Introduction
Uncontrolled hemorrhagic shock (UHS) is a kind of
clinically common disease, which is the ‘lethal triad’ with low
body temperature, acidosis and coagulation dysfunction as typical
pathophysiological changes. Further, its treatment is based
primarily on the principle of fluid resuscitation that includes
restoration of the blood perfusion and oxygen supply to end organs
(1). The early fluid resuscitation
program was based on the Wiggers controlled hemorrhagic shock model
(2). Earlier, the above method was
utilized widely but a number of clinical observations revealing
iatrogenic secondary strikes greatly affected its success rate
(3). On the other hand, controlled
fluid resuscitation emphasizes the maintenance of blood volume in
basal metabolic cycle, instead of rapid stability of vital signs.
In this way, it gave full play to the body's own compensatory
mechanism and reduced the complications of fluid resuscitation
(4). Furthermore, a study in the
recent past has confirmed that stress as well as inflammatory
response disorders played an important role in the development of
UHS and during fluid resuscitation (5). A variety of inflammatory indexes, such
as C-reactive protein (CRP), interleukin-6 (IL-6), tumor necrosis
factor-α (TNF-α) and procalcitonin (PCT), have important
application values in reflecting the severity of UHS as well as the
effect of fluid resuscitation (6,7).
Moreover, recent studies have exhibited that human neutrophil
lipocalin (HNL), is a kind of novel secreted protein in neutrophil
secondary granules (8,9). Furthermore, it was closely associated
with inflammatory response, activation of signal transduction
pathway, immune response and development of tumors. So, HNL has a
better application value in diagnosing the early renal injury.
Also, it helps to distinguish between acute, bacterial and viral
infections (10,11). Therefore, the present study aimed
primarily to evaluate the association between the effect of
controlled fluid resuscitation on massive hemorrhage as well as the
HNL expression, which would contribute to the improvement of the
assessment and treatment of UHS.
Materials and methods
Study design
A total of 112 patients diagnosed with UHS in
People's Hospital of Baise from March 2015 to March 2017 were
continuously selected as study subjects. Inclusion criteria were:
i) patients with the trauma index <12 according to AIS90-ISS
standard, injury severity score (ISS) >16 and survival time
>72 h, accompanied with different degrees of shock (12); ii) patients who received effective
treatment of traumatic disease; iii) patients who could undergo
fluid resuscitation according to different groups, with complete
clinical data and informed consent. Exclusion criteria were: i)
patients complicated with serious underlying diseases, such as
dysfunction in heart, liver, lung, kidney, brain or other organs,
or coagulation dysfunction; ii) patients with uncontrolled
infection or pain. The patients were divided into the control group
(n=56) and observation group (n=56) using the random number method.
The baseline data of the groups were comparable (P>0.05)
(Table I). The Ethics Committee of
People's Hospital of Baise (Baise, China) duly approved the present
study as well as all experimental methods. The consent forms were
obtained from all the patients or their guardians before the
treatment.
 | Table I.Comparison of baseline data between
the two groups. |
Table I.
Comparison of baseline data between
the two groups.
| Items | Control group
(n=56) | Observation group
(n=56) | t/χ2 | P-value |
|---|
| Male/female | 33/23 | 35/21 | 0.150 | 0.699 |
| Age (years) | 48.9±6.7 | 47.6±6.5 | 0.253 | 0.648 |
| Onset time (h) | 3.5±0.6 | 3.7±0.9 | 0.185 | 0.767 |
| Trauma index | 8.9±1.7 | 8.6±1.5 | 0.089 | 0.865 |
| ISS | 19.5±2.4 | 21.2±2.5 | 0.326 | 0.587 |
| Shock degree (n,
%) |
|
| 0.766 | 0.682 |
| Mild | 18 (32.1) | 15 (26.8) |
|
|
|
Moderate | 23 (41.1) | 22 (39.3) |
|
|
|
Severe | 15 (26.8) | 19 (33.9) |
|
|
| Trauma site (n,
%) |
|
| 0.301 | 0.960 |
|
Chest | 22 (39.3) | 22 (39.3) |
|
|
|
Abdomen | 18 (32.1) | 17 (30.4) |
|
|
| Pelvic
cavity and head | 6 (10.7) | 5 (8.9) |
|
|
| Combined
trauma | 10 (17.9) | 12 (21.4) |
|
|
Research methods
The patients received immediate treatment in the
Emergency Department or selective operation, followed by
resuscitation and monitoring in ICU. They underwent general
physical examination in accordance with ‘CRASHPLAN’ and ‘VIPC’
rescue process. At least two venous channels were established using
the balanced crystalloid solution (lactated Ringer's solution or
Ringer's sodium bicarbonate solution) supplemented by colloidal
fluid (low molecular dextran and 706 dextran) at the right time
with the crystal/colloid ratio of 2–3:1. According to the blood
pressure recovery, the infusion rate, dose and vasoactive drugs
used were determined. The control group was treated with rapid
fluid resuscitation to maintain the mean arterial pressure (MAP)
above 60 mmHg. The observation group was treated with controlled
fluid resuscitation according to MAP or central venous pressure
(CVP), and the MAP was maintained at approximately 50 mmHg before
hemostasis. After full hemostasis, MAP in both groups was
maintained at 80–85 mmHg and the hematocrit was maintained above
30%. Moreover, the arterial oxygen saturation, blood routine,
hepatic, renal and coagulation function as well as arterial blood
gas, were monitored.
