Introduction
Osteoarthritis (OA) is a multifactorial,
degenerative and incapacitating disease that affects the soft
tissues and bones of the involved articulations, causing pain and
decreased function due to differences between the rate of synthesis
and extracellular matrix degradation of articular cartilage
(1–3).
Nonsteroidal anti-inflammatory drugs and
intra-articular steroid injections are commonly indicated as a
first choice treatment in OA. Together with physical exercise and
corporal weight control, the purpose of this treatment is to
relieve pain and to improve articular function; however, it is not
always effective. Although the intra-articular injection of
hyaluronic acid has been approved as a knee OA treatment in
patients for which non-drug treatment and simple analgesics have
been unsuccessful, this treatment is palliative but not therapeutic
(4).
The amniotic membrane (AM) is the innermost fetal
membrane, usually discarded following birth as part of the
placenta. The membrane itself and stem cells isolated from it have
shown potential for applications in the regenerative medicine
field, due to bacteriostatic and anti-angiogenic properties. It
also has been shown that AM reduces pain, regulates the
inflammatory process, and improves wound healing and
epithelialization (5–8); it also exhibits low or no
immunogenicity and acts as a physical barrier in the case of an
exposed wound (9,10). In clinical trials, complete AM has
been evaluated for the treatment of skin burns (11), as a scaffold biomaterial in the
reconstruction of the ocular surface (12), in head and neck surgery (13), and to prevent tissue adhesion in
abdominal, head and pelvic surgery (14). Acellular AM has been evaluated in
articular cartilage and tendon defects (15) and also in peripheral nerves (16).
Morphologically, AM is a thin and flexible membrane
comprising a monolayer of epithelial cells aligned on a basal
membrane, where the underlying stroma contains mesenchymal cells
(17). These cells have the ability
to differentiate into several lineages, including adipogenic,
osteogenic, chondrogenic, hepatic, neurogenic and cardiomyogenic
tissue (18–23). Amniotic cells are immunomodulatory
in vitro (23), and the AM
and allogeneic amniotic cells have been applied in clinical trials
without evidence of immunologic rejection (10). The osteogenic capability of this
membrane, and the fact it can act as a stimulator in repairing
musculoskeletal injuries have been reported (24).
The aim of the present study was to analyze the
histological changes produced by lyophilized and pulverized human
AM, administered as a treatment in an OA model of the knee
developed in rabbits.
Materials and methods
Study type and ethics
The present study was an experimental,
cross-sectional, comparative, prospective, simple blind study. The
protocol was submitted to the Institutional Ethics and Research
Committee of Universidad Autónoma de Nuevo León (Monterrey, Mexico)
and approved (approval no. OR15-015).
AM isolation and processing
The placentas were obtained from healthy donors who
were scheduled to have cesarean surgery in the obstetrics
department of the Hospital General de Occidente (Zapopan, Mexico)
from May 2017 to August 2017. The placentas were supplied by Top
Health (Zapopan, Mexico) who provided proof of informed consent of
the donors. Following separating of the placenta from the placental
button, the chorionic membrane was then carefully separated. To
decellularize the AM, it was washed with 15% NaCl and gently mixed
in NaOH 0.01 N until brown in color. NaOH was neutralized by adding
ascorbic acid (1N). Hydrogen peroxide solution and gentle mixing
were used to obtain a white color membrane, following which
dehydration with 96% ethanol was performed. The membrane was placed
to be dried for 24 h at room temperature in a ventilated area. The
dried membrane was pulverized, and a screening was performed to
determine the particle size. The membrane was lyophilized and
irradiated with gamma rays of 25 kGy prior to use in animals.
Chemical AO model
In the present study, six adult male New Zealand
rabbits aged ~3 months old and with an average weight of 2.5 kg
were obtained from the Animal Production Unit of the Facultad de
Agronomia (Escobedi, Mexico). The experimental animals were
anesthetized with an intramuscular injection of 1.9 mg/kg xylazine
and 46 mg/kg ketamine. Intra-articular injections of 250 µl of
collagenase type II (Clostridium histolyticum type II, active
enzyme 425 U/mg, 4 mg/ml; Thermo Fisher Scientific, Inc., Waltham,
MA, USA) were performed at days 0 and 4 (25). The rabbits were housed in a bioterium
for 3 and 6 weeks. Rabbits were kept in individual cages at a
temperature of 21°C and a relative humidity of 55% with a 12 h
light/dark cycle and ad libitum access to food and
water.
