Introduction
Peripheral arterial disease (PAD), caused by
occlusion of the arteries extending to the lower extremities, is a
growing medical problem that affects >200 million individuals
worldwide (1–3). Delivery of oxygen, nutrients and other
mediators to ischemic sites in patients with PAD via the blood
circulation is dependent on neovascularization, including
angiogenesis and arteriogenesis (4–7).
However, at present, no medications are available to induce
functional neovascularization and thereby treat patients with PAD
(8–10).
Curcumin is a bright-yellow compound isolated from
the root of Curcuma longa, which is a member of the ginger
family, and has traditionally been used to treat a variety of
clinical conditions, including cancer, Alzheimer's disease and
insulin resistance (11–13). Previous studies suggested that
curcumin induces therapeutic angiogenesis and improves hind limb
perfusion recovery after surgical femoral artery ligation in
diabetic mice (14). However,
whether curcumin provides a therapeutic benefit in PAD without
diabetes has remained elusive. Considering that a large proportion
of patients with PAD do not have any accompanying diabetes mellitus
(2,15), the present study was performed in
order to investigate the potential effects of curcumin on perfusion
recovery in a non-diabetic mouse model of PAD, and to elucidate the
mechanism of action of angiogenic microRNA.
Materials and methods
Murine hindlimb ischemia (HLI)
Unilateral HLI was generated via surgical ligation
and excision of the femoral artery to create an experimental PAD
model, as described previously (16). In the present study, 32 male BALB/c
mice (age, 14 weeks; weight, 20–25 g) were anesthetized with 3%
isoflurane. Immediately after HLI, the mice were randomized into
two groups (n=16 in each): In the control group, the mice received
300 µl olive oil only, and in the curcumin group, the mice received
1,000 mg/kg curcumin (Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany) in 300 µl olive oil. All mice received treatment by
gavage, once per day for two weeks.
All procedures of the present study followed the
Guide for the Care and Use of Laboratory Animals published by the
US National Institutes of Health (publication no. 85–23, revised
1996). The experimental protocol was approved by the Committee on
Animal Experiments of Wuhan University School of Medicine (Wuhan,
China). The BALB/c mice were obtained from the Experimental Animal
Center of Wuhan University (Wuhan, China). Mice were housed in a
specific pathogen-free laboratory environment at a temperature of
25°C and a constant humidity of 50±10% with free access to food and
water under a 12-h light/dark cycle.
Perfusion recovery
Mice were anesthetized and subjected to a
non-invasive assessment of ischemic and non-ischemic limb perfusion
using a laser Doppler perfusion imaging system (LDPI; Perimed
Instruments AB, Stockholm, Sweden) at 0, 7, 14, 21 and 28 days
after HLI, as described previously (17). Perfusion of the ischemic limb was
quantified and normalized to the non-surgical limb, and the results
are presented as a percentage of the values in the non-ischemic
side.
Immunofluorescence
Mice were sacrificed in a CO2 chamber at
28 days after HLI, and the gastrocnemius anterior muscles from the
ischemic side were cryo-sectioned in 6-µm sections. Anti-CD31
antibody (rat anti-mouse CD31; cat. no. 550274; 1:100 dilution; BD
Pharmingen, San Jose, CA, USA) was applied to acetone-fixed
sections (fixed for −20°C for 10 min) of ischemic gastrocnemius
muscle tissue, followed by incubation overnight at 4°C with an
Alexa Fluor 555 anti-rabbit secondary antibody (1:400 dilution;
cat. no. BM2004; Boster Biological Technology, Wuhan, China).
Images were acquired using an Olympus IX71 high-magnification
microscope (Olympus, Tokyo, Japan). Capillary densities were
analyzed by counting in four randomly selected high-power fields
(magnification, ×100) and expressed as the number of
CD31+ cells per field.
RNA isolation and reverse
transcription-quantitative polymerase chain reaction (RT-qPCR)
analysis
Total RNA was isolated from tissue or cells using a
PureLink® RNA Mini kit (cat. no. 12183018A; Thermo
Fisher Scientific, Inc., Waltham, MA, USA) according to the
manufacturer's protocol. Real-time qPCR for microRNA (miR)
quantification and a miR assay (assay no. 001090; cat. no: 4427975;
Thermo Fisher Scientific, Inc.) were used for RT-qPCR according to
the manufacturer's protocols. Small nucleolar RNA MBII-202 (assay
no. 001095; Thermo Fisher Scientific, Inc.) served as an internal
control for miR quantification. The quantification cycle (Cq) value
obtained for each gene was normalized to that of the respective
internal control (ΔCq). Each gene was then further normalized to
the average ΔCq value of its control group (ΔΔCq). The final fold
expression changes were calculated using the 2−ΔΔCq
equation (18).
