Introduction
Venous malformations (VMs) consist of distorted and
ectatic veins, which are enveloped sparsely by smooth muscle cells
(SMCs) (1). VMs are low-flow
vascular anomalies and will develop throughout life in the body
without appropriate management (2,3). VMs
comprise 50–75% of vascular malformations (4). Almost 40% of VMs are located in the
head and neck region, particularly in the oral cavity, airway tract
and related muscles (5). According
to Legiehn and Heran, 98% of VMs are sporadic and non-inherited,
and inherited VMs are typically multifocal (6). It has been estimated that VM occurs at
an incidence of 1–2 individuals per 10,000 births (7). VMs in the temporal muscle of the face
commonly cause cosmetic deformity and migraine, and those located
in the extremities often lead to the development of hypotrophy or
hypertrophy, as well as muscle weakness (8). Treatment regimens include
sclerotherapy, laser therapy, embolization and surgical resection
(9). The primary goals of treating
VM include alleviating pain, mitigation of functional disability
and amelioration of cosmetic deformity (10). Severe VMs often persist despite
current treatment alternatives (11), and for this reason, a novel
therapeutic strategy utilizing rapamycin to alleviate VM was
explored in the present study.
Rapamycin, as a macrolide antibiotic, allosterically
regulates the process of substrates entering the catalytic site of
the mammalian target of rapamycin (mTOR) (12). Rapamycin not only binds to mTOR but
also serves as the prototypical inhibitor of mTOR (13). Produced by Streptomyces
hygroscopicus, rapamycin has multiple biological and
pharmacological properties (14),
including immunosuppressive (15),
anti-neoplastic (16),
neuro-protective (17) and
anti-aging activities (18).
Rapamycin serves a critical role in modulating endothelial cells by
repressing mTOR, and it can not only suppress inflammation, but
also prevent and mitigate post-angioplasty coronary artery
restenosis (19). Cell contact in
endothelial cells is mediated by the characteristics of endothelial
monolayers, regulating the biological behaviors of endothelial
cells and contributing to vascular homeostasis (20). Accordingly, aberrant disruptions of
cell contact in endothelial cells are of substantial importance in
cardiovascular diseases and are key features of pathologically
altered vascular endothelium (21).
Venous endothelial cells have differing responses to angiogenic
signals, thus the biological behaviors of endothelial cells have
been investigated previously in the pathogenesis and treatment of
VM (4). The aim of the current study
was to investigate the effects of rapamycin on the biological
behaviors of endothelial cells, such as proliferation, migration
and apoptosis in human VMs.
Materials and methods
Cell separation and culture
Between January 2016 and January 2017, 10 cases of
single oral buccal and facial VM were reported at Department of
Oral and Maxillofacial Surgery, The Affiliated Stomatological
Hospital of Nanjing Medical University, including 4 male and 6
female patients, with a mean age of 29.4±13.7 years. The diagnosis
of buccal facial vein malformation was confirmed by preoperative
pathological examination. The inclusion criteria were as follows:
Patients who were diagnosed with single oral buccal and facial
venous malformation by pathological examination. The exclusion
criteria were as follows: Patients who were diagnosed with other
types of venous malformations on the face, hypertension, serious
cardiovascular and cerebrovascular diseases, and other patients who
were not suitable for treatment (for example cardiopulmonary
dysfunction or poor recovery). The present study was approved by
the Ethics Committee of The Affiliated Stomatological Hospital of
Nanjing Medical University (Nanjing, China) and written informed
consent was obtained from each subject. Surgically resected VM
tissues were separated under aseptic conditions, and the exposed
malformed vascular mass was cut open. Sponge-like sinusoids were
then visualized and were sliced into tissue blocks of approximately
3–5 mm2. Following immersing in culture medium for
minimal humidification, tissue blocks were inoculated in a culture
flask that was subsequently plated on 1% gelatin, with the intima
facing downward. Tissue blocks were separated by a distance of ~5
mm. The tissue blocks were then incubated in Dulbecco's modified
Eagle's medium containing 20% fetal bovine serum (Gibco; Thermo
Fisher Scientific, Inc., Waltham, MA, USA) at 37°C with the culture
flask inverted. Following 6 h, the culture flask was upended for
incubation at 37°C. Tissue blocks and non-adherent cells were
removed, and adherent cells were incubation in Endothelial Cell
medium (cat. no. 1001; ScienCell Research Laboratories, Inc., San
Diego, CA, USA) for 3 days at 37°C. Cellular morphology was
observed under an inverted microscope at a magnification of ×400,
and cells outside the circle were removed using a cytopipette.
Subsequently, tissue blocks were washed using PBS twice to remove
other cells, and the culture medium was replaced. When cells had
reached 70–90% confluency, 0.25% trypsin supplemented with
ethylenediaminetetraacetic acid was used for cell subculture.