Intra-articular infiltration of the
AM
Once the OA model was established in both knees of
all rabbits, the animals were divided into two observation groups,
with three animals in each group. Each rabbit underwent an
intra-articular infiltration in the right knee of the lyophilized
human AM (0.040 mg/0.200 ml) and saline solution (0.6 ml) in the
left knee (control group). The animals were sacrificed with an
overdose of xylazine and ketamine IV at 3 and 6 weeks (Group 1 and
2, respectively). The knees were obtained from each rabbit and
placed in formaldehyde solution for preservation. All previously
identified samples were sent for histological examination.
Morphological and histological
analysis
The macroscopic morphological analysis was performed
using the scale published by Yoshioka et al (26) in which the grades are as follows:
Grade 1, intact articular surface; grade 2, minimal fibrillation;
grade 3, evident fibrillation; grade 4, erosion with bone exposure
(Table I).
 | Table I.Yoshioka's scale for macroscopic
evaluation and Mankin's scale for histological evaluation. |
Table I.
Yoshioka's scale for macroscopic
evaluation and Mankin's scale for histological evaluation.
| Group | Time post-injection
(weeks) | Left knee injury | Right knee
injury+AM | P-value |
|---|
| Yoshioka's scale |
| 1 | 3 | 3.15±0.73 | 2.36±0.76 | 0.024 |
| 2 | 6 | 4.25±0.32 | 1.29±0.49 | 0.015 |
| Mankin's scale |
| 1 | 3 | 4.33±0.67 | 2.44±0.21 | 0.028 |
| 2 | 6 | 6.54±0.43 | 1.87±0.73 | 0.015 |
Each knee sample was fixed and decalcified prior to
being embedded in paraffin blocks. From these, 4-µm sagittal
sections were made and stained with hematoxylin and eosin (H&E)
for structure, cellularity and ‘tidemark’ integrity evaluation.
Masson's trichrome staining was used for the extracellular matrix
evaluation. Histopathological assessment of cartilage damage was
performed following Mankin's scale (27) (Table
I). This scale assigns a histological score by adding the
corresponding values to the changes in the cartilage structure,
cellularity, matrix staining and in the ‘tidemark’ or basophilic
limiting line. In this way, normal cartilage corresponds to 0
points and the most severe cartilage affectation corresponds to 14
points. The morphologic and histopathologic evaluations were
performed by independent observers who did not know which group
they assessed. Slides were observed using a Nikon fluorescent
microscope (E600; Nikon Corporation, Tokyo, Japan).
Statistical analysis
The sample size calculation for animal models with
α=0.05, β=0.08 (one-tailed) was six individuals per group.
Calculating a sample size for comparison of related averages
α=0.05, β=0.08 (two-tailed), taking a minimum difference of 2.5, it
was seven individuals per group. The numerical variables were
analyzed using one-way analysis of variance with Tukey's multiple
comparisons post-hoc test to estimate the differences between
groups.
Significance was determined at P≤0.05 was considered
to indicate a statistically significant difference. Descriptive and
inferential statistical analyses were performed using STATA-10-08
software (Stata Corporation, College Station, TX, USA).