Cell culture and in vitro
transfection
Human umbilical vein endothelial cells (HUVECs) were
isolated from a donor umbilical cord, as described previously
(19), and then cultured in
endothelial cell growth medium (Cell Applications, Inc., San Diego,
CA, USA) supplemented with 10% fetal bovine serum (Wuhan Boster
Biological Technology). To mimic endothelial cells under ischemic
conditions as a model for HLI, HUVECs were subjected to hypoxia (2%
oxygen; BioSpherix, Lacona, NY, USA) and serum starvation (HSS).
The use of HUVECs was approved by the Institutional Review Boards
of Wuhan University (Wuhan, China).
In vitro transfection of miRNA inhibitors was
used to knock down miR-93 expression in HUVECs, as described
previously (20). In brief, a
reverse transfection protocol using neofx transfection agent
(Ambion, Austin, TX, USA) was used to transfect miR-93 inhibitor,
or miRNA inhibitor negative control (cat. no. 4464084; Thermo
Fisher Scientific, Inc) into HUVECs for 48 h.
Cellular viability and angiogenesis
assay
For assessment of cellular viability, HUVECs
transfected with an miR-93 inhibitor or control miR were seeded
into a 96-well plate at a density of 1×104 cells/well
(n=8/group), and then cultured under HSS conditions with/without