Identification of endovascular
epithelial cells separated from deformed veins in human VM
Flow cytometry analysis was used to detect
endovascular epithelial markers in order to identify endovascular
epithelial cells. Separated cells from deformed veins in human VM
were detached using 2.5 g/l tryptase and centrifuged at 167 × g and
4°C for 5 min. The cells were washed with cold PBS at 4°C and
centrifuged at 167 × g and 4°C for 5 min. The washing and
centrifugation were repeated and then the cells were made into a
single cell suspension. With 1×106 cells per tube, a
15-min incubation at 37°C was performed with the addition of 20 µl
phycoerythrin-conjugated anti-human cluster of differentiation
(CD)31 antibody (cat. no. 566177; 1:500; BD Biosciences, San Jose,
CA, USA), or a 30-min incubation at 4°C with the addition of 20 µl
mouse anti-human von Willebrand factor (vWF) monoclonal antibody
(cat. no. 555849; 1:500; BD Biosciences). For determination of
CD31/vWF, a simultaneous incubation was performed for 15 min at
37°C. Subsequently, a second incubation for 30 min at 4°C with the
addition of 50 µl fluorescein isothiocyanate-labeled rabbit
anti-mouse IgG (cat. no. TA130002; 1:1,000; OriGene Technologies,
Inc., Beijing, China) was performed. Cells were place in tubes on
the ice in the dark for 30 min, washed three times using 2 ml PBS
and at 167 × g and 4°C and to remove the supernatant. Then 500 µl
PBS (containing 4% paraformaldehyde) was used to fix the cells at
4°C for 30 min prior to performing the flow cytometry. Cell
identification was conducted using a FACSCan flow cytometer and the
data was analyzed by Cell Quest Software (version 5.1; both BD
Biosciences, Franklin Lakes, NJ, USA).
Cell grouping and treatment
The separated and determined endothelial cells of
human VM were assigned into a blank group (cells cultured
conventionally, without any treatment); a 1 ng/ml group (cells
cultured in medium with rapamycin working solution at a
concentration of 1 ng/ml); a 10 ng/ml group (cells cultured in
medium with rapamycin working solution at a concentration of 10
ng/ml); a 100 ng/ml group (cells cultured in medium with rapamycin
working solution at a concentration of 100 ng/ml), and a 1,000
ng/ml group (cells cultured in medium with rapamycin working
solution at a concentration of 1,000 ng/ml). Rapamycin was
purchased from Hunan TaiRen Pharmaceutical Co., Ltd. (Changsha,
China).
MTT assay
Cell viability of the endothelial cells in each
group was measured at 24, 48 and 72 h following incubation. The
optimal reaction time point for rapamycin was determined for the
observation of cell morphological changes under an inverted
microscope and other experiments. A cell suspension for each group
was inoculated in 96-well plates at a density of 5×104
cells/well following dilution. A total of 6 reduplicate wells were
set up for each group. Upon reaching 80% confluency, endothelial
cells were treated as described above. Following reoxygenation, 20
µl MTT solution (Sigma Aldrich; Merck KGaA, Darmstadt, Germany) was
added and incubated for 4 h at 37°C, followed by the removal of MTT
solution. Subsequently, each well was supplemented with 150 µl
dimethyl sulfoxide (Sigma Aldrich; Merck KGaA). Following shaking
on a shaking table for 10 min, the optical density (OD) value of
each well was measured using a microplate reader at a wavelength of
490 nm. The experiment was repeated 3 times, and the mean OD value
was calculated. Cell viability was calculated as follows: (OD
valueexperimental group-OD valueblank
group)/OD valueblank group.
Terminal
deoxynucleotidyl-transferase-mediated dUTP nick end labelling
(TUNEL) assay
Slides with attached cells were fixed in 4% (w/v)
paraformaldehyde for 30 min at room temperature, rinsed in PBS,
blocked with 0.3% H2O2 in methanol for 15 min
at room temperature, and finally rinsed in PBS. Subsequently,
slides were maintained in 0.1% Triton X-100 at 4°C for 20 min. The
TUNEL assay (cat. no. C1098; Beyotime Institute of Biotechnology,
Haimen, China) was performed according to the manufacturer's
instructions. Slides were blocked with 3% bovine serum albumin
(cat. no. C0225; Beyotime Institute of Biotechnology) at 37°C for
20 min, followed by 3 washes with PBS (5 min per wash).
Subsequently, peroxidase solution was added, and the slides were
incubated in a humidity chamber at 37°C for 30 min, followed by PBS
washing 3 times (5 min/wash). Diaminobenzidine (0.3 ml) as a
substrate was added as a chromogen, and the slides were incubated
in a humidity chamber at 15–20°C for 10 min, followed by 3 washes
with PBS (5 min per wash). Counterstaining was performed
conventionally with hematoxylin at 37°C for 10 sec. Subsequently,
ethanol-hydrochloric acid was used for differentiation, and ammonia
was used to color the cells blue. The cells were mounted with 4%
Paraformaldehyde Fix Solution (cat. no. P0099; Beyotime Institute
of Biotechnology) and photographed. Normal endothelial cells were
stained blue, and apoptotic cells were yellow and brown. Five
fields of vision were randomly selected. The apoptosis rate for a
fixed area was calculated (apoptosis rate=apoptotic cells/total
cells in a field).
