Introduction
Craniopharyngiomas (CPs) are rare, histologically
benign class of epithelial tumors arising from embryological
remnants of squamous epithelium of the craniopharyngeal duct, which
are commonly located in the sellar and suprasellar regions
(1,2). They account for 1.2–4.0% of all
intracranial tumors (3). CPs are
classified as grade I tumors by the World Health Organization (WHO)
(4), and though considered
histologically benign, they often present with a locally aggressive
growth pattern. Furthermore, exceptional cases of malignant
transformation have been reported (5). CPs pose numerous clinical challenges,
most of which are neurological signs and symptoms, due to their
intimate involvement and mass effect on adjacent structures,
including the hypothalamus, pituitary gland and optic chiasm. The
initial clinical manifestation at the time of diagnosis is often
dominated by non-specific symptoms of elevated intracranial
pressure, including headache and nausea. Further primary
manifestations include visual impairment (i.e. visual acuity
disorder and visual field defect; 62–84%) and endocrine
deficiencies (52–87%) (6–8). At present, surgical resection followed
by radiotherapy is the major treatment modality for CPs, although
resection may contribute to a high risk of endocrine, neurological
and hypothalamic post-operative complications due to the large
lesion size, the location and its association with vital
neurological structures (2,8).
The estimated annual incidence of CPs is 0.5–2 per
100,000 individuals, and 30–50% of all cases occur during childhood
and adolescence (9). CPs may be
classified into two major histological subtypes according to the
WHO classification of tumors of the central nervous system
(4): Adamantinomatous CP (ACP) and
papillary CP (PCP). However, transitional or mixed forms have also
been described (10). These two
subtypes are pathologically distinct and ACPs are more common than
PCPs (ratio, 9:1) (11). ACPs occur
in patients of all ages, with a bimodal age distribution; the first
peak occurs in the age window of 5–14 years and the second peak at
50–74 years (12). Histopathological
features of ACPs are the formation of wet keratin nodules, a
palisading basal layer of cells, loose aggregates of stellate
cells, as well as the presence of large areas of regressive
changes, i.e., multinucleated foreign body giant cells, hemosiderin
deposits, cholesterol crystals, inflammation and calcification. Wet
keratin is a hallmark of this variant (13). ACPs contain mutations in exon 3 of
the gene encoding β-catenin (CTNNB1) in 92% of cases, leading to
the overactivation of the WNT/β-catenin signaling pathway, which
has a crucial role in the tumorigenesis of ACP. However, the
mutation of the β-catenin gene is not detectable in PCP (14).
By contrast, the papillary variant most frequent in
adults aged 40–55 years (12).
Histologically, PCPs are predominantly solid and are characterized
by well-differentiated squamous epithelium with compact,
monomorphic sheets covering fibrovascular cores with miniature
capillaries and scattered immune cells, including macrophages and
neutrophils. Areas with marked regressive changes, including
cholesterol clefts, wet keratin, calcification and inflammation are
absent. Ciliated epithelium and goblet cells are only occasionally
observed, and the histological morphology resembles that of
Rathke's cleft cysts with squamous metaplasia (12,14,15).
Mutations in B-Raf proto-oncogene, serine/threonine kinase
(BRAF)V600E have been described in 95% of ACPs, causing
constitutive activation of the mitogen-activated protein kinase
pathway, thereby affecting cell division and differentiation
(16).
CTNNB1 and BRAF mutations are mutually exclusive and
specific for each subtype, indicating that ACP and PCP are two
biologically distinct entities. They display differences in
clinical manifestation, imaging characterization, histopathological
morphology and recurrence rate (12,17). In
the present study, 741 cases of CP were assessed and a
retrospective analysis of neuroendocrine dysfunction in ACP and PCP
patients prior to and after surgical removal of the mass was
performed.
Materials and methods
Patients
Patients with CP who underwent surgical resection at
the Department of Neurosurgery of Beijing Tiantan Hospital
affiliated to Capital Medical University (Beijing, China) between
January 2011 and December 2016 were included in the present study.
Subjects with an unknown pathological classification and those with
a history of endocrine disorders, including primary hypothyroidism,
adrenal insufficiency and hypogonadism, were excluded. The present
retrospective study was performed in accordance with the
declaration of Helsinki for research on humans and the protocol was
approved by the Ethics Committee of Beijing Tiantan Hospital
affiliated to Capital Medical University (Beijing, China).
