Introduction
Economic evaluations of health care interventions
are assuming increasing importance. There has been continued growth
of medical expenses in China over the past decade, and attention
has been increasingly focused on evaluating the cost-effectiveness
of medical treatments that patients received. The National Health
and Family Planning Commission (NHFPC) of the People's Republic of
China requested in 2016 that the growth of national health
expenditure should be less than 10% by the end of 2017. For that
reason, it is not surprising that there has been considerable
interest in reducing medical expenses by adopting more
cost-effective medical treatments including surgical
techniques.
Although traumatic disruption of the pelvic ring is
uncommon and accounts for about 3 to 8% of all skeletal injuries,
it has often carried a relatively high risk of mortality with
current estimates ranging from 5 to 35%, and up to 50%, based on
the severity of the associated injury patterns (1–6). These
injuries are predominantly the result from high energy blunt trauma
such as falling from a height, crushing by heavy loads at the
workplace, and motor vehicle collisions (7–10).
Severe associated injuries and multiple trauma are prevalent in
patients with pelvic ring fracture, which has increased the
complexity of surgical treatment, and also the hospitalization
costs. A previous study showed that the direct hospitalization cost
per patient with a pelvic fracture was $12,012 (US dollars) between
1999 to 2006 in the United States. This amount was just lower than
for hip fracture and multiple fractures (11).
Apart from the relatively high expenses, the
hospitalization costs among patients with pelvic fractures vary
greatly. On the one hand, it is because the severity of the injury
of the patients with pelvic fracture are heterogeneous (12–15); on
the other hand, the surgical treatments of pelvic fracture do vary
(16–19). Both these facts play an important
role in the length of stay and health care costs in hospital, which
contribute significantly to the overall hospitalization costs of
these patients.
There is no doubt that the in-hospital medical costs
increase with the increase in injury severity of patients with
pelvic fracture (20,21). Among all the surgical techniques of
the pelvis, open reduction and internal fixation has been commonly
used to treat fracture of the pelvic ring for decades.
Traditionally, ORIF procedures can be performed successfully with
either small or large locking compression or fragment
reconstruction plates and screws (22). Although ORIF is considered as
sophisticated and widely applicable, many surgeons prefer to choose
minimally invasive techniques such as a subcutaneous pedicle
screw-rod fixation system for their patients instead (23). This is mainly because both ORIF and
MIS can achieve similar short-term clinical outcomes and long-term
treatment results, as a number of studies have reported. In
addition, MIS had superior results to ORIF in terms of the
operation time, length of incision, blood loss during operation,
and length of stay (24,25).
However, there is still no consensus on whether MIS
or ORIF is more cost-effective in the treatment of traumatic pelvic
ring fractures. Additionally, no relevant studies have compared the
cost effectiveness of MIS and ORIF for pelvic fracture treatment so
far. Therefore, it is necessary to make an economic evaluation and
to compare the cost effectiveness of these two types of surgical
techniques for the treatment of pelvic fractures.
There are four types of economic evaluation methods
which can be used to gather evidence and compare the expected costs
and outcomes of different surgical techniques (26).
i) A cost-utility analysis (CUA) is characterized by
analysis of utility-based outcomes such as the quality-adjusted
life years following treatment; ii) A cost-benefit analysis (CBA)
is concerned with the consequences expressed in monetary units and
is commonly used to evaluate distribution of resources to diverse
areas of health care; iii) A cost-effectiveness analysis (CEA) is
characterized by analysis of both costs and clinical or
physiological outcomes, where the outcomes of alternative
treatments might be different in magnitude; and iv) A
cost-minimization analysis (CMA), which is a form of
cost-effectiveness analysis, is used when outcomes of different
treatments are equivalent and the aim is to identify which
alternative has the lowest cost (26).
To determine the most appropriate economic
evaluation approach in this study, a literature review was first
conducted to ascertain whether the clinical outcomes between MIS
and ORIF were equivalent. Based on reviewing the relevant studies
we found that although MIS resulted in slightly better scores than
ORIF on post-operative outcomes such as functional score, imaging
score, reduction quality, and complication rate, the statistical
difference between these two kinds of surgical techniques was
barely significant (22,24,25,27,28).
Because both methods achieved equivalent outcomes according to the
literature studied, cost-minimization analysis (CMA) could be an
appropriate economic evaluation form.
We hypothesize that the cost effectiveness of MIS is
better than ORIF for the treatment of pelvic fracture because the
units of blood transfusion, nursing workload, antibiotics
consumption, and post-operative length of stay are expected to be
reduced for the patients treated with minimally invasive pelvic
surgery.
The main aim of this study was to determine whether
there were any differences in the cost effectiveness of pelvic
fracture treatment by MIS or ORIF. Additionally, all the cost data
were analyzed to evaluate the composition of hospitalization costs
of different surgical techniques.
Materials and methods
Patient selection
This retrospective study involved a single-center
series of patients who were diagnosed with pelvic fractures
according to the International Classification of Diseases (ICD-10)
codes at Shanghai General Hospital from January 2012 to December
2016. Pelvic fractures included all fracture types affecting the
following bony anatomy region: Acetabulum, pubis, sacrum, ilium,
ischium, and coccyx.
The inclusion criteria were as follows: i) patients
aged between 18 and 90 years old (because there is controversy on
whether pediatric pelvic fractures are different injuries from
adults) (14); ii) patients who
failed to accept conservative treatment and had to undergo surgical
treatment for pelvic fracture.
The exclusion criteria were as follows: i) patients
who had undergone surgeries for other parts of the body besides the
pelvis; ii) patients who had received closed reduction and external
fixation (CREF) or fixation removal surgery; iii) patients who were
diagnosed with severe comorbidities (including cancers,
cardiovascular and cerebrovascular diseases, and coagulation
disorders) or acute associated injuries (especially severe open
pelvic fracture and multiple organ failure); and iv) patients who
were lost to follow-up (either by being lost to contact or by other
socioeconomic factors).
Data collection
The demographic and physiological data of patients
on admission including age, gender, mechanism of injury, systolic
blood pressure, heart rate, respiratory rate, temperature,
consciousness, need for ICU on admission, and units of blood
transfused within the first 24 h post injury were obtained from the
hospital's routine nursing records.
Injury-specific data were extracted from the
hospital's electronic clinical records. These data included
fracture type, whether associated with internal organ injury, the
need for pelvic digital-subtraction angiography (DSA), and whether
it was an isolated or multiple pelvic fracture (more than 3 sites
of pelvic fractures). In addition, the American Society of
Anesthesiologists score was recorded, which is an overall score
that assesses the physical status of patients before surgery and
ranges from 1 to 5, corresponding to ‘normal healthy patient’ to
‘moribund patient who is not expected to survive’, and the number
of consultations before the operation. The types of pelvic fracture
were classified separately by two resident physicians according to
all the available radiological data and using Tile's classification
system adopted by the Orthopedic Trauma Association (OTA). Type A
fractures are vertically and rotationally stable; Type B fractures
are vertically stable but rotationally unstable; Type C fractures
are vertically and rotationally unstable (29). Cases that were undecided were
discussed in regular weekly meetings held by the department
director to minimize inter-observer bias.