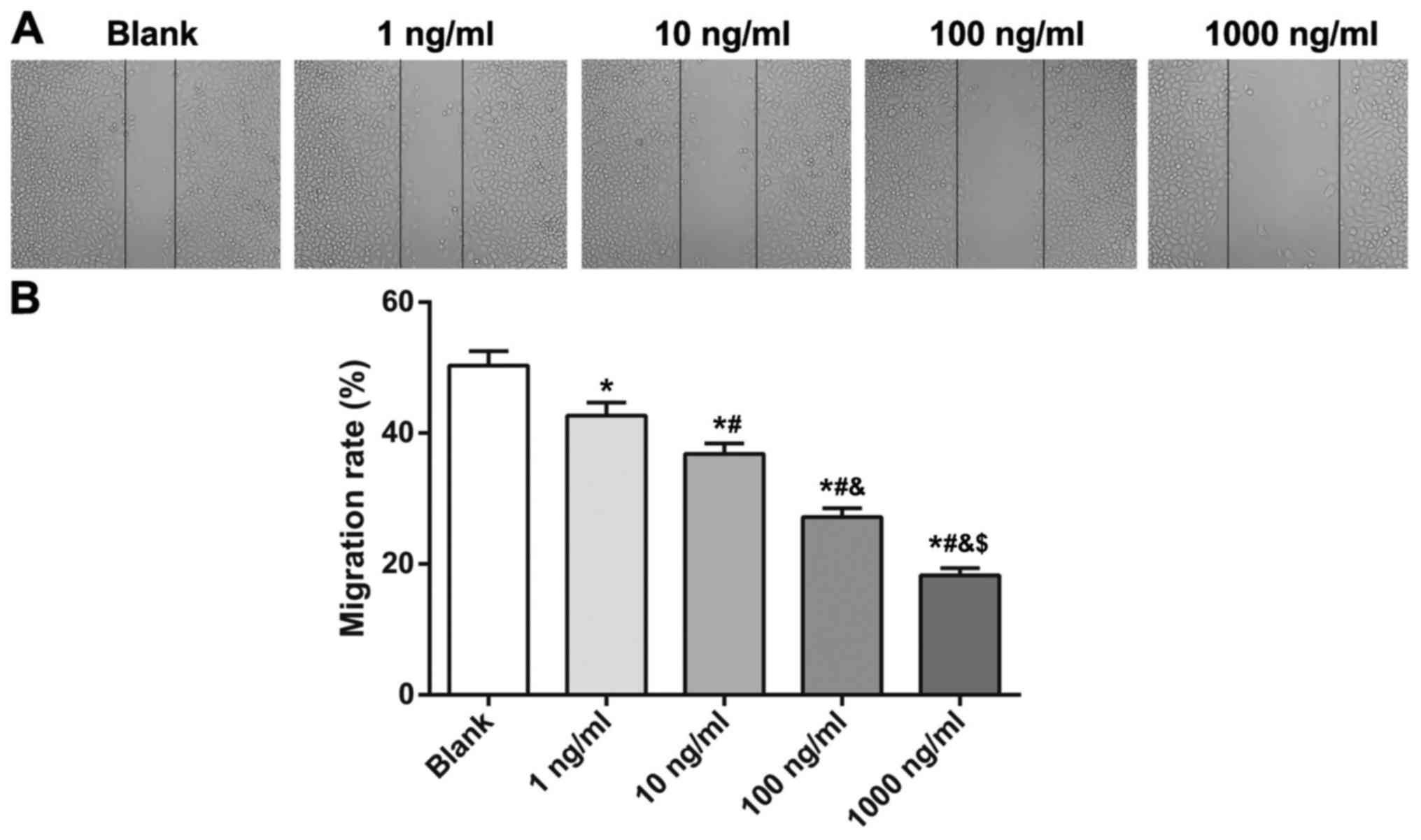
Wound-healing assay
On the back of a 6-well plate, uniform horizontal
lines at intervals of approximately 0.8 cm were drawn across the
wells using a marker. Each well was crossed by at least 5 lines,
and ~5×105 cells were inserted into each well and grown
to 100% confluency. The following day, a sterile 10-µl pipette tip,
perpendicular to the horizontal lines on the back, was used to
scratch wounds along a ruler. Importantly, the pipette tip was
upright, rather than slanted. Following wound scratching, the cells
were rinsed gently with PBS 3 times. Then, PBS was added along the
wall, and the scratched cells were rinsed and removed. The
endothelial cells were incubated with culture medium in a 5%
CO2 incubator at 37°C. Samples were taken at 48 h and
then photographed. The rate of wound closure was calculated by
measuring the distance between the two wound edges at 0 h and at 48
h. The experiment was repeated 3 times, and the mean value was
calculated.
Statistical analysis
SPSS 21.0 software (IBM Corp., Armonk, NY, USA) was
used to analyze data in the present study. Measurement data are
presented as the mean ± standard deviation. Comparisons among
multiple groups were performed using one-way or two-way analysis of
variance followed by Tukey's post hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
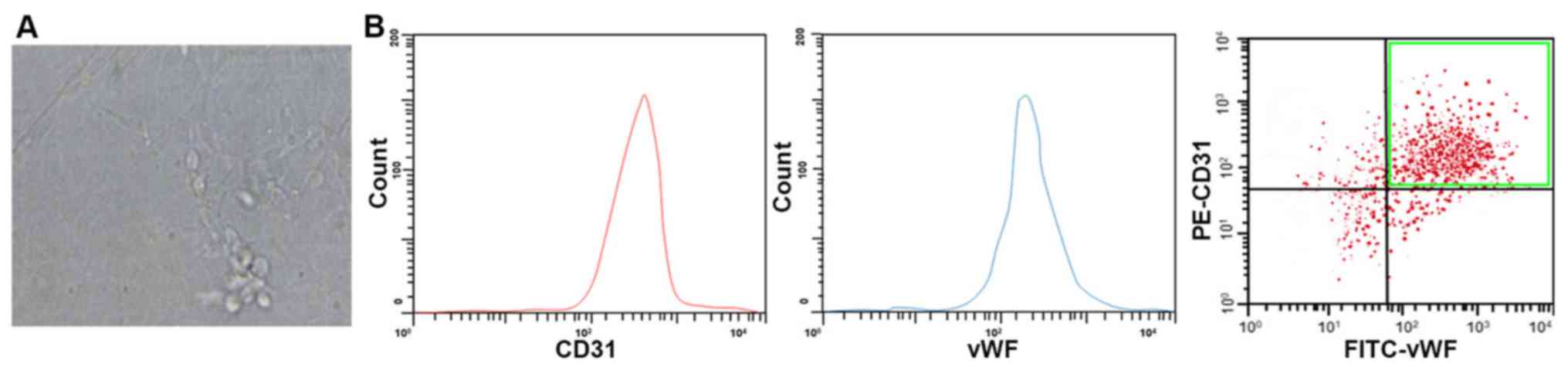
Observation and determination of human
VM endothelial cells
The cellular morphology of separated human VM
endothelial cells was observed under an inverted microscope. When
the separated endothelial cells grew adherent to the wall, they
were enlarged to different degrees and grew in clusters, resembling
paving stones, with clear, homogeneous cytoplasm and a round or
oval nucleus (Fig. 1A). For accurate
identification of endovascular epithelial cells separated from the
deformed vein of a human VM, flow cytometry was performed to
evaluate a more specific marker for endovascular epithelial cells,
CD31 and vWF, and it was demonstrated that there were 92.5%
CD31-positive cells, 88.2% vWF-positive cells, and 76.3% CD31- and
vWF-positive cells (Fig. 1B).
