Introduction
Simple bone cysts (SBC) are fluid-containing cystic
lesions that are surrounded by a hard bony wall without an
epithelial lining and without evidence of infection (1). The etiology of SBC is still
controversial (2). Despite
possessing many alternate names, ncluding solitary, traumatic,
hemorrhagic or unicameral bone cysts, the classification of bone
tumors and associated lesions included in the fourth edition of the
World Health Organization's classification of head and neck tumors
recommends using the term simple bone cyst (3). SBC represents ~1% of all jaw cysts
(4). In the second decade of life,
SBC usually occurs in the metaphyseal region of long bones and in
the body of the mandible (2,4,5). In
addition, SBC that forms in the maxillomandibular region has no sex
predilection (2,4). Although mandibular SBC is usually
asymptomatic and detected incidentally by radiographs, it may cause
swelling due to bone expansion, pain, pathologic fractures and
hypoesthesia of the inferior alveolar nerve (2,4,6–8). In
general, SBC has a well-delineated unilocular radiolucent lesion
and a scalloped appearance at the upper edge extending between the
roots (4,5). Displacement of the mandibular canal as
a result of mandibular cystic lesions, including SBC, has also been
reported (6,8,9). The
majority of these reports detected mandibular canal displacement
via panoramic radiograph and computed tomography (CT) scanning.
However, no reports have described the detection of the inferior
alveolar arteriovenous nerve bundle in the lesion lumen using an
endoscope. The current study reports a case of mandibular SBC
accompanied by a floating inferior alveolar neurovascular bundle
that was diagnosed using an endoscope.
Case report
A 13-year-old boy presented to the Department of
Dentistry and Oral Surgery at the University of Fukui Hospital
(Fukui, Japan) in March 2017 with a painless swelling in the right
buccal region that had been present for the last 1.5 months.
Physical examination revealed facial asymmetry due to swelling in
the right buccal region. Intraoral examination uncovered a hard
diffuse bony bulging of the right posterior mandible. The patient
had no remarkable medical history or history of trauma.
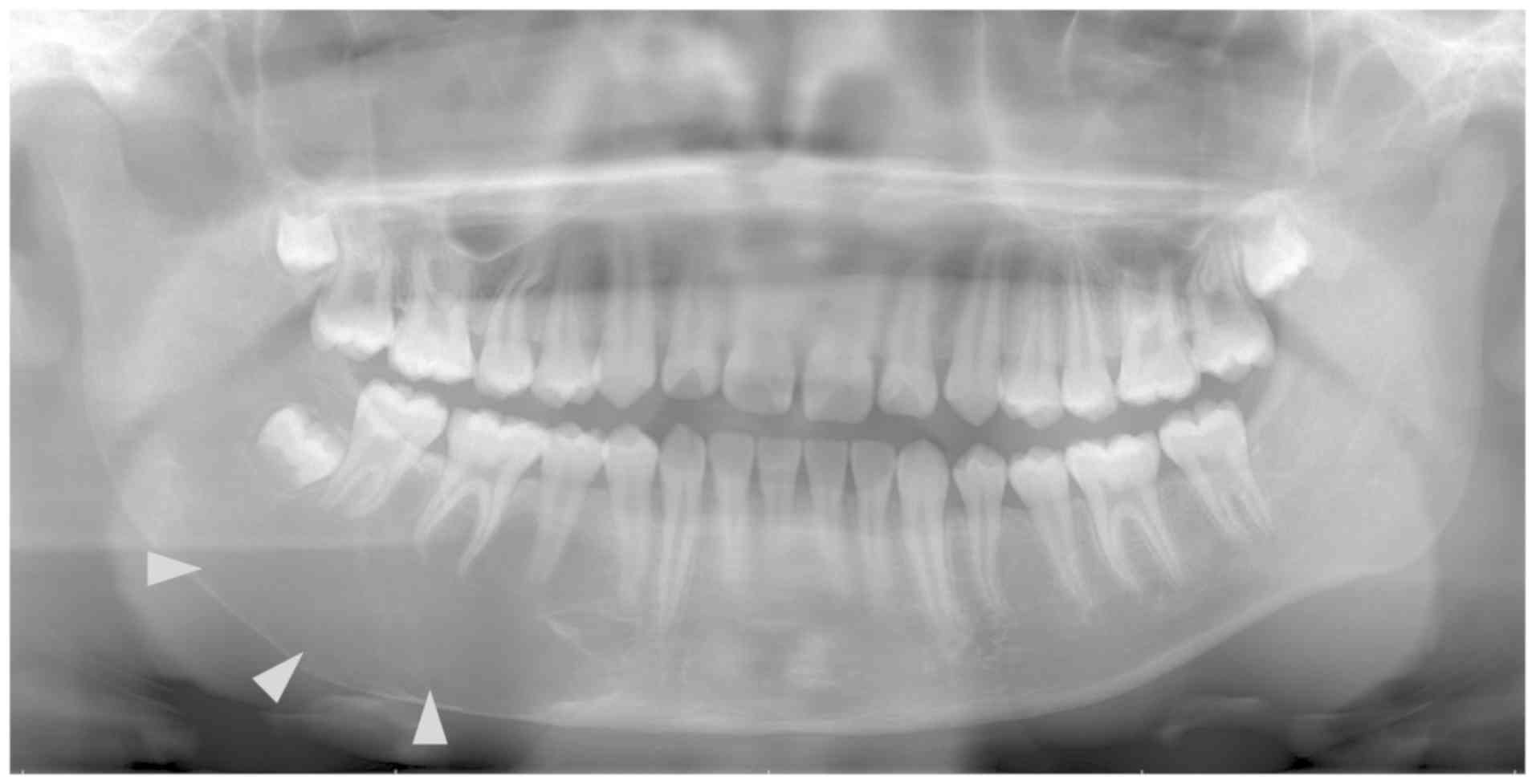
Panoramic radiograph and enhanced computed
tomography (CT) scanning revealed a well-delineated unilocular
radiolucent lesion ranging from the first premolar to the
mandibular ramus with lamina dura resorption accompanied with bony