The surgery-related data including the type of
surgical procedure, duration of operation, length of incision,
intra-operative bleeding volume, and post-operative length of
hospital stay were collected from the paper-based operative notes.
Moreover, the incidence rate of peri-operative complications were
gathered from medical records and the Majeed postoperative
functional outcome scores were obtained from follow-up records. The
follow-ups were performed and pelvic radiographs were taken to
evaluate the reduction and the osseous union. The Majeed functional
score of all patients were evaluated at 6 and 12 months after the
operation.
The data of direct medical costs in hospital
including medical tests, medical materials, surgical services,
medications, blood production, nursing care, ward-bed occupation,
and miscellaneous items were identified by accessing the hospital's
financial records.
Surgical technique
The criteria were classified into 2 groups by the
pattern of surgeries they received. One group underwent open
reduction and internal fixation (ORIF), and the other group
underwent minimally invasive surgery (MIS). All surgeries were
performed under general anesthesia.
In the open reduction and internal fixation (ORIF)
group, patients were placed in the supine position, a midline
vertical incision was made, then a 4.5 mm locking compression plate
with 9–12 holes was bent and placed closely to the bone surface
with 2–3 holes remaining on each side, and then screws were
inserted and tightened on each end of the plate.
In the minimally invasive surgery (MIS) group, all
patients underwent percutaneous pedicle screw-rod fixation (PSRF).
From 2 to 4 pedicle screws (60–80 mm long and 7 mm wide) were
inserted into the bilateral supra-acetabular bone through small
incisions which spanned the fractured pelvic ring by
interconnecting the left and right hemipelvis with an appropriate
length curved titanium or stainless steel rod.
Financial analysis
For each patient, hospitalization costs were
extracted from the hospital financial information system. Direct
medical costs in hospital were based on a fixed internal hospital
fee schedule for services and consisted of medical test costs
(laboratory test and imaging investigation), materials (consumables
and implants), surgical services (procedure and anesthesia),
medications (antibiotics and non-antibiotic drugs), inpatient costs
(nursing service and ward-bed occupation), blood production, and
miscellaneous items costs. Direct non-medical costs, which include
the expenditure caused by transportation and food for patients and
their relatives during hospitalization, were not included in the
study. Indirect medical costs (30),
which mostly refer to the loss of income due to absenteeism and
intangible costs caused by pain and suffering were also excluded.
All cost data were obtained in CNY (¥), and subsequently converted
to USD ($), with ¥1 equivalent to $0.1452 according to the
international exchange rate on May 16, 2017.
Cost minimization analysis (CMA) was used to
determine which kind of surgery method was more cost-effective
because evidence was found that the treatment alternatives have
identical outcomes. In other words, the comparison of cost
effectiveness was equivalent to the comparison of the mean cost
between the different groups (31).
The cost structure of the 2 kinds of surgical techniques was also
analyzed. This was done to clarify the relationship between each
part of the hospitalization costs and related surgical technique.
In addition, one-way sensitivity analyses were used to test the
robustness of the conclusions as well as broaden the
generalizability of the results.
Statistical analysis
Descriptive statistics were presented as mean ±
standard deviation (SD) or median and interquartile range (IQR) for
all continuous variables depending on the distribution of the data
while number with percentages (%) were reported for all categorical
variables.
Bivariate analysis was performed by using t test
(normal distribution) or Mann Whitney U-test (abnormal
distribution) whenever appropriate to compare the mean for all the
continuous variables between the 2 groups. Chi-Square test or
Adjusted Chi-Square test, as appropriate (depending on the sample
size), were used to compare the proportions of all the categorical
variables between the 2 groups. Results with P-values less than or
equal to 0.05 were considered to be statistically significant.
The software SPSS version 20.0 (IBM Corp., Armonk,
NY, USA) was used for data management as well as statistical
analysis.
Ethics statement
This study was reviewed and approved by the
