Introduction
Spinal cord injury (SCI) causes serious disability
and is a medical problem worldwide (1). SCI has two defined phases, consisting
of primary and secondary injury mechanisms that lead to an
excessive inflammatory response (2,3).
Disruption of the spinal tract results in neuronal apoptosis, and
impedes neuronal repair and regeneration. A key challenge is how to
reduce inflammation, improve axonal regeneration and functional
recovery after SCI (4). Recently,
transplantation of bone marrow stromal cells (BMSCs) has emerged as
a novel treatment for SCI (5–7). BMSCs
are a population of heterogeneous mesenchymal cells located in the
bone marrow that possess unlimited proliferative capacity and
multidifferentiation properties (8,9).
Furthermore, it has been reported that BMSCs have an important role
in the immunomodulation of innate and adaptive immune processes
in vitro and in vivo (10,11).
BMSCs transplantation may benefit injured neurons, through the
release of various kinds of factors, which indirectly influence the
process of inflammation by regulating the expression of
inflammatory cytokines from a variety of immune cell types after
SCI (12–15). However, the mechanisms underlying the
regulation of inflammation by BMSCs in the injured spinal cord
remain unclear.
Secondary SCI is accompanied by a series of
intracellular metabolisms, such as inflammatory cell infiltration.
After SCI, the blood-brain barrier (BBB) is disrupted and
inflammatory cells produce potentially toxic molecules, including
free oxygen radicals, cytokines and chemokines which may inhibit
axon regeneration of the spinal lesion (2,4).
Toll-like receptors (TLRs) are a transmembrane receptor family.
Activation of the TLRs has a critical role in the innate immune
response (16). Toll-like receptor 4
(TLR4) is an important member that is associated with SCI-induced
inflammation. Accumulating evidence indicates the involvement of
TLR4 in inducing spinal inflammation, including that in lateral
sclerosis, ischemia reperfusion injury and trauma (17,18). As
one of the most important downstream molecules in the TLR signaling
pathways, nuclear factor (NF)-κB is a transcriptional factor
required for transcriptional activation of its target genes,
including tumor necrosis factor-α (TNF-α), interleukin-1β (IL-1β),
and IL-6 (19,20).
Therefore, in the present study, a modified Allen's
weight-drop SCI rat model was established and BMSCs were
transplanted into the injured spinal cord. Locomotion recovery and
pathological changes in the spinal cord of the SCI rat model were
analyzed after BMSC transplantation. Furthermore, the effect of
BMSCs on modulating the expressions of TLR4 and NF-κB in the
injured spinal cord was investigated. The present study may
challenge the classical view of stem cell transplant therapy for
SCI, not only through neuronal differentiation, but also in
reducing inflammation.
Materials and methods
Ethics statement
The experimental procedures were approved by the
Animal Ethics Committee of Zhejiang University (Hangzhou, China)
and were performed according to institutional guidelines. All
efforts were made to minimize the number of rats used and their
suffering.
Primary BMSC culture and
characterization
Primary rat BMSCs were isolated as previously
described (7). BMSCs were harvested
from the femur of 3-week-old Sprague-Dawley (SD) female rats. Bone
marrow was removed and diluted with an equal volume of Dulbecco's
modified Eagle's medium (DMEM; Gibco; Thermo Fisher Scientific,
Inc., Waltham, MA, USA), which was subsequently centrifuged at
1,200 × g for 7 min. The supernatant was removed, and the pellet
was inoculated into plastic flasks containing DMEM supplemented
with 10% fetal bovine serum (FBS; 10% w/v; Gibco; Thermo Fisher
Scientific, Inc.), 1% L-glutamine (Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany) and 1% penicillin and streptomycin. The flasks
were incubated at 37°C in a humidified tissue culture incubator
containing 5% CO2 and 95% air. The medium was replaced
every 3 days, and cells were passaged at 1:4 when 90% confluence
was reached, using 0.25% trypsin. All stem cells in this experiment
were performed with cells in passage 3.
SCI model
Thirty 6-week-old SD female rats were purchased from
Zhejiang Experimental Animal Center (Hangzhou, China) and divided
into three groups at random: sham operation (control) group, SCI
group and BMSC-treated SCI group. Rats were anesthetized with an
intraperitoneal injection of 40 mg/kg sodium pentobarbital. The
vertebral column of the rats was then exposed, and a laminectomy
carried out at T10 vertebrae. A weight of 10 g was dropped from a
height of 5 cm onto the exposed spinal cord to cause moderate
contusion at the T10 vertebrae in the SCI group and BMSC treatment
group rats (6). The sham operation
rats received the same surgical procedure, with no injury. After
injury, 10 µl DMEM containing 1×106 BMSCs was injected
into the center of the injured spinal cords of the BMSC treatment
group rats, using electrode microneedles. The same volume of cell
culture media was injected into the SCI and sham operation animals.
All rats were subcutaneously injected with ampicillin (100 mg/kg)
daily for the first 7 days to prevent infection. Twice per day, the
bladder was emptied manually. A certain number of rats were
sacrificed for immunohistochemical staining of TLR4, NF-κB, and
caspase-12 48 h after SCI, while others were sacrificed 7 days
after SCI, for growth-associated protein 43 (GAP-43)
immunofluorescence staining, hematoxylin and eosin (H&E)
Staining and toluidine blue (Nissl).