curcumin (10 µM) for 48 h. Subsequently, the cell viability was
assessed using tetrazolium dye incorporation (BioVision, Milpitas,
CA, USA).
In vitro angiogenesis assays were performed
as previously described (20), under
HSS conditions. In brief, HUVECs transfected with miR-93 inhibitor
or control were seeded in 96-well dishes coated with growth
factor-reduced Matrigel (BD Biosciences, Franklin Lakes, NJ, USA)
at a density of 1×104 cells/well, and then exposed to
HSS conditions in the presence of curcumin (10 µM) or vehicle alone
for 12 h to assess tube formation. Each set of conditions was
replicated in 6 wells from the 96-well dish. The degree of tube
formation was determined by measuring the length of the tubes and
the number of loops in each well under a magnification, ×40 using
ImageJ software 1.15K (National Institutes of Health, Bethesda, MD,
USA). Each experiment was repeated using at least two different
batches of HUVECs in total.
Statistical analysis
Statistical analysis was performed with GraphPad
Prism 7.0 software (GraphPad Inc., La Jolla, CA, USA). An unpaired
t-test was used for comparisons between two groups; comparisons
between ≥3 groups were performed with one-way analysis of variance
and Tukey's post-hoc test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Curcumin improves perfusion recovery,
angiogenesis and causes upregulation of miR-93 expression in
experimental PAD
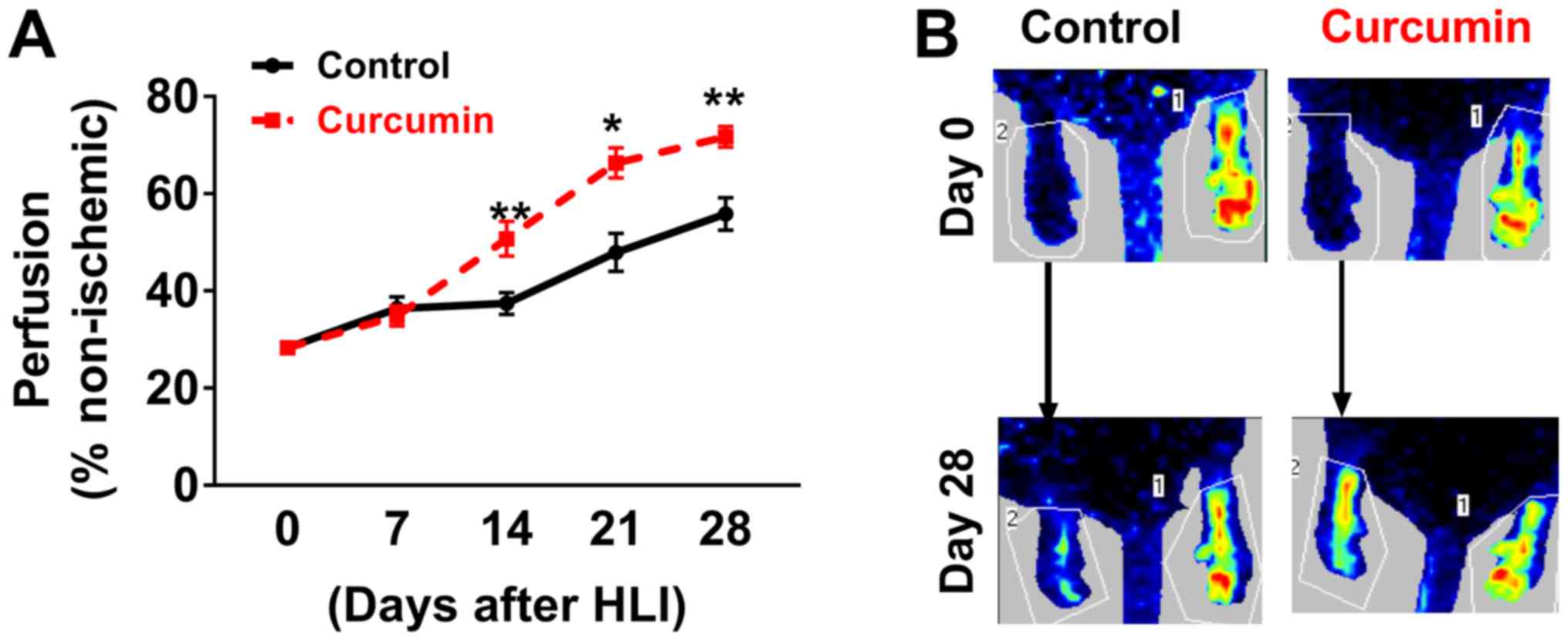
LDPI imaging revealed that BALB/c mice receiving
curcumin experienced better perfusion recovery at 14, 21 and 28
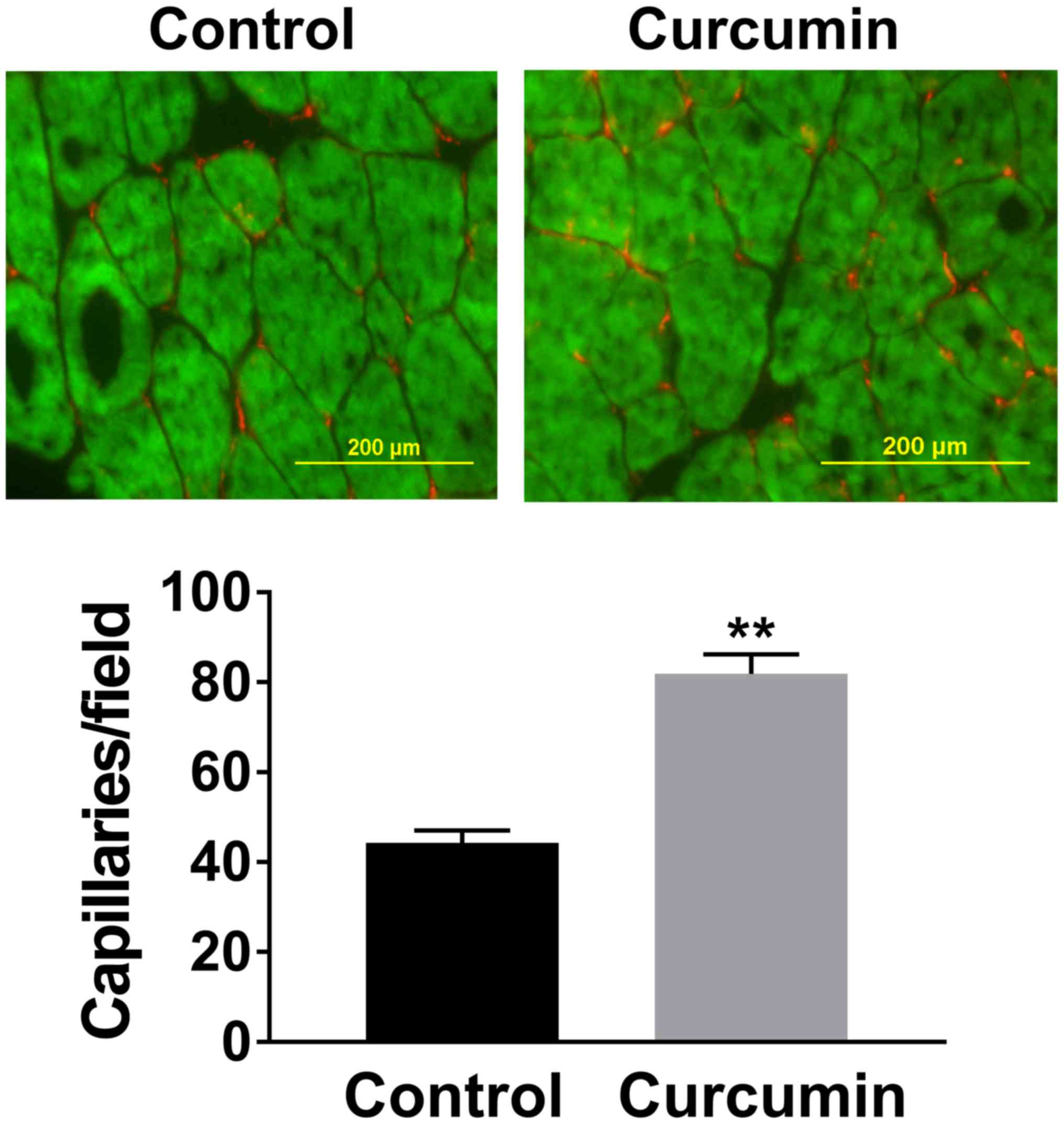
days after HLI compared with those receiving olive oil (Fig. 1). Immunostaining with CD31 to
visualize capillaries indicated that after 28 days of post-HLI
treatment, the gastrocnemius anterior muscles from the ischemic
side of the mice receiving curcumin exhibited a higher capillary
density compared with those receiving olive oil (81.9±4.3 vs.
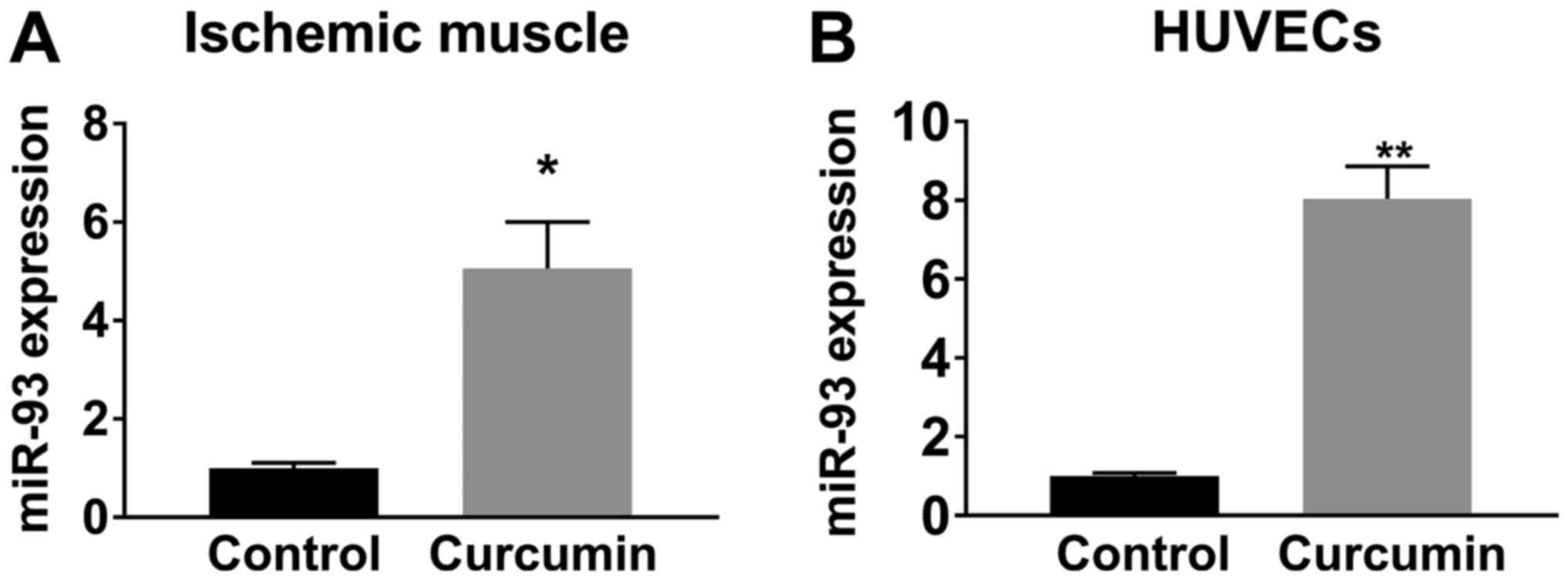
44.3±2.7 capillaries/field, n=10/group; P<0.01; Fig. 2). A previous study indicated that
miR-93 is a potent regulator of angiogenesis in the ischemic limbs
of patients with PAD and in animal models (20). Given that curcumin induced
angiogenesis as a therapeutic benefit after HLI, the level of
miR-93 was assessed, revealing that curcumin treatment increased
miR-93 expression by ~5 fold (n=5/group) in the ischemic muscle at
7 days after HLI (Fig. 3A).