Observational indexes
The success rate of resuscitation, incidence rate of
complications, and HNL levels at 3, 10, 24 and 72 h both before and
after resuscitation were compared between the groups. Successful
resuscitation was defined as follows: the bleeding as well as shock
was controlled and consciousness was recovered. Moreover, blood
pressure, heart rate, urine volume and CVP were returned to normal
and were maintained for at least 24 h without obvious
complications. The serum HNL level was detected via enzyme-linked
immunosorbent assay (ELISA). The reagents were purchased from
Jiangsu Beyotime Technology Co., Ltd. (Jiangsu, China). The level
was measured three times strictly according to the instructions of
kit and the average was recorded.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
20.0 software (IBM Corp., Armonk, NY, USA) was utilized for the
statistical analysis. Measurement data are presented as mean ±
standard deviation. The independent-samples t-test was used for
comparison between the two groups, and the repeated measures
analysis of variance and post hoc Tukeys test were performed and
used for comparisons of data at different time-points. Enumeration
data were presented as case or %, and Chi-square test was used for
the intergroup comparison. P<0.05 was considered to indicate a
statistically significant difference.
Results
Basic characteristics
The baseline data of the two groups are shown in
Table I. There were no significant
differences of gender ratio, age, onset time, trauma index, ISS,
shock degree and trauma site between control group and observation
group (P>0.05).
Comparison of success rate of
resuscitation and incidence rate of complications
In the observation group, the success rates of
resuscitation showed significant increase, while the incidence rate
of complications showed significant decrease (P<0.05) (Table II).
 | Table II.Comparison of success rate of
resuscitation and incidence rate of complications between the two
groups (n, %). |
Table II.
Comparison of success rate of
resuscitation and incidence rate of complications between the two
groups (n, %).
| Groups | n | Success rate | Dilutional
coagulation disorders | Detachment of
thrombus | Rebleeding | Pulmonary edema or
respiratory distress syndrome | Complications |
|---|
| Control group | 56 | 44 (78.6) | 3 (5.4) | 2 (3.6) | 4 (7.1) | 3 (5.4) | 12 (21.4) |
| Observation
group | 56 | 52 (92.9) | 0 | 1 (1.8) | 2 (3.6) | 1 (1.8) | 4 (7.1) |
| χ2 |
| 4.667 |
|
|
|
| 4.667 |
| P-value |
| 0.031 |
|
|
|
| 0.031 |
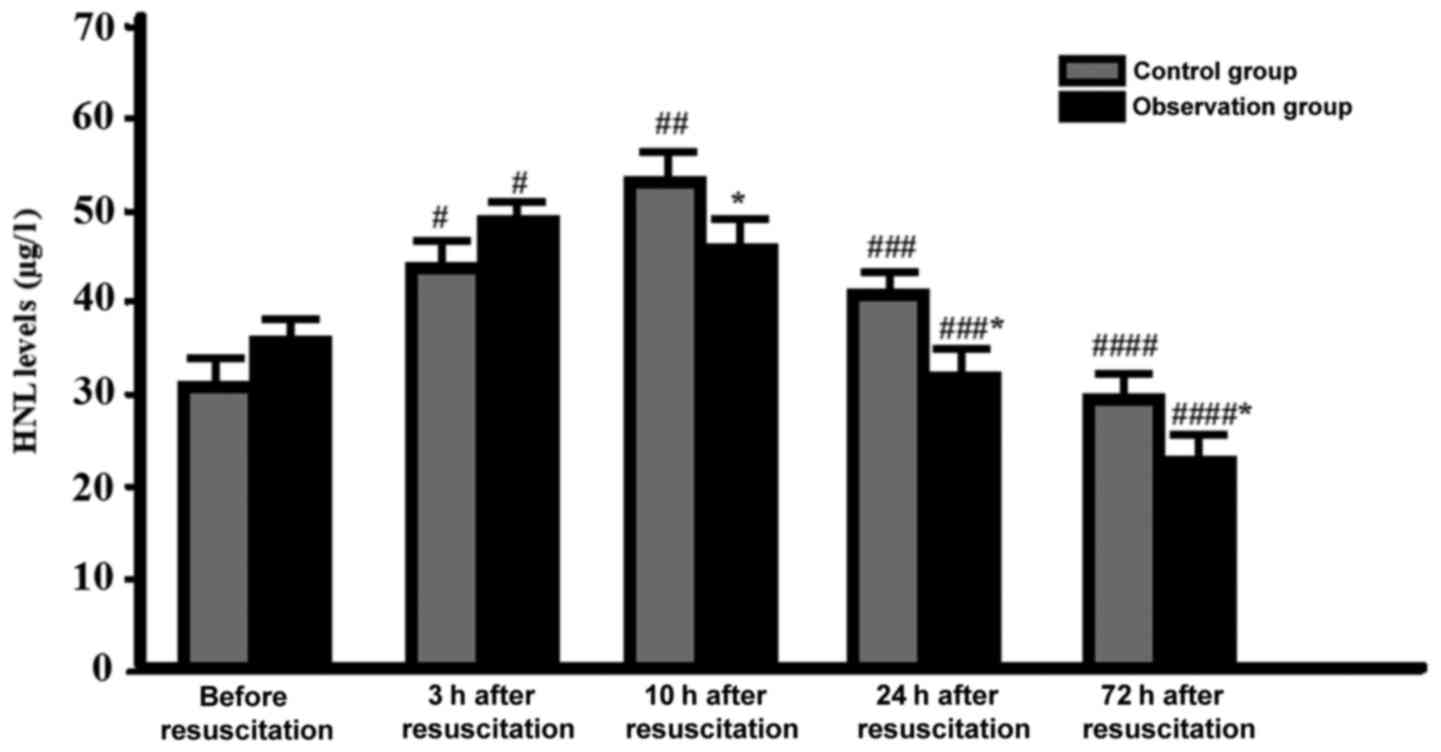
Comparison of serum HNL levels at
different time-points
The HNL levels in both groups were increased
significantly reaching the peak at 3–10 h after resuscitation, and
then were decreased. The HNL levels of the observation group at 10
h was similar to that at 3 h (P>0.05). However, the HNL levels
of the control group at 10 h was significantly higher than that at
