Introduction
As a clinical comprehensive disease with a change of
the cardiac function aroused by various factors, heart failure (HF,
mainly refers to the failure of the heart muscle), generally has
such clinical symptoms as tachypnea, dyspnea, cyanosis,
tachycardia, and frothy sputum (1).
Causes of HF are manifold, including myocardial overwork,
cardiovascular and cerebrovascular diseases, autoimmune diseases,
and sudden decrease of cardiac output caused by immune system
diseases, a decreased ventricular pumping function or myocardial
contractile function (2). In recent
years, the morbidity of HF is ever-increasing, with elderly people
occupying a large proportion of the patients. Characterized by high
mortality, high morbidity, and high repeated hospitalization rate
(3), HF has become the main killer
of elderly patients with chronic diseases (4). Without a timely and effective treatment
and with the ever-worsening condition, patients with HF are
vulnerable to repeated hospitalization and changed heart structure,
thus suffering from severe HF which has higher mortality and is
much harder to cure (5). According
to statistics, more than 26 million people in the world have been
diagnosed with HF, approximately 54.35% of whom have died within 4
years after diagnosis (6). The
common pathogenesis is often related to endocrine disorders,
abnormal systemic circulatory function, and myocardial dysfunction
(7). Routine emergency treatment of
this tricky severe HF using diuretics, invasive oxygen supply,
cardiotonic (8) generally brings
poor efficacy.
As a β-blocker, recently metoprolol has been found
to be beneficial in relief of HF by relieving the symptoms of the
drug users since it can indirectly inhibit the renin-angiotensin
system, dilate peripheral blood vessels, significantly reduce
water-sodium retention (9), reduce
myocardial injury aroused by excessive myocardial calcium ion,
lower blood pressure through stabling heart rate and reducing
cardiac output (10). Irbesartan is
an angiotensin-II receptor blocker that reduces the preload and
afterload of the heart and effectively dilates the blood vessels
(11). Hydrochlorothiazide is a
diuretic that activates the sympathetic nervous system and the
renin-angiotensin system and increases the renin activity in blood
generally (12), which when combined
with irbesartan that can eliminate diuretic-induced hypokalemia,
can better activate renin-angiotensin activity, improve drug safety
and reduce adverse reactions (13).
Brain natriuretic peptide (BNP), often used as a quantitative
marker for HF in clinical practice, is a peptide hormone mainly
produced in the ventricle and has active amino acid fragments
(14). The occurrence, development,
severity of symptoms and prognosis of HF are directly related to
BNP. The higher the BNP, the more severe the symptoms. Studies
showed that metoprolol combined with irbesartan and
hydrochlorothiazide can reduce BNP and improve cardiac functions in
HF patients (15).
Mechanical ventilation can be divided into
non-invasive ventilation and invasive which are currently very
effective in treating dyspnea, a common symptom of HF patients
(16). Invasive ventilation refers
to the method of assisting breathing through a tracheal intubation
or tracheotomy connected to a Continuous Positive Airway Pressure;
while noninvasive ventilation (NIV) refers to the use of a
Continuous Positive Airway Pressure through a nasal mask to achieve
positive pressure ventilation and increase alveolar ventilation
without tracheal intubation (17).
After repeated research worldwide, the safety, efficacy and
economic practicability of NIV have been confirmed because it
reduce the possibility of concurrent infection and adverse
reactions caused by invasive mechanical ventilation, and improve
long-term prognosis (18).
Continuous Positive Airway Pressure is commonly used in the
treatment of patients with sleep apnea syndrome and pulmonary
respiratory failure, and shows good results. With the advancement
of science and technology, the continuously improved NIV technology
has gradually gained much attention from cardiologists as
non-invasive ventilator can effectively reduce the heart preload,
correct hypoxemia and acidosis, promote the efficacy of anti-heart
failure drugs, and prevent cardiac-respiratory arrest caused by
hypoxia (19,20).
There is an urgent need to find a safer and more
effective severe HF emergency treatment plan, considering the
yearly-increasing incident cases and the unsatisfactory current
treatment. To this end, this study explored the clinical efficacy
of metoprolol combined with irbesartan and hydrochlorothiazide and
non-invasive ventilator in the emergency treatment of patients with
severe HF, looking for a safe and effective severe HF emergency
treatment plan, providing a further scientific basis for the
clinical use.
Patients and methods
Clinical baseline data
This study retrospectively analyzed the medical
records of 124 patients with severe HF admitted to the Emergency
Department of Binzhou Medical University Hospital (Binzhou, China)
from May 2012 to August 2016 and who all met the diagnostic
criteria for heart failure. Among them, 78 patients treated with
metoprolol combined with irbesartan and hydrochlorothiazide and
non-invasive ventilator for emergency treatment were enrolled into
the Research Group, including 41 male patients and 37 female
patients with an average age of 71.34±5.26, while the Control
Group, consisted of 46 patients (26 men and 20 women) treated with
routine medical treatment in the emergency depart, with an average
age of 70.41±6.39. The study was conducted after approval by the
Medical Ethics Committee of Binzhou Medical University Hospital.
Written informed consent was obtained from patients and their
families.
Criteria for inclusion and
exclusion
Inclusion criteria: age >60 years; left
ventricular ejection fractions (LVEF) ≤0.35; enlargement of left
ventricular showed by echocardiography; graded NYHA cardiac
function as Level 4 and above; intact structure of upper
respiratory tract without excessive respiratory secretion; stable
hemodynamics.
Exclusion criteria: those who were allergic to drugs
used in this study such as metoprolol, irbesartan or
hydrochlorothiazide; those with severe angina pectoris, myocardial
infarction or liver and kidney dysfunction; those with systolic
blood pressure <90 mmHg; those with malignant tumors; those
uncooperative with the treatment; those with serious
infections.
