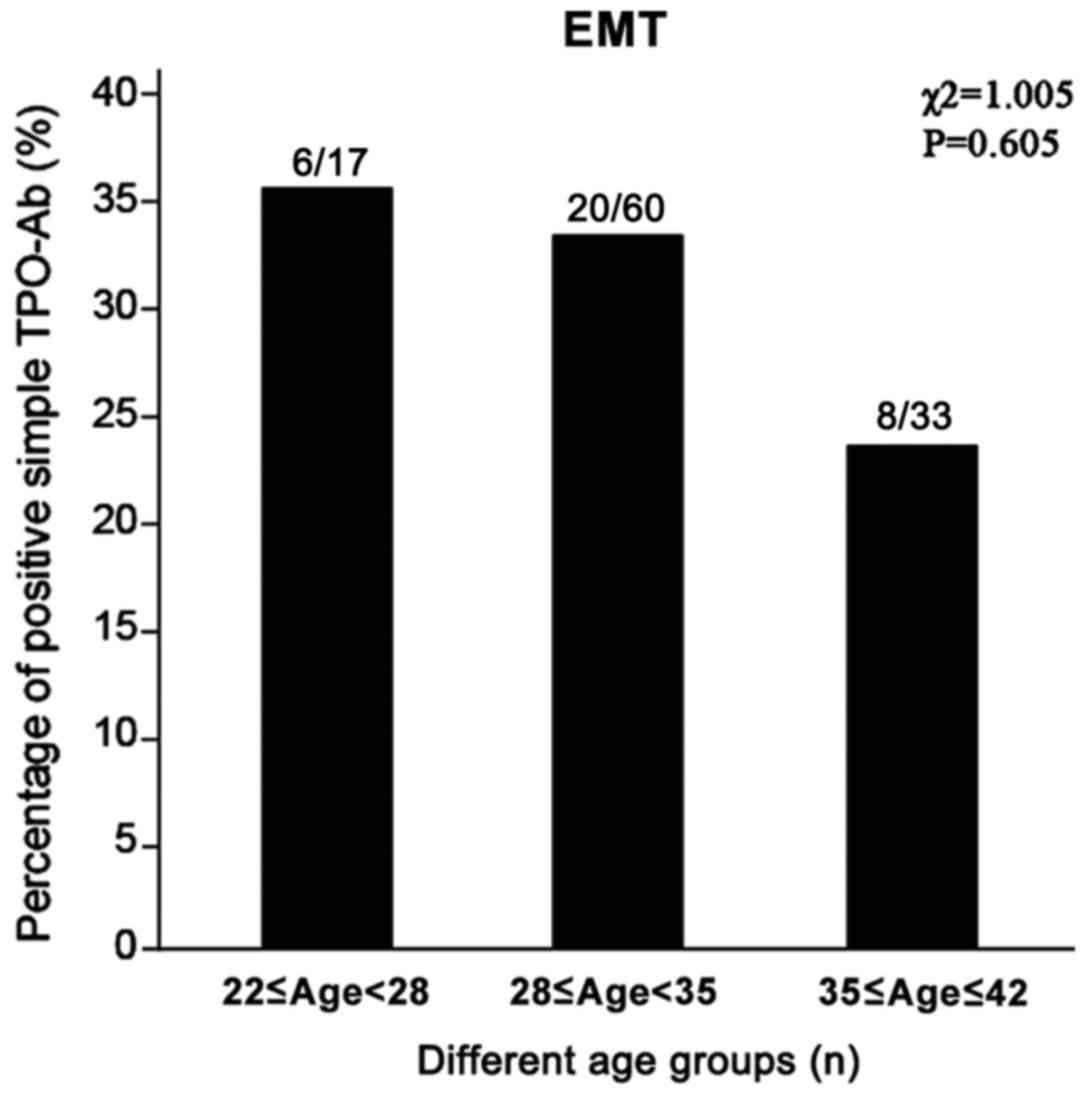
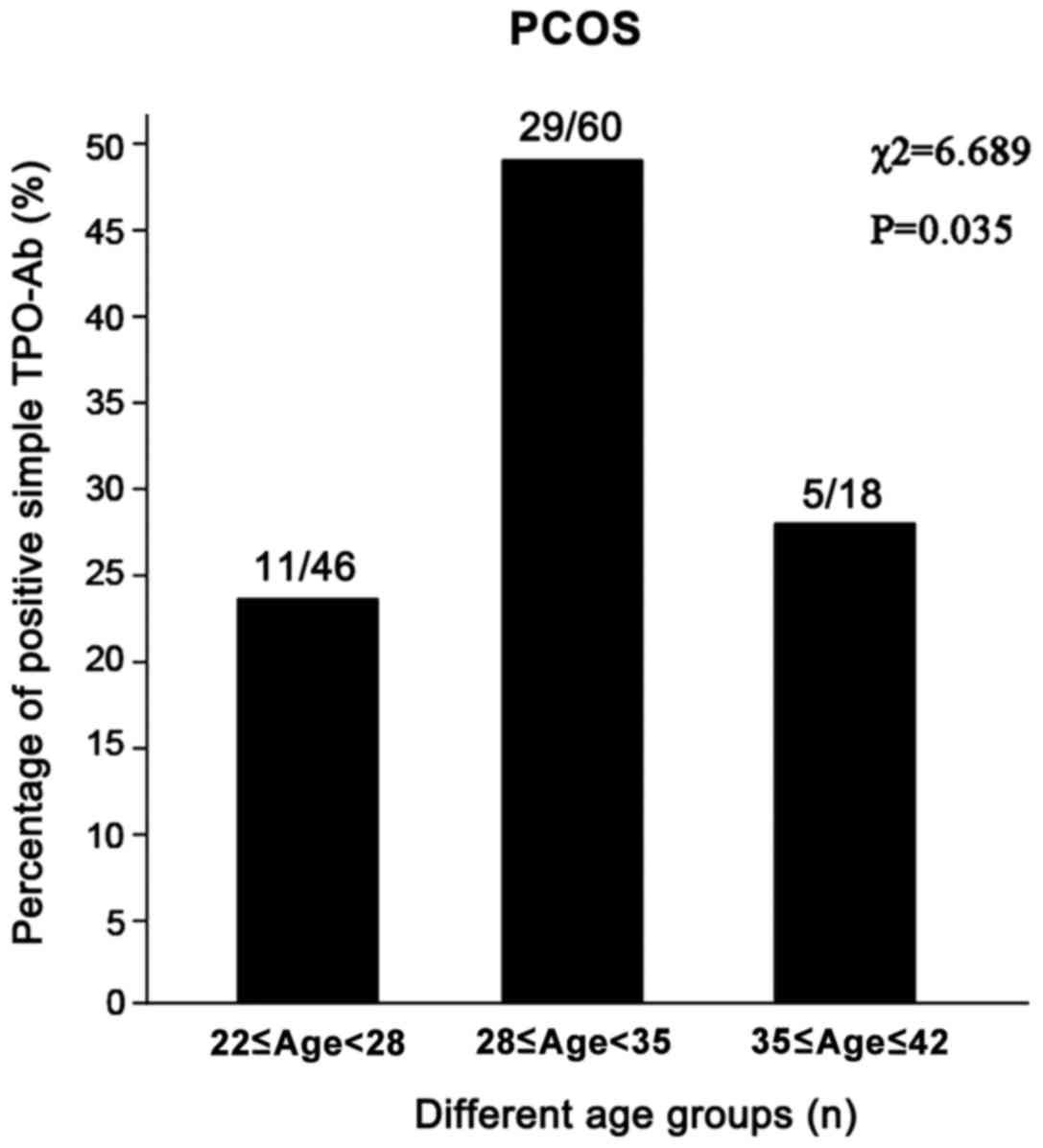
In the present study, the numbers of patients with
EMT and PCOS were compared among different age groups. The results
showed that patients aged 28–35 years old took up the most in terms
of EMT and PCOS (Fig. 1), among
which the comparison of the percentage of positive simple TOP-Ab
among the three age groups with EMT had no statistical difference
(χ2=1.005; P=0.605; Fig.
2), while patients with PCOS aged 28–35 years showed relatively
high percentage of positive simple TPO-Ab (χ2=6.689;
P=0.035; Fig. 3).