Assessment of motor function
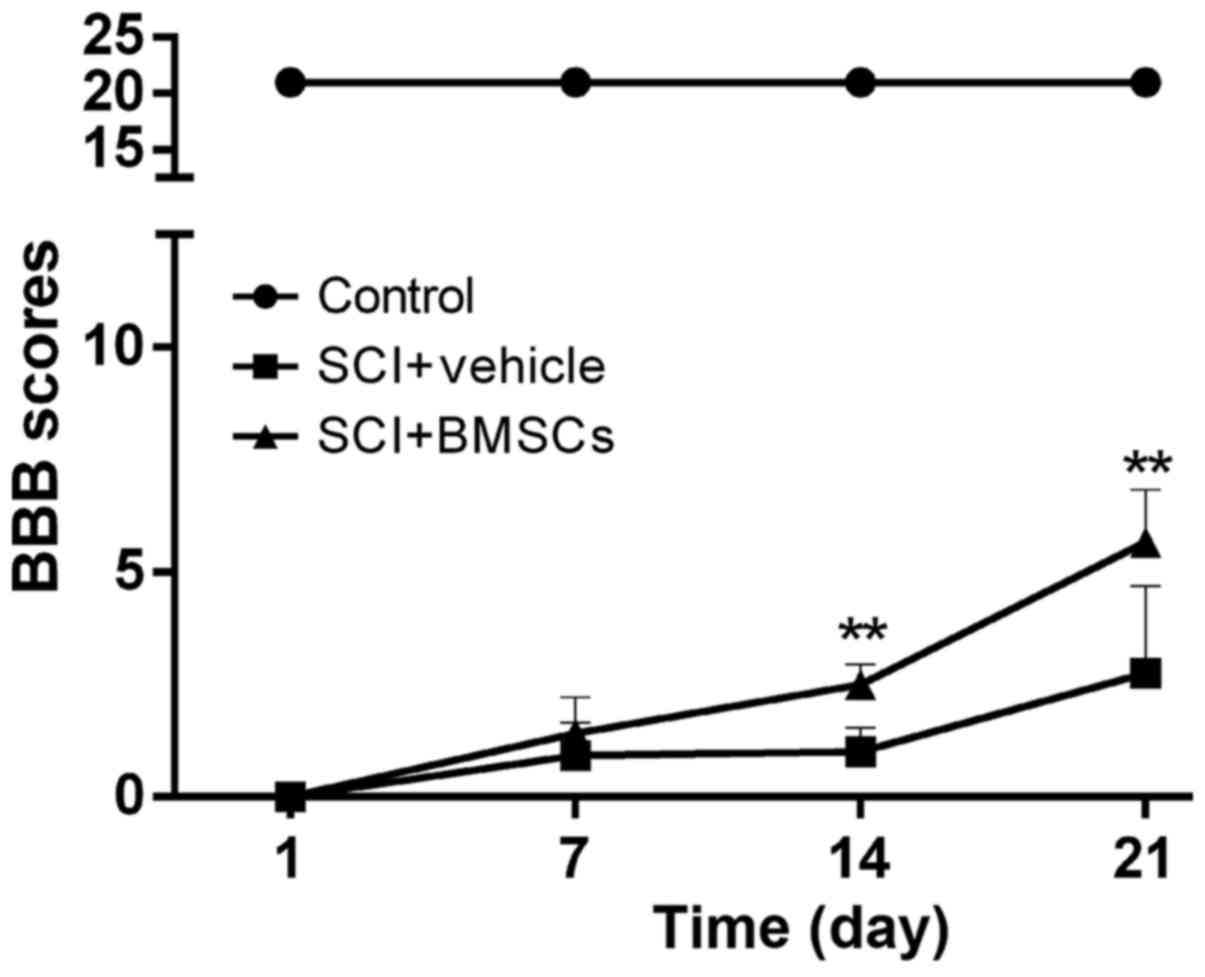
The Basso, Beattie, and Bresnahan (BBB) locomotor
scale was used to evaluate the rats after transplantation (21). The ranging scale from 0 (complete
paralysis) to 21 (normal locomotion) was applied to evaluate the
motor function in an open field for 2–3 min in all groups at days
1, 7, 14 and 21 after surgery in all three groups.