Emergency treatment plan for the
Research Group
Patients in the Research Group adopted a low-sodium
diet, strictly controlled amount of drinking water, and enough rest
during the treatment. Patients were treated with metoprolol
(manufacturer: AstraZeneca plc., code number of medical product
approved by SFDA: medical product approved by SFDA H32025391)
combined with irbesartan and hydrochlorothiazide (manufacturer:
Zhejiang Huahai Pharmaceutical Co., Ltd., Zhejiang, China; code
number of medical product approved by SFDA: medical product
approved by SFDA H20058709) and non-invasive ventilator
(manufacturer: Respironics Inc; product model: BiPAP-Vision) for
emergency treatment. Patients took orally metoprolol 25 mg/day,
twice a day, irbesartan and hydrochlorothiazide (150 mg for
irbesartan/ and 12.50 mg for hydrochlorothiazide)/day, twice a day.
The Research Group used the non-invasive ventilator with the S/T
mode and automatic parameter setting. Oxygen was directly connected
to the mask which was in close contact with the patient's face to
avoid oxygen leakage. The inspiratory positive airway pressure and
the expiratory positive airway pressure were set separately with an
initial auxiliary ratio of 85%. According to the relief of the
patient's breathing difficulties, the auxiliary ratio was gradually
reduced to 70, 50, and 30%. The positive airway pressure of the
expiratory term was set to 5–6 cm H2O; the positive
airway pressure of the inspiratory item was set to 6 cm
H2O, and the initial oxygen concentration was 100%. The
NIV time was extended as much as possible until the patient's
breathing difficulties were significantly relieved, then the
ventilation time was gradually shortened, and the ventilation
pressure was reduced until offline. One week was a course of
treatment.
Emergency treatment plan for the
Control Group
The Control Group was guaranteed a low-sodium diet,
strictly controlled amount of drinking water, and enough rest
during treatment. Patients were prescribed to take orally
furosemide tablets (manufacturer: Dongbei Pharmaceutical Group
Company Shenyang No. 1 Pharmaceutical Co., Ltd., Shenyang, China;
code number of medical product approved by SFDA: medical product
approved by SFDA H21022890) 40 mg/day, twice a day; to take
nitroglycerin through sublingual administration (manufacturer:
Beijing Yimin Pharmaceutical Plant, Beijing, China; code number of
medical product approved by SFDA: medical product approved by SFDA
H11021022) 0.25–0.5 mg/time (can be re-administered once after 5
min), 1–2 times a day; to take intravenous infusion of sodium
nitroprusside (light avoided) (manufacturer: Henan Wanxi
Pharmaceutical Co., Ltd., Henan, China; code number of medical
product approved by SFDA: medical product approved by SFDA
H20143166), which was diluted with 5% glucose solution (each
kilogram of the patients' weight required 30 µg/min, 12 h/day). One
week was a course of treatment.
Detection indicators
Echocardiography
After admitted to the emergency department of
internal medicine, the patients were examined by Color Doppler
Echocardiography (manufacturer: Hewlett-Packard Co., Palo Alto, CA,
USA, model: HP77020Ac). All patients were treated with the same
Doppler ultrasound system and the same doctor performed the
examination. Cardiac index (CI), stroke volume (SV), cardiac output
(CO), and fractional shortening (FS) were recorded before and after
treatment.
LVEF
LVEF is the percentage of stroke volume to the
ventri-cular end-diastolic volume. The volume of ventricular
diastolic is approximately 145 ml in the left ventricle,
approximately 138 ml in the right ventricle, and the SV is
approximately 60–80 ml. Cardiac color Doppler examination is an
important indicator for diagnosing HF. Under normal circumstances,
LVEF ≥0.5, right ventricular ejection fraction ≥0.4, the results
less than normal scores can prove cardiac dysfunction.
Six-minute walk experiment
The experiment was a test for the motor function
status of patients with moderate to severe HF (21), which examined the motion state of
patients from both the Research and Control Groups before the
treatment, 1 day after the treatment, and 7 days after the
treatment. The test site was an unimpeded corridor with one chair
placed every 15 meters for the patients to rest halfway. The
patients were told to walk as far as possible within the prescribed
site to record the longest distance the patients walked within 6
min. During the walking, verbal encouragements such as ‘well done,
please go on’ were delivered every fixed time. Break during the
walk was allowed, but moving on after physical recovery was
strongly required.
Examination of BNP
BNP content in the serum is an important indicator
for assessing cardiac function. The more severe the HF is, the
higher the BNP expression level in the serum is. Blood samples
taken from the elbow venous of all patients before the treatment, 1
day after the treatment, and 7 days after the treatment were sent
to the professional inspectors in the laboratory of the hospital.
The test method was enzyme-linked immunosorbent assay, the kits
were from Hangzhou Zheda Dixun Biological Gene Engineering Co.,
Ltd. (Hangzhou, China) with a product code of 59400364827.
Judging criteria of the efficacy of
emergency treatment
Effective: After the emergency treatment, the
symptoms of HF patients were relieved. The BNP expression level
decreased, and the LVEF score increased. Ineffective: After the
emergency treatment, the symptoms of HF patients were not relieved
or even aggravated, and the cardiac function was unchanged or
worsened.
Grading criteria of cardiac
function
According to the degree of activity of the HF
patients, the impairment of cardiac function was divided into 4
levels, as shown in Table I.
 | Table I.Grading criteria of cardiac
function. |
Table I.