Institutional Review Board of the Shanghai General Hospital
affiliated to Shanghai Jiao Tong University. The study was carried
out in accordance with the principles of the World Medical
Association's Declaration of Helsinki. The application of the
exemption for informed consent was approved by the Ethics Committee
of Shanghai General Hospital since the study did not involve any
identifying patient information.
Results
Baseline characteristics
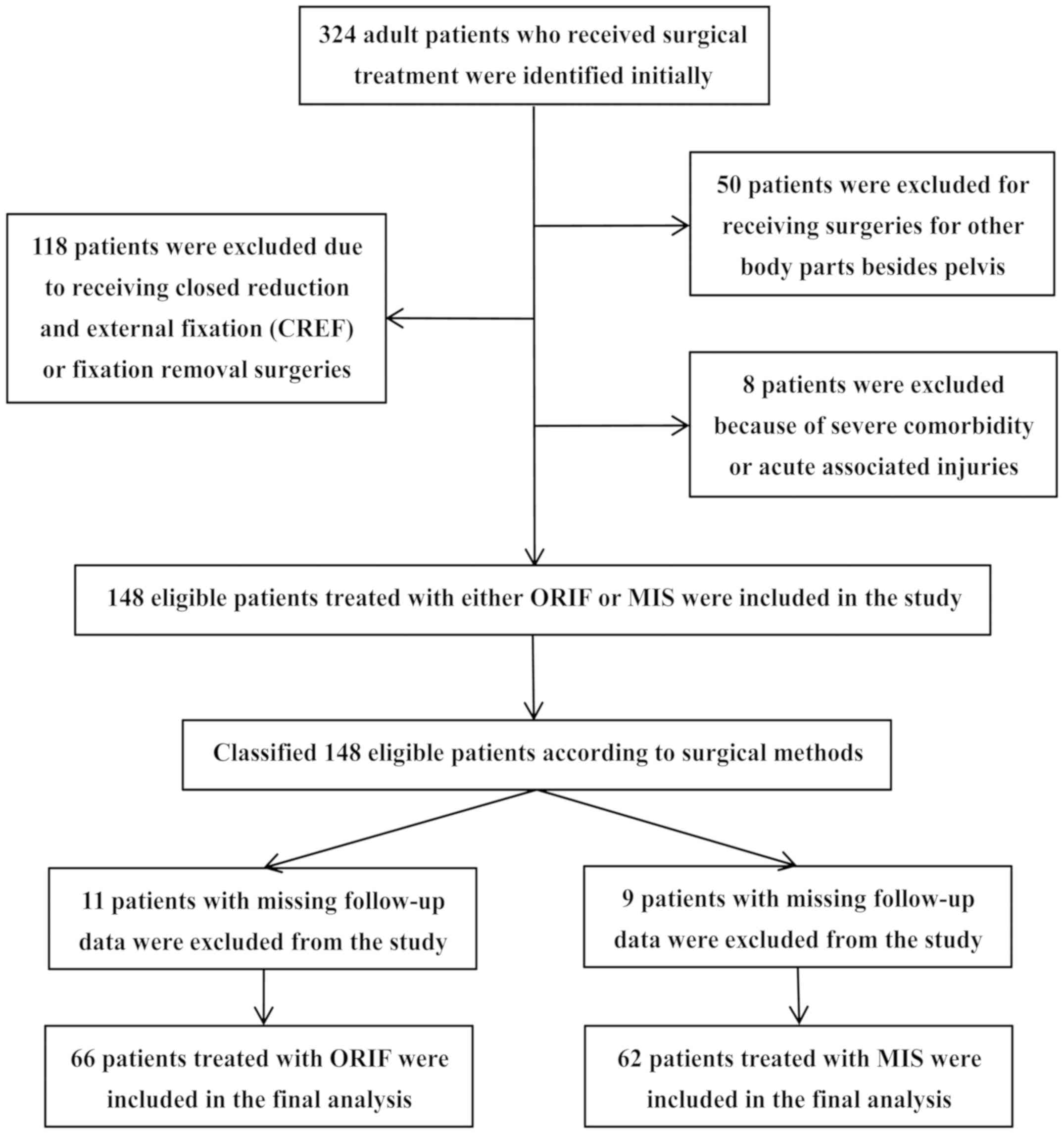
During the study period, 324 adult patients were
diagnosed with pelvic fracture and received surgical treatment
(ICD-10 code: S32.801), among whom 274 patients received surgery
for the pelvis without surgery for other parts of the body. There
were 118 patients excluded for receiving a nonspecific method of
surgery and 8 patients were excluded because of severe
comorbidities or acute associated injuries. Moreover, 20 patients
were lost to follow-up due to invalid contact information provided
or referral to local hospitals where these patients lived. After
the selection process, 66 patients with a mean age of 44 years who
underwent ORIF surgery, and 62 patients with a mean age of 41 years
who underwent MIS were finally included in this study. The
follow-up rate was 85.7% in the ORIF group and 87.3% in the MIS
group, respectively. A detailed flow chart of patient selection is
presented in Fig. 1.
Because different surgical treatments were based on
the clinical condition of patients, all baseline data of the 2
groups of patients including demographic information, preoperative
clinical characteristics, severity of the illness, types of the
pelvic fracture, and other factors were compared to ensure that the
2 groups were comparable in this study. According to the
statistical results, patients in the MIS group showed no
differences in baseline characteristics from the ORIF group. The
results are summarized in Tables I
and II.
 | Table I.Demographic and physiological data of
patients with pelvic fracture. |
Table I.
Demographic and physiological data of
patients with pelvic fracture.
| Patient
variables | ORIF, n=66 | MIS, n=62 | P-value |
|---|
| Sex, n (%) |
|
| 0.965 |
|
Male | 37 (56.1) | 35 (56.5) |
|
|
Female | 29 (43.9) | 27 (43.5) |
|
| Age (years, mean ±
SD) | 43.76±13.43 | 44.14±13.19 | 0.408 |
| Mechanism of
injury, n (%) |
|
| 0.280 |
| High
fall | 11 (16.7) | 14 (22.6) |
|
| Motor
vehicle collision | 37 (56.1) | 26 (41.9) |
|
| Crush
injury | 8
(12.1) | 6
(9.7) |
|
| Stumble
fall | 10 (15.1) | 16 (25.8) |
|
| Physiological
indicators on arrival |
|
|
|
|
Systolic blood pressure (mm
Hg, mean ± SD) | 125.72±14.96 | 120.73±15.34 | 0.122 |
| Heart
rate (bpm, median and IQR) | 77 (76,
80) | 78 (76,
80) | 0.273b |
|
Respiratory rate (bpm, median
and IQR) | 20 (18,
20) | 19 (18,
20) | 0.595b |
|
Temperature (°C, median and
IQR) | 36.9 (36.6,
37.0) | 37.0 (36.7,
37.0) | 0.574b |
| Consciousness on
arrival, n (%) |
|
| 0.128a |
|
GCS≥9 | 55 (83.3) | 58 (93.5) |
|
|
GCS<9 | 11 (16.7) | 4 (6.5) |
|
| Need for ICU on
arrival, n (%) |
|
| 0.114 |
|
Yes | 17 (25.8) | 8
(14.5) |
|
| No | 49 (74.2) | 54 (85.5) |
|
| Blood transfused
within the first 24 h after admission (Units, median and IQR) | 0 (0,
1) | 0 (0,
1.5) | 0.776b |
 | Table II.Pre-operative injury-severity factors
of patients with pelvic fracture. |
Table II.
Pre-operative injury-severity factors
of patients with pelvic fracture.
| Patient
factors | ORIF, n=66 | MIS, n=62 | P-value |
|---|
| Tile's
classification, n (%) |
|
| 0.499 |
| A
type | 20 (30.3) | 14 (22.6) |
|
| B
type | 37 (56.1) | 41 (66.1) |
|
| C
type | 9
(13.6) | 7
(11.3) |
|
| Internal organ
injury, n (%) |
|
| 0.758 |
|
Yes | 12 (18.2) | 10 (16.1) |
|
| No | 54 (81.2) | 52 (83.9) |
|
| Need for DSA, n
(%) |
|
| 0.249a |
|
Yes | 8
(12.1) | 3 (4.8) |
|
| No | 58 (87.9) | 57 (95.2) |
|
| Multiple pelvic
fractures, n (%) |
|
| 0.234 |
|
Yes | 23 (34.8) | 28 (45.2) |
|
| No | 43 (65.2) | 34 (54.8) |
|
| Preoperative
consultation (times, median and IQR) | 1 (0,
1) | 1 (0,
1.5) | 0.977b |
| ASA score (mean ±
SD) | 2.20±0.72 | 1.91±0.68 | 0.055 |
Operation records and outcomes
Differences in length of incision were significant
(Table III). The median incision
length in the MIS and ORIF group was 14 and 6 cm respectively
(P<0.001). A significant difference was observed regarding
duration of operation (P=0.001; Table
III), which was shorter in the MIS group than the ORIF group
(103 min vs. 152 min). The MIS group had significantly less
intra-operative bleeding volume (50 vs. 250 ml) than the ORIF group
(P<0.001; Table III).
 | Table III.Surgery records of patients with
pelvic fracture. |
Table III.