expansion. This radiolucent lesion had a maximum anteroposterior
and buccolingual measurement of 70×30 mm. The mandibular canal
could not be confirmed by panoramic radiograph and enhanced CT
examinations of the lesion area (Figs.
1 and 2). In the lesion area,
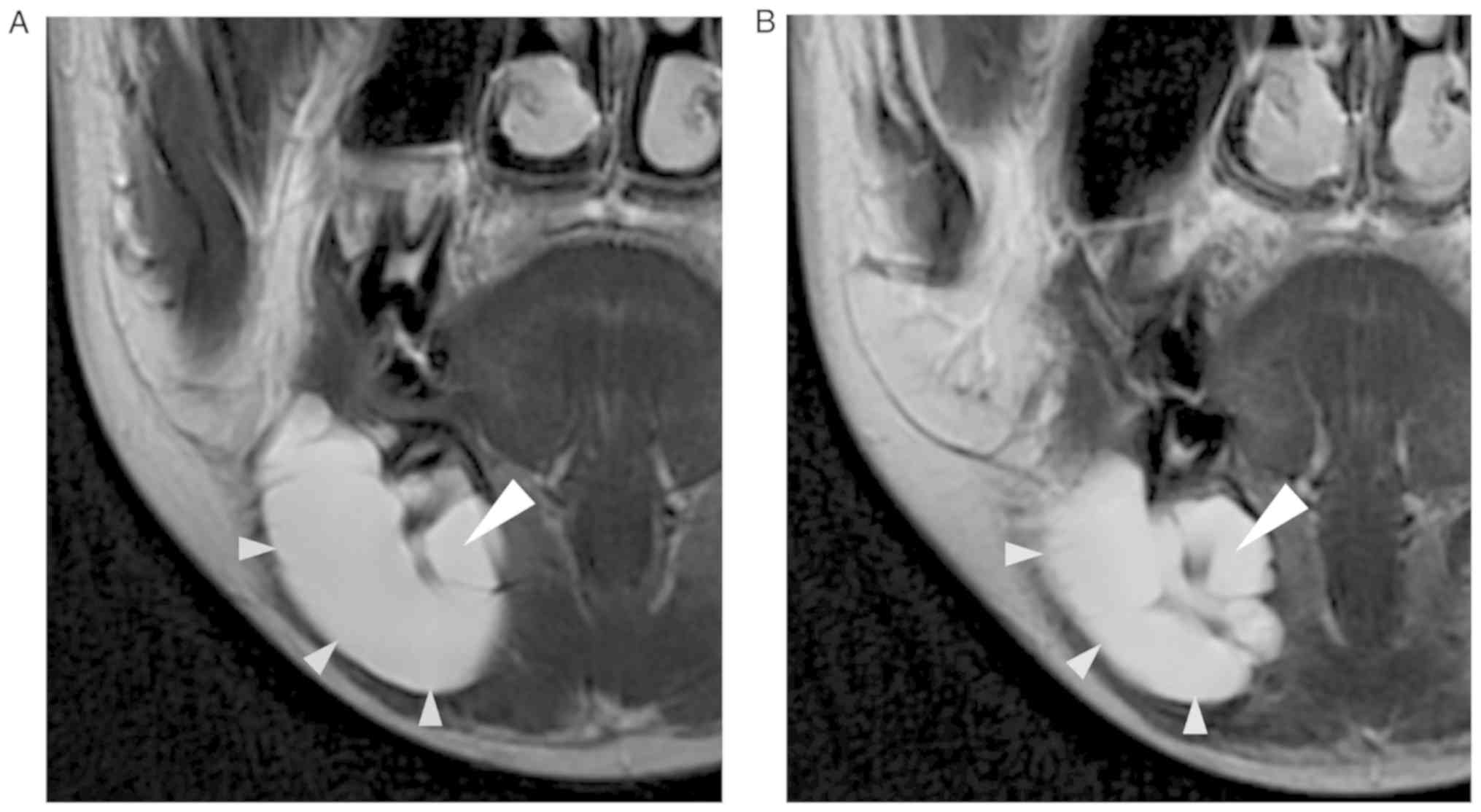
magnetic resonance imaging (MRI) demonstrated homogeneous
intermediate signal intensity on the T1-weighted image and
homogeneous high signal intensity including linear low signal area,
which was considered an inferior alveolar nerve on the T2-weighted
image (Fig. 3A and B). Laboratory
experiments were conducted at the Department of Clinical Laboratory
in University of Fukui Hospital to find the white blood cell count
(6,100 cells/µl; normal range, 3,300–8,600 cells/µl) and C-reactive
protein level (0.01 mg/dl; normal range, 0–0.14 mg/dl); no abnormal
findings were revealed. The normal ranges were based on the result
of measurements performed by the Department of Clinical Laboratory
in University of Fukui Hospital. The results of these examinations
indicated that the lesion was SBC or odontogenic cyst. To minimize
the surgical invasion, the authors planned to treat the lesion with
fenestration surgery using the tooth extraction socket of the right
mandibular third molar.
