Introduction
The prevalence of diabetes mellitus (DM) has been
rapidly increasing due to an aging population, urbanization,
physical inactivity and obesity (1).
An estimated 200 million individuals are affected by DM worldwide
(2). Coronary artery disease (CAD)
is the major cause of death in patients with DM. Affected patients
are frequently asymptomatic regarding CAD until the development of
myocardial infarction or sudden cardiac death (3). CAD is usually significantly more
advanced in patients with DM at the time-point of diagnosis
(4,5). Its asymptomatic presentation and
aggressiveness have made CAD the most common cause of death in
patients with DM (6).
Non-invasive imaging methods for the detection of
CAD have evolved rapidly over the past decades. With the advance of
multidetector row computed tomography (CT), coronary CT angiography
(CTA) has been effective in providing information on the extent and
morphology of CAD, including disease severity, lesion location and
characteristics of atherosclerotic plaques (7). It has been extensively validated that
the combination of CTA with coronary calcium scoring is sensitive
and specific in detecting CAD (8).
Since CAD is frequently asymptomatic in patients with DM, coronary
CTA may be applied to decrease cardiovascular morbidity and
mortality through the early detection of CAD in DM patients at
risk. CAD-associated CTA findings in patients with asymptomatic DM
were reported to be associated with a higher risk of cardiac events
(9–11).
Previous studies have investigated the association
between DM and the risk of CAD among diabetic patients undergoing
coronary CTA (12). However, only
few studies have analyzed the prognostic role of CTA in Chinese
patients with DM that are asymptomatic regarding CAD. The present
study assessed the prognostic role of coronary CTA in Chinese
patients with type 2 DM (T2DM) who exhibited no symptoms of
CAD.
Materials and methods
Subjects
A total of 164 Chinese T2DM patients that were
asymptomatic regarding CAD and underwent coronary CTA at the
Weifang Traditional Chinese Hospital (Weifang, China) between
January 2011 and March 2012 were enrolled in the present study.
T2DM was confirmed according to the criteria of the American
Diabetes Association (13). Glycated
hemoglobin (HbA1c) levels of ≥6.5%, fasting blood glucose levels of
≥126 mg/dl and/or a post-challenge blood glucose level of ≥200
mg/dl (2 h after a 75-g oral glucose load). The asymptomatic status
of the subjects was evaluated using the Rose questionnaire for
angina (14). Patients without CAD
were defined as asymptomatic.
A structured interview was performed by a physician
prior to the study to record the demographic and clinical data.
Hypertension was defined as a systolic blood pressure of ≥140 mmHg
and/or a diastolic blood pressure of ≥90 mmHg, or the use of
anti-hypertensive medication (15).
Dyslipidemia was defined as ongoing treatment with lipid-lowering
medications at the time of examination, or known but untreated
dyslipidemia. The exclusion criteria were as follows: i) T1
diabetes; ii) known or suspected CAD; iii) abnormal resting
electrocardiographic results; iv) history of prior myocardial
infarction, coronary revascularization or heart failure; v) history
of allergy to iodinated contrast. The present study was approved by
the Review Board of Weifang Traditional Chinese Hospital (Weifang,
China) and written informed consent was provided by all
patients.
Coronary CTA
Scans were analyzed by two experienced radiologists.
All examinations were performed using the Sensation 64 Slice CT
scanner (Siemens AG, Munich, Germany). The coronary artery calcium
(CAC) score was calculated using the Agatston method (16). Coronary CTA was performed using the
electrocardiogram-gated protocol: Detector collimation 64 (32×2) ×
0.6 mm, 80–120 kV assessed according to the patient's body habitus,
240–400 mA/rotation according to the patient's body habitus,
rotation time of 0.33 sec, radiation dose of 8–13 mSv, pitch value
of 0.2–0.5 according to the patient's heart rate. Next, 55–80 ml
iodine (400 mg/ml; Iomeron; Bracco Imaging SpA, Milan, Italy) was
injected at 4–6 ml/sec.
Coronary arteries were divided into 18 segments
following the Society of Cardiovascular Computed Tomography
guidelines (14). Each segment was
examined for coronary plaques. Structures of >1 mm2
adjacent to or within the coronary artery lumen that could be
clearly separated from the vessel lumen, was scored as a coronary
plaque (17). Each coronary segment
was scored individually for the presence of plaque and stenosis was
visually quantified. The severity of stenosis was categorized as
follows: <25, 25–49, 50–69, 70–99 and 100%. A stenosis of ≥50%
was considered obstructive. CAD was defined as the presence of any
coronary plaques or a CAC score of >0. A CAC score of 0 and no
coronary plaques signified the absence of CAD.
End-points and follow-up
Medical treatments, including the administration of
anti-hypertensive agents, statins and anti-diabetic agents, were
continued during the acquisition of the data for the present study.
The primary end-point was time to occurrence of any cardiac event.
A cardiac event was defined as a composite of non-fatal myocardial
infarction, unstable angina that required hospitalization, cardiac
death and late coronary revascularization.
A 5-year follow-up was performed by a research nurse
or dedicated physician. Any clinical events were determined by a
phone and/or face-to-face interview with the patients, and/or based
on their medical records.
Statistical analysis
Continuous variables are expressed as the mean ±
standard deviation. The differences in continuous variables among
normal, non-obstructive and obstructive CAD groups were compared
using one-way analysis of variance. A post-hoc test (Tukey's test)
was performed to identify differences between two groups.
