Introduction
Pelvic fractures are mostly caused by high energy
injuries, such as traffic accidents, industrial accidents, crushing
injuries and falling injuries, which account for 10–25% of all
fractures in the body. Among them, unstable fractures account for
7–22%, and the death rate of fracture is approximately 3–28%, which
seriously threatens both the quality and life of patients (1). Conventional conservative treatment
tends to result in pelvic deformity, limb shortening, limb wasting
and recurrent fracture rate, and the disability rate is as high as
50–66% (2). Especially for unstable
fractures, the active surgical reduction is recommended (3). The posterior pelvic ring consists of
sacrospinous ligament, sacro-tuberous ligament, sacroiliac joint
and surrounding ligament, structured in geometrically stable
system, which is relatively stable and its stable effect is 60%
(4). In the case of Tile B and C
fracture, the internal fixation of percutaneous sacrum, sacroiliac
joint screw fixation and minimally invasive plate-screw fixation
can be adopted. They are all applied in clinic according to
different surgical indications (5,6).
Previous studies have been conducted to compare the effects in the
treatment of fracture of the ring instability with different
surgical methods, but there is no uniform conclusion, which
indicates that there are advantages and disadvantages of different
operation methods (7,8). This study summarized the effects of
minimally invasive plate-screw internal fixation and sacroiliac
joint screw fixation of posterior pelvic ring fracture.
Patients and methods
Patient information
A total of 20 patients with unstable fractures in
the pelvic area were diagnosed in Laiwu City People's Hospital
(Laiwu, China) from January 2014 to June 2015, excluding fractures
of other parts, such as fractures of the chest and multiple
fractures. Other exclusion criteria were: Hemorrhagic shock, severe
infection, lower limb paralysis combined with severe anterior ring
fracture, the first stage of operation cannot be completed, and the
surgery needs to be performed, surgical failure, and incomplete
follow-up data. The study was approved by the Ethics Committee of
Laiwu City People's Hospital and was completed by the same
operation and nursing team. Signed written informed consent was
obtained from the patients or guardians.
According to the surgical indications, there were 13
cases (steel plate group) and 7 cases of sacroiliac screw fixation
group (sacroiliac screw group). Among the steel plate group, 8 were
males and 5 were females, aged 26–48 years, (average 35.7±12.3
years),the onset time was 1–12 h (average 5.3±2.5 h), tile
somatotype B type 7 cases, and C type 6 cases. Denis somatotype
standard I, 4 cases; standard II, 6 cases; standard III, 3 cases.
Six cases of injury caused by accident, 4 cases caused by falling
from height, 3 cases caused by crushing, 5 cases of combined
intestinal injury, 2 cases of urethra and bladder injury, 3 cases
of soft tissue open injury, and 3 cases of sacral plexus nerve
injury. Among sacroiliac screw group, 5 were males and 2 were
females, aged 23–46 years (average 33.6±11.4 years), the onset time
was 1.5–12.5 h (average 5.5±2.6 h), tile somatotype B type 6 cases,
and C type 1 case. Denis somatotype standard I, 3 cases; standard
II, 3 cases; standard III, 1 case. Four cases of injury caused by
accident, 2 caused by falling from height, 1 caused by crushing, 2
of combined intestinal injury, 2 of urethra and bladder injury, 2
of soft tissue open injury, and 1 case of sacral plexus nerve
injury. Baseline data of the two groups were not statistically
significant (P>0.05).
Operation method
Two groups of patients were treated with systemic
chemotherapy. This includes stabilizing vital signs, treating
various blood loss, hypoxia, rehydration, electrolyte and acid-base
balance, infection, and treating open wounds, searching for
potential wounds, preventing complications, completing various
examinations and assessing the risks of surgery. Posterior tension
band steel surgical indications: After preoperative traction
reduction of sacroiliac joint fracture dislocation Denis
classification I, II, III area sacrum with vertical fracture,
sacroiliac joint dislocation after iliac spine fracture or iliac
wing fractures. Contraindications: Old fracture cannot be reset,
severe osteoporosis, large soft tissue injury in the posterior ring
area, obvious weight loss, flat surface of steel plate top
pressure. Percutaneous sacrosacroiliac screw fixation syndrome:
Five days after injury, preoperative traction caused pelvic
reposition, severe soft tissue injury, intestinal injury or both.
Contraindications: Closed reduction failure, C-arm cannot see the
posterior lateral and lateral structure of the sacrum, the sacrum
deformity and osteoporosis.