Discussion
TPO is a thyroid-specific antigen, which destroys
thyroid tissue mainly through infiltrating lymphocytes, thus
resulting in autoimmune thyroid disease (AITD) (9). Currently, the correlation between AITD
and recurrent miscarriage and pregnancy loss is confirmed in many
studies (10–12), while the interference of thyroid
autoantibodies in the normal fertility of women of childbearing age
is still an outstanding problem (13–15). At
present, there are relatively few studies on the influence of
positive TPO-Ab on infertility. Therefore, a total of 529 infertile
females were selected for experimental study so as to confirm the
potential influence of positive TPO-Ab on infertility.
The results of the present study showed that basal
hormone levels and BMI had no significant differences in females
with positive simple TPO-Ab and normal thyroid function
(P>0.05), while the percentages were relatively high in
infertile females with positive simple TPO-Ab, and the expressions
in EMT and PCOS were significant (P<0.05). A study of Chen et
al (15) showed that the
incidence rate of positive TPO-Ab is high in infertile females,
which is significantly related to idiopathic poor ovarian reserve
function (P=0.020), leading to more unexplained infertility. A
study of Medenica et al (16)
showed that positive TPO-Ab is significantly correlated with EMT
(P=0.001). A study conducted by Drobniak et al (17) showed that increased TPO-Ab is
observed in 12–25% of females with autoimmune thyroid diseases,
while the positive rate of TPO-Ab in females with PCOS and EMT is
increased significantly, and TPO-Ab with a high titer is observed
more frequently. A study of Sinha et al (18) showed that the positive rate of
anti-TPO-Ab in patients with PCOS is increased (P<0.05), which
is more significant in infertile patients with positive TPO-Ab than
that in the control group (22.5% vs. 1.25%, P<0.01). Another
study of Weghofer et al (19)
also showed that the incidence rate of anti-TPO-Ab in patients with
PCOS is significantly higher than that in the control group (normal
females) (P<0.01). The aforementioned test results are basically
identical with those of this study, which suggests that positive
simple TPO-Ab may be correlated with female infertility caused by
EMT and PCOS, while the mechanism of infertility of patients with
EMT and PCOS caused by increased TPO-Ab still needs to be explored
further.
There was no statistically significant difference in
the incidence rate of EMT among the three age groups at different
ages (P=0.605), while the positive rate of TPO-Ab in infertile
females with PCOS aged 28–35 years old was increased significantly
(P=0.035), which suggests that positive simple TPO-Ab may have a
greater impact on infertile females aged 28–35 years (20,21).
This experimental study still has some shortcomings.
The conditions of infertile females with positive TPO-Ab after
treatment can be further analyzed to provide more support for this
experimental study. As the experimental samples have regional
limitations, a multi-center study on a large sample size can prove
the significance of the experiment in a more powerful way.
In conclusion, positive simple TPO-Ab may be
correlated with EMT and PCOS. Patients with EMT and PCOS
(especially females with PCOS aged 28–35 years old) should undergo
screening of thyroid autoantibodies actively to provide better
interventions.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XW and XD conceived and designed the study. XX
collected the patient data. FX and RF were responsible for the
analysis and interpretation of the data. XW drafted this
manuscript. XD revised the manuscript critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of The Affiliated Wuxi Maternity and Child Health Care
Hospital of Nanjing Medical University (Wuxi, China). Signed
written informed consent was obtained from the patients and/or
their guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Carp HJ, Selmi C and Shoenfeld Y: The
autoimmune bases of infertility and pregnancy loss. J Autoimmun.
38:J266–J274. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Deroux A, Dumestre-Perard C, Dunand-Faure
C, Bouillet L and Hoffmann P: Female infertility and serum
auto-antibodies: A systematic review. Clin Rev Allergy Immunol.
53:78–86. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mobeen H, Afzal N and Kashif M: Polycystic
ovary syndrome may be an autoimmune disorder. Scientifica (Cairo).
2016:40717352016.doi: 10.1155/2016/4071735. PubMed/NCBI
|
|
4
|
Feldthusen AD, Pedersen PL, Larsen J,
Kristensen Toft T, Ellervik C and Kvetny J: Impaired fertility
associated with subclinical hypothyroidism and thyroid
autoimmunity: The Danish General Suburban Population Study. J
Pregnancy. 2015:1327182015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Busnelli A, Paffoni A, Fedele L and
Somigliana E: The impact of thyroid autoimmunity on IVF/ICSI
outcome: A systematic review and meta-analysis. Hum Reprod Update.