3 h (P<0.05). Moreover, the HNL levels were significantly
decreased in both the control and observation groups at 24 h
compared with that at 10 h (P<0.05), which suggested that the
time of peak reduction in the observation group appeared earlier
(Fig. 1). Furthermore, the HNL
levels of the observation group was significantly lower than that
of the control group at 10, 24 and 72 h (P<0.05) (Fig. 1).
Discussion
Wiggers controlled hemorrhagic shock model advocates
that fluid resuscitation should be early and sufficient, while the
fluid volume should be 2–3 times that of blood loss volume. At the
same time, the positive inotropic drugs and vasoactive drugs should
be used to raise the blood pressure, immediately. Furthermore,
recovery and restoration of the effective blood volume should be
performed as soon as possible. This ensures effective perfusion of
organs as well as tissues. Also, the traumatic hemorrhagic shock is
closely related to the mortality rate of patients and incidence
rate of complications (13).
However, before the active bleeding could be effectively
controlled, a large amount of fluid resuscitation would result in
the rise of blood loss leading to the dilution of coagulation
dysfunction (14). Also, a recent
report observed significant damage to the mitochondrial function
along with the reduction in the oxygen supply to tissues causing
acidosis (15). At the same time, a
large amount of rapid infusion has been reported to cause decrease
in the vasoconstriction, leading to thrombus translocation,
increased complications and high mortality rates (16). The concept of controlled fluid
resuscitation is to reduce the harmful effects of early massive
fluid resuscitation, effectively so as to improve the perfusion as
well as oxygen supply to organ tissues in shock phase. This in turn
reduced the occurrence of traumatic coagulopathy without causing
over-diluted blood. It also effectively prevented the detachment of
thrombus as well as bleeding within the allowable low blood
pressure range. Furthermore, it caused reduction in apoptosis while
maintaining the compensatory mechanism thereby, improving the
survival rate (17). In addition,
the type and dosage of resuscitation fluid and monitoring of the
resuscitation effects are also important contents of recovery
management. In addition to the traditional blood pressure, heart
rate, urine volume and CVP (as the parameters of full perfusion and
resuscitation outcomes), the non-invasive cardiac output, cardiac
ultrasound, pulse indicator continuous cardiac output monitoring,
blood lactate, base deficit, intestinal mucosal pH, central venous
oxygen saturation, orthogonal polarization spectral imaging and
bypass dark-field imaging technique, have a certain application
value in accurate assessment of the resuscitation time and mode
(18,19). At the same time, selection of
biochemical markers with higher sensitivity as well as specificity
to assess the resuscitation effect is also an important task of
UHS.