Surgery records of patients with
pelvic fracture.
| Surgery
records | ORIF, n=66 | MIS, n=62 | P-value |
|---|
| Surgery times (min,
median & IQR) | 152 (105, 168) | 103 (90, 118) | 0.00a |
| Length of incision
(cm, median & IQR) | 14 (10, 16) | 6 (5, 8.5) |
<0.00a |
| Estimated blood
loss (ml, median & IQR) | 250 (200, 800) | 50 (20, 100) |
<0.00a |
There was also a statistically significant
difference in the post-operative length of stay between the 2
groups, with a median stay of 8 days and 15 days in the MIS and
ORIF group, respectively (P<0.001; Table III).
We found no statistically significant difference in
the Majeed functional scores between the 2 groups at the final
follow-up (P=0.614; Table IV). The
average evaluation score was 79.6 points with an excellent rate of
77.4% in the MIS group vs. 81.4 points with an excellent rate of
75.8% in the ORIF group (P=0.825; Table
IV). With regard to complications, in the ORIF group, there
were 2 patients with surgical site infection, 2 patients treated
with unplanned re-operation due to hardware failure, and 1 patient
was reported as having malunion. By comparison, 3 patients who
underwent MIS were found to have infection at the surgical site.
Even though the complication rate in the ORIF group (7.6%) was
higher than that in MIS group (4.8%), the difference was not
statistically significant (P=0.719; Table IV). Furthermore, no patients died in
either the ORIF or the MIS group. Because both groups achieved
equivalent outcomes according to the statistics (P<0.05),
cost-minimization analysis (CMA) is the most appropriate form of
economic evaluation for this study because the CMA assumes that
outcomes are equivalent while seeking the least expensive
alternative (26).
 | Table IV.Comparison of outcomes between the
MIS and ORIF group. |
Table IV.
Comparison of outcomes between the
MIS and ORIF group.
| Outcomes | ORIF, n=66 | MIS, n=62 | P-value |
|---|
| The Majeed
functional score (mean ± SD) | 81.4±7.7 | 79.6±9.0 | 0.614 |
| Excellent reduction
n (%) | 50 (75.8) | 48 (77.4) | 0.825 |
| Perioperative
complications n (%) | 5 (7.5) | 3 (4.8) | 0.719a |
|
Surgical site infection | 2 | 3 | / |
|
Unplanned re-operation | 2 | 0 | / |
|
Malunion | 1 | 0 | / |
Hospitalization costs
For all subjects, the average total hospital direct
cost was estimated to be $6,178.4 in the MIS group vs. $9,227.7 in
the ORIF group and a significant difference was observed between
the 2 groups (P=0.032). All the details of the costs are summarized
in Table V.
 | Table V.Comparison of direct medical costs of
patients with pelvic fracture. |
Table V.
Comparison of direct medical costs of
patients with pelvic fracture.
| Direct medical
cost | ORIF, n=66 (mean ±
SD) | MIS, n=62 (mean ±
SD) |
P-valuea | Mean difference
(ORIF minus MIS) |
|---|
| Medical test
($) | 344.2±133.1 | 342.8±189.5 | 0.984b | +1.7 |
|
Laboratory test | 185.3±91.3 | 198.3±97.2 | 0.765b | −13 |
| Imaging
investigation | 158.8±84.3 | 144.5±105.5 | 0.725b | +14.3 |
| Medical
materialsc ($) |
6,057.0±2,010.9 | 3,998.2±901.2 | 0.029b | +2058.8 |
|
Consumablesc |
1,248.0±1,036.4 | 646.4±128.4 | <0.001 | +601.6 |
|
Implants |
4,809.0±2,187.4 | 3,351.8±889.0 | 0.149b | +1457.2 |
| Surgical
servicec ($) | 1,003.7±267.4 | 815.4±23.4 | <0.001 | +188.3 |
|
Anesthesia | 226.4±103.7 | 212.6±21.7 | 0.451 | +13.8 |
|
Operating room occupation and
staff laborc | 777.3±240.1 | 602.9±3.9 | <0.001 | +174.4 |
|
Medicationc ($) | 1,112.1±654.5 | 646.4±128.4 | <0.001 | +465.7 |
|
Antibioticsc | 257.9±478.4 | 88.4±34.6 | 0.021 | +169.5 |
|
Non-antibioticsc | 854.2±347.2 | 558.0±113.0 | 0.009 | +296.2 |
| Blood
productionc ($) | 117.0±311.8 | 33.4±74.7 | <0.001 | +83.6 |
| Nursing
carec ($) | 140.8±199.7 | 57.8±29.6 | 0.014 | +83.0 |
| Ward bed
occupationc ($) | 189.5±207.1 | 113.8±74.2 | 0.018 | +75.6 |
| Miscellaneous items
($) | 263.4±169.1 | 170.6±26.2 | 0.233 | +92.8 |
| Total in-hospital
direct costsc ($) |
9,227.7±3,107.3 |
6,178.4±1,087.8 | 0.032b | +3049.3 |
Most of the hospital direct cost in both groups was
due to the direct cost of medical materials which consist of
disposable medical consumables ($1,248.0 vs. $646.4, P<0.001)
and surgical implants ($4809.0 vs. $3,351.8, P=0.149). The medical
materials cost in the MIS group and ORIF group was $6,057.0 and
$3,998.2 respectively, and the difference between the 2 groups was
statistically significant (P=0.029).
A significant difference was also found between the
2 groups in the surgical services cost, which includes anesthesia
($226.4 vs. $212.6, P=0.451) and operating room occupation and
staff labor ($777.3 vs. $602.9, P<0.001). The surgical services
cost in the ORIF group was much higher, by an average of $189, than
the MIS group ($1,003.7 vs. $815.4) (P<0.001).
The medication cost in the MIS group and ORIF group
was $646.4 and $1,112.1, respectively, and the difference between
the 2 groups was statistically significant (P<0.001). It is
notable that the cost of antibiotics in the ORIF group was 2.9
times than that in the MIS group ($257.9 vs. $88.4, P=0.021). With
regard to non-antibiotics, the cost was also much higher in the
ORIF group compared with that in the MIS ($854.2 vs. $558.0,
P=0.009). Other costs that were statistically higher in the ORIF
group included the cost of nursing care service (+$83.0, P=0.014)
and ward-bed occupation (+$75.6, P=0.018).
No significant difference was observed in the cost
of medical tests. The cost of various imaging tests such as X-ray,
computed tomography (CT), magnetic resonance imaging (MRI),
ultrasound testing (UT), and the cost of laboratory tests such as
for blood, urine, and other body fluid did not differ between the 2
groups, with a cost of $344.2 in the MIS group vs. $342.8 in the
ORIF group (P=0.984).