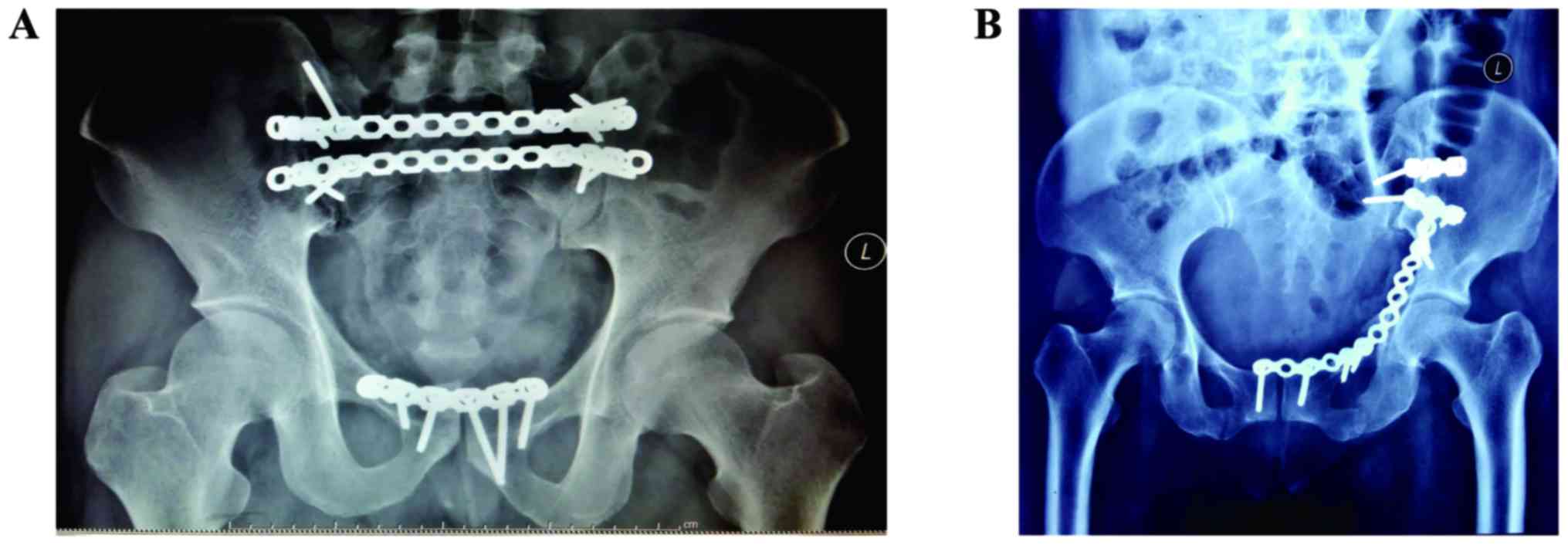
Posterior tension belt plate
fixation
Selecting general anesthesia, prone position, and
the longitudinal incision of 3–4 cm on the lateral iliac spine of
the posterior superior iliac spine, dissecting the attachment of
the gluteal superior iliac spine, revealing the posterior side of
the iliac flank, exposing the fracture line, removing sacroiliac
articular cartilage, and correcting the fracture and dislocation of
sacroiliac joint by pulling, prying and squeezing. Preparing the
14–16 hole with one or two pieces of steel plate, inserting steel
plate respectively along the sacrum subcutaneous tunnel to the
contralateral posterior spine, crossing the sacrum, bending steel
plate on both sides of a bow to adapt to the spines on the slope
after skeletons, making side plate appropriate for long fracture
dislocation; after C-arm machine proved fracture or dislocation
position can be accepted, turning the screws in turn on both sides;
plate length ensured that both sides can be fixed with more than
three screws. After iliac spine on the vertex angle of the screw
down along the ilium between inner and outer plate, intraoperative
probes for sounding are available, and borehole walls are bone,
which will have long cancellous bone screw into the iliac crest,
and postoperative iliac cancellous bone graft (Fig. 1).
Percutaneous sacroiliac joint screw
fixation
General anesthesia machine, supine, C-arm to rotate
photographs of entrance and exit, lumbar di ministry soft pillow up
hip pad through X-ray, below the surface of the skin before the
entry point is located in the femoral screw axis and iliac spines
on the perpendicular intersection point <2 cm, skin incision,
gram in ilium posterolateral needle, and show needle point to push
S1 perpendicular to the sacroiliac joint. C-arm machine line side,
confirmed that the guide for S1 vertebral was central, accurate
location, needle to S1 vertebral body direction, until export to
the outside of the needle tip to S1 nerve hole on the surface.