Grading criteria of cardiac
function.
| Levels | Degree of activity of
HF patients |
|---|
| Level 1 | The patients have
heart disease, but the amount of daily activities is not
limited. |
|
| General physical
activities do not cause excessive fatigue, palpitations, asthma or
angina. |
| Level 2 | Physical activities
in patients with heart disease are slightly limited. No
self-consciousness at rest. |
|
| General physical
activities can cause excessive fatigue, palpitations, asthma or
angina. |
| Level 3 | The patients have
heart disease, so physical activities are significantly
limited. |
|
| Asymptomatic at rest,
but activities with lower labor intensity than general |
|
| physical activities
can cause excessive fatigue, palpitations, asthma or angina. |
| Level 4 | Patients with heart
disease can not engage in any physical activity, and symptoms |
|
| of heart failure
occur at rest, which is aggravated after physical activities. |
Results
Comparison between the clinical
baseline data of two groups
According to the comparison between the two groups
in terms of age, sex, body mass index (BMI), LVEF, blood glucose,
heart rate, systolic blood pressure, diastolic blood pressure, mean
arterial pressure, CI, SV, FS and CO, no statistical difference was
shown between the two groups (P>0.05) (Table II).
 | Table II.Comparison of the clinical baseline
data between the Research Group and Control Group [n (%)] (mean ±
SD). |
Table II.
Comparison of the clinical baseline
data between the Research Group and Control Group [n (%)] (mean ±
SD).
| Terms | The Research Group
(n=78) | The Control Group
(n=46) | χ2/t
value | P-value |
|---|
| Age (year) |
|
| 0.253 | 0.708 |
| ≤70 | 32 | 21 |
|
|
|
>70 | 46 | 25 |
|
|
| Sex |
|
| 0.182 | 0.712 |
|
Male | 41 | 26 |
|
|
|
Female | 37 | 20 |
|
|
| BMI
(kg/m2) |
|
| 0.308 | 0.683 |
|
<24 | 24 | 14 |
|
|
|
≥24 | 54 | 32 |
|
|
| LVEF |
|
| 0.976 | 0.424 |
|
≤0.30 | 51 | 34 |
|
|
|
>0.30 | 27 | 12 |
|
|
| Blood glucose
(mmol/l) |
|
| 0.150 | 0.712 |
| ≤8 | 35 | 19 |
|
|
|
>8 | 43 | 27 |
|
|
| Heart rate
(bpm) | 123.13±14.24 | 125.34±12.24 | 0.878 | 0.382 |
| Systolic blood
pressure (mmHg) | 156.34±12.34 | 157.43±13.21 | 0.463 | 0.644 |
| Diastolic blood
pressure (mmHg) | 88.32±4.25 | 86.68±6.31 | 1.727 | 0.087 |
| Mean arterial
pressure (mmHg) | 132.32±7.43 | 134.53±7.43 | 1.600 | 0.112 |
| CI
(l/min/m2) | 1.85±0.44 | 1.92±0.31 | 1.084 | 0.281 |
| SV (ml) | 37.31±5.33 | 35.78±6.88 | 1.383 | 0.169 |
| FS (%) | 16.43±6.29 | 17.11±5.32 | 0.615 | 0.540 |
| CO (l/min) | 1.35±0.28 | 1.40±0.23 | 1.024 | 0.308 |