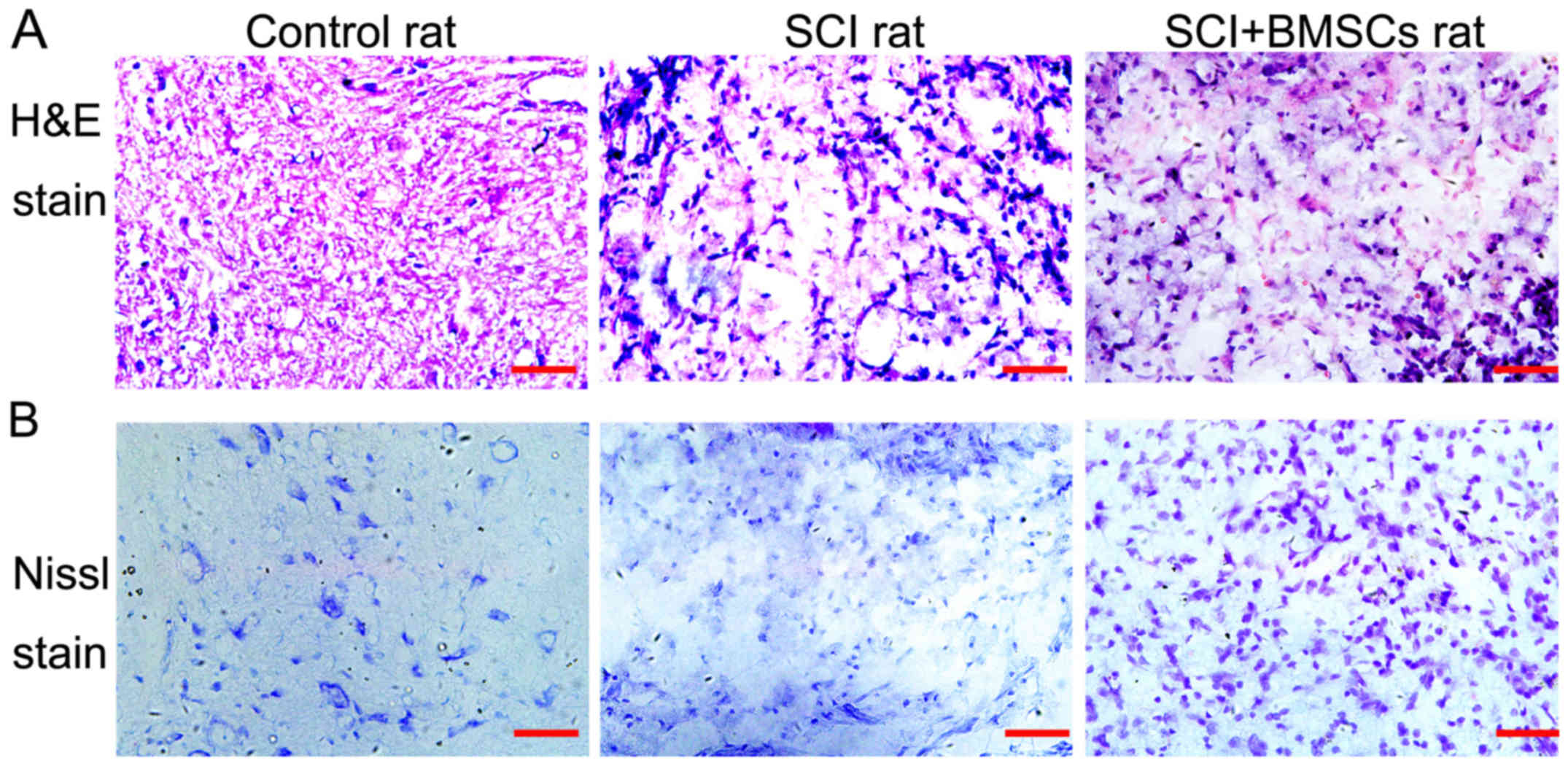
H&E and Nissl staining
For pathological analysis, the sections were
respectively subjected to H&E and Nissl staining. Five rats
from each group were anesthetized with an intraperitoneal injection
of 60 mg/kg sodium pentobarbital, and perfused with 4%
paraformaldehyde in PBS 7 days after SCI. The lesion epicenter (4
mm) of the injured spinal cord was removed, fixed for 24 h and
prepared for cryostat sectioning. The transverse sections (10 µm
thick) were mounted in silane-coated slides. Rat sections were
subsequently stained with cresyl violet (0.3%; VWR International,
Buffalo Grove, IL, USA) for H&E and Nissl Staining. All images
were collected in the same area of the section using an Olympus
BX61 microscope (Olympus Corporation, Tokyo, Japan). Area
measurements were performed using Image-Pro Plus 5.0 image analysis
software (Media Cybernetics Inc., Atlanta, GA, USA).