Curcumin therapy increases
angiogenesis under hypoxia
In HUVECs cultured under HSS conditions (mimicking
in vivo ischemia), curcumin treatment for 12 h significantly
increased miR-93 expression (Fig.
3B), consistent with the in vivo results obtained with
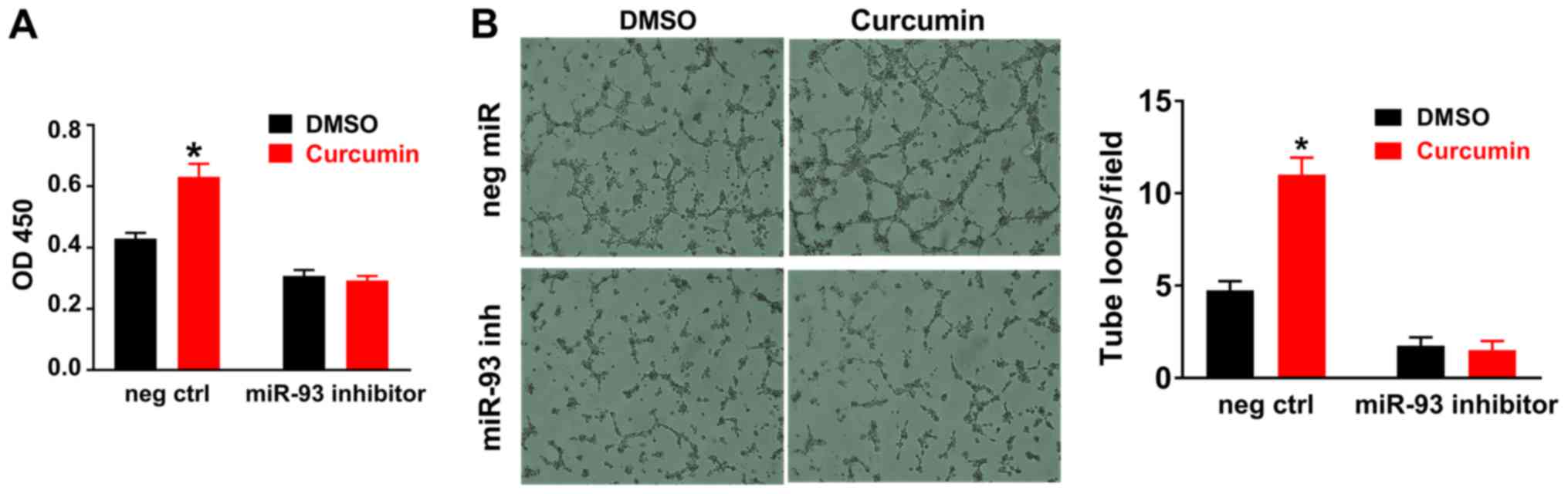
ischemic muscle tissue. In addition, curcumin increased endothelial
cell viability (Fig. 4A) and tube
formation (Fig. 4B) in vitro
under HSS conditions. It was also revealed that miR-93 knockdown
using a miR-93 inhibitor reduced angiogenesis and curcumin-induced
angiogenesis and endothelial cell survival were attenuated when
miR-93 was knocked down by an miR-93 inhibitor in vitro
(Fig. 4A and B).