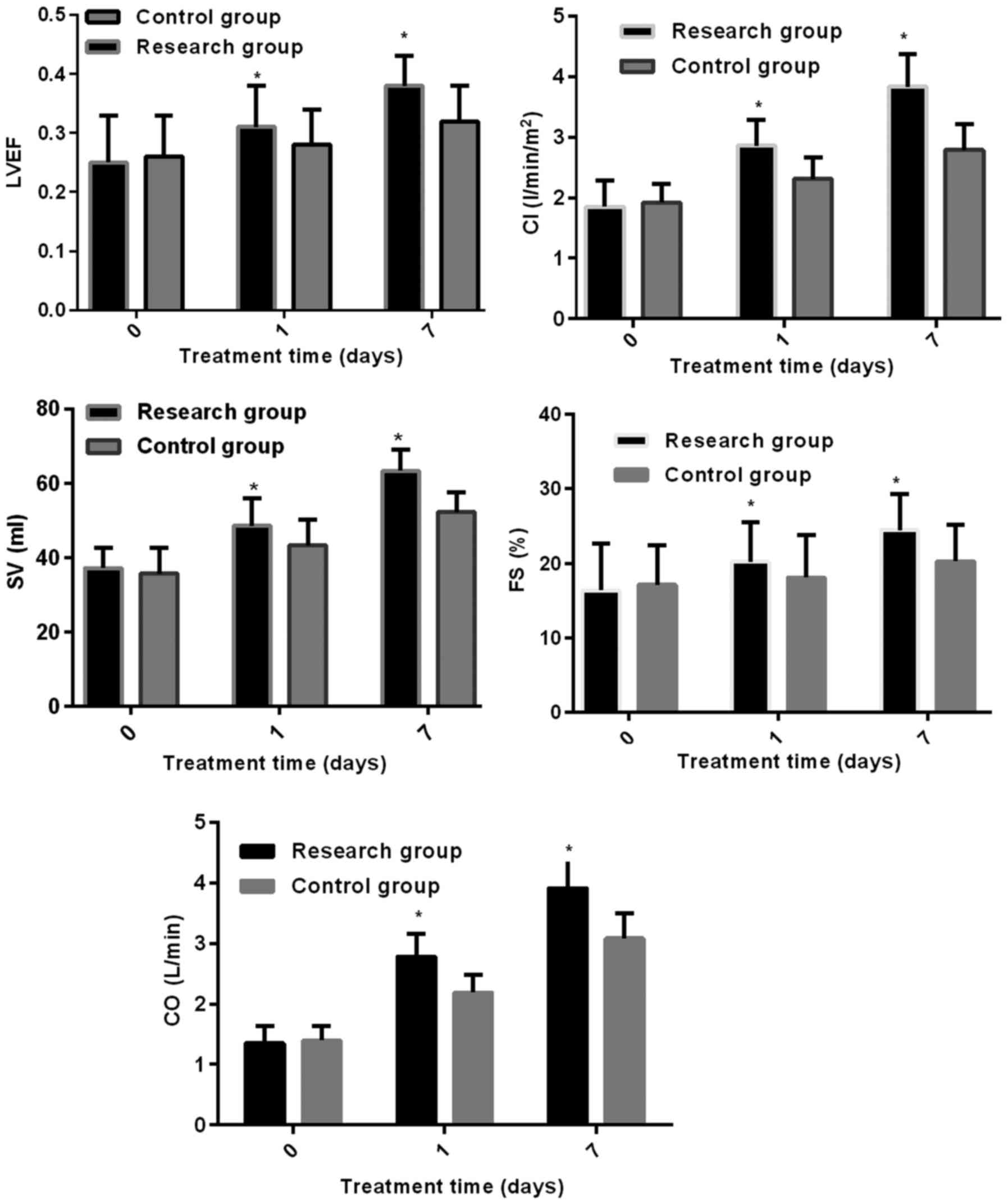
Changes of echocardiography test
results after the emergency treatment
After 7 days of the emergency treatment, the indexes
of echocardiography of the Research and Control Groups were
increased to different degrees. Statistical difference was
indicated between the two groups in terms of LVEF as the LVEF of
the Research Group was 0.31±0.07 on the 1st and 0.38±0.05 on the
7th day after the emergency treatment, higher than that of the
Control Group (0.28±0.06) on the 1st and 7th day (0.32±0.06) after
the emergency treatment (P<0.05). Statistical difference existed
between the two groups since the CI results of the Research Group
on the 1st and 7th day after treatment were 2.86±0.42
l/min/m2, 3.83±0.54 l/min/m2 respectively,
which were higher than those of the Control Group on the 1st
(2.31±0.36 l/min/m2) and 7th day (2.79±0.42
l/min/m2) after the emergency treatment (P<0.05). The
two groups proved to be statistically different by the results that
the SV of the Research Group 1 and 7 days after the emergency
treatment was 48.65±7.43 ml, and 63.43±5.67 ml, respectively,
higher than 43.35±6.95 ml on the 1st day and 52.35±5.42 ml on the
7th day after treatment of the Control Group (P<0.05). The FS of
the Research Group 1 and 7 days after the emergency treatment was
20.21±5.32%, and 24.45±4.79%, respectively, higher than 18.11±5.67%
on the 1st day and 20.30±4.93% on the 7th day after treatment of
the Control Group (P<0.05). The CO of the Research Group 1 and 7
days after the emergency treatment was 2.78±0.37 l/min, and
3.91±0.47 l/min, respectively, higher than 2.19±0.29 l/min on the
1st day and 3.08±0.42 l/min on the 7th day after treatment of the
Control Group (P<0.05) (Fig.
1).
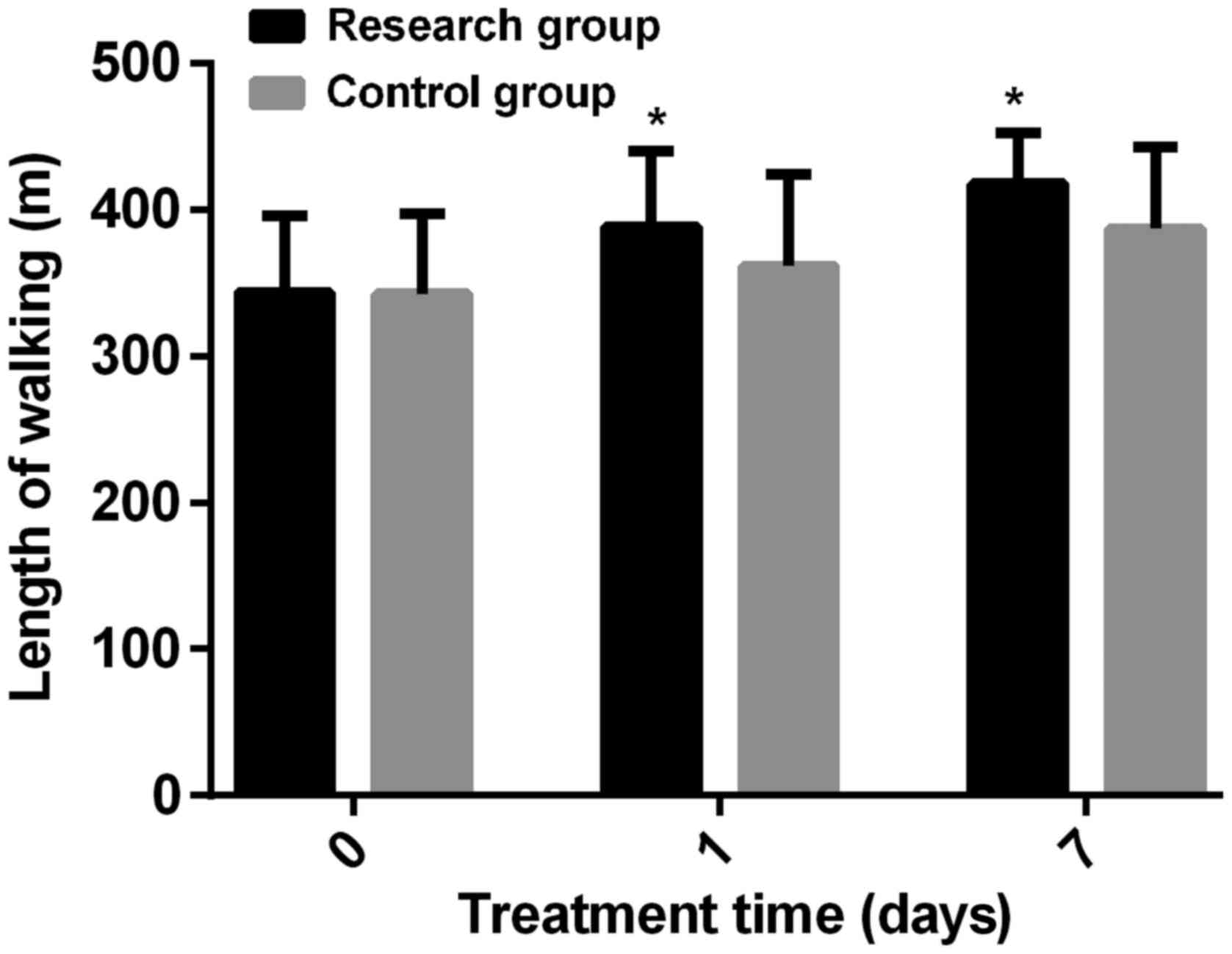
Comparison of the 6-minute walking
test of the two groups before and after the emergency
treatment
No statistical difference in terms of the 6-minute
walk test before emergency treatment between the two groups was
seen since the test result of the Study Group was 343.35±52.57
meters and the Regular Group was 342.88±54.43 meters before the
emergency treatment (t=0.047, P=0.962), while after the seven-day
long emergency treatment, the length of walking of the Study Group
1 day after the emergency treatment was 388.45±65.39 meters, longer
than the 361.45±62.91 meters of the Regular Group (t=2.252,
P=0.026). The length of walking of the Study Group 7 days after the
emergency treatment was 417.56±48.94 meters, longer than the
386.71±55.83 meters of the Regular Group (t=3.217, P=0.002)
(Fig. 2).