HNL, also known as neutrophil gelatinase associated
lipocalin, belongs to the lipocalin superfamily that exists mainly
in the form of monomer (25 kD), homodimer (45 kD) and
heteromultimer covalently bound to neutrophil gelatinase. HNL is a
kind of iron carrier protein, whose main ligand is a small
iron-binding molecule. When the neutrophils are activated or
epithelial cells are damaged under inflammatory stimulation, HNL is
often expressed on a large scale (20). The present study showed that the
serum HNL was at a high level before UHS resuscitation, indicating
that HNL was expressed in the early stage of UHS and was involved
in the occurrence as well as development of the disease. HNL, as an
important molecular marker in the early inflammatory response of
the body, is the product secreted by neutrophil activation. It is
the chemotactic factor of a variety of inflammatory cells and the
inducible factor of a variety of inflammatory mediators that are
core molecule in the inflammatory cascade reaction (21). The serum HNL levels in both groups
were further increased after resuscitation at 3 h, and it reached
the peak in the observation group. However, it was not
significantly different when compared with the control group. This
confirmed that the fluid resuscitation may further activate the
inflammatory response in the body and is possibly the result of
further development of UHS. In the control group, the serum HNL
level was increased to the peak at 10 h after resuscitation,
indicating that the early rapid fluid resuscitation may also be
responsible for observed increase of the degree of inflammatory
response in the body. The above observation could be due to the
massive rapid fluid resuscitation, leading to an inflammatory
response in the body. The serum HNL levels in both groups began to
decrease gradually at 24 h after resuscitation, and the level in
the observation group was significantly lower than that in the
control group. This suggested that HNL has a certain application
value in the early evaluation of inflammatory response degree and
has confirmed effects of fluid resuscitation on UHS.
There were also some limitations in this study. The
sample size is relatively small and the follow-up time is
relatively short. The signal pathway was not investigated in this
study. Further study with a lager sample size and longer follow-up
time or focused on the mechanism is still needed.
In conclusion, hemorrhagic shock produces
hemodynamic changes that often result in a systemic inflammatory
response that can lead to multiple organ failure and death. Early
recognition of hemorrhagic shock is paramount in civilian and
military communities to effectively implement damage-control
resuscitation strategies to prevent progression into a state of
irreversible shock and permit appropriate allocation of resources.
The present study concludes that the controlled fluid resuscitation
on massive hemorrhage is superior to that of rapid fluid
resuscitation. Also, controlled fluid resuscitation could decrease
the HNL levels and inflammatory response. Our results may promote
the improvement of the assessment and treatment of UHS.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JYY wrote the paper, analyzed the data, conceived
and designed the experiments. JYY, JHP and LH performed the
experiments. HQH, MHT and GJ contributed
reagents/materials/analysis tools. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The Ethics Committee of People's Hospital of Baise
(Baise, China) approved the present study. The consent forms were
obtained from all the patients or their guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhao G, Wu W, Feng QM and Sun J:
Evaluation of the clinical effect of small-volume resuscitation on
uncontrolled hemorrhagic shock in emergency. Ther Clin Risk Manag.
13:387–392. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li T, Zhu Y, Tian K, Xue M, Peng X, Lan D
and Liu L: Ideal resuscitation pressure for uncontrolled
hemorrhagic shock in different ages and sexes of rats. Crit Care.