A total of 2 weeks following the first visit, the
authors performed the fenestration surgery under general
anesthesia. The alveolar bone of the right mandibular third molar
region was removed and the serous fluid was released as soon as the
instrument reached the lesion. The impacted right mandibular third
molar was then extracted. No neoplastic lesion or cyst wall was
found in the lesion by visual observation from the tooth extraction
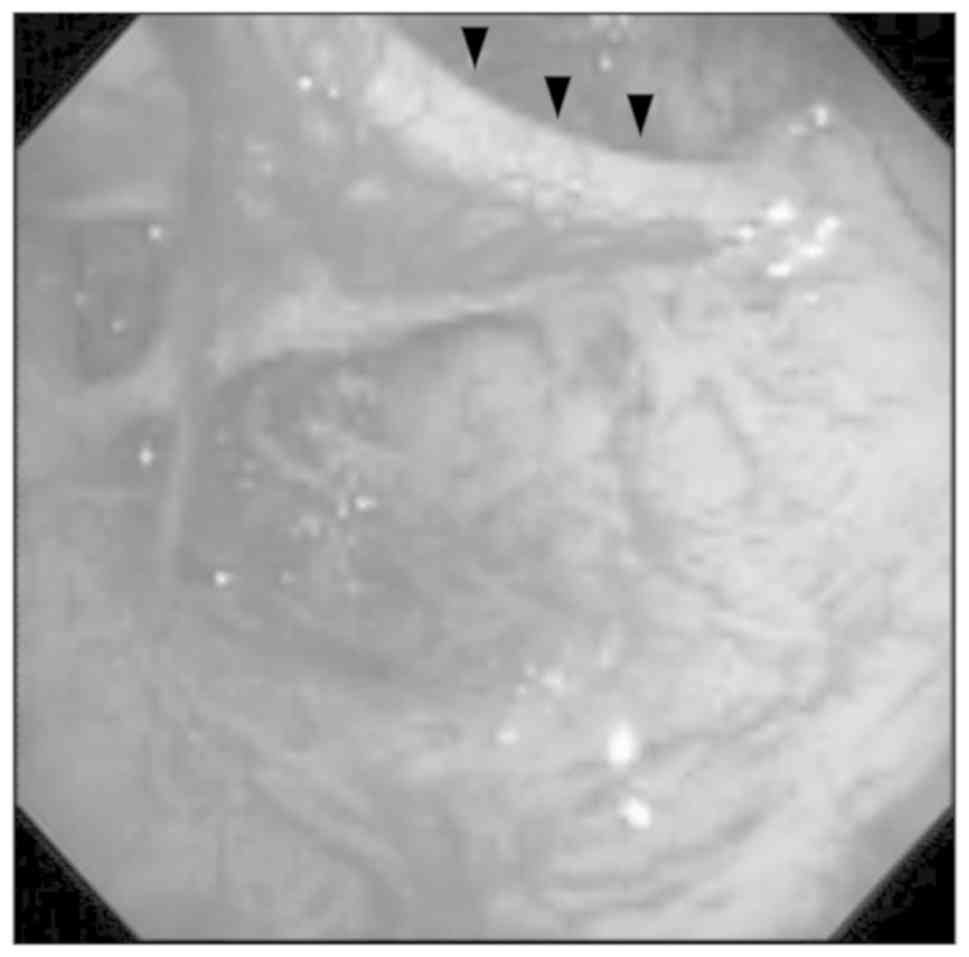
socket of the right mandibular third molar. An endoscope was
subsequently inserted through the socket and the lesion lumen was
observed, confirming that the lesion lumen was surrounded by
cortical bone without an epithelial lining. These results indicated
that the lesion was SBC. Furthermore, an inferior alveolar
neurovascular bundle floating in the lesion lumen was confirmed via
endoscopic examination (Fig. 4).
Endoscopy also revealed that the inferior alveolar neurovascular
bundle branched off into the incisive and mental nerve bundle in
the anterior part of the lesion lumen. These results were
consistent with the linear low signal area of the preoperative
T2-weighted MRI. The tooth extraction socket was packed with gauzes
including Bacitracin-fradiomycin sulfate (TOYO Pharmaceutical Co.,
Ltd, Osaka, Japan). Cefazolin sodium (2 g/day, twice a day) was
administered intravenously for 5 days, and then Cefdinir (300
mg/day, three times a day; both Astellas Pharma Inc., Tokyo, Japan)
was orally administered for 4 days.
Histopathological examinations performed by another
scientist in the division of Surgical Pathology, University of
Fukui (Fukui, Japan). The examinations of the soft tissues around
the right third molar exhibited no evidence of neoplasia. The
patient was subsequently diagnosed with SBC based on the results of
histopathological examination, transparent serous content fluid
from the lesion and intraoperative results including those of
endoscopy.