Results
Human AM prevents macroscopic changes
in the cartilage of OA model
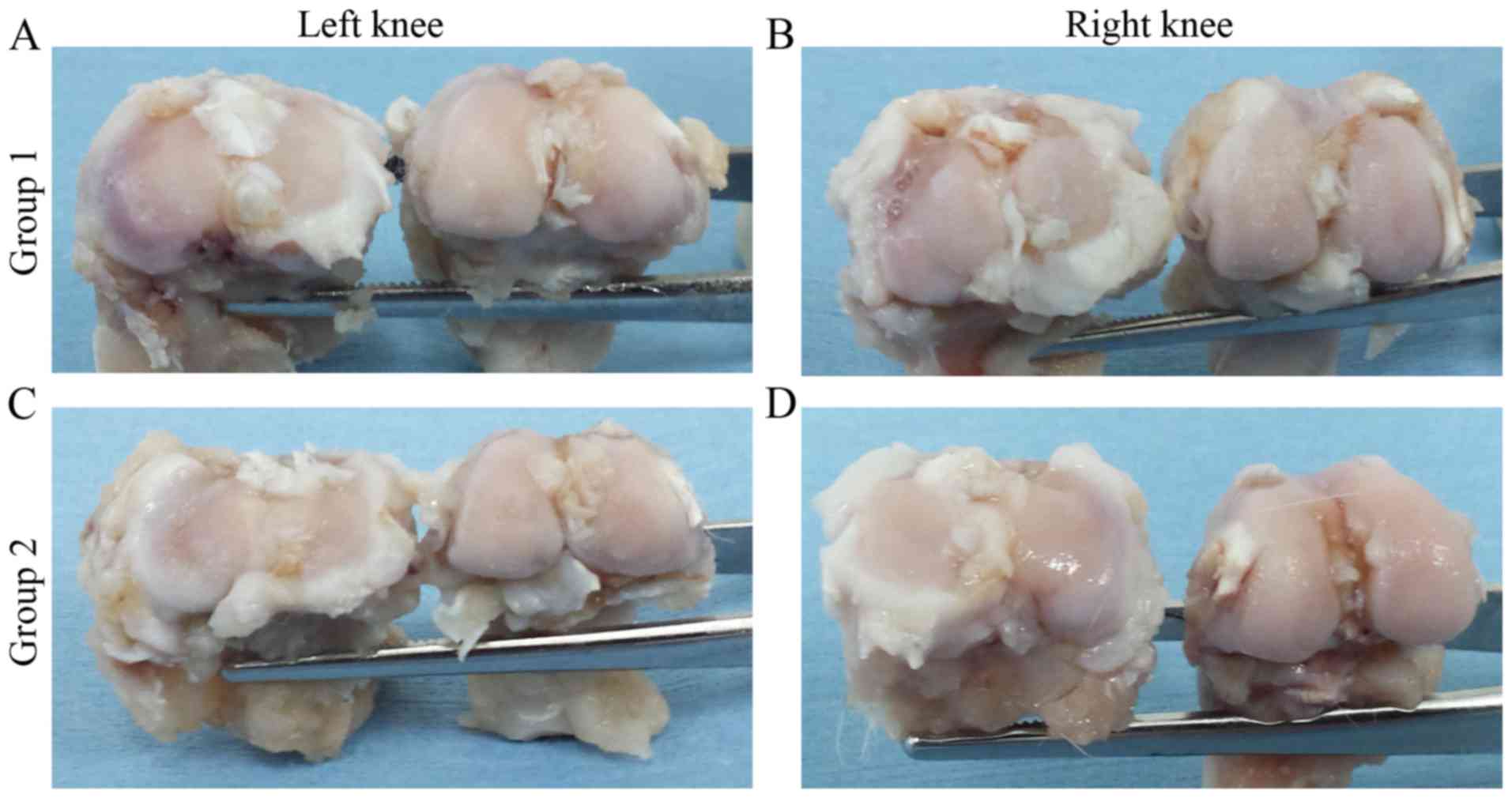
In the left knees of group 1, cartilage fibrillation
and color changes were observed on the joint surface compared with
the right knees which showed a macroscopic apparently intact
surface. However, small areas with poor fibrillation were observed
in the right knees (Fig. 1A and B).
Despite these data, a statistically significant difference
(P=0.024) was found when Yoshioka's scale scores of the left knees
(3.15±0.73) and right knees (2.36±0.76) were compared.
In the left knees of group 2, subchondral bone was
observed in regions of the femoral condyles and the tibial plateau
(Fig. 1C and D). The left knees were
assigned a score of 4.25±0.32 according to Yoshioka's scale
evaluation, whereas the right knees were assigned a score of
1.29±0.49 (P=0.015; Table I).