Scoring methods
According to their pathological classification
(4), the patients were divided into
the ACP group and PCP group. A self-designed scoring method was
used to evaluate the neuroendocrine dysfunction in these two CP
subtypes prior to and after surgery.
The tumor mass effect was assessed by the three
major symptoms, namely intracranial pressure (headache and nausea),
loss of visual acuity and visual field defects. Each symptom was
assigned a score of 0 (negative) or 1 (positive). The total score
for the tumor mass effect therefore ranged from 0 to 3.
Hypothalamic dysfunction was assessed based on the
six manifestations, namely obesity and eating disorders, polydipsia
and polyuria, sleep disorder, cognitive dysfunction and personality
changes, imbalances in the regulation of body temperature and
memory loss. Each manifestation was scored as 1 (positive) or 0
(negative). The total score for hypothalamic dysfunction ranged
from 0 to 6.
The pituitary hormones, including
thyroid-stimulating hormone (TSH), adrenocorticotropic hormone
(ACTH), luteinizing hormone (LH)/follicle-stimulating hormone
(FSH), prolactin (PRL) and growth hormone, as well as the
corresponding target gland (thyroid, adrenal and gonadal) hormones,
including total triiodothyronine, free triiodothyronine, total
thyroxine, free thyroxine, cortisol, testosterone, progesterone and
estradiol, were measured to evaluate the function of the
pituitary-target gland axis. Pituitary-target gland axis
dysfunction was scored as follows: Low levels of TSH, or ACTH and
cortisol, or FSH and LH were scored as 1, while normal levels
scored as 0 to evaluate pituitary-thyroid, pituitary-adrenal or
pituitary-gonadal axis dysfunction, respectively. The total score
for pituitary-target gland axis dysfunction ranged from 0 to 3.
In addition, the incidence of central diabetes
insipidus was compared prior to and after the surgery within each
group and between the two groups by measuring the 24-h urine volume
and electrolytes.
Statistical analysis
All statistical analyses were performed by using
SPSS version 20.0 software (IBM Corp., Armonk, NY, USA). The
collected data were presented as the median (interquartile range)
or n (%). Outcomes were compared with the Wilcoxon rank-sum test
for continuous variables and the chi-square test for categorical
variables. P<0.05 was considered to indicate a statistically
significant difference.
Results
Age and sex distribution of ACP and
PCP patients
A total of 741 patients with CPs were included in