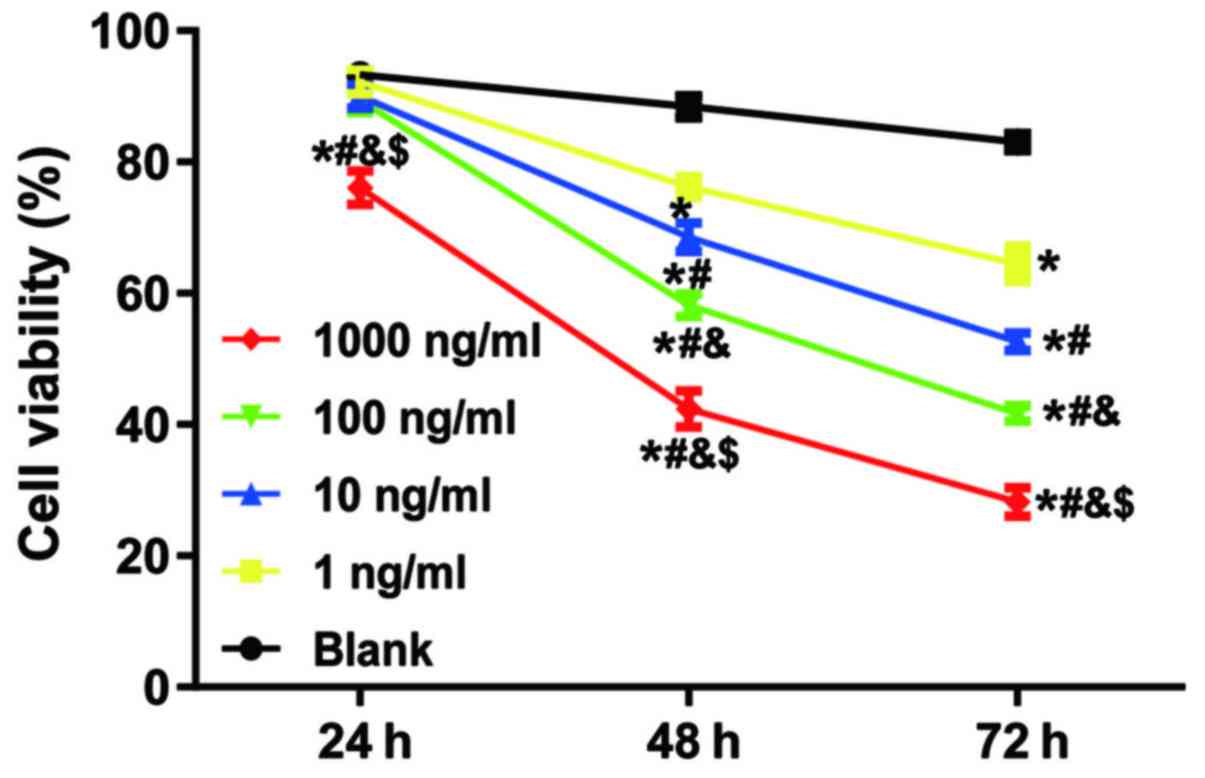
Rapamycin inhibited the cell viability
of human VM endothelial cells
An MTT assay was performed to detect the cell
viability of human VM endothelial cells exposed to rapamycin
(Fig. 2). Rapamycin significantly
inhibited the proliferation of human VM endothelial cells at 48 and
72 h. Higher concentration of rapamycin induced greater inhibitory
effects. However, only rapamycin at a concentration of 1,000 ng/ml
significantly inhibited the viability of human VM endothelial cells
at 24 h, suggesting that the inhibitory effects of rapamycin on
human VM endothelial cells were concentration- and time-dependent.
Therefore, 48 h following incubation was determined to be the
optimal reaction time.