Cost structure
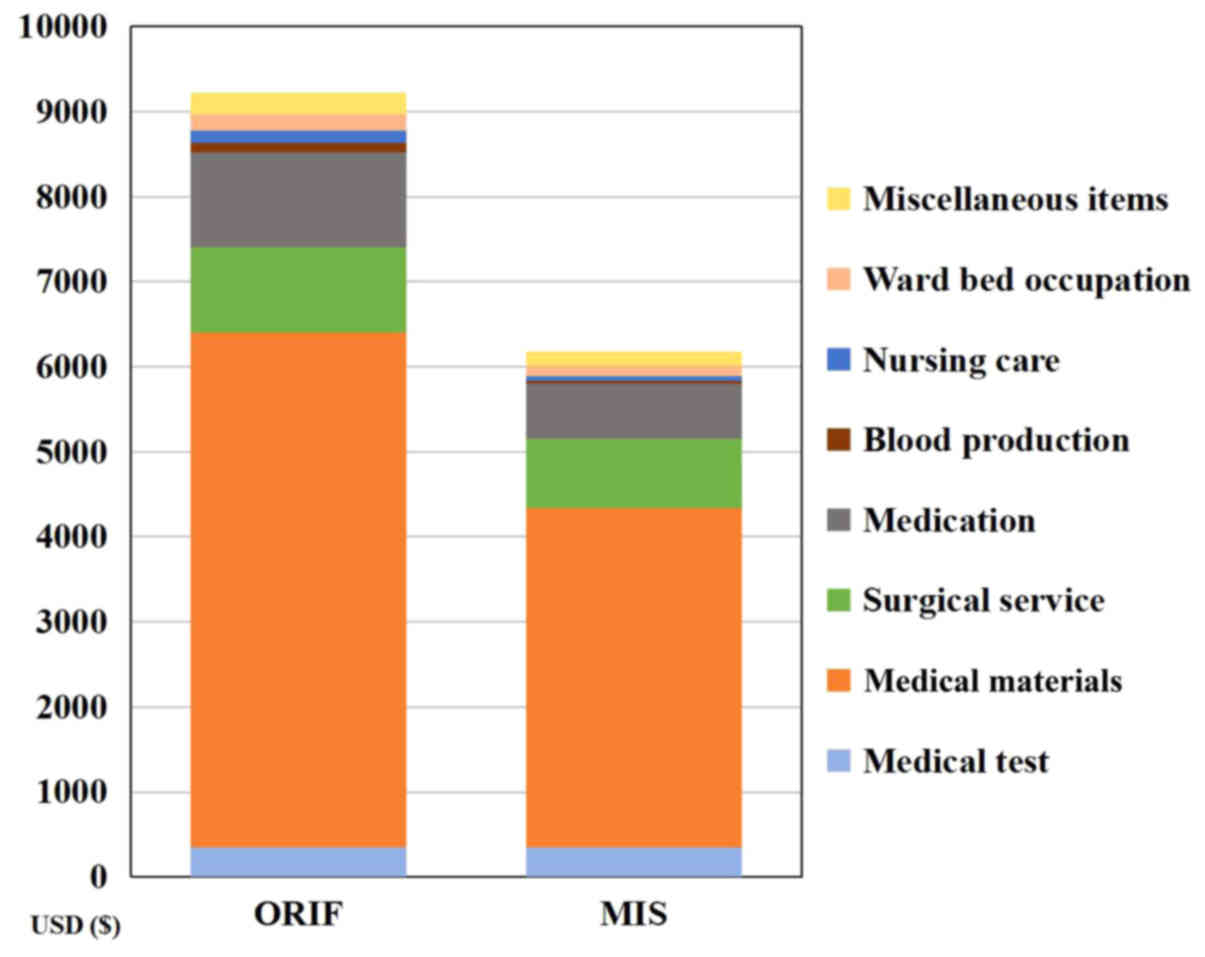
Fig. 2 shows the
composition of hospitalization costs per patient for the 2
different kinds of surgical methods. As can be seen from the
figure, in the ORIF group, medical materials accounted for 68.1% of
the cost, followed by medication taking up 12.1%, and surgical
service 10.9%. These 3 major components were responsible for a
great proportion of the total cost, which was similar to the
situation in the MIS group, although medical materials accounted
for 69.1%, surgical service 14.1%, and medication cost 11.2%.
The cost proportion of surgical service was quite
similar in both groups as well, with a percentage of 14.1% in the
MIS group and 11.3% in the ORIF group by comparison. Furthermore,
similarity was also found between the 2 groups with regard to
miscellaneous items, which accounted for 3.0% in both groups.
Blood production, nursing care and ward-bed
occupation were the 3 smallest cost areas in both groups,
altogether amounting to only 3.5 and 5.0% of the total cost in the
MIS and ORIF group, respectively.
With regard to medical tests, the cost proportion in
the MIS group (5.9%) was about 1.5 times greater than that in the
ORIF group (3.9%), which was the biggest difference between the 2
groups in this study (Fig. 2).
Sensitivity analyses
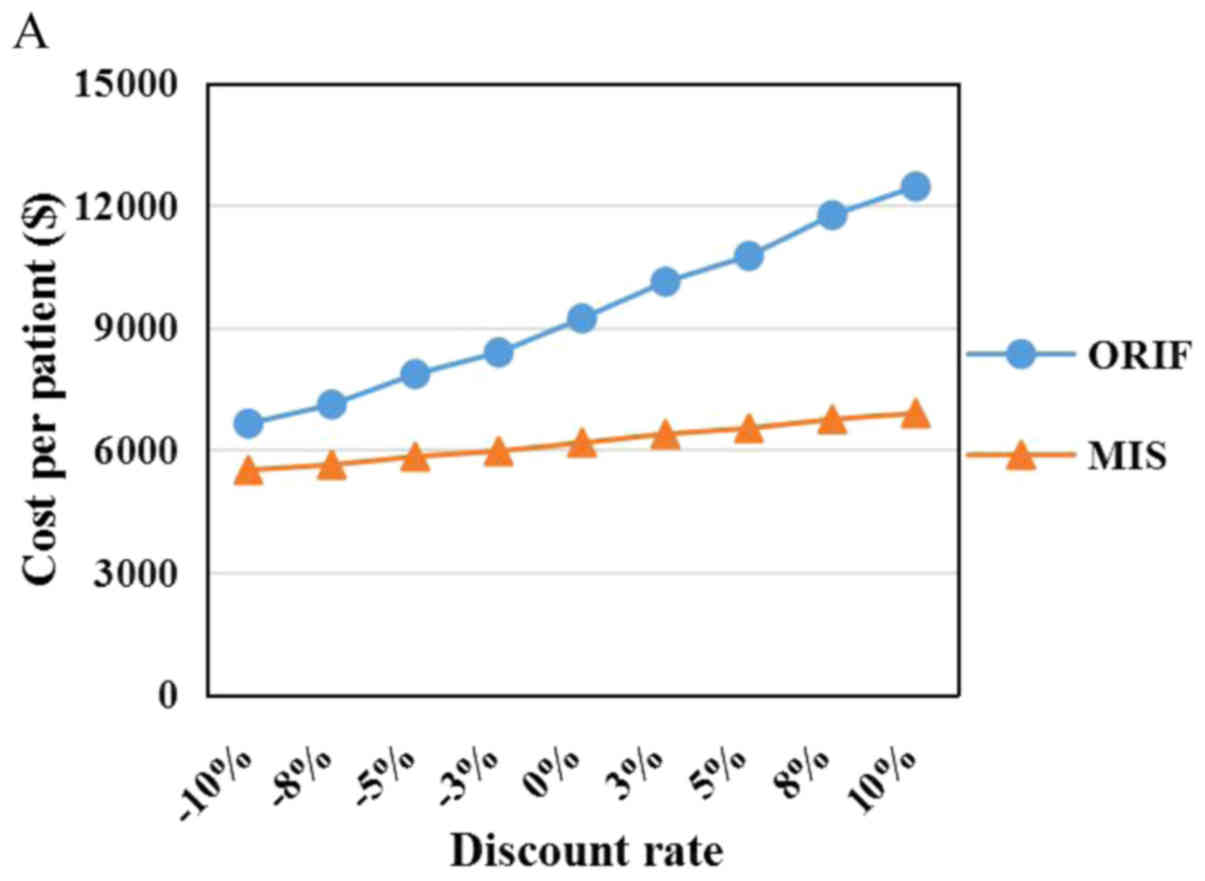
One-way sensitivity analyses were performed to
simulate different possible scenarios and test the robustness of
the results, by changing only one variable in a resonable range
while keeping all the other variables constant and then observing
the change of the new outcomes. In the current study, the
sensitivity analyses included the following parameters: Discount
rate, surgeon's fee for surgical service, daily hospitalization
cost and implants cost. The sensitivity range of each variable was
obtained by varying the lower and upper limit by 50% of the base
value (except the discount rate, which ranged from −10% to 10% in
light of actual conditions in the real world) (Table VI). The surgeon's fee for surgical
service refers to the labor costs of surgeons incurred by
performing surgeries, and the daily hospitalization cost includes
medications and bed and nursing charges. In addition, the implants
included the locking compression plate (used in the ORIF group),
titanium surgical screw (used in both groups) and rod (used in the
MIS group). All the outcomes of sensitivity analyses are presented
in Fig. 3A-F. It should be noted
that the variations in each selected key variable did not affect
the original conclusion within the sensitivity range, which means
our results are robust to these changes.
 | Table VI.Sensitivity ranges of key
variables. |
Table VI.
Sensitivity ranges of key
variables.
| Variables | Base value | Sensitivity
range |
|---|
| Discount rate | 0% | −10%-10% |
| Surgeon's fee for
surgical service | $601.1 | $300.6-$901.7 |
| Daily
hospitalization cost | $414.3 | $207.2-$621.5 |
| Implants cost |
|
|
| Locking
compression plate | $1,707.6 |
$853.8-$2,561.3 |
|
Titanium surgical screw | $819.5 |
$409.8-$1,229.3 |
|
Titanium surgical rod | $327.9 | $163.9-$491.8 |
Discussion
The incidence of pelvic ring injuries is estimated
to be 19–37 per 100,000 people/year according to the published
relevant literature (4) and has been
reported to make up from 3 to 8% of all skeletal injuries (12). With the recent decades of rapid
economic development and urban construction in China, pelvic
fractures caused by motor vehicle accidents and industrial injuries
in the workplace have gradually become more prevalent, which
constitutes a major cause of death as well as economic burden on
national healthcare in contemporary society (32).
The economic burden on patients with pelvic fracture
injury is heavy, not only for the immediate reconstructive surgery
but may also involve rehabilitation training or assisted living
placement resulting from loss of functional status. Alessandro
Aprato et al (30) reported
that the median direct and indirect cost of pelvic fracture is