the present study, of which 622 had ACP and 119 PCP. In the ACP
group, 333 patients (53.5%) were males and 289 (46.5%) were
females. The median age of the patients was 14 years (interquartile
range, 7–40 years). In the PCP group, 83 patients (69.7%) were
males and the remaining 36 (30.3%) were females. The median age of
the patients was 43 years (interquartile range, 29–51 years).
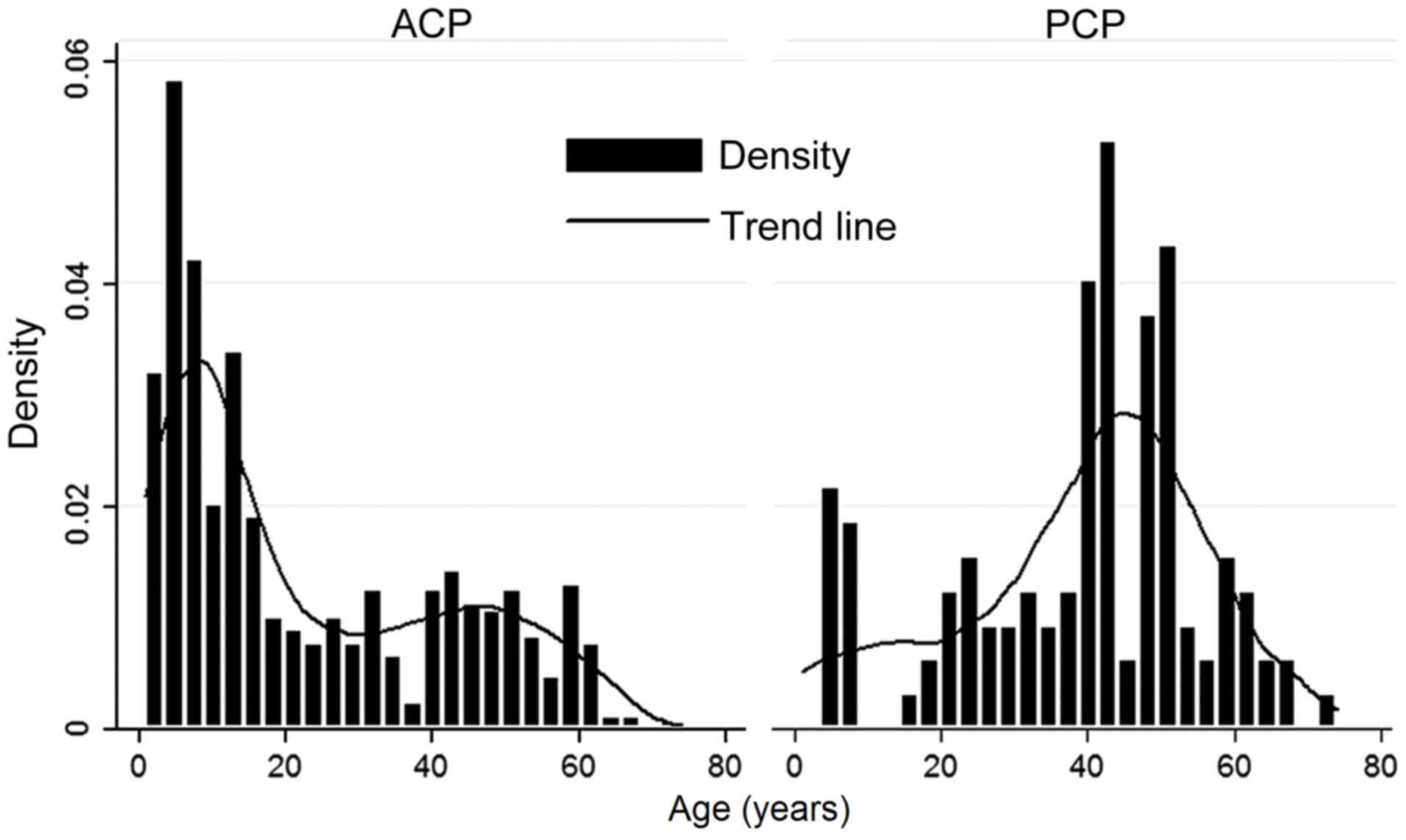
As presented in Fig.
1, a bimodal age distribution was observed in ACP patients,
with peaks at 1–15 years and 40–45 years. Most of the ACP cases
were of pediatric age. The PCP subtype primarily occurred in adults
aged 40–53 years. The difference in age between the ACP and PCP
groups was statistically significant (P<0.0001).
As presented in Table
I, the male/female ratio in the ACP group was 1.15 and that in
the PCP group was 2.31. Most of the CP patients were males. A
significant difference in the sex ratio between the two CP subtypes
was observed (P=0.001). In the ACP group, 52.7% of cases were aged
1–15 years, while this age group only accounted for 11.8% of PCP
cases; significant differences in the percentages of the age groups
(1–15 and >15 years) were observed within and between the ACP
and PCP groups (P<0.0001).
 | Table I.Age and sex distribution of ACP and
PCP patients. |
Table I.
Age and sex distribution of ACP and
PCP patients.
| Parameter | ACP (n=622) | PCP (n=119) | P-value |
|---|
| Age (years) | 14 (7–40) | 43 (29–51) | <0.0001 |
| 1–15 | 328 (52.7) | 14 (11.8) | <0.0001 |
|
>15 | 294 (47.3) | 105 (88.2) |
|
| Sex |
| M | 333 (53.5) | 83 (69.7) | 0.001 |
| F | 289 (46.5) | 36 (30.3) |
|
Comparison of neuroendocrine
dysfunction of ACP and PCP patients
Prior to surgery, the patients with a score of 1–3
for the tumor mass effect accounted for 88.1% in the ACP group and
94.1% in the PCP group. The average score in the PCP group was
significantly higher than that in the ACP group (P<0.0001).
After surgery, the patients with a score of 1–3 for the tumor mass
effect accounted for 53.5% in the ACP group and 70.6% in the PCP
group. The scores in the PCP group were significantly higher than
those in the ACP group (P<0.0001; Table II). After the surgery, the scores on
the tumor mass effect in the ACP group (P<0.0001) and the PCP
group (P<0.0001) were significantly decreased (Table III).
 | Table II.Comparison of neuroendocrine
dysfunction prior to and after the surgical removal of mass between
the two groups. |
Table II.