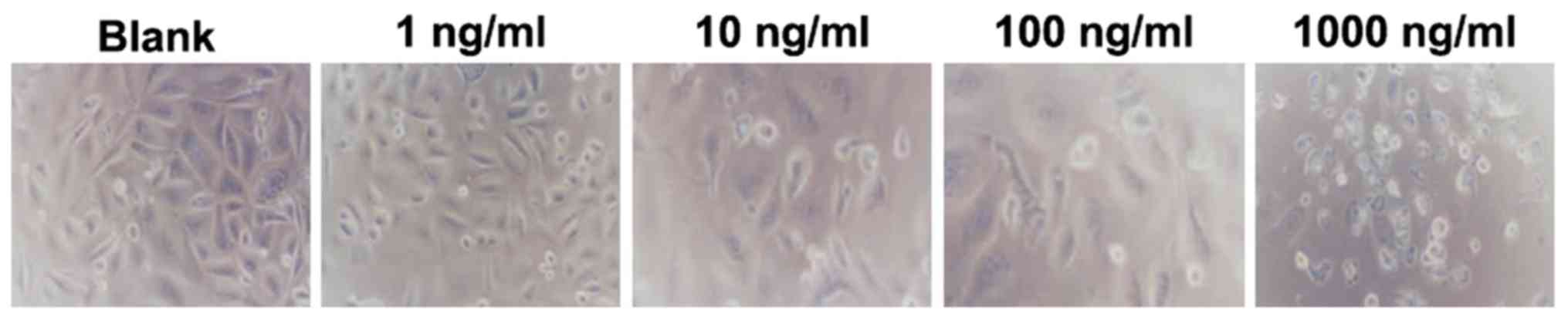
Effects of rapamycin on cellular
morphology of human VM endothelial cells
An inverted microscope was used to observe the
morphological changes of human VM endothelial cells exposed to
rapamycin at different concentrations (Fig. 3). At 48 h, when compared with the
blank group, treatment with rapamycin at a concentration of 1 ng/ml
produced a few shrunken cells and a reduced cell number; however,
the majority of cells exhibited a clear boundary and a regular
shape. Treatment with rapamycin at 10 and 100 ng/ml reduced the
number of cells even further and caused some cells to become round
and desquamated; treatment with rapamycin at 1,000 ng/ml produced
more obvious desquamation, round-shaped cells and necrosis.
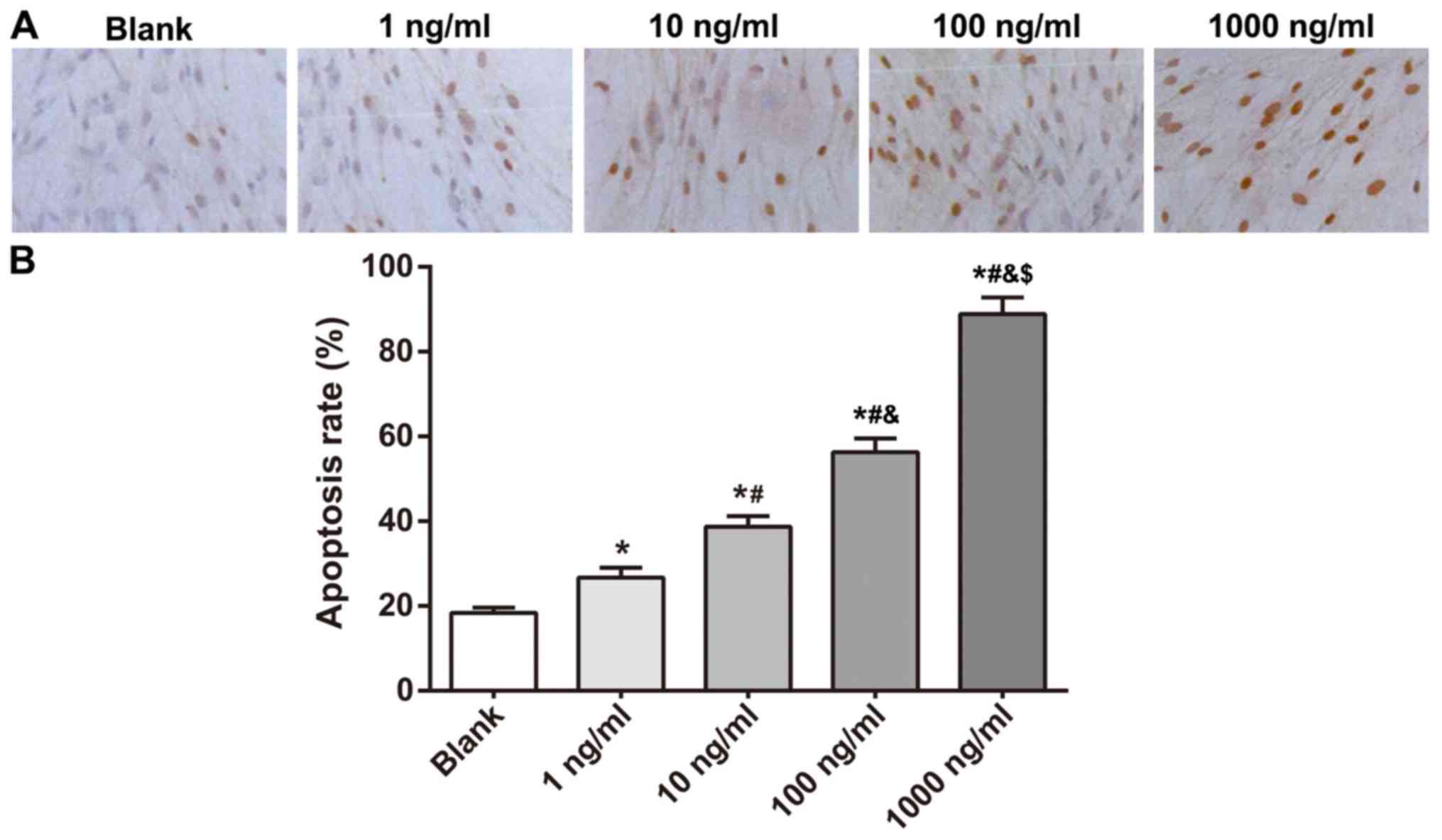
Rapamycin enhanced apoptosis
conditions in human VM endothelial cells
A TUNEL assay was conducted to determine the
apoptosis conditions of human VM endothelial cells exposed to
rapamycin at different concentrations (Fig. 4). In comparison with the blank group,
apoptosis of human VM endothelial cells was significantly elevated
when treated with rapamycin at 1, 10, 100 and 1,000 ng/ml. Higher
concentrations yielded greater numbers of apoptotic endothelial
cells, indicating that rapamycin treatment promoted the apoptosis
of human VM endothelial cells.