Reposition the lateral perspective to confirm that the guide tip is
in the safe zone of S1. The whole process should be completed in
three directions under the perspective; if the needle position is
good, immediately turned the screw, not using excessive reset or
pressure, in order to avoid injury of nerve root, and trying not to
make the screw over the midline (Fig.
1).
Postoperative treatment
Postoperative treatment involved: Ηip knee joint
activities, muscle strength training, turning over and lying on the
side, being in semi-reclining position after 1 week, sitting in a
wheelchair at 2–4 weeks, walking with crutches with part load after
4 weeks, and gradually to full load, trying to walk without
crutches after 6 months, trying to half crouch after 8 months.
Observation indexes
During the follow-up of approximately 1 year, the
indexes of perioperative period, including operation time,
radiation exposure, intraoperative blood loss, incision length,
partial load time and total load time, and the complications
occurred were compared. Clinical effect evaluation: According to
patients' life self-care ability, pain degree, degree of
dysfunction and fracture healing, Function rating criteria: Majeed
pelvis (9), 85–100 was considered
optimal, 70–84 was good, 55–69 was medium, and ≤54 was poor.
Anatomic effect evaluation: According to the Matta and Tornetta
standard (10) pelvic posterior ring
displacement of ≤4 mm is optimal, 4–10 mm is good, 11–20 mm is
medium and >20 mm is poor.
Statistical methods
Using SPSS 19.0 (IBM Corp., Armonk, NY, USA)
statistical software for input and analysis of quantitative data to
average ± standard deviation, comparison between groups using
independent sample t-test, qualitative data using the number of
cases or percentage (%), the comparison between group using
Chi-square test (χ2), level data by using rank and
inspection. P<0.05 was considered to indicate a statistically
significant difference.
Results
Comparison of perioperative
indicators
There was no statistically significant difference
between the two groups of surgical time, radiation exposure,
intraoperative bleeding, incision length, partial load time and
total load time (P>0.05) (Table
I).
 | Table I.Comparison of perioperative
indicators. |
Table I.
Comparison of perioperative
indicators.
| Groups | The operation time
(min) | Radiation exposure
(Gy) | Intraoperative blood
loss (ml) | The length of the
incision (cm) | Partial load time
(day) | Full load time
(day) |
|---|
| Steel | 65.8±9.6 | 56.7±6.7 | 326.4±34.2 | 7.8±1.2 | 6.5±1.3 | 24.7±3.4 |
| Sacroiliac screw | 61.2±10.2 | 53.3±6.9 | 335.7±26.8 | 7.6±1.3 | 6.3±1.4 | 25.8±3.3 |
| t-value | 0.637 | 0.768 | 0.649 | 0.329 | 0.729 | 0.492 |
| P-value | 0.428 | 0.539 | 0.755 | 0.487 | 0.632 | 0.527 |
Comparison of complications
In steel plate group, 3 cases of incision and
internal plant infection, 2 cases of intraoperative blood vessel
and nerve injury, 1 case of displacement of steel plate, 3 cases of
fracture of internal fixation and curved nail, 1 case of bone not
healing, a total of 10 cases of complications (21.7%). In
sacroiliac screw group, there were 2 cases of incision and internal
plant infection, 3 cases of intraoperative blood vessel and nerve
injury, 5 cases of fracture of internal fixation and curved nail, 2
cases of bone not healing, a total of 12 cases of complications
(30.0%). Comparing complication rates between the two groups, there
was no statistically significant difference (Chi-square =0.767,
P=0.767) (Data not shown).
Comparison of clinical effect
evaluation and anatomic effect evaluation
In the comparison of clinical effect evaluation and
anatomic effect evaluation between the groups, there was no
statistically significant difference (P>0.05) (Table II).
 | Table II.Comparison of clinical effect
evaluation and anatomic effect evaluation [case (%)]. |
Table II.