Comparison of neuroendocrine
dysfunction prior to and after the surgical removal of mass between
the two groups.
|
| Prior to surgery | After surgery |
|---|
|
|
|
|
|---|
| Parameter/score | ACP | PCP | P-value | ACP | PCP | P-value |
|---|
| Tumor mass
effect | 1.74±0.99 | 2.11±0.93 | <0.0001 | 1.05±1.02 | 1.37±0.97 | <0.0001 |
| 0 | 74 (11.9) | 7 (5.9) |
| 289 (46.5) | 35 (29.4) |
|
| 1 | 182 (29.3) | 24 (20.1) |
| 37 (5.9) | 12 (10.1) |
|
| 2 | 195 (31.4) | 37 (31.1) |
| 275 (44.2) | 65 (54.6) |
|
| 3 | 171 (27.4) | 51 (42.9) |
| 21 (3.4) | 7 (5.9) |
|
| Hypothalamic
dysfunction | 0.47±0.79 | 0.62±0.87 | 0.040 | 0.60±0.92 | 0.88±0.97 | <0.0001 |
| 0 | 408 (65.6) | 66 (55.5) |
| 354 (56.9) | 43 (36.1) |
|
| 1 | 158 (25.4) | 40 (33.6) |
| 213 (34.2) | 61 (51.3) |
|
| 2 | 41 (6.6) | 7 (5.9) |
| 23 (3.7) | 7 (5.9) |
|
| 3 | 9 (1.4) | 4 (3.4) |
| 18 (2.9) | 3 (2.5) |
|
|
4–6 | 6 (1.0) | 2 (1.6) |
| 14 (2.3) | 5 (4.2) |
|
| Pituitary-target
gland dysfunction | 0.94±1.00 | 1.63±1.22 | <0.0001 | 1.94±0.95 | 2.54±0.77 | <0.0001 |
| 0 | 275 (44.2) | 32 (26.9) |
| 54 (8.7) | 2 (1.7) |
|
| 1 | 170 (27.3) | 22 (18.5) |
| 135 (21.7) | 14 (11.8) |
|
| 2 | 118 (19.0) | 23 (19.3) |
| 225 (36.2) | 21 (17.6) |
|
| 3 | 59 (9.5) | 42 (35.3) |
| 208 (33.4) | 82 (68.9) |
|
| Central diabetes
insipidus | 153 (24.6) | 41 (34.5) | 0.030 | 267 (42.9) | 78 (65.5) | <0.0001 |
 | Table III.Comparison of neuroendocrine
dysfunction prior to and after the surgical removal of mass within
each group. |
Table III.
Comparison of neuroendocrine
dysfunction prior to and after the surgical removal of mass within
each group.
|
| ACP group | PCP group |
|---|
|
|
|
|
|---|
| Parameter | Prior to
surgery | After surgery | P-value | Prior to
surgery | After surgery | P-value |
|---|
| Tumor mass
effect | 1.74±0.99 | 1.05±1.02 | <0.0001 | 2.11±0.93 | 1.37±0.97 | <0.0001 |
| 0 | 74 (11.9) | 289 (46.5) |
| 7 (5.9) | 35 (29.4) |
|
| 1 | 182 (29.3) | 37 (5.9) |
| 24 (20.1) | 12 (10.1) |
|
| 2 | 195 (31.4) | 275 (44.2) |
| 37 (31.1) | 65 (54.6) |
|
| 3 | 171 (27.4) | 21 (3.4) |
| 51 (42.9) | 7 (5.9) |
|
| Hypothalamic
dysfunction | 0.47±0.79 | 1.60±0.92 | 0.004 | 0.62±0.87 | 0.88±0.98 | 0.008 |
| 0 | 408 (65.6) | 354 (56.9) |
| 66 (55.5) | 43 (36.1) |
|
| 1 | 158 (25.4) | 213 (34.2) |
| 40 (33.6) | 61 (51.3) |
|
| 2 | 41 (6.6) | 23 (3.7) |
| 7 (5.9) | 7 (5.9) |
|
| 3 | 9 (1.4) | 18 (2.9) |
| 4 (3.4) | 3 (2.5) |
|
|
4–6 | 6 (1.0) | 14 (2.3) |
| 2 (1.6) | 5 (4.2) |
|
| Pituitary-target
gland dysfunction | 0.94±1.00 | 1.94±0.95 | <0.0001 | 1.63±1.22 | 2.54±0.77 | <0.0001 |
| 0 | 275 (44.2) | 54 (8.7) |
| 32 (26.9) | 2 (1.7) |
|
| 1 | 170 (27.3) | 135 (21.7) |
| 22 (18.5) | 14 (11.8) |
|
| 2 | 118 (19.0) | 225 (36.2) |
| 23(19.3) | 21 (17.6) |
|
| 3 | 59 (9.5) | 208 (33.4) |
| 42 (35.3) | 82 (68.9) |
|
| Central diabetes
insipidus | 153 (24.6) | 267 (42.9) | <0.0001 | 41 (34.5) | 78 (65.5) | <0.0001 |
The patients with a score of 1–6 on hypothalamic
dysfunction accounted for 34.4% in the ACP group and 44.5% in the
PCP group prior to surgery. Patients with PCP had significantly
higher scores than patients with ACP (P=0.040). After the surgery,
the patients with a score of 1–6 on hypothalamic dysfunction
accounted for 43.1% in the ACP group and 63.9% in the PCP group.