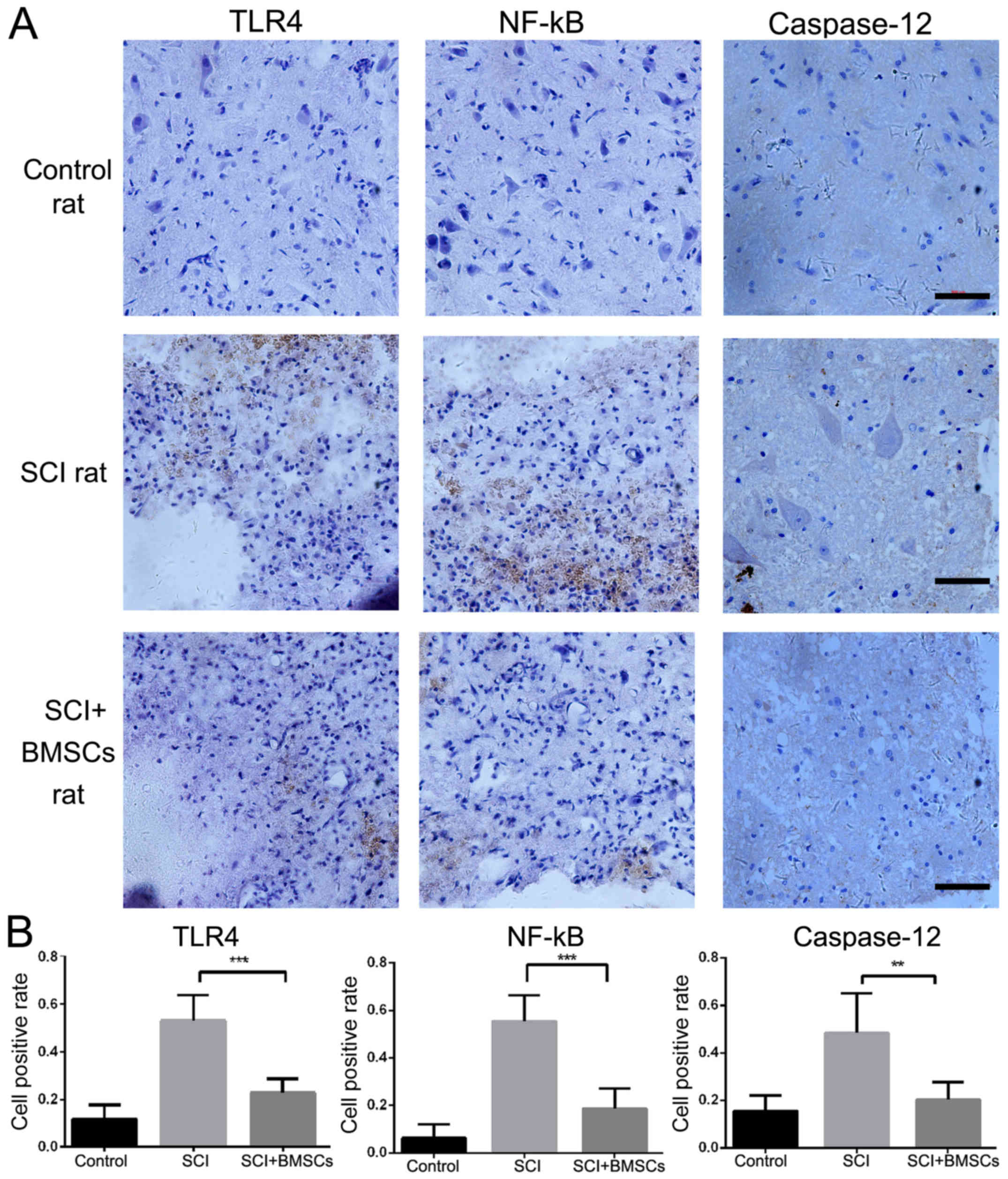
Immunohistochemical and
immunofluorescence staining
Tissue sections from all groups were washed in 0.01
M PBS containing 0.3% Triton X-100 (pH 7.4, PBS-T) for
immunohistochemical analysis, prior to immersion in 2% normal horse
serum in PBS for 120 min at 37°C and incubation overnight at 4°C
with polyclonal rabbit anti-NF-κB, TLR4 and caspase-12 (1:200;
Boster Biotechnology Co., Ltd., Wuhan, China) antibodies. Sections
were washing with PBS and subsequently incubated with HRP goat
anti-rabbit immunoglobulin G (IgG; 1:200; Boster Biotechnology Co.,
Ltd.) secondary antibody for 1 h. Hematoxylin was used to
counterstain nuclei. The samples were mounted in Fluoromount/Plus
(Diagnostic BioSystems, Pleasanton, CA, USA). Images were obtained
on an Axio Imager M1 microscope with AxioVision software (Carl
Zeiss, Tokyo, Japan).