Human AM protects from extracellular
matrix destruction in the OA model
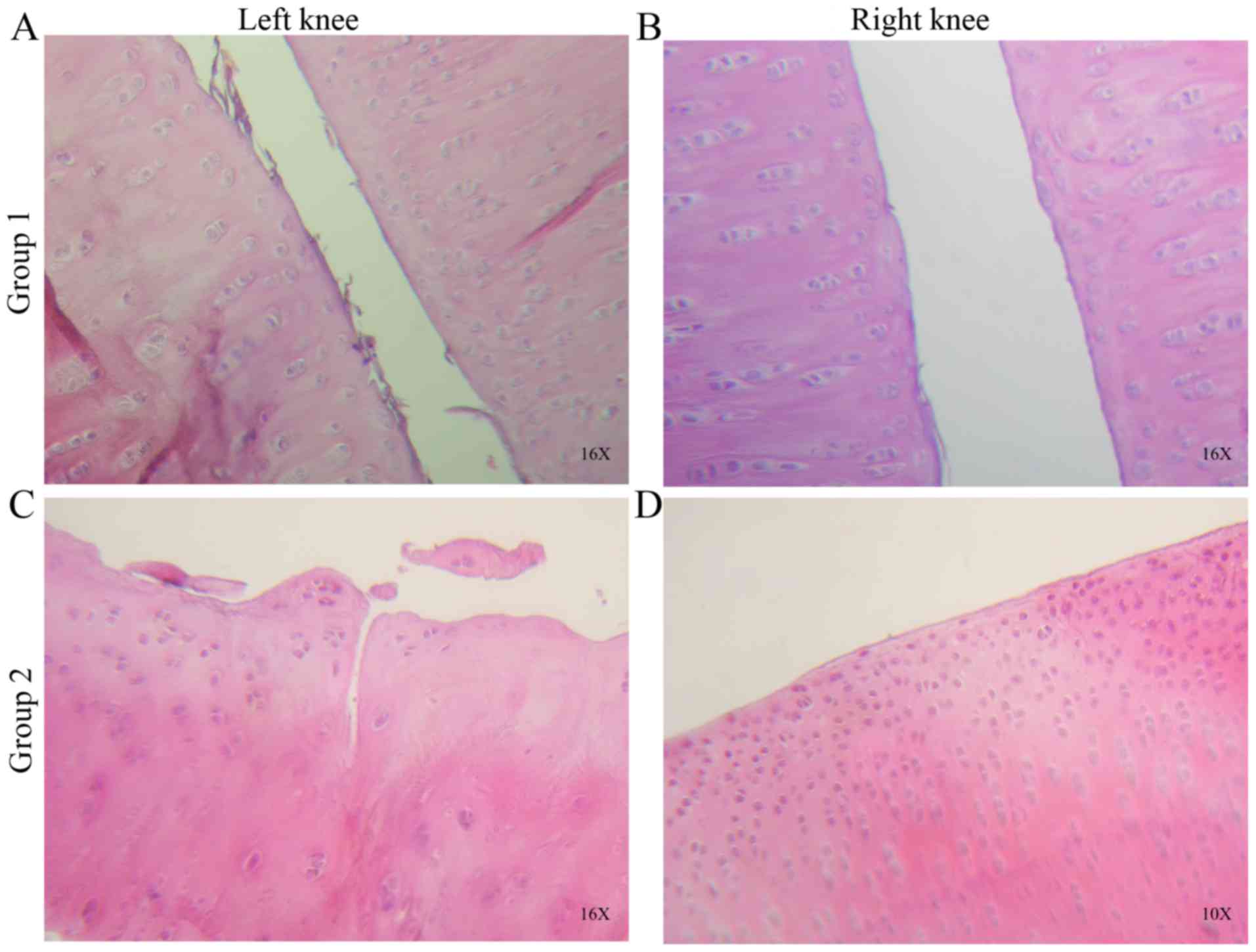
On examining the cartilage morphology in left knees
of the group 1, increased fibers in the superficial cartilage zone
and irregularities on the surface were observed. Compared with the
right knees of the same group, the cartilage surface was more
complete and continuous, with less fibrillation or observed
indentations (Fig. 2A and B).
When the cellularity and matrix staining were
evaluated, the left knees exhibited more cell clusters and reduced
staining in regions where joint surface fibrillation was detected.
By contrast, the right knees exhibited fewer and isolated cell
clusters, with no decrease or loss of staining density. Overall, a
significant statistical difference was observed when comparing the
left and right knees of group 1 (P=0.028).