The hypothalamic dysfunction scores in patients with PCP were
significantly higher than those in patients with ACP (P<0.0001;
Table II). After the surgery, the
scores on hypothalamic dysfunction in ACP (P=0.004) and PCP
patients (P=0.008) were significantly increased (Table III).
The patients with a pituitary-target gland axis
dysfunction score of 1–3 accounted for 55.8% in the ACP group and
73.1% in the PCP group prior to surgery. The PCP patients had
significantly higher scores than the ACP patients (P<0.0001).
After the surgery, patients with a pituitary-target gland axis
dysfunction score of 1–3 accounted for 91.3% in the ACP group and
98.3% in the PCP group. The scores in the PCP group were
significantly higher than those in the ACP group (P<0.0001;
Table II). After the surgery, the
scores on the pituitary-target gland axis dysfunction were
significantly increased in the ACP (P<0.0001) and PCP groups
(P<0.0001; Table III).
Central diabetes insipidus occurred in 24.6% of
cases with ACP and 34.5% of cases with PCP prior to surgery. After
the surgery, 42.9% of ACP patients and 65.5% of PCP patients
presented with central diabetes insipidus. Prior to and after the
surgery, the prevalence of central diabetes insipidus in the PCP
group was significantly higher than that in the ACP group (P=0.030
and P<0.0001, respectively). After surgical removal of the mass,
the incidence of central diabetes insipidus increased significantly
from 24.6 to 42.9% in the ACP group (P<0.0001), and from 34.5 to
65.5% in the PCP group (P<0.0001).
Discussion
CPs are non-neuroepithelial intracerebral neoplasms
with a variable histological appearance. They frequently behave
aggressively with invasion of the surrounding vital neurologic
structures, including the optic nerve and hypothalamic-pituitary
axes, consequently causing hypopituitarism and hypothalamic
syndromes (7). Depending on patient
age, location and size of the tumor, as well as extension to
adjacent structures, the clinical presentation of CPs is variable.
Accordingly, the management of CPs remains a challenge for
neurosurgeons. At present, CPs may be treated and controlled but
not cured, and studies have reported that recurrence rates after
radical gross total resection of CP with hypothalamic involvement
were similar to the progression rates after limited surgery,
resulting in residual tumor (18).
In addition, due to the inflammatory adhesions between the tumor
and surrounding brain tissue, further damage may occur during
surgery and/or radiotherapy. The surgical removal of the tumor
tissue may cause irreversible damage to the hypothalamic-pituitary
target gland axes, affecting the neuroendocrine function. Most
patients require lifelong pituitary hormone replacement therapy.
Visual impairment, hormonal disturbances of hypothalamus and
pituitary glands, obesity, cognitive impairment and personality
changes are common complications caused not only by the growth of
the tumor but also frequently as a consequence of treatment with
surgery and/or radiation therapy (15). Pre-operative demonstration of the
extensive adherence of the large tumor to hypothalamic structures
may be associated with a poor endocrinological outcome after
surgical resection (19).