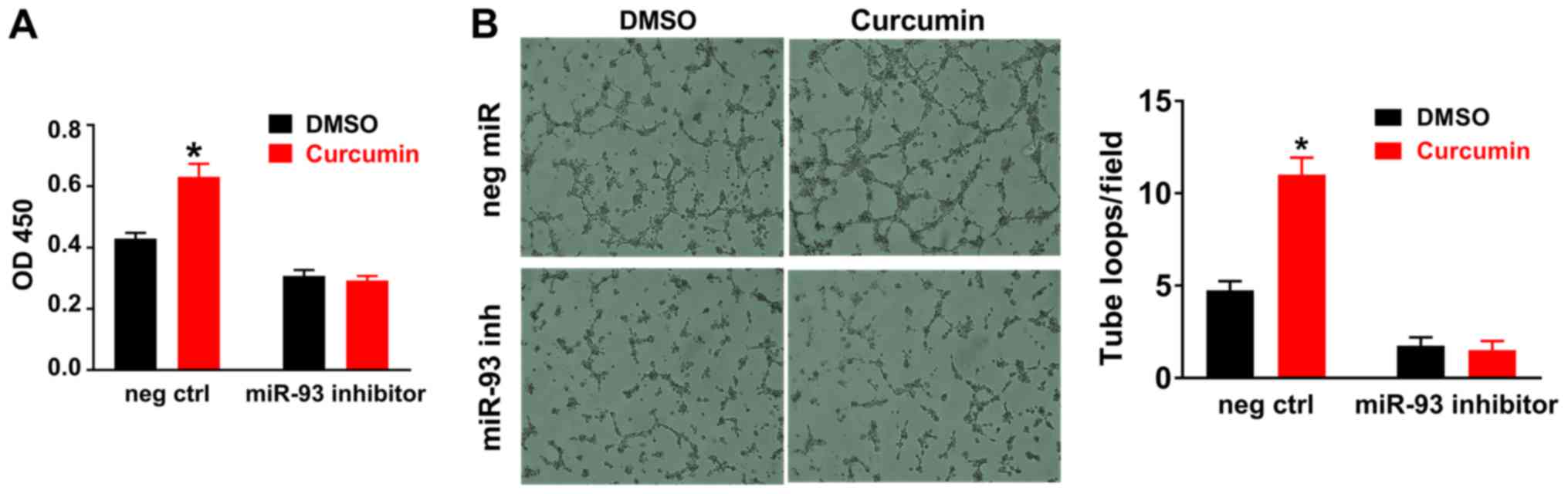 | Figure 4.Curcumin treatment increases the cell
viability and tube formation of cultured HUVECs under HSS
conditions. (A) HUVECs were incubated with curcumin or DMSO for 48
h, and curcumin significantly increased the cell viability. (B)
HUVECs were seeded on 96-well plates coated with Matrigel; curcumin
treatment for 12 h significantly increased tube formation, as
indicated by increased loops (magnification, ×40). DMSO (0.02%,
volume concentration in the medium) served as a negative control
for curcumin, as curcumin used in the in vitro study was
dissolved in DMSO. miR-93 knockdown reduces angiogenesis in
vitro, furthermore following miR-93 knockdown, curcumin did not
alter endothelial cell viability or tube formation. Values are
expressed as the mean ± standard error of the mean. *P<0.05 vs.
control. HUVECs, human umbilical cord vascular endothelial cells;
HSS, hypoxia and serum starvation; OD 450, optical density at 450
nm; neg ctrl, negative control; miR, microRNA; inh, inhibitor;
DMSO, dimethylsulfoxide. |
Discussion
To the best of our knowledge, the present study is
the first to demonstrate that curcumin improves angiogenesis and
perfusion recovery in non-diabetic experimental PAD. Furthermore,
it was indicated that curcumin treatment increased miR-93
expression in ischemic muscle tissue and cultured endothelial
cells, and that miR-93 elevation may be involved in
curcumin-induced therapeutic angiogenesis under ischemic
conditions.