Comparison of clinical effect
evaluation and anatomic effect evaluation [case (%)].
|
|
| Clinical effect
evaluation | Anatomic effect
evaluation |
|---|
|
|
|
|
|
|---|
| Groups | No. of cases | Optimum | Fair | Medium | Poor | Optimum | Fair | Medium | Poor |
|---|
| Steel | 13 | 3 (23.1) | 3 (23.1) | 4 (30.8) | 3 (23.1) | 2 (15.4) | 3 (23.1) | 3 (23.1) | 5 (38.5) |
| Sacroiliac screw | 7 | 1 (14.3) | 2 (28.6) | 3 (42.9) | 1 (14.3) | 1 (14.3) | 2 (28.6) | 1 (14.3) | 3 (42.9) |
| χ2 |
| 0.400 |
|
|
| 0.265 |
|
|
|
| P-value |
| 0.940 |
|
|
| 0.968 |
|
|
|
Discussion
Matta and Tornetta (10) reported for the first time, closed
reduction and satisfactory dislocation of sacroiliac joint
position, percutaneous implantation of sacroiliac joints under
perspective screws, clinical effect was satisfactory, and the
sacroiliac joint screw fixation was centric, the fixed strength was
more than steel plate internal fixation, small surgical trauma,
good stability and less complications. Routt et al (11) found that percutaneous sacroiliac
screw implanting in S1 vertebral body, there is a narrow area of
security, and the front is iliac wing slope cortex, the left L5
nerve root and iliac blood vessels, and the rear of the security
area is S1 nerve root hole, and implant screw should be in pelvic
inlet and outlet, and the sacrum is oblique perspective under the
auxiliary. The biomechanical study confirmed that (12), S1, S2, parallel double screw had
better pelvic ring stability than single S1 screw. Type C-Arm X-ray
machine perspective can be safely inserted under tension screw, but
X-ray machine under the perspective of sacroiliac complex
three-dimensional structure of the image is not accurate; for
patients with obesity, pneumatosis lumen X-ray image is blurred,
and intraoperative needs to take an entrance and exit, and the
needle point location is difficult to grasp, repeatedly in
perspective. Nelson and Duwelius (13) reported the satisfactory curative
effect of CT guided percutaneous sacroiliac screw fixation for
posterior pelvic fracture. CT guided percutaneous nailing accurate
operation, with small surgical trauma and radioactive damage, and
can maintain the continuity of the fracture surrounding soft
tissue, and biomechanical stability is high, which has fewer
complications, and patients are active earlier. The disadvantages
are that patients must be moved to the CT room, and the operation
is cumbersome, which increases the risk of infection, and there is
a possibility of fracture remigration. Computer assisted
orthopaedic surgery (CAOS) has been increasingly applied to
treating pelvic fractures due to its numerous advantages (14). CAOS intraoperatively can directly
obtain image simulation of the operation, again without perspective
to find the needle point. No replacement of the surgical position
is needed when the pelvic and posterior rings are fixed at the same
time, which can effectively reduce the operation time and patients
X-ray radiation. But the development time of CAOS in orthopaedic
treatment is shorter, with complex equipment, complicated
operation, long learning curve, and high price. Only some medical
institutions with better conditions can carry out these operations.
So the CAOS is still in the stage of clinical research, with its
unique advantages, which still has a broad application
prospect.
Krappinger et al (15) treated 31 cases of Tile type C pelvic
ring fractures with minimally invasive plate-screw fixation, which
achieved satisfactory clinical efficacy. They considered the
unstable pelvic fractures minimally invasive plate can effectively
be fixed, reconstructing the stability of pelvic ring, reduced the
incidence of iatrogenic neural tissue and vascular injury. The
disadvantages are the poor success rate of the anatomical
repositioning, needing bridge bilateral sacroiliac joints at the
same time, and taking out the steel plate later. Reconstruction
plate internal fixation was characterized by simple operation,
small trauma, firm fixing, and the steel plate is easy to shape.
Applied to bilateral and comminuted sacroiliac complex injuries,
the fixing and reconstruction plate not only can maintain reset,
but also does not produce any compression effect on the sacral
foramen and sacral canal, as to avoid the injury of sacral nerve
and pelvic vessels (16).
Through this study, we concluded that the operation
time, amount of radiation exposure, intraoperative blood loss,
length of incision, partial load and full load time, and comparison
of complications between the two groups, there were no
statistically significant differences. There were no significant
differences between the two groups in the evaluation of clinical
effect and the evaluation of anatomical effects.