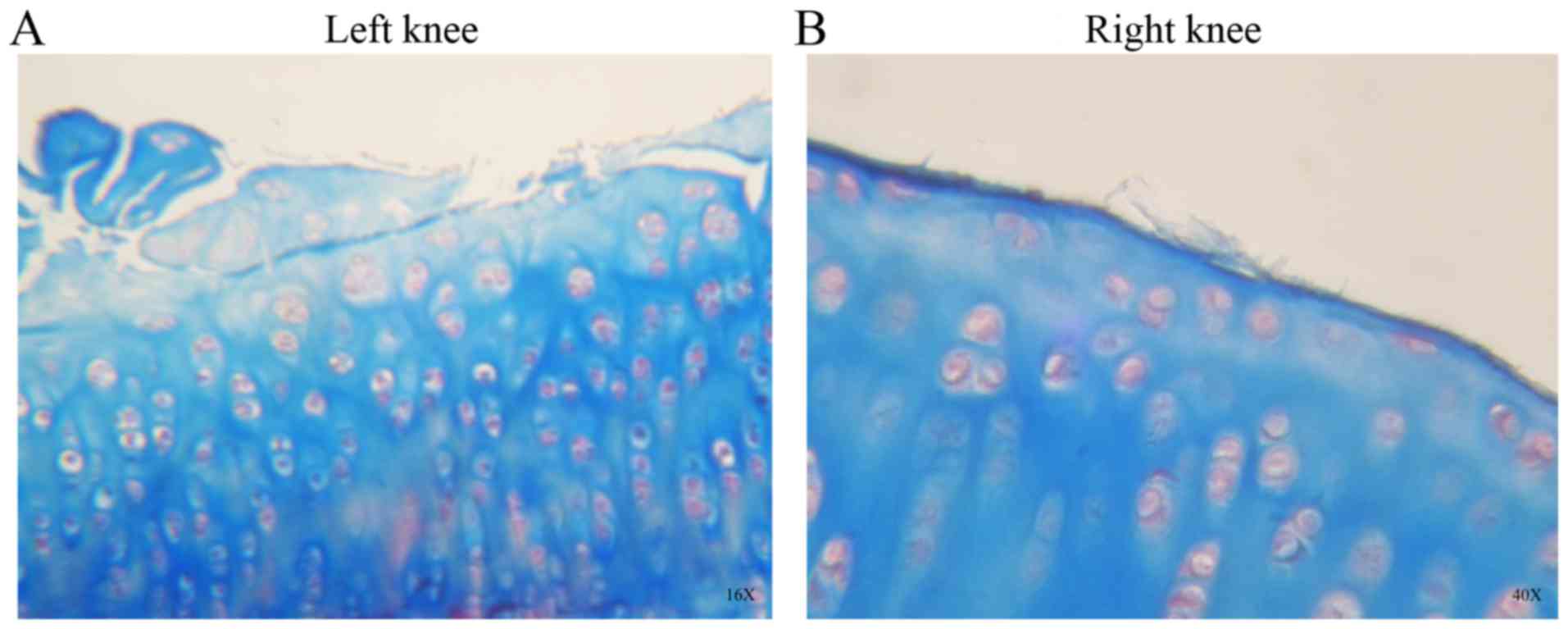
In group 2, the H&E (Fig. 2C and D) and Masson’ trichrome
staining (Fig. 3A and B) showed
cracks, loss of structure, recesses, erosion, and fibrillation in
the left knee cartilage. Abundant cell clusters and decreased
staining were observed on the surface and extracellular matrix. The
right knees of group 2 exhibited an almost intact surface with
minimal articular fibrillation, no cracks and no evident surface
erosion (Figs. 2 and 3). A number of cell clusters were observed
in isolated areas where the cartilage surface was not compromised.
Normal staining was observed on the cartilage surface and
extracellular matrix.
For groups 1 and 2, there was no evident ‘Tidemark’
injury and statistical differences were found on comparing the
right and left knees for Mankin's evaluation scale (Table I; P=0.028 and P=0.015).