Previous studies have demonstrated that curcumin has
a protective effect on ischemic limbs in diabetic mouse models
(14,15). However, the effects of curcumin on
limb ischemia in non-diabetic subjects have remained to be
assessed. Angiogenesis is an important process of new blood vessel
formation, which includes the stimulation, promotion and
stabilization of endothelial cells; it is a key factor in the
perfusion recovery of tissue following ischemia. Curcumin has a
pro-angiogenic effect on wound healing and HLI in type 1 diabetes
(21). However, it has been
indicated to have anti-angiogenic effects in pituitary adenomas and
hepatic cancer (11,22). Taken together, curcumin exhibits
bi-directional effects under different disease conditions.
Therefore, under non-diabetic conditions, the effects of curcumin
on angiogenesis in PAD require further study.
A noteworthy result of the present study is that
curcumin improves perfusion recovery after HLI through the
induction of miR-93 upregulation in ischemic endothelial cells.
miRs are a group of small non-coding RNAs containing ~22
nucleotides that function through RNA silencing and the
post-transcriptional regulation of gene expression (23–27).
miR-93 has been reported to act as a potent mediator to induce
neovascularization in PAD. In a mouse model of PAD, miR-93
knockdown was reported to reduce angiogenesis and perfusion
recovery; conversely, miR-93 overexpression improved perfusion
recovery and angiogenesis by targeting cell cycle regulatory
pathways (21). A more recent study
indicated that miR-93 induces macrophage M2 polarization, which
eventually leads to enhanced angiogenesis and arteriogenesis in a
mouse model of PAD (28). In the
present study, treatment with curcumin was identified to cause an
upregulation of miR-93 in ischemic muscle tissue and endothelial
cells. In addition, miR-93 inhibition blocked curcumin-induced
therapeutic angiogenesis in vitro. This may suggest that
miR-93 is involved in the therapeutic effects of curcumin on
PAD.
At present, limited therapies are available for PAD,
and no known treatment is capable of increasing neovascularization
in the ischemic limbs of patients with PAD (10,17).
Combined with the previous result that curcumin improves outcomes
in diabetic PAD, the present study suggests that curcumin may serve
as an effective alternative treatment approach for PAD in
non-diabetic subjects.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JZ and RH conceived and designed the current study.
JZ, QW and RH wrote and edited the manuscript. JZ, QW, GR, JQ and
RH performed the experiments, and read and approved the final
manuscript.
Ethics approval and consent to
participate
The experimental animal protocol was approved by the
Committee on Animal Experiments of Wuhan University School of
Medicine. The use of HUVECs isolated from donor umbilical cords was
approved by the Institutional Review Boards of Wuhan
University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Guerchet M, Aboyans V, Mbelesso P, Mouanga
AM, Salazar J, Bandzouzi B, Tabo A, Clément JP, Preux PM and
Lacroix P: Epidemiology of peripheral artery disease in elder
general population of two cities of Central Africa: Bangui and
Brazzaville. Eur J Vasc Endovasc Surg. 44:164–169. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Criqui MH and Aboyans V: Epidemiology of
peripheral artery disease. Circ Res. 116:1509–1526. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fowkes FG, Aboyans V, Fowkes FJ, McDermott
MM, Sampson UK and Criqui MH: Peripheral artery disease:
Epidemiology and global perspectives. Nat Rev Cardiol. 14:156–170.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Espinola-Klein C and Savvidis S:
Peripheral arterial disease. Epidemiology, symptoms and diagnosis.
Internist (Berl). 50:919–926. 2009.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Grundmann S, Piek JJ, Pasterkamp G and
Hoefer IE: Arteriogenesis: Basic mechanisms and therapeutic
stimulation. Eur J Clin Invest. 37:755–766. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hirsch AT: Treatment of peripheral
arterial disease-extending ‘intervention’ to ‘therapeutic choice’.
N Engl J Med. 354:1944–1947. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Joh JH, Joo SH and Park HC: Simultaneous
hybrid revascularization for symptomatic lower extremity arterial
occlusive disease. Exp Ther Med. 7:804–810. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aviles RJ, Annex BH and Lederman RJ:
Testing clinical therapeutic angiogenesis using basic fibroblast
growth factor (FGF-2). Brit J Pharmacol. 140:637–646. 2003.
View Article : Google Scholar
|
|
9
|
Owens CD and Conte MS: Medical management
of peripheral arterial disease: Bridging the ‘Gap’? Circulation.