In conclusion, minimally invasive plate-screw
internal fixation and sacroiliac joint screw fixation in the
treatment of posterior pelvic ring fracture both have indications
and their therapeutic effects are about the same. We will increase
the sample size, extend the follow-up time, expand the selected
population for prospective study in further studies, in order to
master the respective indications, improve the surgical effect, and
reduce the complications.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SL wrote this manuscript. SL, DZ XM and WL collected
and analyzed the data. ZS and XW performed the experiments. HQ and
SW interpreted the results. DZ revised and finalized this study.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Laiwu City People's Hospital (Laiwu, China). Patients who
participated in this research, had complete clinical data. Informed
consent was obtained from the patients or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Referenc
|
1
|
Acker A, Perry ZH, Blum S, Shaked G and
Korngreen A: Immediate percutaneous sacroiliac screw insertion for
unstable pelvic fractures: Is it safe enough? Eur J Trauma Emerg
Surg. 14:5–6. 2016.
|
|
2
|
Costantini TW, Coimbra R, Holcomb JB,
Podbielski JM, Catalano R, Blackburn A, Scalea TM, Stein DM,
Williams L, Conflitti J, et al: AAST Pelvic Fracture Study Group:
Current management of hemorrhage from severe pelvic fractures:
Results of an American Association for the Surgery of Trauma
multi-institutional trial. J Trauma Acute Care Surg. 80:717–723;
discussion 723–725. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Buller LT, Best MJ and Quinnan SM: A
nationwide analysis of pelvic ring fractures: Incidence and trends
in treatment, length of stay, and mortality. Geriatr Orthop Surg
Rehabil. 7:9–17. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fan Y, Lei J, Liu H, Li Z, Cai X and Chen
W: Three-dimensional finite element analysis to T-shaped fracture
of pelvis in sitting position. Sheng Wu Yi Xue Gong Cheng Xue Za
Zhi. 32:997–1003. 2015.(In Chinese). PubMed/NCBI
|
|
5
|
Halawi MJ: Pelvic ring injuries: Surgical
management and long-term outcomes. J Clin Orthop Trauma. 7:1–6.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Prasarn ML, Horodyski M, Schneider PS,
Pernik MN, Gary JL and Rechtine GR: Comparison of skin pressure
measurements with the use of pelvic circumferential compression
devices on pelvic ring injuries. Injury. 47:717–720. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shrestha D, Dhoju D, Shrestha R and Sharma
V: Percutaneous ilio-sacral screw fixation in supine position under
fluoroscopy guidance. Kathmandu Univ Med J KUMJ. 13:56–60. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu XM, Pan CW, Wang GD, Cai XH, Chen L,
Meng CF and Huang JC: Finite element analysis of the stability of
combined plate internal fixation in posterior wall fractures of
acetabulum. Int J Clin Exp Med. 8:13393–13397. 2015.PubMed/NCBI
|
|
9
|
Majeed SA: Grading the outcome of pelvic
fractures. J Bone Joint Surg Br. 71:304–306. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Matta JM and Tornetta P III: Internal
fixation of unstable pelvic ring injuries. Clin Orthop Relat Res.
329:129–140. 1996. View Article : Google Scholar
|
|
11
|
Routt ML Jr, Simonian PT, Agnew SG and
Mann FA: Radiographic recognition of the sacral alar slope for
optimal placement of iliosacral screws: A cadaveric and clinical
study. J Orthop Trauma. 10:171–177. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cai HM, Liu YW, Li HJ, Wu XJ, Tang HT,
Zhang Y, Jia YD and Li WY: S2 iliosacral screw insertion technique.
Zhongguo Gu Shang. 28:910–914. 2015.(In Chinese). PubMed/NCBI
|
|
13
|
Nelson DW and Duwelius PJ: CT-guided
fixation of sacral fractures and sacroiliac joint disruptions.
Radiology. 180:527–532. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Collinge C, Coons D, Tornetta P and
Aschenbrenner J: Standard multiplanar fluoroscopy versus a
fluoroscopically based navigation system for the percutaneous
insertion of iliosacral screws: A cadaver model. J Orthop Trauma.
19:254–258. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Krappinger D, Larndorfer R, Struve P,
Rosenberger R, Arora R and Blauth M: Minimally invasive transiliac
plate osteosynthesis for type C injuries of the pelvic ring: A
clinical and radiological follow-up. J Orthop Trauma. 21:595–602.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kobbe P, Hockertz I, Sellei RM, Reilmann H
and Hockertz T: Minimally invasive stabilisation of posterior
pelvic-ring instabilities with a transiliac locked compression
plate. Int Orthop. 36:159–164. 2012. View Article : Google Scholar : PubMed/NCBI
|