The postoperative course, such as postoperative
haemorrhage or postoperative pain, was uneventful and swelling in
the right buccal region decreased. The tooth extraction socket of
the right mandibular third molar was closed 4 months following the
first visit. A follow-up CT scan was performed 5 months following
the first visit (Fig. 5). It
revealed bone regeneration of the lesion area and the regeneration
of the mandibular canal in the linear low signal area of the
T2-weighted preoperative MRI was confirmed. A total of 17 months
after the operation, clinical findings associated with recurrence
have not been observed.
Discussion
In the present case, an inferior alveolar
neurovascular bundle floating in the lesion lumen of SBC was
confirmed endoscopically. These results were consistent with the
linear low signal area of the preoperative T2-weighted MRI.
Furthermore, regeneration of the mandibular canal in the linear low
signal area of the T2-weighted preoperative MRI was confirmed in
the postoperative follow-up CT scan 5 months following the first
visit.
The etiology of SBC is controversial, but three
predominant hypotheses have been presented for its occurrence: i)
An abnormality of bone growth, ii) the tumor degeneration process
and iii) traumatic-hemorrhagic theory (4). Although the traumatic-hemorrhagic
theory is the most widely accepted, >50% of patients with SBC
have no history of trauma (4).
Further, the patient of the present case exhibited no remarkable
traumatic history. Harnet et al (4) have indicated that the
traumatic-hemorrhagic theory may apply to the mandible due to
microtraumas to the teeth and alveolar bone. Previous literature
has also reported cases of SBC accompanied by an expansion of the
cortical plate and the displacement of the mandibular canal
(6,8,9). Mathew
et al (8) speculated that the
displacement of the mandibular canal is caused by a local rise in
osmotic pressure or intraosseous hematoma formation, which may
support the traumatic-hemorrhagic theory as etiology. In addition,
Matsumura et al (6) analyzed
53 SBCs and reported that there was no significant association
between the radiographic margin, tooth margins, displacement of the
mandibular canal, and histopathological results.
Hatakeyama et al (2) reported a case of mandibular condyle SBC
treated using an endoscope, which had the advantage of observing
the lesion lumen of the mandible with minimal surgical invasion. In
the current case, an endoscope was inserted through the tooth
extraction socket of the right mandibular third molar, from which
the entire lesion lumen was observed. Consequently, it was
confirmed that the lesion lumen was surrounded by cortical bone
without an epithelial lining, which is a characteristic of SBCs.
The present case indicated that the combination of tooth extraction
and endoscopy minimizes surgical invasion for the treatment of SBC
including the third molar tooth.
Surgical exploration and biopsy are necessary to
diagnose various radiolucent lesions, including SBC (10,11).
Treatment methods for SBC include curettage of the bone wall,
fenestration, packing the cavity, aspiration and osteotomy
(12). Curettage is often sufficient
to stimulate bleeding and facilitate osteogenesis (11). Additionally, graft materials are used
for treatment of larger SBCs (10).
However, SBC often heals spontaneously (11). To minimize surgical invasion,
fenestration surgery using the tooth extraction socket of the right
mandibular third molar was performed in the present case. Suei
et al (12) reported that
recurrence was observed in 2 of 13 patients with SBC that were
treated using fenestration. In addition, Suei et al
suggested an association between the prognosis and radiographic
features of SBCs, including absent lamina dura, scalloped margins,
nodular bone expansion, radiopaque mass and multiple cavities
(12). In the present case, the
postoperative course was uneventful and a follow-up CT scan 5
months after the first visit revealed bone regeneration in the
lesion area. However, the follow-ups will continue for the
foreseeable future as a long-term follow-up is necessary to account
for the possibility of recurrence, as the radiographic examination
performed at the first visit revealed resorbed lamina dura.
Several limitations of endoscopic surgical procedure
for SBCs should be considered. First, it may be difficult to use in
SBCs with a multilocular appearance included internal structure,
including trabeculae or septa (13).