Rapamycin inhibited the migration
capacity of human VM endothelial cells
A wound-healing assay further verified the
inhibitory effects of rapamycin on the migration capacity of human
VM endothelial cells (Fig. 5).
Compared with the blank group, rapamycin significantly suppressed
the migration capacity of human VM endothelial cells at different
concentrations. Higher concentrations yielded greater inhibitory
effects.
Discussion
VMs damage the appearance and circulatory
functioning of patients and even produce deadly bleeding and
respiratory obstruction (3).
Extensive VMs require lifelong treatment and may persist or become
exacerbated (7,22). Rapamycin has already been reported in
clinical trials to serve as an effective treatment for cancer,
vascular restenosis and immune rejection of transplanted organs
(23,24). The aim of the present study was to
explore the biological behaviors of human VM endothelial cells and
their responses to rapamycin, which may be significant in the
design of effective strategies for human VM treatment.
Initially, endothelial cells of human VM were
separated and identified by detecting the positive expression of
CD31 and vWF. CD31 and vWF are widely acknowledged as a specific
marker for human endothelial cells (25); therefore, the strong positive
expression of these markers confirmed the successful isolation of
human VM endothelial cells. Endothelial cells secrete cytokines and
adhesion molecules during the process of inflammation;
additionally, accumulation of neutrophils within vascular
endothelia is associated with the inflammatory process (2). Endothelial cells are also considered to
be markers of endothelial dysfunction and endothelial injury
(26). The number of proliferating
endothelial cells and vascular SMCs is rather limited in normal
vascular tissues, whereas a physiological or pathological stimulus
can stimulate endothelial cells and SMCs to progress in the cell
cycle (27). More specifically, it
has been noted in a previous study that endothelial cells separated
from VMs best represent the biological characteristics of VMs
(4).
The cell viability of endothelial cells treated with
rapamycin was determined by MTT assay at 24, 48 and 72 h following
culture. The results indicated that rapamycin suppressed
proliferation of human VM endothelial cells. As an mTOR inhibitor,
rapamycin has been hypothesized to block the progression of cell
cycle from G1 phase to S phase by inhibiting p70
ribosomal protein S6 kinase (p70S6K) (13,28).
mTOR, as a threonine kinase, phosphorylates S6K1 and 4E-BP1, and
promotes transcription of key mRNAs associated with the progression
of the cell cycle from G1 phase to S phase (29,30).
Through its interaction with p70S6K, it is associated with cell
growth, proliferation and differentiation by regulating ribosome
biogenesis, protein synthesis, cell cycle progression and
metabolism (31). Consistent study
demonstrates that rapamycin significantly represses the
proliferation and migration of hemangioma, and reduces vascular
tumor growth by suppressing the mTOR complex, which regulates cell
mass and cell number. In addition, it has been revealed that
rapamycin delays the aging process of mice by attenuating the
degeneration of the liver and the heart, reducing the proliferation
of adrenal gland lesions and altering tendon elasticity (32). Via its anti-proliferative properties,
rapamycin reduces the cell viability of lymphocytes, vascular
endothelial cells and SMCs and decreases the fibro-proliferative
responses in vascular injuries (33).
The migration capacity of human VM endothelial cells
was demonstrated to be suppressed following treatment with
rapamycin. At the same time, apoptosis conditions in human VM
endothelial cells were enhanced, as detected using flow cytometry.
These findings are corroborated by the results of Liu et al
(34), which demonstrated that
rapamycin suppressed reendothelialization by attenuating the
migration and promoting the apoptosis of endothelial cells
following percutaneous coronary intervention. Inhibition of mTOR by
rapamycin, has been revealed to repress the activity of vascular
endothelial cell growth factor (VEGF) by inhibiting VEGF signal
transduction and synthesis (35).
Notably, VEGF is a crucial modulator for endothelial cell migration
and angiogenesis (36). Barilli
et al (37) demonstrated that
rapamycin could damage cell viability and reduce migration of human
endothelial cells through inhibition of mTOR complex 2 (mTORC2). A
previous study by Zhu et al (38) indicated that rapamycin inhibits
proliferation and migration of human vascular SMCs, preventing
arteriovenous grafts in hemodialysis patients. The present study
demonstrated that the effects of rapamycin on the biological
behaviors of human VM endothelial cells were concentration- and
time-dependent. Similarly, rapamycin has been demonstrated in an
in vitro study to suppress the migration and promote the
apoptosis of aortic endothelial cells in rats in a time- and
dose-dependent manner (39).
Rapamycin has been reported to decrease further expansion of VMs in
mouse models, and ameliorate such symptoms and signs as pain,
lesion size, bleeding and functional impairment in patients with
VMs (40).