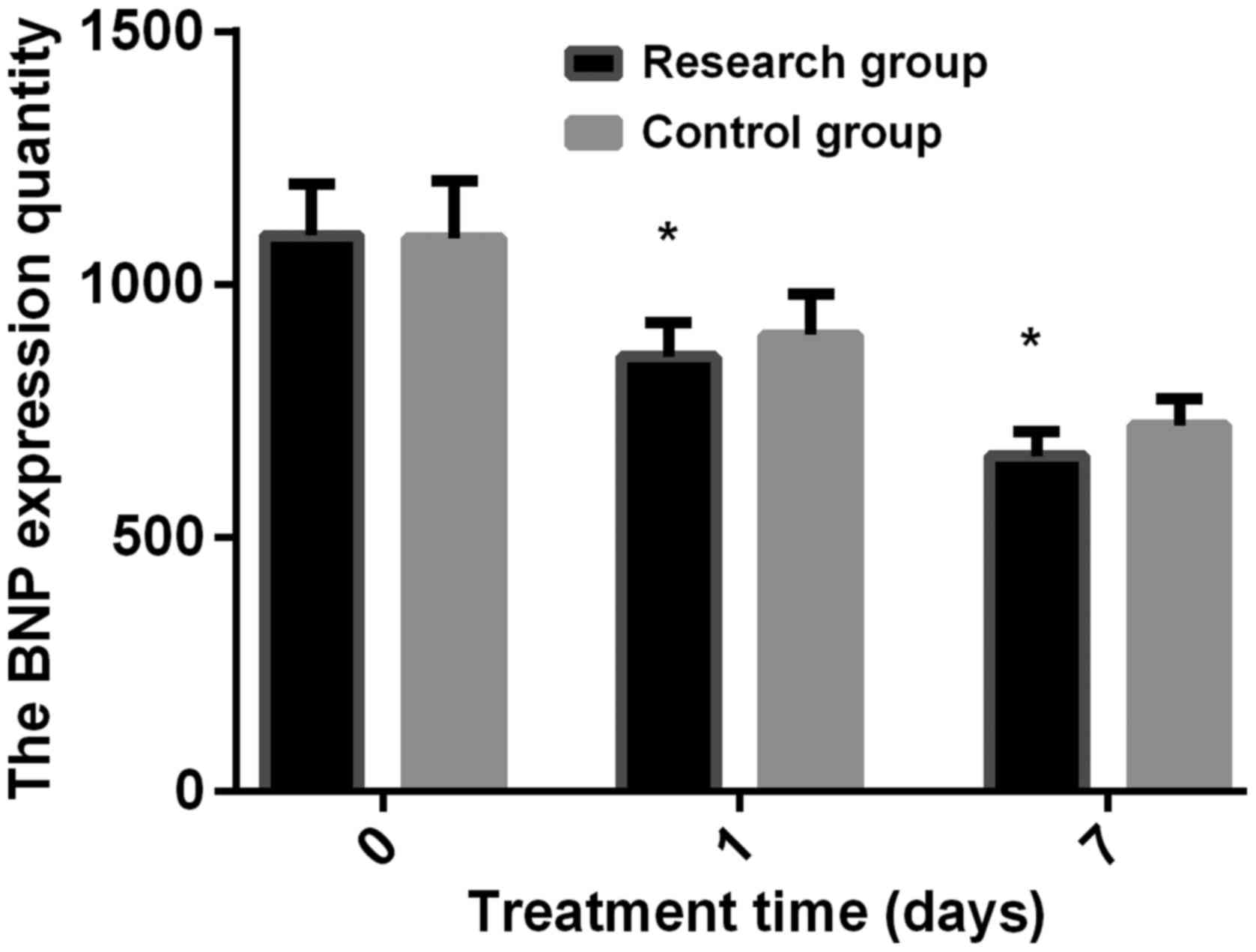
Changes of the serum BNP expression
level of the two groups before and after the emergency
treatment
No statistical difference in terms of the BNP
expression level before the emergency treatment between the two
groups was detected since the BNP expression of the Study Group was
1096.43±103.53, similar to 1091.54±112.42 of the Regular Group
(t=0.246, P=0.806). After seven days of the emergency treatment,
the BNP expression of the Research Group was 857.53±67.61 1 day
after the emergency treatment, lower than the 900.53±79.82 of the
Control Group (t=3.197, P=0.018). The BNP expression of the
Research Group was 662.34±46.78, 7 days after the emergency
treatment, lower than the 721.55±52.83 of the Control Group
(t=6.487, P<0.001) (Fig. 3).