17:R1942013. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ertmer C, Kampmeier T, Rehberg S and Lange
M: Fluid resuscitation in multiple trauma patients. Curr Opin
Anaesthesiol. 24:202–208. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Duan C, Li T and Liu L: Efficacy of
limited fluid resuscitation in patients with hemorrhagic shock: A
meta-analysis. Int J Clin Exp Med. 8:11645–11656. 2015.PubMed/NCBI
|
|
5
|
Moran A, Thacker SA, Arikan AA,
Mastrangelo M-AA, Wu Y, Yu B and Tweardy DJ: IL-6-mediated
activation of Stat3α prevents trauma/hemorrhagic shock-induced
liver inflammation. PLoS One. 6:e214492011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liappis AP, Gibbs KW, Nylen ES, Yoon B,
Snider RH, Gao B and Becker KL: Exogenous procalcitonin evokes a
pro-inflammatory cytokine response. Inflamm Res. 60:203–207. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wright EH and Khan U: Serum
complement-reactive protein (CRP) trends following local and
free-tissue reconstructions for traumatic injuries or chronic
wounds of the lower limb. J Plast Reconstr Aesthet Surg.
63:1519–1522. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Constantin JM, Futier E, Perbet S, Roszyk
L, Lautrette A, Gillart T, Guerin R, Jabaudon M, Souweine B, Bazin
J-E, et al: Plasma neutrophil gelatinase-associated lipocalin is an
early marker of acute kidney injury in adult critically ill
patients: A prospective study. Crit Care. 25:176.e10–176.e6.
2010.
|
|
9
|
Cruz DN, de Cal M, Garzotto F, Perazella
MA, Lentini P, Corradi V, Piccinni P and Ronco C: Plasma neutrophil
gelatinase-associated lipocalin is an early biomarker for acute
kidney injury in an adult ICU population. Intensive Care Med.
36:444–451. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Portal AJ, McPhail MJ, Bruce M, Coltart I,
Slack A, Sherwood R, Heaton ND, Shawcross D, Wendon JA and Heneghan
MA: Neutrophil gelatinase - associated lipocalin predicts acute
kidney injury in patients undergoing liver transplantation. Liver
Transpl. 16:1257–1266. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
de Geus HR, Bakker J, Lesaffre EM and le
Noble JL: Neutrophil gelatinase-associated lipocalin at ICU
admission predicts for acute kidney injury in adult patients. Am J
Respir Crit Care Med. 183:907–914. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Baker SP, O'Neill B, Haddon W Jr and Long
WB: The injury severity score: A method for describing patients
with multiple injuries and evaluating emergency care. J Trauma.
14:187–196. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Morrison CA, Carrick MM, Norman MA, Scott
BG, Welsh FJ, Tsai P, Liscum KR, Wall MJ Jr and Mattox KL:
Hypotensive resuscitation strategy reduces transfusion requirements
and severe postoperative coagulopathy in trauma patients with
hemorrhagic shock: Preliminary results of a randomized controlled
trial. J Trauma. 70:652–663. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
White NJ, Wang X, Liles C and Stern S:
Fibrinogen concentrate improves survival during limited
resuscitation of uncontrolled hemorrhagic shock in a Swine model.
Shock. 42:456–463. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li T, Zhu Y, Hu Y, Li L, Diao Y, Tang J
and Liu L: Ideal permissive hypotension to resuscitate uncontrolled
hemorrhagic shock and the tolerance time in rats. Anesthesiology.
114:111–119. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rezende-Neto JB, Rizoli SB, Andrade MV,
Lisboa TA and Cunha-Melo JR: Rabbit model of uncontrolled
hemorrhagic shock and hypotensive resuscitation. Braz J Med Biol
Res. 43:1153–1159. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lu YQ, Cai XJ, Gu LH, Fan YJ, Wang Q and
Bao DG: Effects of three fluid resuscitation methods on apoptosis
of visceral organs in rats with hemorrhagic shock. J Zhejiang Univ
Sci B. 6:907–912. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ho L, Lau L, Churilov L, Riedel B, McNicol
L, Hahn RG and Weinberg L: Comparative evaluation of crystalloid
resuscitation rate in a human model of compensated haemorrhagic
shock. Shock. 46:149–157. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
De Backer D, Ospina-Tascon G, Salgado D,
Favory R, Creteur J and Vincent JL: Monitoring the microcirculation
in the critically ill patient: Current methods and future
approaches. Intensive Care Med. 36:1813–1825. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Venge P, Eriksson A-K, Douhan-Håkansson L
and Pauksen K: Human neutrophil lipocalin in activated whole blood
is a specific and rapid diagnostic biomarker of bacterial
infections in the respiratory tract. Clin Vaccine Immunol.
24:e00064–e17. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Venge P, Douhan-Håkansson L, Garwicz D,
Peterson C, Xu S and Pauksen K: Human neutrophil lipocalin as a
superior diagnostic means to distinguish between acute bacterial
and viral infections. Clin Vaccine Immunol. 22:1025–1032. 2015.
View Article : Google Scholar : PubMed/NCBI
|