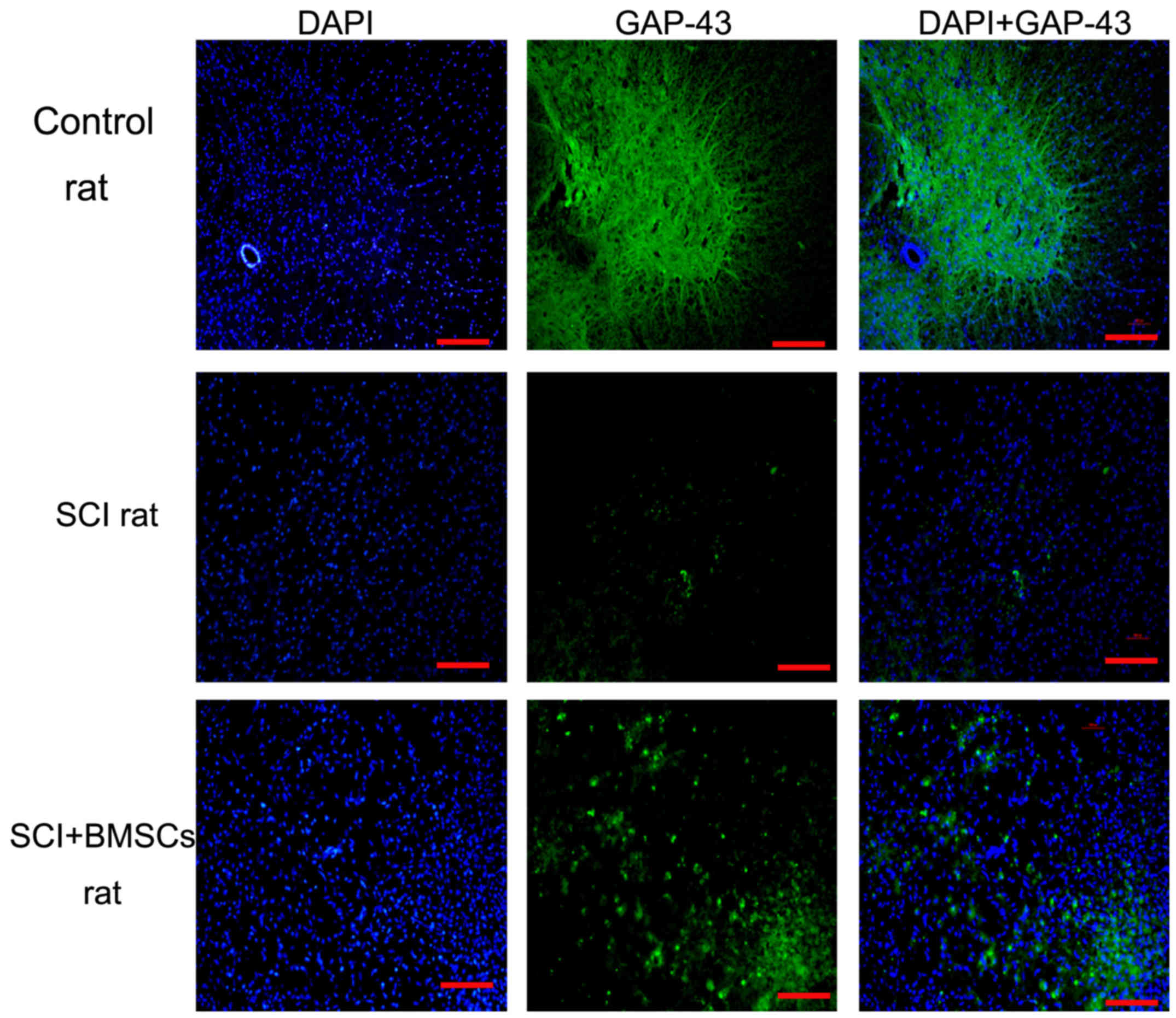
Immunofluorescence analysis was used to detect the
expression of GAP-43 in all groups. The sections were incubated
overnight with GAP-43 antibody (1:100; Boster Biotechnology Co.,
Ltd.) overnight at 4°C, washed three times with PBS and
subsequently incubated with fluorescent-conjugated secondary
antibody. Slides were counterstained with DAPI for 5 min and
coverslipped. All images were captured in the same area of the
section using an Olympus FluoView FV1000 Confocal laser scanning
microscope.
Statistical analysis
Data are presented as mean ± standard deviation.
One-way analysis of variance (ANOVA) with a post-hoc Tukey's test
was used for comparisons between more than two groups. P<0.05
was considered to indicate a statistically significant
difference.
Results
BBB scores
1 day after SCI establishment, rats in the SCI and
BMSC-treated groups displayed typical paraplegia syndrome; the tail
was dropped and both hind limbs were paralyzed with muscle strength
scores of 0. Rats were followed up at 14 and 21 days after BMSC
transplantation. The BBB score in the BMSCs treatment group was
significantly higher than that of the SCI group (P<0.05), while
the animals in the sham operation group walked normally. Comparison
of BMSC treatment rats at different time points revealed that the
BBB score exhibited a gradual upward trend at 7, 14 and 21 days
after SCI. The improvement in the BMSC treatment rats was
significantly different from the SCI rats at 14 and 21 days after
BMSCs transplantation (P<0.05; Fig.
1).
H&E and Nissl staining assay
7 days after BMSC transplantation, H&E staining
was used to analyze pathological changes after SCI. The results
demonstrated that neurons in the sham operation group appeared
normal, with intact, round, full nuclei and clear nucleoli.
However, neuronal swelling and shrunken neurons with darkly
stained, condensed nuclei, as well as significant loss and damage
to neuronal and glial cells, were observed in the SCI and SCI+BMSCs
groups (Fig. 2). Furthermore, the
tissues appeared disorderly and irregularly arranged. However, the
pathological changes observed improved with BMSC treatment, as the
cavity of the SCI+BMSC group was reduced, compared with the SCI
group. In addition, Nissl staining was used to investigate the
extent of neuronal demyelination at the injury site. It was
observed that the sections from the sham group contained myelin
sheaths of different diameters in an orderly arrangement with even
distribution whereas demyelination was present after injury, with
disorderly arrangement and irregular distribution, accompanied by
numerous swellings and near-disruption in the SCI group. However,
these changes were improved in the BMSCs treatment group (Fig. 2B). Both H&E staining and Nissl
staining results indicated that BMSC treatment improved the
pathological changes induced after SCI.
TLR4, NF-κB, and caspase-12 expression
in the injured spinal cord
As cavity formation was reduced under BMSCs
treatment, whether BMSCs transplantation reduced the inflammatory
response and neuronal apoptosis was investigated. The expression of
the inflammatory factors TLR4 and NF-κB, as well as apoptosis
factor caspase-12, was detected by immunohistochemical staining.