The efficacy of emergency treatment and comparison
of cardiac function grading between the two groups after the
emergency treatment. After a 7-day emergency treatment, the
efficiency rate of treatment of the Research Group was 94.87%,
higher than that of the Control Group (80.43%)
(χ2=6.426, P=0.016), which explained why 2 patients from
the Research Group and no patient from the Control Group were
graded as Level 1 in terms of the heart function (no difference
between the two groups, χ2=1.199, P=0.530). In addition,
23 patients from the Research Group and 6 patients from the Control
Group were graded as Level 2 (χ2=4.367, P=0.048), while
42 patients from the Research Group and 16 patients from the
Control Group were graded as Level 3 (P<0.05,
χ2=4.367, P=0.048). Finally, 11 patients from the
Research Group and 24 patients from the Control Group were graded
as Level 4 (χ2=20.702, P<0.001) (Table III).
 | Table III.The efficacy of emergency treatment
and comparison of cardiac function grading between the two groups
after the emergency treatment. |
Table III.
The efficacy of emergency treatment
and comparison of cardiac function grading between the two groups
after the emergency treatment.
| Terms | The Research Group
(n=78) | The Control Group
(n=46) | χ2
value | P-value |
|---|
| Efficacy |
|
|
6.426 | 0.016 |
|
Effective | 74 (94.87) | 37 (80.43) |
|
|
|
Ineffective | 4 (5.13) | 9
(19.57) |
|
|
| Cardiac function
grades |
| 1 | 2 (2.56) | 0 (0.00) |
1.199 | 0.530 |
| 2 | 23 (29.49) | 6
(13.04) |
4.367 | 0.048 |
| 3 | 42 (53.85) | 16 (34.78) |
4.224 | 0.043 |
| 4 | 11 (14.10) | 24 (52.17) | 20.702 | <0.001 |
Discussion
HF is a common internal medical disease manifesting
as ventricular filling and impaired ejection ability with the
complication of obstructive pulmonary disease, caused by a variety
of factors, such as autoimmune diseases, tumors, cardiogenic
diseases and metabolic diseases (22). HF has a gradually increasing
mortality as the patients get older, becoming an important reason
for the abnormal death of the elderly in the contemporary era. The
disease of HF has sudden and severe symptoms and rapid development
to destroy the cardiac function to produce enough cardiac output to
meet the daily metabolic needs of the body, and easily turn into
severe HF without timely treatment (23), which has extremely high mortality and
poor prognosis, leading to an average survival time of less than 5
years (24). Emergency treatment is
an important part of severe HF rescue treatment, so active and
effective emergency treatment is the key to improve the prognosis,
improve the survival rate of patients with severe HF, and improve
the patients' quality of life (25).
Studies have pointed out that when patients suffered
from heart failure, noradrenergic nerves in the body would be
over-activated, causing necrosis and apoptosis of cardiomyocytes
directly through cytotoxicity, promoting hypertrophy of cardiac
fibroblasts, leading to myocardial fibrosis and abnormal
hypertrophy (26). β-blockers can
effectively block the excessive activation of the noradrenergic
nervous system, improve cardiac function in patients with severe
HF, and block ventricular remodeling (27). In patients with severe HF, pulmonary
compliance is weakened, resulting in increased airway resistance
and dysfunction in ventilation. Clinically, sudden dyspnea and
cyanosis are common for patients with severe HF, and can be
life-threatening in severe cases. The method of mechanical
ventilation is often used in the clinical emergency treatment of
severe HF patients as it can help patients breath, increase
inspiratory volume, increase myocardial oxygen supply, reduce
cardiac burden, improve oxygenation (28). Compared with traditional invasive
mechanical ventilation, NIV has advantages of no need to open the
trachea of severe HF patients, no need for intubation, eliminating
the corresponding serious complications, decreasing tracheal loss,
and reducing medical expenses (29).
The study made by Kuhn et al (30) found that NIV achieved good results in
the emergency treatment of patients with acute left heart failure
and contributed to the recovery of patients. Irbesartan is a
powerful angiotensin-II receptor blocker, and hydrochlorothiazide a
common diuretic, and the combination of the two is a common
compound preparation for the treatment of essential hypertension,
beneficial to activating sympathetic nerve and renin-angiotensin,
inhibiting the decline of serum potassium level, improving
medication safety, and reducing adverse reactions (31). A study (32) showed that irbesartan and
hydrochlorothiazide combined with conventional medication for
severe HF could effectively reduce the adverse reactions and
recurrence rate, and promise high safety. As commonly used drugs in
severe HF, irbesartan and hydrochlorothiazide do not show good
clinical efficacy to improve the symptoms of patients. Chrysant
et al (33) found that
irbesartan and hydrochlorothiazide combined with metoprolol in the
treatment of chronic elderly patients with HF could significantly
improve the efficacy and cardiac function, which agrees with our
study results that metoprolol combined with and irbesartan and
hydrochlorothiazide and non-invasive ventilator had a good effect
in the emergency treatment of patients with severe HF, conducive to
the recovery of cardiac function, the relief of the patient's
breathing difficulties and the reduction of the preload and
afterload of the heart.