Altogether, evidence has been provided in this
current study to suggest that rapamycin inhibits the proliferation
and migration of human VM endothelial cells and accelerates their
apoptosis. Furthermore, the effects of rapamycin exerted on human
VM endothelial cells were concentration-dependent. However, the use
of rapamycin may have adverse effects; therefore, further studies
are required to investigate the safety and risk factors presented
by the use of rapamycin in the treatment of VM.
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
HJ and YS conceived of the study, designed the
study, and wrote and reviewed the manuscript. YS designed the
study. HC, RX and WZ acquired the data. TX, XS and YF analyzed and
interpreted the data. HJ supervised the study.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Affiliated Stomatological Hospital of Nanjing Medical University
and written informed consent was obtained from each subject.
Patient consent for publication
Written informed consent was obtained from each
subject.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Boscolo E, Limaye N, Huang L, Kang KT,
Soblet J, Uebelhoer M, Mendola A, Natynki M, Seront E, Dupont S, et
al: Rapamycin improves TIE2-mutated venous malformation in murine
model and human subjects. J Clin Invest. 125:3491–3504. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jia Y, Jia J and Zhao Y:
Pingyangmycin-regulated expressions of adhesion molecules in human
venous malformation endothelial cells. J Huazhong Univ Sci
Technolog Med. 32:760–766. 2012. View Article : Google Scholar
|
|
3
|
Zheng JW, Mai HM, Zhang L, Wang YA, Fan
XD, Su LX, Qin ZP, Yang YW, Jiang YH, Zhao YF and Suen JY:
Guidelines for the treatment of head and neck venous malformations.
Int J Clin Exp Med. 6:377–389. 2013.PubMed/NCBI
|
|
4
|
Wang Y, Qi F and Gu J: Endothelial cell
culture of intramuscular venous malformation and its invasive
behavior related to matrix metalloproteinase-9. Plast Reconstr
Surg. 123:1419–1430. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Buckmiller LM, Richter GT and Suen JY:
Diagnosis and management of hemangiomas and vascular malformations
of the head and neck. Oral Dis. 16:405–418. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Legiehn GM and Heran MK: Venous
malformations: Classification, development, diagnosis, and
interventional radiologic management. Radiol Clin North Am.
46:545–597, vi. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
McRae MY, Adams S, Pereira J, Parsi K and
Wargon O: Venous malformations: Clinical course and management of
vascular birthmark clinic cases. Australas J Dermatol. 54:22–30.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dompmartin A, Vikkula M and Boon LM:
Venous malformation: Update on aetiopathogenesis, diagnosis and
management. Phlebology. 25:224–235. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lackner H, Karastaneva A, Schwinger W,
Benesch M, Sovinz P, Seidel M, Sperl D, Lanz S, Haxhija E, Reiterer
F, et al: Sirolimus for the treatment of children with various
complicated vascular anomalies. Eur J Pediatr. 174:1579–1584. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Glade RS, Richter GT, James CA, Suen JY
and Buckmiller LM: Diagnosis and management of pediatric
cervicofacial venous malformations: Retrospective review from a
vascular anomalies center. Laryngoscope. 120:229–235.
2010.PubMed/NCBI
|
|
11
|
Lee AB, Laredo J and Neville R:
Embryological background of truncular venous malformation in the
extracranial venous pathways as the cause of chronic cerebro spinal
venous insufficiency. Int Angiol. 29:95–108. 2010.PubMed/NCBI
|
|
12
|
Malagelada C, Jin ZH, Jackson-Lewis V,
Przedborski S and Greene LA: Rapamycin protects against neuron
death in in vitro and in vivo models of Parkinson's disease. The J
Neurosci. 30:1166–1175. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shafer A, Zhou C, Gehrig PA, Boggess JF
and Bae-Jump VL: Rapamycin potentiates the effects of paclitaxel in
endometrial cancer cells through inhibition of cell proliferation
and induction of apoptosis. Int J Cancer. 126:1144–1154.
2010.PubMed/NCBI
|
|
14
|
Zhao S, Huang D, Qi H, Wen J and Jia X:
Comparative metabolic profiling-based improvement of rapamycin
production by Streptomyces hygroscopicus. Appl Microbiol
Biotechnol. 97:5329–5341. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huber TB, Walz G and Kuehn EW: mTOR and
rapamycin in the kidney: Signaling and therapeutic implications
beyond immunosuppression. Kidney Int. 79:502–511. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Nichols LA, Adang LA and Kedes DH:
Rapamycin blocks production of KSHV/HHV8: Insights into the
anti-tumor activity of an immunosuppressant drug. PLoS One.
6:e145352011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Su W, Li Z, Jia Y and Zhuo Y: Rapamycin is
neuroprotective in a rat chronic hypertensive glaucoma model. PLoS
One. 9:e997192014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lamming DW, Ye L, Katajisto P, Goncalves
MD, Saitoh M, Stevens DM, Davis JG, Salmon AB, Richardson A, Ahima
RS, et al: Rapamycin-induced insulin resistance is mediated by
mTORC2 loss and uncoupled from longevity. Science. 335:1638–1643.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zheng N, Ding X and Jahan R: Low
concentration of rapamycin inhibits hemangioma endothelial cell
proliferation, migration, and vascular tumor formation in mice.
Curr Ther Res Clin Exp. 76:99–103. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wallez Y and Huber P: Endothelial adherens
and tight junctions in vascular homeostasis, inflammation and
angiogenesis. Biochim Biophys Acta. 1778:794–809. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
DiStefano PV, Kuebel JM, Sarelius IH and
Glading AJ: KRIT1 protein depletion modifies endothelial cell
behavior via increased vascular endothelial growth factor (VEGF)
signaling. J Biol Chem. 289:33054–33065. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Richter GT and Friedman AB: Hemangiomas
and vascular malformations: Current theory and management. Int J
Pediatr. 2012:6456782012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sarbassov DD, Ali SM, Sengupta S, Sheen
JH, Hsu PP, Bagley AF, Markhard AL and Sabatini DM: Prolonged
rapamycin treatment inhibits mTORC2 assembly and Akt/PKB. Mol Cell.