The results revealed that both TLR4 and NF-κB expression increased
after SCI, However, BMSC treatment resulted in a significant
decrease in expression, compared with the SCI group (P<0.01).
The expression of caspase-12 was markedly upregulated after SCI.
BMSC treatment resulted in significantly lower caspase-12 levels
compared with the SCI group (P<0.05; Fig. 3), indicating that neuronal apoptosis
caused by SCI was significantly improved by BMSC treatment. Taken
together, the results demonstrated that BMSC transplant reduced the
inflammatory response and apoptotic cell death following SCI.
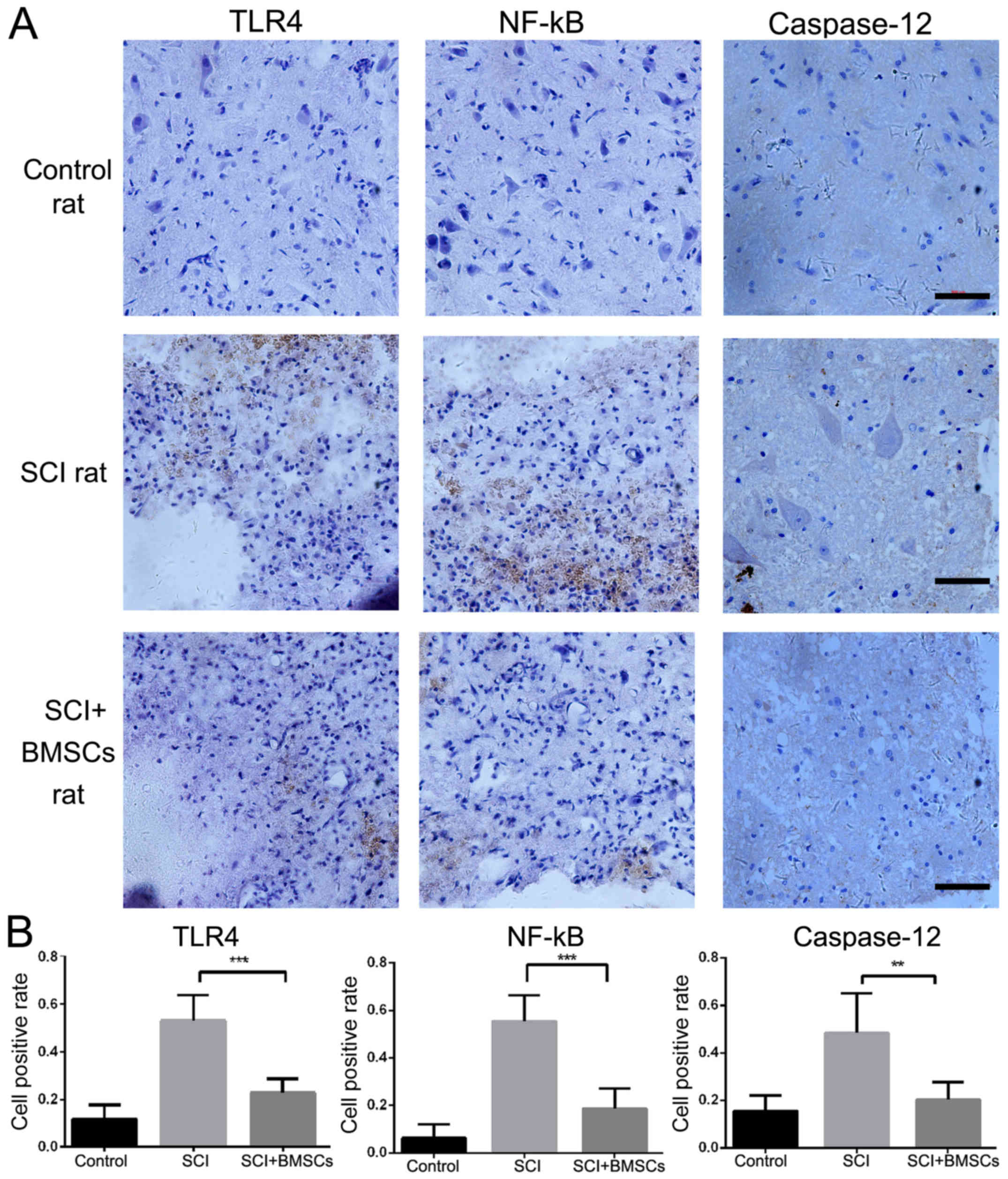 | Figure 3.(A) Immunohistochemical staining of
TLR4, NF-κB and caspase-12 expression, (B) the proportion of TLR4,
NF-κB and caspase-12 positive cells in each group, 24 h
post-surgery. Scale bar=500 µm (magnification, ×400). ***P<0.01,
vs. SCI rats, **P<0.05, vs. SCI rats. TLR4, Toll-like receptor
4; NF-κB, nuclear factor-κB; BMSC, bone marrow stromal cell; SCI,
spinal cord injury. |
GAP43 expression is promoted by BMSC
transplantation
It was hypothesized that decreased inflammation and
apoptosis may promote axon regeneration. The present study focused
on spinal GAP43 expression 7 days after BMSC transplantation. GAP43
is highly expressed in the axons, and is the most widely used
marker for nerve regeneration. By immunofluorescence staining, it
was demonstrated that GAP43-positive fibers were significantly
increased in response to BMSC treatment (Fig. 4), indicating that BMSC treatment
increased GAP43 expression and may have supported axon
regeneration.