Discussion
The AM has been investigated mainly for
ophthalmologic applications, including regenerative medicine in the
cornea (12). A number of studies
investigating AM use in articular cartilage lesion regeneration
have been reported and a chondroprotective effect with reduced
proteoglycan loss, preventing damage progression of the
extracellular matrix, were demonstrated (28). In a study investigating the injection
of dehydrated human amnio/chorionic product, fewer defects and
smaller lesion volumes were observed when compared with saline
solution-injected control animals at day 21 post-injection; the
study demonstrated cartilage destruction attenuation with increases
in cartilage thickness and volume, and a decrease in total lesion
area in animals injected with particulate AM (29). However, this previous study used a
model in Lewis rats that underwent medial meniscal transection
surgery to induce OA and did not perform histopathological
analysis, which is considered to be the ‘gold standard’ for
evaluating the potential therapeutics for OA. In the present study,
a chemical OA model in rabbits was used and, as the joints of these
animals are larger than the knees of rats, this may provide further
support to the significance to the results.
In another study, in which a particulate AM and
umbilical cord tissue in an OA model were used, their results were
compared with EPIC-micro CT and histopathology to demonstrate a
significant reduction in cartilage degeneration and calcified
cartilage at week 1 post-injection, providing further evidence that
AM assists in preventing and treating OA (30).
he present study demonstrated that pulverized AM
injected intra-articularly improved histological features of OA
cartilage in rabbit knees, decreased disease progression and
delayed histological changes, including loss of extracellular
matrix staining. This is possibly due to it being responsible for
supplying growth factors, that allow adequate re-epithelialization
and epithelial cell migration. The low or absent immunogenicity of
AM represents an advantage that reduces complications. However, it
remains necessary to obtain further scientific evidence prior to
indicating that AM is safe for its use in humans as a treatment for
OA of the knee. Therefore, a novel animal model of a higher level
in the phylogenetic scale is required to investigate the efficacy
and safety of the AM application.
Although the majority of the studies involving AM
use animal models to reproduce OA disease, a number of studies have
used AM for clinical trials in human volunteers. Vines et al
(31) demonstrated the
intraarticular injection feasibility of cryogenically preserved
human amniotic suspension allografts for human patients suffering
OA of the knee. Díaz-Prado et al (32) used human AM as a scaffold in human
articular cartilage repair, and demonstrated that cryopreserved
human AM can be used to support chondrocyte proliferation (32). Previous studies in tissue engineering
have used cultured chondrocytes on the AM for use as a scaffold,
and the results indicated the presence of collagen type II and an
extracellular matrix similar to hyaline cartilage (32,33).
This fact may be due to the AM having a high content of
transforming growth factor-β1, and this protein upregulates
chondrogenic gene expression (34,35).
These results of the present study suggested that
the treatment of early OA is feasible using an AM with different
presentations, either fresh or cryopreserved. The present study
used lyophilized, pulverized AM in saline solution as a vehicle for
resuspension. This presentation is easy to handle and store, and
reduces the infection risk as it is dried until resuspension in
PRP. However, further investigations are required to determine the
safety and efficacy of AM in clinical trials for the treatment of
OA and other orthopedic problems, including ligament sprains, and
fracture complications, including pseudoarthrosis, among
others.
Acknowledgements
The present study was supported by The Orthopedics
and Traumatology Service, Hospital Universitario ‘Dr. José E.
González’, Universidad Autónoma de Nuevo León, and Top Health SAPI
de CV.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
IAMM analyzed and interpreted the data. AGMC
established the animal model. VJRD performed the histological knee
examination. VMPM participated in the design of the protocol for
animal model development. CAAO examined the histological sections
as a blind observer and contributed to the statistical analysis.
FVC participated in the interpretation of results and the writing
of the final manuscript. FVC was also responsible for processing
amniotic membranes at the Bone and Tissue Bank of the Universidad
Autónoma de Nuevo León prior to use in the study. AGL obtained
knees following euthanasia and processed sections using
histological techniques. EPR contributed to the experiments. JAOB
participated in the construction of the Discussion section of the
final manuscript and reviewing the English. JLA contributed to the
design of the study, the reviewing of all procedures and the
writing of the final manuscript. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The protocol was submitted to the Institutional
Ethics and Research Committee of Universidad Autónoma de Nuevo León
and approved (approval no. OR15-015). Informed consent was provided
by the donors of placentas.
Patient consent for publication
Not applicable.
Competing interests
The authors confirm that they have no competing
interests.