€33,710 with the interquartile range from €23,266 to €51,012. They
concluded that the most direct cost of pelvic fracture was accrued
in the sector of surgical intervention, which amounted to a median
of €8,279 with the interquartile range from €5,674 to €14,365.
However, different surgical techniques are expected to result in
different direct hospitalization costs. Johnsen et al
(33) reported that the average
direct medical cost of surgery for patients with pelvic fracture
urethral-disruption injuries varied from $16,907 to $19,925 with
different surgical intervention strategies. As a consequence of the
significant resources expended on the treatment of pelvic fracture
injuries, the cost of various pelvic procedures should be evaluated
comprehensively and systematically.
However, few previous studies have compared the cost
effectiveness between different surgical treatment methods for
pelvic fracture injuries, and most of the existing research focused
on the comparison of biomechanical characteristics and clinical
outcomes in either the short or long term because surgeons are more
concerned with clinical effect than the medical cost of a surgical
technique (16,25,28). To
the best of our knowledge, this is the first study to make an
economic comparison between MIS and ORIF techniques for pelvic
fracture from a cost-minimization perspective.
The selection of surgical technique plays either an
extremely or very important role in direct medical cost for
patients. In this study, we analyzed the inpatient hospital costs
associated with the MIS and ORIF procedures thoroughly. The results
are consistent with the initial hypothesis that the MIS is a more
cost-effective alternative.
Patients in the MIS group had a shorter operation
time, less intra-operative bleeding volume, smaller incision, and
shorter post- operative length of stay than patients in the ORIF
group. These clinical factors accounted for most of the difference
in the hospitalization costs between the 2 groups and explained the
higher total cost in the ORIF group compared with the MIS
group.
For example, the shorter duration of surgery
required a shorter anesthesia time, shorter occupation time of the
operating room, and less workload for surgeons, which decreased the
charge and cost of surgical services with a net difference of
$188.3 ($1,003.7 for ORIF vs. $815.4 for MIS). The MIS procedure is
often associated with a significantly smaller incision. For these
patients, the antibiotic consumption could be reduced significantly
with a lower probability of surgical site infection, which leads to
a lower cost of medication with a net difference of $465.7
($1,112.1 for ORIF vs. $646.4 for MIS). Less intra-operative
bleeding volume definitely contributed to a lower cost of blood
production for patients who were treated with MIS and the net
difference was $83.6. In addition, patients in the MIS group had a
significantly shorter post-operative length of stay than those who
were treated with open reduction surgery, which lowered the costs
of ward-bed occupation as well as nursing care for the MIS group
with a net difference of $75.6 and $83.0, respectively. Shortening
the length of stay in the hospital can also effectively accelerate
bed turnover and significantly improve the operating capacity.
It should be noted that the surgical implants can be
rather expensive and always make up a large proportion of any
orthopedics operation. In the current study, the cost of implants
accounted for more than half of the total medical direct cost in
both the ORIF (54.0%) and MIS (57.9%) group, and the proportion of
the cost was similar. Specifically, 4 to 16 screws with 1 to 6
locking compression plates or reconstruction plates were used in an
ORIF surgery; by comparison, 2 to 6 screws with a titanium or
stainless steel rod were employed in a MIS. It is clear that the
MIS procedure typically used fewer implants than the ORIF. The mean
difference of implant cost between the 2 groups was relatively
large at the amount of $1,457.2, even though the difference was not
statistically significant (P=0.149, Table V).