126:1319–1321. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Annex BH: Therapeutic angiogenesis for
critical limb ischaemia. Nat Rev Cardiol. 10:387–396. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Allegra A, Innao V, Russo S, Gerace D,
Alonci A and Musolino C: Anticancer activity of curcumin and its
analogues: Preclinical and clinical studies. Cancer Invest.
35:1–22. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Goozee KG, Shah TM, Sohrabi HR,
Rainey-Smith SR, Brown B, Verdile G and Martins RN: Examining the
potential clinical value of curcumin in the prevention and
diagnosis of Alzheimer's disease. Br J Nutr. 115:449–465. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jiménez-Osorio AS, Monroy A and Alavez S:
Curcumin and insulin resistance-Molecular targets and clinical
evidences. Biofactors. 42:561–580. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
You J, Sun J, Ma T, Yang Z, Wang X, Zhang
Z, Li J, Wang L, Ii M, Yang J and Shen Z: Curcumin induces
therapeutic angiogenesis in a diabetic mouse hindlimb ischemia
model via modulating the function of endothelial progenitor cells.
Stem Cell Res Ther. 8:1822017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Barrett PM, Wall CAM and Stack AG:
Peripheral artery disease prevalence and mortality trends of United
States dialysis population: 1995–2005. Irish J Med Sci.
179:S409–S410. 2010.
|
|
16
|
Waters RE, Terjung RL, Peters KG and Annex
BH: Preclinical models of human peripheral arterial occlusive
disease: Implications for investigation of therapeutic agents. J
Appl Physiol (1985). 97:773–780. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Albadawi H, Oklu R, Cormier NR, O'Keefe
RM, Heaton JT, Kobler JB, Austen WG and Watkins MT: Hind limb
ischemia-reperfusion injury in diet-induced obese mice. J Surg Res.
190:683–691. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Baudin B, Bruneel A, Bosselut N and
Vaubourdolle M: A protocol for isolation and culture of human
umbilical vein endothelial cells. Nat Protoc. 2:481–485. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hazarika S, Farber CR, Dokun AO,
Pitsillides AN, Wang T, Lye RJ and Annex BH: MicroRNA-93 controls
perfusion recovery after hindlimb ischemia by modulating expression
of multiple genes in the cell cycle pathway. Circulation.
127:1818–1828. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Elavarasu S, Suthanthiran T, Thangavelu A,
Alex S, Palanisamy VK and Kumar TS: Evaluation of superoxide
dismutase levels in local drug delivery system containing 0.2%
curcumin strip as an adjunct to scaling and root planing in chronic
periodontitis: A clinical and biochemical study. J Pharm Bioallied
Sci. 8 Suppl 1:S48–S52. 2016.PubMed/NCBI
|
|
22
|
Huang F, Yao Y, Wu J, Liu Q, Zhang J, Pu
X, Zhang Q and Xia L: Curcumin inhibits gastric cancer-derived
mesenchymal stem cells mediated angiogenesis by regulating
NF-kB/VEGF signaling. Am J Transl Res. 9:5538–5547. 2017.PubMed/NCBI
|
|
23
|
He L and Hannon GJ: MicroRNAs: Small RNAs
with a big role in gene regulation. Nat Rev Genet. 5:522–531. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
González-Duarte RJ, Cázares-Ordoñez V and
Ávila-Chávez E: The microRNA biogenesis machinery: Regulation by
steroid hormones and alterations in cancer. Rev Invest Clin.
66:460–464. 2014.PubMed/NCBI
|
|
25
|
Ha M and Kim VN: Regulation of microRNA
biogenesis. Nat Rev Mol Cell Biol. 15:509–524. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jonas S and Izaurralde E: Towards a
molecular understanding of microRNA-mediated gene silencing. Nat
Rev Genet. 16:421–433. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhou X, Yuan P and He Y: Role of microRNAs
in peripheral artery disease (review). Mol Med Rep. 6:695–700.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ganta VC, Choi MH, Kutateladze A, Fox TE,
Farber CR and Annex BH: A MicroRNA93-interferon regulatory
factor-9-immunoresponsive gene-1-itaconic acid pathway
modulatesM2-like macrophage polarization to revascularize ischemic
muscle. Circulation. 135:2403–2425. 2017. View Article : Google Scholar : PubMed/NCBI
|