References
|
1
|
Felson DT, Lawrence RC, Dieppe PA, Hirsch
R, Helmick CG, Jordan JM, Kington RS, Lane NE, Nevitt MC, Zhang Y,
et al: Osteoarthritis: New insights. Part 1 The disease and its
risk factors. Ann Intern Med. 133:635–646. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Giménez Basallote S, Pulido Morillo FJ and
Trigueros Carrero JA: Definición, etiopatogenia, factores de riesgo
y pronóstico. In: Guía de Buena Práctica Clínica en Artrosis. 2nd.
International Marketing & Communication, SA (IM&C); Madrid,
Spain: pp. 11–17. 2008, (In Spanish).
|
|
3
|
Ajadi RA, Otesile EB and Kasali OB:
Short-term changes in lipid profile following experimental
osteoarthritis in dogs. Bulgarian J Veterinary Med. 15:166–171.
2012.
|
|
4
|
Anitua E, Sanchez M, Nurden AT, Zalduendo
MM, de la Fuente M, Azofra J and Andía I: Platelet-released growth
factors enhance the secretion of hyaluronic acid and induce
hepatocyte growth factor production by synovial fibroblasts from
arthritic patients. Rheumatology (Oxford). 46:1769–1772. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gajiwala K and Gajiwala AL: Evaluation of
lyophilized, gamma-irradiated amnion as a biological dressing. Cell
Tissue Bank. 5:73–80. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gruss JS and Jirsch DW: Human amniotic
membrane: A versatile wound dressing. Can Med Assoc J.
118:1237–1246. 1978.PubMed/NCBI
|
|
7
|
Subrahmanyam M: Amniotic membrane as a
cover for microskin grafts. Br J Plast Surg. 48:477–478. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ward DJ, Bennett JP, Burgos H and Fabre J:
The healing of chronic venous leg ulcers with prepared human
amnion. Br J Plast Surg. 42:463–467. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Adinolfi M, Akle CA, McColl I, Fensom AH,
Tansley L, Connolly P, Hsi BL, Faulk WP, Travers P and Bodmer WF:
Expression of HLA antigens, beta 2-microglobulin and enzymes by
human amniotic epithelial cells. Nature. 295:325–327. 1982.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Akle CA, Adinolfi M, Welsh KI, Leibowitz S
and McColl I: Immunogenicity of human amniotic epithelial cells
after transplantation into volunteers. Lancet. 2:1003–1005. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Faulk WP, Matthews R, Stevens PJ, Bennett
JP, Burgos H and His BL: Human amnion as an adjunct in wound
healing. Lancet. 1:1156–1158. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim JC and Tseng SC: Transplantation of
preserved human amniotic membrane for surface reconstruction in
severely damaged rabbit corneas. Cornea. 14:473–484. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zohar Y, Talmi YP, Finkelstein Y, Shvili
Y, Sadov R and Laurian N: Use of human amniotic membrane in
otolaryngologic practice. Laryngoscope. 97:978–980. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rennekampff HO, Dohrmann P, Föry R and
Fändrich F: Evaluation of amniotic membrane as adhesion prophylaxis
in a novel surgical gastroschisis model. J Invest Surg. 7:187–193.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
He Q, Li Q, Chen B and Wang Z: Repair of
flexor tendon defects of rabbit with tissue engineering method.
Chin J Traumatol. 5:200–208. 2002.PubMed/NCBI
|
|
16
|
Mligiliche N, Endo K, Okamoto K, Fujimoto
E and Ide C: Extracellular matrix of human amnion manufactured into
tubes as conduits for peripheral nerve regeneration. J Biomed Mater
Res. 63:591–600. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Parolini O, Alviano F, Bagnara GP, Bilic
G, Buhring HJ, Evangelista M, Hennerbichler S, Liu B, Magatti M,
Mao N, et al: Concise review: Isolation and characterization of
cells from human term placenta: Outcome of the first international
workshop on placenta derived stem cells. Stem Cells. 26:300–311.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Miki T, Lehmann T, Cai H, Stolz DB and
Strom SC: Stem cell characteristics of amniotic epithelial cells.
Stem Cells. 23:1549–1559. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Portmann Lanz CB, Schoeberlein A, Huber A,
Sager R, Malek A, Holzgreve W and Surbek DV: Placental mesenchymal
stem cells as potential autologous graft for pre- and perinatal
neuro regeneration. Am J Obstet Gynecol. 194:664–673. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sakuragawa N, Kakinuma K, Kikuchi A, Okano
H, Uchida S, Kamo I, Kobayashi M and Yokoyama Y: Human amnion
mesenchyme cells express phenotypes of neuroglial progenitor cells.