Discussion
SCI is a serious disease that eventually results in
loss of movement and sensation below the lesion (15,22).
After SCI occurs, the inflammatory response has an important role
in the pathogenesis of the injured spinal cord (23,24). The
present study demonstrated that BMSC transplantation suppressed the
expression of TLR4 and NF-κB in the injured spinal cord after
trauma. Furthermore, locomotor deficits, pathological changes in
the spinal cord and caspase-12 expression were markedly ameliorated
following BMSCs transplantation to SCI rats. To the best of our
knowledge, the present study is the first to demonstrate that BMSCs
transplantation improved functional recovery following SCI by
inhibiting the inflammatory response via TLR4/NF-κB signaling.
After SCI, inflammatory cell infiltration and
hypoxia occur around the original injury site. These inflammatory
responses begin immediately after injury, and continue in the days
and weeks following SCI. This process results in further tissue
damage, leading to the loss of motor and sensory function below the
lesion (3). The inflammatory
response in the injured spinal cord is a key mechanism mediating
the secondary injury stage after SCI (2,25). The
cells at the site of injury trigger the inflammatory response
through the activation of multiple receptors, including TLR4, in
immune-competent cells, neurons and astrocytes (26). These receptors promote the activation
of NF-κB, a multifunctional transcription factor that controls
several pro-inflammatory and stress responses, which may ultimately
induce apoptosis, neuronal degeneration and disease progression
(27). A previous study revealed
that the ideal treatment for SCI would focus on preventing
inflammation in the injured spinal cord, improving the
microenvironment around the injured lesion and promoting axonal
regeneration (27). Our results
demonstrated that SCI activated TLR4/NF-κB signaling and increased
caspase-12 expression in the injured spinal cord. Furthermore, BMSC
transplantation significantly improved the pathological changes
observed and rat locomotor function; this may have been through the
suppression of TLR4 and NF-κB expression in the injured spinal
cord. Furthermore, the number of caspase-12 positive cells was
notably decreased in BMSC-treated SCI rats.
In conclusion, the present study demonstrated that
BMSC transplantation to the injured spinal cord may contribute to
functional restoration in SCI rats. BMSC treatment gradually
improved the injured spinal cord tissue and dramatically decreased
the number of caspase-12 positive cells, potentially through
downregulation of TLR4/NF-κB expression. The results provided a
novel insight into the therapeutic potential of BMSCs, which may
lead to the development of a novel therapeutic approach to prevent
inflammation following SCI.
Acknowledgements
Not applicable.
Funding
The present study was supported by Zhejiang
Provincial Natural Science Foundation of China (grant no.
LY15H090002) and the Public Applied Technology Research Project of
Zhejiang Province (grant no. 2015C37081).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
SB performed the experiments and wrote the
manuscript. HZ performed the experiments and analyzed the data. LW
contributed in designing the study and revising the manuscript.
Ethics approval and consent to
participate
The experimental procedures were approved by the
Animal Ethics Committee of Zhejiang University (Hangzhou, China)
and were performed according to institutional guidelines.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rubiano AM, Carney N, Chesnut R and Puyana
JC: Global neurotrauma research challenges and opportunities.
Nature. 527:S193–S197. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Allison DJ and Ditor DS: Immune
dysfunction and chronic inflammation following spinal cord injury.
Spinal Cord. 53:14–18. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Orr MB, Simkin J, Bailey WM, Kadambi NS,
McVicar AL, Veldhorst AK and Gensel JC: Compression Decreases
Anatomical and Functional Recovery and Alters Inflammation after
Contusive Spinal Cord Injury. J Neurotrauma. 34:2342–2352. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Okada S: The pathophysiological role of
acute inflammation after spinal cord injury. Inflamm Regen.
36:202016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lin L, Lin H, Bai S, Zheng L and Zhang X:
Bone marrow mesenchymal stem cells (BMSCs) improved functional
recovery of spinal cord injury partly by promoting axonal
regeneration. Neurochem Int. 115:80–84. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pu Y, Meng K, Gu C, Wang L and Zhang X:
Thrombospondin-1 modified bone marrow mesenchymal stem cells
(BMSCs) promote neurite outgrowth and functional recovery in rats
with spinal cord injury. Oncotarget. 8:96276–96289. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gu C, Li H, Wang C, Song X, Ding Y, Zheng
M, Liu W, Chen Y, Zhang X and Wang L: Bone marrow mesenchymal stem
cells decrease CHOP expression and neuronal apoptosis after spinal
cord injury. Neurosci Lett. 636:282–289. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tang X, Chen F, Lin Q, You Y, Ke J and
Zhao S: Bone marrow mesenchymal stem cells repair the hippocampal
neurons and increase the expression of IGF-1 after cardiac arrest
in rats. Exp Ther Med. 14:4312–4320. 2017.PubMed/NCBI
|
|
9
|
Zhang L, Chen J, Chai W, Ni M, Sun X and
Tian D: Glycitin regulates osteoblasts through TGF-β or AKT
signaling pathways in bone marrow stem cells. Exp Ther Med.