ACP and PCP subtypes are completely distinctive
entities, which differ in their histological, genetic and clinical
behavior. Esheba and Hassan (20)
have demonstrated that β-catenin mutations and/or nuclear
accumulation are diagnostic hallmarks of ACP and are helpful in the
differential diagnosis between these two subtypes. The
histopathological classification has clinical significance and
prognostic value. Szeifert et al (17) have indicated that the pathological
classification of CPs may influence the post-operative outcome, and
the ACP subtype is associated with a high recurrence rate and poor
prognosis. The aim of the present study was to compare the
neuroendocrine dysfunction prior to and after surgical resection
within and between the two histopathological types of CP.
The present study included 622 cases of ACP and 119
cases of PCP. CPs may be detected at any age. The age distribution
of ACPs exhibited a bimodal distribution with peak incidence rates
in children and adolescents aged 1–15 years and adults aged 40–45
years. Apart from a small proportion of pediatric cases, PCPs
almost exclusively occur in adults aged 40–53 years. The difference
in age between the ACP and PCP groups was statistically significant
(P<0.0001). The above results were consistent with those of a
previously published study (12).
ACPs are the most common form of non-neuroepithelial neoplasm in
children, accounting for 5–10% of intracranial tumors in this
population (21). An equal sex ratio
has been reported in population-based studies from the United
States (22) and Finland (23). However, in the present study, males
were more commonly affected than females (P=0.001). An admission
bias may have been present, as the current study was a
single-center retrospective cohort study.
Neuroendocrinological evaluation was performed
during the pre- and post-operative periods using a self-designed
scoring method. The results of the present study indicated that the
scores on the tumor mass effect, hypothalamic dysfunction and
pituitary-target gland axis dysfunction, as well as the incidence
of central diabetes insipidus in PCP were all significantly higher
than those in ACP regardless of whether surgery had been performed
(all P<0.05). This indicated that the symptoms associated with
neuroendocrine dysfunction were more severe among PCP patients with
a greater degree of damage. The tumor mass effect scores in ACP and
PCP patients were decreased after surgery (all P<0.05). Clinical
symptoms arising from the tumor mass effect were relieved. Visual
impairment as an initial clinical symptom of CPs is reported in
more than half of affected patients, and vision was reported to
have improved post-operatively in 41–48% of patients with
pre-operative visual impairment (24).
However, in the present study, the scores on the
hypothalamic dysfunction and the pituitary-target gland axis
dysfunction, as well as the incidence of central diabetes insipidus
in ACP and PCP patients were all increased after surgical removal
of the mass (all P<0.05). The clinical symptoms of hypothalamic
dysfunction and pituitary-target gland axis dysfunction were
aggravated in these two subtypes. Most patients with CPs presented
with multiple deficits of hypothalamic-pituitary function at the
time of diagnosis. Surgical removal of the mass may further affect
hypothalamic and pituitary function due to the proximity of the
tumor to the hypothalamic-pituitary axes, aggravating hypothalamic
dysfunction and endocrine disorders; in severe cases, the condition
may be life-threatening (24,25).
Hypothalamic neuroendocrine dysfunction, including obesity,
behavioral changes, disturbed circadian rhythm and sleep disorder,
imbalances in the regulation of the body temperature, polydipsia
and memory loss, was reported in 35% of CP patients at diagnosis
(1). The rate of hypothalamic
dysfunction markedly increases following radical surgery to up to
65–80% (26).
Pituitary hormone deficiencies are common in
patients with CPs. Prior to surgery, 40–87% of patients have been
reported to have at least one hormonal deficit, and post-surgical
pituitary hormone deficiencies occur in up to 85–95% of patients.
Central diabetes insipidus frequently occurs prior to (17–27% of
cases) or after surgery (40–93% of cases) (6). Anti-diuretic hormone is synthesized in
the supraoptic nucleus and the paraventricular nucleus of the
hypothalamus, and is transported through the pituitary stalk and
stored in the posterior pituitary gland. This hormone is released
into the circulation in response to changes in plasma osmotic
pressure, which regulates the amount of urine. Patients with ACP or
PCP may have central diabetes insipidus due to the tumor
compressing the pituitary stalk. The present study indicated that
surgery may damage or even sever the pituitary stalk, which may
aggravate central diabetes insipidus. This is also supported by the
post-operative images displaying an abnormal structure or absence
of the pituitary stalk (results not shown).