J Neurosci Res. 78:208–214. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wolbank S, Peterbauer A, Fahrner M,
Hennerbichler S, van Griensven M, Stadler G, Redl H and Gabriel C:
Dose-dependent immunomodulatory effect of human stem cells from
amniotic membrane: A comparison with human mesenchymal stem cells
from adipose tissue. Tissue Eng. 13:1173–1183. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhao P, Ise H, Hongo M, Ota M, Konishi I
and Nikaido T: Human amniotic mesenchymal cells have some
characteristics of cardiomyocytes. Transplantation. 79:528–535.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Stadler G, Hennerbichler S, Lindenmair A,
Peterbauer A, Hofer K, van Griensven M, Gabriel C, Redl H and
Wolbank S: Phenotypic shift of human amniotic epithelial cells in
culture is associated with reduced osteogenic differentiation in
vitro. Cytotherapy. 10:743–752. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lindenmair A, Wolbank S, Stadler G, Meinl
A, Peterbauer-Scherb A, Eibl J, Polin H, Gabriel C, van Griensven M
and Redl H: Osteogenic differentiation of intact human amniotic
membrane. Biomaterials. 31:8659–8665. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kikuchi T, Sakuta T and Yamaguchi T:
Intra-articular injection of collagenase induces experimental
osteoarthritis in mature rabbits. Osteoarthritis Cartilage.
6:177–186. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yoshioka M, Coutts RD, Amiel D and Hacker
SA: Characterization of a model of osteoarthritis in the rabbit
knee. Osteoarthritis Cartilage. 4:87–98. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mankin HJ, Dorfman H, Lippiello L and
Zarins A: Biochemical and metabolic abnormalities in articular
cartilage from osteo-arthritic human hips. II. Correlation of
morphology with biochemical and metabolic data. J Bone Joint Surg
Am. 53:523–537. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Buckland J: Osteoarthritis: Blocking
cartilage damage in a rat model of OA by intra-articular injection
of an amniotic membrane allograft. Nat Rev Rheumatol. 10:1982014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Willett NJ, Thote T, Lin AS, Moran S, Raji
Y, Sridaran S, Stevens HY and Guldberg RE: Intraarticular injection
of micronized dehydrated human amnion/chorion membrane attenuates
osteoarthritis development. Arthritis Res Ther. 16:R472014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Raines AL, Shih MS, Chua L, Su CW, Tseng
SC and O'Connell J: Efficacy of particulate amniotic membrane and
umbilical cord tissues in attenuating cartilage destruction in an
osteoarthritis model. Tissue Eng Part A. 23:12–19. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Vines JB, Aliprantis AO, Gomoll AH and
Farr J: Cryopreserved amniotic suspension for the treatment of knee
osteoarthritis. J Knee Surg. 29:443–450. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Díaz-Prado S, Rendal-Vázquez ME,
Muiños-López E, Hermida-Gómez T, Rodríguez-Cabarcos M,
Fuentes-Boquete I, de Toro FJ and Blanco FJ: Potential use of the
human amniotic membrane as a scaffold in human articular cartilage
repair. Cell Tissue Bank. 11:183–195. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lucero JM, Castiglioni AE, Hovanyecz P,
Gorla A, Berasategui O, Fedrigo GV and Lorenti AS: Culture of
chondrocytes on an acellular matrix derived from amniochorionic
membrane. Rev Asoc Argent Ortop Traumatol. 77:207–212. 2012.(In
Spanish). View
Article : Google Scholar
|
|
34
|
Bischoff M, Stachon T, Seitz B, Huber M,
Zawada M, Langenbucher A and Szentmáry N: Growth factor and
interleukin concentrations in amniotic membrane-conditioned medium.
Curr Eye Res. 42:174–180. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kim YI, Ryu JS, Yeo JE, Choi YJ, Kim YS,
Ko K and Koh YG: Overexpression of TGF-β1 enhances chondrogenic
differentiation and proliferation of human synovium-derived stem
cells. Biochem Biophys Res Commun. 450:1593–1599. 2014. View Article : Google Scholar : PubMed/NCBI
|