22:159–168. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Guba M, von Breitenbuch P, Steinbauer M,
Koehl G, Flegel S, Hornung M, Bruns CJ, Zuelke C, Farkas S,
Anthuber M, et al: Rapamycin inhibits primary and metastatic tumor
growth by antiangiogenesis: Involvement of vascular endothelial
growth factor. Nat Med. 8:128–135. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gluhovschi C, Gluhovschi G, Potencz E,
Herman D, Trandafirescu V, Petrica L, Velciov S, Bozdog G, Bob F,
Vernic C and Cioca D: The endothelial cell markers von Willebrand
factor (vWF), CD31 and CD34 are lost in glomerulonephritis and no
longer correlate with the morphological indices of glomerular
sclerosis, interstitial fibrosis, activity and chronicity. Folia
Histochem Cytobiol. 48:230–236. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mohamed AS, Thomson J, McDonald KJ,
Hillyard DZ, Mark PB, Elliott HL and Jardine AG: Circulating
endothelial cells in renal transplant recipients. Transpl Proc.
37:2387–2390. 2005. View Article : Google Scholar
|
|
27
|
Humar R, Kiefer FN, Berns H, Resink TJ and
Battegay EJ: Hypoxia enhances vascular cell proliferation and
angiogenesis in vitro via rapamycin (mTOR)-dependent signaling.
FASEB J. 16:771–780. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Marqués L, Núñez-Córdoba JM, Aguado L,
Pretel M, Boixeda P, Nagore E, Baselga E and Redondo P: Topical
rapamycin combined with pulsed dye laser in the treatment of
capillary vascular malformations in Sturge-Weber syndrome: Phase
II, randomized, double-blind, intraindividual placebo-controlled
clinical trial. J Am Acad Dermatol. 72:151–158.e1. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhou C, Gehrig PA, Whang YE and Boggess
JF: Rapamycin inhibits telomerase activity by decreasing the hTERT
mRNA level in endometrial cancer cells. Mol Cancer Ther. 2:789–795.
2003.PubMed/NCBI
|
|
30
|
Nadal M, Giraudeau B, Tavernier E,
Jonville-Bera AP, Lorette G and Maruani A: Efficacy and safety of
mammalian target of rapamycin inhibitors in vascular anomalies: A
systematic review. Acta Derm Venereol. 96:448–452. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Shin S, Wolgamott L, Yu Y, Blenis J and
Yoon SO: Glycogen synthase kinase (GSK)-3 promotes p70 ribosomal
protein S6 kinase (p70S6K) activity and cell proliferation. Proc
Natl Acad Sci USA. 108:E1204–E1213. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wilkinson JE, Burmeister L, Brooks SV,
Chan CC, Friedline S, Harrison DE, Hejtmancik JF, Nadon N, Strong
R, Wood LK, et al: Rapamycin slows aging in mice. Aging Cell.
11:675–682. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Visner GA, Lu F, Zhou H, Liu J, Kazemfar K
and Agarwal A: Rapamycin induces heme oxygenase-1 in human
pulmonary vascular cells: Implications in the antiproliferative
response to rapamycin. Circulation. 107:911–916. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Liu HT, Li F, Wang WY, Li XJ, Liu YM, Wang
RA, Guo WY and Wang HC: Rapamycin inhibits re-endothelialization
after percutaneous coronary intervention by impeding the
proliferation and migration of endothelial cells and inducing
apoptosis of endothelial progenitor cells. Tex Heart Inst J.
37:194–201. 2010.PubMed/NCBI
|
|
35
|
Moss SC, Lightell DJ Jr, Marx SO, Marks AR
and Woods TC: Rapamycin regulates endothelial cell migration
through regulation of the cyclin-dependent kinase inhibitor
p27Kip1. J Biol Chem. 285:11991–11997. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Shirazi F, Cohen C, Fried L and Arbiser
JL: Mammalian target of rapamycin (mTOR) is activated in cutaneous
vascular malformations in vivo. Lymphat Res Biol. 5:233–236. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Barilli A, Visigalli R, Sala R, Gazzola
GC, Parolari A, Tremoli E, Bonomini S, Simon A, Closs EI, Dall'Asta
V and Bussolati O: In human endothelial cells rapamycin causes
mTORC2 inhibition and impairs cell viability and function.
Cardiovasc Res. 78:563–571. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhu W, Masaki T, Cheung AK and Kern SE:
In-vitro release of rapamycin from a thermosensitive polymer for
the inhibition of vascular smooth muscle cell proliferation. J
Bioequiv Availab. 1:3–12. 2009.PubMed/NCBI
|
|
39
|
Guo N, Chen F, Zhou J, Fang Y, Li H, Luo Y
and Zhang Y: Curcumin attenuates rapamycin-induced cell injury of
vascular endothelial cells. J Cardiovasc Pharmacol. 66:338–346.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Laurian C, Diner P, Enjolras O,
LeMarchand-Venencie F, Herbreteau D and Merland JJ: Surgical
treatment of superficial vascular malformations. Indications for
tissue expansion. J Des Maladies Vasculaires. 21:31–35. 1996.(In
French).
|