The present study compared the neuroendocrine
dysfunction prior to and after surgical treatment between and
within the ACP and PCP groups. Systematic evaluation of the
functional status of hypothalamic-pituitary-target gland axes in
different histological types of CPs after removal of the tumor
in situ may contribute to the formulation of individualized
target hormone replacement therapy protocols and neuroendocrine
rehabilitation therapy. At the genetic level, the apparent mutual
exclusivity of CTNNB1 and BRAFV600E mutations in the CP variants is
a potential target for pharmaceutical therapy (13).
Of note, the present study has certain limitations.
The present study included more male than female cases, while
previous studies reported equal sex ratios. This may be caused by
the high male sex ratio at birth during the past decades in China.
Another possible reason is that due to the female discrimination in
rural areas of China, females with severe diseases are less likely
to be treated locally and referred to higher-level hospitals. In
addition, due to the retrospective nature of the present study,
bias may have been introduced in the results.
In conclusion, the PCP variant exhibited a greater
damage to the neuroendocrine function compared with the ACP variant
prior to and after surgery. Further study of neuroendocrine
dysfunction in the two histologic subtypes of CPs with larger
sample sizes is warranted to confirm and expand the results of the
present study. Besides the removal of the mass effect, the
treatment of patients with CP requires to focus on and monitor
long-term changes in neuroendocrine function. To improve the
quality of life of affected patients, functional reconstruction of
the hypothalamic-pituitary-gonadal axis should be emphasized.
Acknowledgements
Not applicable.
Funding
The present study was supported by the
Characteristic Project on Capital Clinical Research, Beijing
Municipal Science and Technology Committee (no:
Z181100001718122).
Availability of data and materials
The analysed data sets generated during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YF collected and analyzed clinical data, and
prepared the manuscript; LZ designed the trial and prepared the
manuscript; and MN and YW collected clinical data. The final
version of the manuscript has been read and approved by all
authors, and each author believes that the manuscript represents
honest work.
Ethical approval and consent to
participate
The present study was approved by the Ethics
Committee of Beijing Tiantan Hospital affiliated to Capital Medical
University (Beijing, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CPs
|
craniopharyngiomas
|
|
ACP
|
adamantinomatous CP
|
|
PCP
|
papillary CP
|
|
WHO
|
World Health Organization
|
|
FSH
|
follicle-stimulating hormone
|
|
LH
|
luteinizing hormone
|
|
ACTH
|
adrenocorticotropic hormone
|
|
TSH
|
thyroid-stimulating hormone
|
References
|
1
|
Elliott RE and Wisoff JH: Surgical
management of giant pediatric craniopharyngiomas. J Neurosurg
Pediatr. 6:403–416. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Poretti A, Grotzer MA, Ribi K, Schonle E
and Boltshauser E: Outcome of craniopharyngioma in children:
Long-term complications and quality of life. Dev Med Child Neurol.
46:220–229. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Qi ST, Zhou J, Pan J, Zhang C, Silky C and
Yan XR: Epithelial-mesenchymal transition and clinicopathological
correlation in craniopharyngioma. Histopathology. 61:711–725. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aquilina K, Merchant TE, Rodriguez-Galindo
C, Ellison DW, Sanford RA and Boop FA: Malignant transformation of
irradiated craniopharyngioma in children: Report of 2 cases. J
Neurosurg Pediatr. 5:155–161. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Daubenbuchel AM and Muller HL:
Neuroendocrine disorders in pediatric craniopharyngioma patients. J
Clin Med. 4:389–413. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Balcazar-Hernandez L, Vargas-Ortega G,
Valverde-Garcia Y, Mendoza-Zubieta V and Gonzalez-Virla B:
Anorexia-cachexia syndrome-like hypothalamic neuroendocrine
dysfunction in a patient with a papillary craniopharyngioma.