The results of the experiment showed no obvious
difference between the echocardiographic indexes of the Research
Group and the Control Group (P>0.05), but after the emergency
treatment, the echocardiographic indexes of both groups were
increased to different degrees, with the LVEF, CI, SV, FS, and CO
of the echocardiogram of the Research Group on the 1st and 7th day
after the emergency treatment being higher than that of the Control
Group (P<0.05). The results of the experiment indicated that the
emergency treatment using metoprolol and irbesartan and
hydrochlorothiazide combined with non-invasive ventilator helped to
recover normal cardiac function, to increase cardiac output, to
normalize the ventricular ejection of severe HF patients. Before
the emergency treatment, the Research Group and the Control Group
walked similar length within 6 min (P>0.05). After the emergency
treatment, the length of walking in the two groups was extended,
with the walking length of the Research Group on the 1st and 7th
day after emergency treatment being longer than that of the Control
Group (P<0.05), which showed that the use of metoprolol and
irbesartan and hydrochlorothiazide combined with non-invasive
ventilator for emergency treatment of severe HF patients could
quickly restore normal body function and improve clinical symptoms
such as dyspnea in patients with severe HF. The patient has
clinical symptoms such as difficulty in breathing. No difference in
serum BNP expression was detected between the Research and Control
Groups before the emergency treatment (P>0.05). After the
emergency treatment, the BNP expression levels in the two groups
decreased in different degrees, with the BNP expression level of
the Research Group on the 1st and 7th day after the emergency
treatment was lower than that of the Control Group (P<0.05),
showing that the use of metoprolol and irbesartan and
hydrochlorothiazide combined with non-invasive ventilator for the
emergency treatment of severe HF patients could relieve the
symptoms in patients, and bring better prognosis if the severity of
disease development was lower. After the 7-day emergency treatment,
the efficiency rate of treatment of the Research Group was 94.87%,
higher than that of the Control Group (80.43%) (P<0.05), which
explained why 2 patients from the Research Group, but no patient
from the Control Group was graded as Level 1 in terms of the heart
function. In addition, 23 patients from the Research Group and 6
patients from the Control Group were graded as Level 2 (P<0.05),
while 42 patients from the Research Group and 16 patients from the
Control Group were graded as Level 3 (P<0.05). At last, 11
patients from the Research Group and 24 patients from the Control
Group were graded as Level 4 (P<0.05). The results of this study
indicated that the method of using metoprolol and irbesartan and
hydrochlorothiazide combined with non-invasive ventilator for the
emergency treatment of patients with severe HF was more
efficient.
However, a limitation of this study was that the
method of retrospective analysis did not achieve perfection in the
collection of data of clinical and special examinations for
patients, and the limited number of cases admitted was not capable
of offering sufficient data for statistical comparison.
In summary, the method of using metoprolol and
irbesartan and hydrochlorothiazide combined with non-invasive
ventilator in the emergency treatment of severe HF patients proved
to be of high safety and is worth clinical promotion because it was
significantly efficient to help patients with the recovery of
respiratory function, to relieve symptoms in short time and improve
cardiac function.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
FZ, GZ, and LG conceived and designed the study,
compared the 6-minute walking test of the two groups before and
after the emergency treatment and analyzed the echocardiography
result. FL and GZ examined the serum BNP expression level of the
two groups before and after the emergency treatment. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Binzhou Medical University Hospital (Binzhou, China). Patients who
participated in this research had complete clinical data. Signed
written informed consents were obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chang AM, Maisel AS and Hollander JE:
Diagnosis of heart failure. Heart Fail Clin. 5:25–35. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li JD, Cheng AY, Huo YL, Fan J, Zhang YP,
Fang ZQ, Sun HS, Peng W, Zhang JS, Wang HP, et al: Bilateral renal
denervation ameliorates isoproterenol-induced heart failure through
downregulation of the brain renin-angiotensin system and
inflammation in rat. Oxid Med Cell Longev. 2016:35626342016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Díez J: Serelaxin: A novel therapy for
acute heart failure with a range of hemodynamic and non-hemodynamic
actions. Am J Cardiovasc Drugs. 14:275–285. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Valbusa F, Agnoletti D, Scala L, Grillo C,
Arduini P, Bonapace S, Calabria S, Scaturro G, Mantovani A, Zoppini
G, et al: Non-alcoholic fatty liver disease and increased risk of
all-cause mortality in elderly patients admitted for acute heart
failure. Int J Cardiol. 265:162–168. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Davarzani N, Sanders-van Wijk S, Karel J,
Maeder MT, Leibundgut G, Gutmann M, Pfisterer ME, Rickenbacher P,
Peeters R and Brunner-la Rocca HP: N-terminal pro-B-type
natriuretic peptide-guided therapy in chronic heart failure reduces
repeated hospitalizations-results from TIME-CHF. J Card Fail.
23:382–389. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Böhm M, Voors AA, Ketelslegers JM,
Schirmer SH, Turgonyi E, Bramlage P and Zannad F: Biomarkers:
Optimizing treatment guidance in heart failure. Clin Res Cardiol.
100:973–981. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Aikawa T, Naya M, Obara M, Manabe O,
Tomiyama Y, Magota K, Yamada S, Katoh C, Tamaki N and Tsutsui H:
Impaired myocardial sympathetic innervation is associated with
diastolic dysfunction in heart failure with preserved ejection
fraction: 11C-Hydroxyephedrine PET Study. J Nucl Med. 58:784–790.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Qavi AH, Kamal R and Schrier RW: Clinical
use of diuretics in heart failure, cirrhosis, and nephrotic
syndrome. Int J Nephrol. 2015:9759342015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mao Y, Tokudome T and Kishimoto I: Ghrelin
as a treatment for cardiovascular diseases. Hypertension.
64:450–454. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kotecha D, Holmes J, Krum H, Altman DG,
Manzano L, Cleland JG, Lip GY, Coats AJ, Andersson B, Kirchhof P,
et al; Beta-Blockers in Heart Failure Collaborative Group, .
Efficacy of β blockers in patients with heart failure plus atrial
fibrillation: An individual-patient data meta-analysis. Lancet.