Second, some SBCs do not exhibit bony expansions (14). Third, SBCs with teeth, which are
acceptable for dental extraction in lesion areas, are rare
(13,14).
In conclusion, the present case revealed that
inferior alveolar neurovascular bundles can float through the
lesion lumen of SBC. Furthermore, T2-weighted MRI may be useful in
confirming the course of the inferior alveolar neurovascular bundle
in SBC. As SBC is often observed in the second decade of life
(2), it is preferable to minimize
surgical invasion. However, in the narrow surgical field,
clinicians should consider the possibility of the floating inferior
alveolar neurovascular bundle in the lesion and avoid damage to the
neurovascular bundle itself.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
SM contributed to the conception and writing the
manuscript. HY and KS revised the manuscript. All authors wrote the
original medical record, analyzed the clinical data, and read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient's parents for the publication of the case and accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Rushton MA: Solitary bone cysts in the
mandible. Br Dent J. 81:37–49. 1946.PubMed/NCBI
|
|
2
|
Hatakeyama D, Tamaoki N, Iida K, Yonemoto
K, Kato K, Makita H, Toida M and Shibata S: Simple bone cyst of the
mandibular condyle in a child: Report of a case. J Oral Maxillofac
Surg. 70:2118–2123. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Speight PM and Takata T: New tumour
entities in the 4th edition of the World Health Organization
Classification of Head and Neck tumours: Odontogenic and
maxillofacial bone tumours. Virchows Arch. 472:331–339. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Harnet JC, Lombardi T, Klewansky P, Rieger
J, Tempe MH and Clavert JM: Solitary bone cyst of the jaws: A
review of the etiopathogenic hypotheses. J Oral Maxillofac Surg.
66:2345–2348. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Suomalainen A, Apajalahti S, Kuhlefelt M
and Hagström J: Simple bone cyst: A radiological dilemma.
Dentomaxillofac Radiol. 38:174–177. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Matsumura S, Murakami S, Kakimoto N,
Furukawa S, Kishino M, Ishida T and Fuchihata H: Histopathologic
and radiographic findings of the simple bone cyst. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 85:619–625. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Strabbing EM, Gortzak RA, Vinke JG,
Saridin CP and van Merkesteyn JP: An atypical presentation of a
solitary bone cyst of the mandibular ramus: A case report. J
Craniomaxillofac Surg. 39:145–147. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mathew R, Omami G, Gianoli D and Lurie A:
Unusual cone-beam computerized tomography presentation of traumatic
(simple) bone cyst: Case report and radiographic analysis. Oral
Surg Oral Med Oral Pathol Oral Radiol. 113:410–413. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
MacDonald-Jankowski DS: Traumatic bone
cysts in the jaws of a Hong Kong Chinese population. Clin Radiol.
50:787–791. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Robinson RA and Vincent SD: Idiopathic and
developmental abnormalities. AFIP atlas of tumor pathology series
4, Tumor and cysts of the jaws. ARP Press. (Silver Spring,
Maryland). 43–48. 2012.
|
|
11
|
El-Naggar AK, Chan JKC, Grandis JR, Takata
T and Slootweg PJ: Giant cell lesions and bone cysts. World Health
Organization classification of tumors, WHO classification of head
and neck tumours. WHO Press. (Geneva). 256–260. 2017.
|
|
12
|
Suei Y, Taguchi A, Nagasaki T and Tanimoto
K: Radiographic findings and prognosis of simple bone cysts of the
jaws. Dentomaxillofac Radiol. 39:65–71. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Imanimoghaddam M, Javadian Langaroody A,
Nemati S and Ataei Azimi S: Simple bone cyst of the mandible:
Report of two cases. Iran J Radiol. 8:43–46. 2011.PubMed/NCBI
|
|
14
|
Madiraju G, Yallamraju S, Rajendran V and
SrinivasaRao K: Solitary bone cyst of the mandible: A case report
and brief review of literature. BMJ Case Rep.
2014:bcr20132009452014. View Article : Google Scholar : PubMed/NCBI
|