Although the differences of patients' clinical
baseline characteristics between the 2 groups were not
statistically significant in this study, the indication and
contraindication of different surgical techniques are not
identical. It is unlikely that all kinds of injury patterns of the
pelvis could be treated successfully with only one universal
surgical approach, and the optimal operative technique is still
controversial. Therefore, the choice of surgical methods in
practice should always depend on the specific condition of the
patients. The ORIF is indicated for pure ligamentous pubic
dislocations, parasymphyseal, or ramii fractures, with plate
fixation spanning the anterior column (23). Many surgeons prefer the ORIF because
of its accurate reduction. Elzohairy and Salama (27) reported that ORIF achieved an 80% rate
of excellent and good reductions in a series of patients with
unstable posterior pelvic-ring disruptions. Lindsay et al
(22) reported that 57 out of 60
patients who had unilateral unstable pelvic-ring injuries and were
treated with ORIF obtained excellent and good outcomes of
reduction. With regard to the MIS procedure, the pedicle screw-rod
fixator is based on the same principles as the 2 pin external
fixator but is applied subcutaneously (25). It combines the advantages and avoids
the disadvantages of ORIF and external fixation, and is often
indicated for unstable unilateral or bilateral osseous and
osseoligamentous injuries of the anterior pelvic ring associated
with rotational or overall instability of the posterior segment of
the pelvis. The pedicle screw-rod fixator is also indicated for
unstable injuries of the anterior pelvic ring in morbidly obese
patients and patients with severe soft tissue injuries (23).
The minimally invasive pedical screw-rod system for
pelvic fracture fixation has been introduced and gradually been
substituted for the traditional open reduction and internal
fixation with plates since January 2014. Therefore, in the current
study, the patients who were admitted to our hospital during the
first half of the study period (from January 1, 2012 to December
31, 2013) were all treated by ORIF, while the other patients who
were admitted during the second half of the study period (from
January 1, 2014 to December 31, 2016) were all treated by MIS,
which ensured that all patients were distributed in each group
randomly and reduced the selection bias that could be introduced by
surgeons' preferences for the surgical treatment of pelvic
fractures.
This study focused on an individual large-scale
general hospital rather than a sample of cases across the entire
population in China. In order to minimize the selection bias, this
study was based on a single surgical team who were experienced at
performing both kinds of procedures. However, this could limit the
generality of the results since the surgical technique levels of
surgeons are varied, which could affect certain clinical parameters
such as blood loss, operation time, postoperative pain, medical
materials consumption, and length of hospital stay. All the factors
mentioned above may have an impact on the total direct medical cost
in a hospital, and any specific figure presented in this study
should not be extrapolated directly to other areas. Thus, more
samples from other medical centers with different MIS technique
levels should be collected and analyzed in further studies.
The data of direct non-medical costs (such as the
expenditure caused by transportation and food for patients and
their family members during hospitalization) and indirect cost
(especially the absenteeism caused by injury) were not considered.
This was because of the heterogeneous socioeconomic levels of
patients which may affect the reliability of the evaluation results
as the sample size was relatively small. In addition, a larger
sample size from different geographic areas with various
social-economic levels should be involved.
This study was also limited by several factors
inherent to the retrospective analysis, even though the nature of
the retrospective method allowed us to match our cohorts based on
patients' clinical baseline characteristics. In the current study,
some data were collected retrospectively, which may have had an
impact on the data completeness. As a large-scale tertiary general
hospital in Shanghai, China, patients admitted to our hospital were
not only from the local area but also from across the nation, which
made it a great challenge to collect follow-up data from all the
patients and resulted in some missing data. A prospective
evaluation with well documented follow-up records should be done in
the future as part of the continuous optimization and improvement
of the information management system in our hospital.
In addition, although the baseline characteristic
differences between the 2 groups were not statistically
significant, the criteria that we chose to reflect the severity of
injury of patients with pelvic fracture did not include the Injury
Severity Score (ISS) due to the limitations of our database.
Therefore, American Society of Anesthesiologists (ASA) scores,
fracture types classified by the Tile classification system, and a
series of physiological indicators on admission which reflect
associated injuries condition of patients were added to substitute
for the value of ISS, which may have introduced some unknown
confounding bias into this study.
Despite the limitations mentioned above, we believe
that this study provides valuable references regarding
cost-effectiveness between minimally invasive surgery (MIS) and
open reduction and internal fixation (ORIF) surgery for patients
with pelvic fracture.
In conclusion, In light of the concept of the
biopsychosocial medical mode (34),
treatment decisions should be made not only based on the clinical
basis of an individual patient but also from an economic aspect.
The results of this study illustrated that MIS performed by
subcutaneous pedicle screw-rod fixator is a cost-minimizing
surgical technique for pelvic injury compared with the technique of
ORIF. Further thorough and systematic economic evaluations
concerning the cost effectiveness analyses of other pelvic-surgery
techniques are still required.
Acknowledgements
The authors would like to thank Dr Guoying Deng
(Trauma Center of Shanghai General Hospital, Shanghai, China) for
valuable amendments to the first draft.
Funding
The present work was supported by the National
Natural Science Foundation of China (grant no. 71432007).
Availability of data and materials
The data sets used or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YZ designed the study. QW performed the pelvic
surgery and provided the original data. YC collected data. LiM and
LeM analyzed the data and wrote the manuscript. YJ was responsible
for the statistical analysis and quality control of the original
data. The final version of the manuscript was read and approved by
all authors.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of the Shanghai General Hospital affiliated to
Shanghai Jiao Tong University (approval number: 2015KY155). The
application of the exemption for informed consent was approved by
the Ethics Committee of Shanghai General Hospital since the study
did not involve any identifying information of patients.
Patient consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CMA
|
cost minimization analysis
|
|
MIS
|
minimally-invasive surgery
|
|
ORIF
|
open reduction and internal
fixation
|
References
|
1
|
Giannoudis PV, Grotz MR, Tzioupis C,
Dinopoulos H, Wells GE, Bouamra O and Lecky F: Prevalence of pelvic
fractures, associated injuries and mortality: The united kingdom
perspective. J Trauma. 63:875–883. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Poole GV, Ward EF, Muakkassa FF, Hsu HS,
Griswold JA and Rhodes RS: Pelvic fracture from major blunt trauma.
Outcome is determined by associated injuries. Ann Surg.
213:532–539. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gabbe BJ, de Steiger R, Esser M, Bucknill
A, Russ MK and Cameron PA: Predictors of mortality following severe
pelvic ring fracture: Results of a population-based study. Injury.