384:2235–2243. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Massie BM, Carson PE, McMurray JJ, Komajda
M, McKelvie R, Zile MR, Anderson S, Donovan M, Iverson E, Staiger
C, et al; I-PRESERVE Investigators, . Irbesartan in patients with
heart failure and preserved ejection fraction. N Engl J Med.
359:2456–2467. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Luo J, Gao X, Peng L, Sun H and Dai G:
Effects of hydrochlorothiazide on cardiac remodeling in a rat model
of myocardial infarction-induced congestive heart failure. Eur J
Pharmacol. 667:314–321. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang JL, Yu H, Hou YW, Wang K, Bi WS,
Zhang L, Wang Q, Li P, Yu ML and Zhao XX: Impact of long-term
potassium supplementation on thiazide diuretic-induced
abnormalities of glucose and uric acid metabolisms. J Hum
Hypertens. 32:301–310. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mowla MM and Bustami BB: Brain natriuretic
peptide in heart failure and beyond. Saudi Med J. 27:1457–1461.
2006.PubMed/NCBI
|
|
15
|
Ghali JK, Piña IL, Gottlieb SS, Deedwania
PC and Wikstrand JC; MERIT-HF Study Group, . Metoprolol CR/XL in
female patients with heart failure: Analysis of the experience in
Metoprolol Extended-Release Randomized Intervention Trial in Heart
Failure (MERIT-HF). Circulation. 105:1585–1591. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Esquinas AM and Kasai T: Non-invasive
mechanical ventilation for sleep disordered breathing and cardiac
function in chronic heart failure. More CPAP or more ASV? That is
the question. Int J Cardiol. 168:29782013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gregoretti C, Mattei A and Carlucci A:
Noninvasive ventilation outside the critical care unit. Practical
Issues Updates in Anesthesia and Intensive Care. Springer
International Publishing. 139–147. 2015. View Article : Google Scholar
|
|
18
|
Dave C, Turner A, Dretzke J, Bayliss S,
O'Brien D, Jowett S and Moore D: Protocol for a systematic review
and economic evaluation of the clinical and cost-effectiveness of
non-hospital-based non-invasive ventilation (NIV) in patients with
stable end-stage COPD with hypercapnic respiratory failure. Syst
Rev. 3:322014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Panacek EA and Kirk JD: Role of
noninvasive ventilation in the management of acutely decompensated
heart failure. Rev Cardiovasc Med. 3 Suppl 4:S35–S40.
2002.PubMed/NCBI
|
|
20
|
Stoltzfus S: The role of noninvasive
ventilation: CPAP and BiPAP in the treatment of congestive heart
failure. Dimens Crit Care Nurs. 25:66–70. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Prescher S, Schoebel C, Koehler K,
Deckwart O, Wellge B, Honold M, Hartmann O, Winkler S and Koehler
F: Prognostic value of serial six-minute walk tests using
tele-accelerometry in patients with chronic heart failure: A
pre-specified sub-study of the TIM-HF-Trial. Eur J Prev Cardiol. 23
Suppl:21–26. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Barth AS, Kumordzie A, Frangakis C,
Margulies KB, Cappola TP and Tomaselli GF: Reciprocal
transcriptional regulation of metabolic and signaling pathways
correlates with disease severity in heart failure. Circ Cardiovasc
Genet. 4:475–483. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
No authors listed: 5 action steps for
early heart failure. Early heart failure may be mild but can worsen
quickly. Learn what you can do to keep symptoms in check. Harv
Heart Lett. 24:32014.
|
|
24
|
Pourafkari L, Ghaffari S, Afshar AH, Anwar
S and Nader ND: Predicting outcome in acute heart failure, does it
matter? Acta Cardiol. 70:653–663. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bonacchi M, Vannini A, Harmelin G,
Batacchi S, Bugetti M, Sani G and Peris A: Inverted-Takotsubo
cardiomyopathy: Severe refractory heart failure in poly-trauma
patients saved by emergency extracorporeal life support. Interact
Cardiovasc Thorac Surg. 20:365–371. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Patel KP: Role of paraventricular nucleus
in mediating sympathetic outflow in heart failure. Heart Fail Rev.
5:73–86. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Berg T: β1-Blockers lower norepinephrine
release by inhibiting presynaptic, facilitating β1-adrenoceptors in
normotensive and hypertensive rats. Front Neurol. 5:512014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen Y, Chen P, Hanaoka M, Huang X, Droma
Y and Kubo K: Mechanical ventilation in patients with hypoxemia due
to refractory heart failure. Intern Med. 47:367–373. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Squadrone E, Frigerio P, Fogliati C,
Gregoretti C, Conti G, Antonelli M, Costa R, Baiardi P and Navalesi
P: Noninvasive vs invasive ventilation in COPD patients with severe
acute respiratory failure deemed to require ventilatory assistance.
Intensive Care Med. 30:1303–1310. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kuhn BT, Bradley LA, Dempsey TM, Puro AC
and Adams JY: Management of mechanical ventilation in decompensated
heart failure. J Cardiovasc Dev Dis. 3:32016.
|
|
31
|
Huang QF, Sheng CS, Li Y, Ma GS, Dai QY
and Wang JG; INCENT Investigators, . Efficacy and safety of a fixed
combination of irbesartan/hydrochlorothiazide in Chinese patients
with moderate to severe hypertension. Drugs R D. 13:109–117. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Croxtall JD and Keating GM:
Irbesartan/Hydrochlorothiazide: In moderate to severe hypertension.
Drugs. 68:1465–1472. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chrysant SG, Neutel JM and Ferdinand KC;
INCLUSIVE investigators, . Irbesartan/hydrochlorothiazide for the
treatment of isolated systolic hypertension: A subgroup analysis of
the INCLUSIVE trial. J Natl Med Assoc. 101:300–307. 2009.
View Article : Google Scholar : PubMed/NCBI
|