12:3063–3067. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zheng YH, Deng YY, Lai W, Zheng SY, Bian
HN, Liu ZA, Huang ZF, Sun CW, Li HH, Luo HM, et al: Effect of bone
marrow mesenchymal stem cells on the polarization of macrophages.
Mol Med Rep. 17:4449–4459. 2018.PubMed/NCBI
|
|
11
|
Ock SA, Baregundi Subbarao R, Lee YM, Lee
JH, Jeon RH, Lee SL, Park JK, Hwang SC and Rho GJ: Comparison of
Immunomodulation Properties of Porcine Mesenchymal Stromal/Stem
Cells Derived from the Bone Marrow, Adipose Tissue, and Dermal Skin
Tissue. Stem Cells Int. 2016:95813502016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ide C, Nakai Y, Nakano N, Seo TB, Yamada
Y, Endo K, Noda T, Saito F, Suzuki Y, Fukushima M, et al: Bone
marrow stromal cell transplantation for treatment of sub-acute
spinal cord injury in the rat. Brain Res. 1332:32–47. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hawryluk GW, Mothe A, Wang J, Wang S,
Tator C and Fehlings MG: An in vivo characterization of trophic
factor production following neural precursor cell or bone marrow
stromal cell transplantation for spinal cord injury. Stem Cells
Dev. 21:2222–2238. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yang W, Yang Y, Yang JY, Liang M and Song
J: Treatment with bone marrow mesenchymal stem cells combined with
plumbagin alleviates spinal cord injury by affecting oxidative
stress, inflammation, apoptotis and the activation of the Nrf2
pathway. Int J Mol Med. 37:1075–1082. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cho SR, Kim YR, Kang HS, Yim SH, Park CI,
Min YH, Lee BH, Shin JC and Lim JB: Functional Recovery after the
Transplantation of Neurally Differentiated Mesenchymal Stem Cells
Derived from Bone Marrow in a Rat Model of Spinal Cord Injury. Cell
Transplant. 25:14232016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lester SN and Li K: Toll-like receptors in
antiviral innate immunity. J Mol Biol. 426:1246–1264. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kigerl KA and Popovich PG: Toll-like
receptors in spinal cord injury. Curr Top Microbiol Immunol.
336:121–136. 2009.PubMed/NCBI
|
|
18
|
Heiman A, Pallottie A, Heary RF and
Elkabes S: Toll-like receptors in central nervous system injury and
disease: A focus on the spinal cord. Brain Behav Immun. 42:232–245.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ntoufa S, Vilia MG, Stamatopoulos K, Ghia
P and Muzio M: Toll-like receptors signaling: A complex network for
NF-κB activation in B-cell lymphoid malignancies. Semin Cancer
Biol. 39:15–25. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu J, Wang Y and Ouyang X: Beyond
toll-like receptors: Porphyromonas gingivalis induces IL-6, IL-8,
and VCAM-1 expression through NOD-mediated NF-κB and ERK signaling
pathways in periodontal fibroblasts. Inflammation. 37:522–533.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhou R, Alvarado L, Ogilvie R, Chong SL,
Shaw O and Mushahwar VK: Non-gait-specific intervention for the
rehabilitation of walking after SCI: Role of the arms. J
Neurophysiol. 119:2194–2211. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kong X and Gao J: Macrophage polarization:
A key event in the secondary phase of acute spinal cord injury. J
Cell Mol Med. 21:941–954. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhou Z, Liu C, Chen S, Zhao H, Zhou K,
Wang W, Yuan Y, Li Z, Guo Y, Shen Z, et al: Activation of the
Nrf2/ARE signaling pathway by probucol contributes to inhibiting
inflammation and neuronal apoptosis after spinal cord injury.
Oncotarget. 8:52078–52093. 2017.PubMed/NCBI
|
|
24
|
Fu Q, Li C and Yu L: Gambogic acid
inhibits spinal cord injury and inflammation through suppressing
the p38 and Akt signaling pathways. Mol Med Rep. 17:2026–2032.
2018.PubMed/NCBI
|
|
25
|
Yuan B, Liu D and Liu X: Spinal cord
stimulation exerts analgesia effects in chronic constriction injury
rats via suppression of the TLR4/NF-κB pathway. Neurosci Lett.
581:63–68. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
He Z, Zhou Y, Lin L, Wang Q, Khor S, Mao
Y, Li J, Zhen Z, Chen J, Gao Z, et al: Dl-3-n-butylphthalide
attenuates acute inflammatory activation in rats with spinal cord
injury by inhibiting microglial TLR4/NF-κB signalling. J Cell Mol
Med. 21:3010–3022. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen X, Chen X, Huang X, Qin C, Fang Y,
Liu Y, Zhang G, Pan D, Wang W and Xie M: Soluble epoxide hydrolase
inhibition provides multi-target therapeutic effects in rats after
spinal cord injury. Mol Neurobiol. 53:1565–1578. 2016. View Article : Google Scholar : PubMed/NCBI
|