Endocrinol Diabetes Metab Case Rep 2017. 2017. View Article : Google Scholar
|
|
8
|
Caldarelli M, Massimi L, Tamburrini G,
Cappa M and Di Rocco C: Long-term results of the surgical treatment
of craniopharyngioma: The experience at the Policlinico Gemelli,
Catholic University, Rome. Childs Nerv Syst. 21:747–757. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nielsen EH, Feldt-Rasmussen U, Poulsgaard
L, Kristensen LO, Astrup J, Jørgensen JO, Bjerre P, Andersen M,
Andersen C, Jørgensen J, et al: Incidence of craniopharyngioma in
Denmark (n=189) and estimated world incidence of craniopharyngioma
in children and adults. J Neurooncol. 104:755–763. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Karavitaki N: Management of
craniopharyngiomas. J Endocrinol Invest. 37:219–228. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lubuulwa J and Lei T: Pathological and
topographical classification of craniopharyngiomas: A literature
review. J Neurol Surg Rep. 77:e121–e127. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Holsken A, Sill M, Merkle J, Schweizer L,
Buchfelder M, Flitsch J, Fahlbusch R, Metzler M, Kool M, Pfister
SM, et al: Adamantinomatous and papillary craniopharyngiomas are
characterized by distinct epigenomic as well as mutational and
transcriptomic profiles. Acta Neuropathol Commun. 4:202016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Martinez-Barbera JP: Molecular and
cellular pathogenesis of adamantinomatous craniopharyngioma.
Neuropathol Appl Neurobiol. 41:721–732. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Martinez-Barbera JP and Buslei R:
Adamantinomatous craniopharyngioma: Pathology, molecular genetics
and mouse models. J Pediatr Endocrinol Metab. 28:7–17. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Brastianos PK and Santagata S: ENDOCRINE
TUMORS: BRAF V600E mutations in papillary craniopharyngioma. Eur J
Endocrinol. 174:R139–R144. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Brastianos PK, Taylor-Weiner A, Manley PE,
Jones RT, Dias-Santagata D, Thorner AR, Lawrence MS, Rodriguez FJ,
Bernardo LA, Schubert L, et al: Exome sequencing identifies BRAF
mutations in papillary craniopharyngiomas. Nat Genet. 46:161–165.
2014. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Szeifert GT, Sipos L, Horvath M, Sarker
MH, Major O, Salomváry B, Czirják S, Bálint K, Slowik F, Kolonics
L, et al: Pathological characteristics of surgically removed
craniopharyngiomas: Analysis of 131 cases. Acta Neurochir (Wien).
124:139–143. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Muller HL: Craniopharyngioma: Long-term
consequences of a chronic disease. Expert Rev Neurother.
15:1241–1244. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lopez-Serna R, Gomez-Amador JL,
Barges-Coll J, Nathal-Vera E, Revuelta-Gutiérrez R, Alonso-Vanegas
M, Ramos-Peek M and Portocarrero-Ortiz L: Treatment of
craniopharyngioma in adults: Systematic analysis of a 25-year
experience. Arch Med Res. 43:347–355. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Esheba GE and Hassan AA: Comparative
immunohistochemical expression of β-catenin, EGFR, ErbB2, and p63
in adamantinomatous and papillary craniopharyngiomas. J Egypt Natl
Canc Inst. 27:139–145. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Puget S, Garnett M, Wray A, Grill J,
Habrand JL, Bodaert N, Zerah M, Bezerra M, Renier D, Pierre-Kahn A
and Sainte-Rose C: Pediatric craniopharyngiomas: Classification and
treatment according to the degree of hypothalamic involvement. J
Neurosurg. 106:3–12. 2007.PubMed/NCBI
|
|
22
|
Bunin GR, Surawicz TS, Witman PA,
Prestonmartin S, Davis F and Bruner JM: The descriptive
epidemiology of craniopharyngioma. J Neurosurg. 89:547–551. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sorva R and Heiskanen O: Craniopharyngioma
in Finland. A study of 123 cases. Acta Neurochir (Wien). 81:85–89.
1986. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Müller HL: Consequences of
craniopharyngioma surgery in children. J Clin Endocrinol Metab.
96:1981–1991. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Muller HL: Craniopharyngioma and
hypothalamic injury: Latest insights into consequent eating
disorders and obesity. Curr Opin Endocrinol Diabetes Obes.
23:81–89. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Scarfone RJ, Loiselle JM, Wiley JF II,
Decker JM, Henretig FM and Joffe MD: Nebulized dexamethasone versus
oral prednisone in the emergency treatment of asthmatic children.
Ann Emerg Med. 26:480–486. 1995. View Article : Google Scholar : PubMed/NCBI
|