22:793–794. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Al-Saab R and Haddad S: Detection of
thyroid autoimmunity markers in euthyroid women with polycystic
ovary syndrome: A case-control study from syria. Int J Endocrinol
Metab. 12:e179542014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhong YP, Ying Y, Wu HT, Zhou CQ, Xu YW,
Wang Q and Li J, Shen XT and Li J: Relationship between antithyroid
antibody and pregnancy outcome following in vitro fertilization and
embryo transfer. Int J Med Sci. 9:121–125. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schankath AC, Fasching N, Urech-Ruh C,
Hohl MK and Kubik-Huch RA: Hysterosalpingography in the workup of
female infertility: Indications, technique and diagnostic findings.
Insights Imaging. 3:475–483. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Unuane D, Velkeniers B, Anckaert E,
Schiettecatte J, Tournaye H, Haentjens P and Poppe K: Thyroglobulin
autoantibodies: Is there any added value in the detection of
thyroid autoimmunity in women consulting for fertility treatment?
Thyroid. 23:1022–1028. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yoshioka W, Amino N, Ide A, Kang S, Kudo
T, Nishihara E, Ito M, Nakamura H and Miyauchi A: Thyroxine
treatment may be useful for subclinical hypothyroidism in patients
with female infertility. Endocr J. 62:87–92. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Speer G: The impact of thyroid function in
women of reproductive age: Infertility, pregnancy and the
postpartum period. Orv Hetil. 154:2017–2023. 2013.(In Hungarian).
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Boufas D, Vryonidou A, Mastorakos G and
Ilias I: Thyroid function and autoimmunity versus number of
pregnancies. J Reprod Infertil. 17:240–242. 2016.PubMed/NCBI
|
|
13
|
Plowden TC, Schisterman EF, Sjaarda LA,
Zarek SM, Perkins NJ, Silver R, Galai N, DeCherney AH and Mumford
SL: Subclinical hypothyroidism and thyroid autoimmunity are not
associated with fecundity, pregnancy loss, or live birth. J Clin
Endocrinol Metab. 101:2358–2365. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Duran B, Ozlü T, Koç O, Eşitken C and
Topçuoğlu A: Relationship of thyroid hormone levels and thyroid
autoantibodies with early pregnancy loss and infertility. J Obstet
Gynaecol. 33:862–864. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen CW, Huang YL, Huang RL, Tzeng CR and
Chen CH: Idiopathic low ovarian reserve is associated with more
frequent positive thyroid peroxidase antibodies. Thyroid.
27:1194–1200. 2017.PubMed/NCBI
|
|
16
|
Medenica S, Nedeljkovic O, Radojevic N,
Stojkovic M, Trbojevic B and Pajovic B: Thyroid dysfunction and
thyroid autoimmunity in euthyroid women in achieving fertility. Eur
Rev Med Pharmacol Sci. 19:977–987. 2015.PubMed/NCBI
|
|
17
|
Drobniak A, Kanecki K, Grymowicz M and
Radowicki S: Serum leptin concentration in women of reproductive
age with euthyroid autoimmune thyroiditis. Gynecol Endocrinol.
32:128–131. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sinha U, Sinharay K, Saha S, Longkumer TA,
Baul SN and Pal SK: Thyroid disorders in polycystic ovarian
syndrome subjects: A tertiary hospital based cross-sectional study
from Eastern India. Indian J Endocrinol Metab. 17:304–309. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weghofer A, Himaya E, Kushnir VA, Barad DH
and Gleicher N: The impact of thyroid function and thyroid
autoimmunity on embryo quality in women with low functional ovarian
reserve: A case-control study. Reprod Biol Endocrinol. 13:432015.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Andreeva P: Thyroid gland and fertility.
Akush Ginekol (Sofiia). 53:18–23. 2014.(In Bulgarian). PubMed/NCBI
|
|
21
|
Fumarola A, Grani G, Romanzi D, Del Sordo
M, Bianchini M, Aragona A, Tranquilli D and Aragona C: Thyroid
function in infertile patients undergoing assisted reproduction. Am
J Reprod Immunol. 70:336–341. 2013. View Article : Google Scholar : PubMed/NCBI
|