42:985–991. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pohlemann T, Stengel D, Tosounidis G,
Reilmann H, Stuby F, Stöckle U, Seekamp A, Schmal H, Thannheimer A,
Holmenschlager F, et al: Survival trends and predictors of
mortality in severe pelvic trauma: Estimates from the german pelvic
trauma registry initiative. Injury. 42:997–1002. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yoshihara H and Yoneoka D: Demographic
epidemiology of unstable pelvic fracture in the united states from
2000 to 2009: Trends and in-hospital mortality. J Trauma Acute Care
Surg. 76:380–385. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
White CE, Hsu JR and Holcomb JB:
Haemodynamically unstable pelvic fractures. Injury. 40:1023–1030.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Holstein JH, Culemann U and Pohlemann T:
Working Group Mortality in Pelvic Fracture Patients: What are
predictors of mortality in patients with pelvic fractures? Clin
Orthop Relat Res. 470:2090–2097. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Durkin A, Sagi HC, Durham R and Flint L:
Contemporary management of pelvic fractures. Am J Surg.
192:211–223. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
El-Haj M, Bloom A, Mosheiff R, Liebergall
M and Weil YA: Outcome of angiographic embolisation for unstable
pelvic ring injuries: Factors predicting success. Injury.
44:1750–1755. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ooi CK, Goh HK, Tay SY and Phua DH:
Patients with pelvic fracture: What factors are associated with
mortality? Int J Emerg Med. 3:299–304. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pike C, Birnbaum HG, Schiller M, Sharma H,
Burge R and Edgell ET: Direct and indirect costs of non-vertebral
fracture patients with osteoporosis in the us. Pharmacoeconomics.
28:395–409. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hauschild O, Strohm PC, Culemann U,
Pohlemann T, Suedkamp NP, Koestler W and Schmal H: Mortality in
patients with pelvic fractures: Results from the German pelvic
injury register. J Trauma. 64:449–455. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Davis JM, Stinner DJ, Bailey JR, Aden JK
and Hsu JR: Skeletal Trauma Research Consortium: Factors associated
with mortality in combat-related pelvic fractures. J Am Acad Orthop
Surg. 20 Suppl 1:S7–S12. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Demetriades D, Karaiskakis M, Velmahos GC,
Alo K, Murray J and Chan L: Pelvic fractures in pediatric and adult
trauma patients: Are they different injuries? J Trauma.
54:1146–1151. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lunsjo K, Tadros A, Hauggaard A, Blomgren
R, Kopke J and Abu-Zidan FM: Associated injuries and not fracture
instability predict mortality in pelvic fractures: A prospective
study of 100 patients. J Trauma. 62:687–691. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li CL: Clinical comparative analysis on
unstable pelvic fractures in the treatment with percutaneous
sacroiliac screws and sacroiliac joint anterior plate fixation. Eur
Rev Med Pharmacol Sci. 18:2704–2708. 2014.PubMed/NCBI
|
|
17
|
Chen HW, Liu GD, Fei J, Yi XH, Pan J, Ou S
and Zhou JH: Treatment of unstable posterior pelvic ring fracture
with percutaneous reconstruction plate and percutaneous sacroiliac
screws: A comparative study. J Orthop Sci. 17:580–587. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cole PA, Gauger EM, Anavian J, Ly TV,
Morgan RA and Heddings AA: Anterior pelvic external fixator versus
subcutaneous internal fixator in the treatment of anterior ring
pelvic fractures. J Orthop Trauma. 26:269–277. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vaidya R, Colen R, Vigdorchik J, Tonnos F
and Sethi A: Treatment of unstable pelvic ring injuries with an
internal anterior fixator and posterior fixation: Initial clinical
series. J Orthop Trauma. 26:1–8. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Giannoudis PV, Grotz MR, Papakostidis C
and Dinopoulos H: Operative treatment of displaced fractures of the
acetabulum. A meta-analysis. J Bone Joint Surg Br. 87:2–9. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Guthrie HC, Owens RW and Bircher MD:
Fractures of the pelvis. J Bone Joint Surg Br. 92:1481–1488. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lindsay A, Tornetta P III, Diwan A and
Templeman D: Is closed reduction and percutaneous fixation of
unstable posterior ring injuries as accurate as open reduction and
internal fixation? J Orthop Trauma. 30:29–33. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cole PA, Dyskin EA and Gilbertson JA:
Minimally-invasive fixation for anterior pelvic ring disruptions.
Injury. 46 Suppl 3:S27–S34. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bi C, Wang Q, Nagelli C, Wu J, Wang Q and
Wang J: Treatment of unstable posterior pelvic ring fracture with
pedicle screw-rod fixator versus locking compression plate: A
comparative study. Med Sci Monit. 22:3764–3770. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Vaidya R, Martin AJ, Roth M, Nasr K,
Gheraibeh P and Tonnos F: Infix versus plating for pelvic fractures
with disruption of the symphysis pubis. Int Orthop. 41:1671–1678.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Drummond ME, Sculpher MJ and Torrance GW:
Methods for the economic evaluations of health care programs, 3rd
edition. J Epidemiol Commun Heath. 60:822–823. 2006.
|
|
27
|
Elzohairy MM and Salama AM: Open reduction
internal fixation versus percutaneous iliosacral screw fixation for
unstable posterior pelvic ring disruptions. Orthop Traumatol Surg
Res. 103:223–227. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wu T, Chen W, Zhang Q, Li X, Lv HZ, Yang G
and Zhang YZ: Therapeutic effects of minimally invasive adjustable
and locking compression plate for unstable pelvic fractures via
posterior approach. Int J Clin Exp Med. 8:827–835. 2015.PubMed/NCBI
|
|
29
|
Bramos A, Velmahos GC, Butt UM, Fikry K,
Smith RM and Chang Y: Predictors of bleeding from stable pelvic
fractures. Arch Surg. 146:407–411. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Aprato A, Joeris A, Tosto F, Kalampoki V,
Stucchi A and Massè A: Direct and indirect costs of surgically
treated pelvic fractures. Arch Orthop Trauma Surg. 136:325–330.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wiedel AP, Norlund A, Petrén S and
Bondemark L: A cost minimization analysis of early correction of
anterior crossbite-a randomized controlled trial. Eur J Orthod.
38:140–145. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chien LC, Cheng HM, Chen WC and Tsai MC:
Pelvic fracture and risk factors for mortality: A population-based
study in Taiwan. Eur J Trauma Emerg Surg. 36:131–137. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Johnsen NV, Penson DF, Reynolds WS, Milam
DF, Dmochowski RR and Kaufman MR: Cost-effective management of
pelvic fracture urethral injuries. World J Urol. 35:1617–1623.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Engel GL: The need for a new medical
model: A challenge for biomedicine. Science. 196:129–136. 1977.
View Article : Google Scholar : PubMed/NCBI
|