Differences in categorical variables were assessed using the
χ2 test. Event-free survival curves were plotted using
the Kaplan-Meier method and compared using the log-rank test.
Univariate and multivariate Cox regression analyses were performed
to identify risk factors associated with cardiac events, including
age, sex, duration of DM, body mass index, systolic and diastolic
blood pressure, hypertension, smoking, family history of CAD,
dyslipidemia, previous stroke, previous peripheral arterial
disease, fasting blood glucose, HbA1c, creatinine, total
cholesterol, low-density lipoprotein (LDL) cholesterol,
high-density lipoprotein (HDL) cholesterol, triglycerides and
anti-DM treatment. Hazard ratios (HR) with 95% confidence intervals
(CIs) were calculated to determine the prognostic factors for
asymptomatic T2DM. P<0.05 (α=0.05) was considered to indicate a
statistically significant difference. All statistical analyses were
performed using SPSS 18.0 software (SPSS, Inc., Chicago, IL,
USA).
Results
Demographic characteristics of
subjects
Following coronary CTA, the patients were classified
into three groups, according to the stenosis diameter: Normal
coronary artery group, obstructive CAD group (≥50% stenosis) and
non-obstructive CAD group (<50% stenosis). The detailed
demographic information for all patients is listed in Table I. Significant differences were
observed in age, sex, duration of DM, family history of CAD,
previous stroke, total cholesterol, LDL cholesterol and
triglycerides among the three groups (all P<0.05). The mean age
of patients in the normal, non-obstructive and obstructive CAD
groups was (56.80±5.43), (58.64±3.22) and (60.61±2.72),
respectively, and significant differences were observed in the age
of patients among the three groups (P<0.001). The amount of
males was 21 (38.89%), 42 (68.85%) and 31 (63.26%) in the normal,
non-obstructive and obstructive CAD groups, respectively, and
significant differences were observed in the number of males among
the three groups (P=0.003). The results also revealed significant
differences in DM duration (P<0.001), hypertension (P=0.041),
family history of CAD (P=0.021), previous stroke (P<0.001),
total cholesterol (P<0.001), LDL cholesterol (P<0.001) and
triglyceride (P<0.001) among the normal, non-obstructive, and
obstructive CAD groups. The coronary CTA findings for all
participants are presented in Table
II.
 | Table I.Association of CAD status with
clinicopathological factors in asymptomatic patients with type 2
DM. |
Table I.
Association of CAD status with
clinicopathological factors in asymptomatic patients with type 2
DM.
| Item | No CAD (n=54) | Non-obstructive CAD
(n=61) | Obstructive CAD
(n=49) | P-value |
|---|
| Age (years) |
56.80±5.43 |
58.64±3.22a |
60.61±2.72a | <0.001 |
| Male gender | 21
(38.89) | 42 (68.85) | 31 (63.26) | 0.003 |
| Duration of DM
(years) |
9.07±2.14 |
11.48±1.34a |
13.71±1.87a,b | <0.001 |
| BMI
(kg/m2) |
25.33±3.17 |
25.64±3.37 |
25.92±2.15 | 0.610 |
| SBP (mm Hg) | 131.11±3.84 |
129.51±3.54 | 130.10±4.44 | 0.093 |
| DBP (mm Hg) |
72.96±3.31 |
72.23±2.47 |
72.80±3.43 | 0.405 |
| Hypertension | 28 (51.85) | 44
(72.13)a | 35 (71.43) | 0.041 |
| Current smoking | 11 (20.37) | 10 (16.39) | 8
(16.33) | 0.819 |
| Family history of
CAD | 3 (5.56) | 8
(13.11)a | 12
(24.49)a,b | 0.021 |
| Dyslipidemia | 31 (57.41) | 42 (68.85) | 27 (55.10) | 0.274 |
| Previous stroke | 4 (7.41) | 12
(19.67)a | 22
(44.90)a,b | <0.001 |
| Previous peripheral
arterial disease | 0 (0.00) | 1 (1.64) | 3 (6.12) | 0.116 |
| Fasting blood glucose
(mg/dl) | 140.52±4.70 | 141.67±5.74 | 140.16±3.42 | 0.221 |
| HbA1c (mmol/l) |
7.07±1.27 |
7.33±1.59 |
7.20±1.31 | 0.629 |
| Creatinine
(mg/dl) |
0.79±0.12 |
0.82±0.19 |
0.82±0.16 | 0.454 |
| Total cholesterol
(mg/dl) | 177.33±3.70 |
176.93±2.94 |
179.65±3.59a,b | <0.001 |
| LDL cholesterol
(mg/dl) | 130.91±3.78 |
128.44±3.01 |
133.61±4.76a,b | <0.001 |
| HDL cholesterol
(mg/dl) |
51.68±2.80 |
52.36±3.10 |
51.26±1.98 | 0.103 |
| Triglyceride
(mg/dl) | 130.91±3.78 |
128.44±3.0a |
133.61±4.76a,b | <0.001 |
| Diabetic
treatment |
|
|
| 0.492 |
| Diet only | 2 (3.70) | 4 (6.56) | 1 (2.04) |
|
| Oral hypoglycemic
agent | 52 (96.30) | 57 (93.44) | 48 (97.96) |
|
 | Table II.Coronary computed tomography
angiography findings for all participants. |
Table II.
Coronary computed tomography
angiography findings for all participants.
| Item | Value |
|---|
| CAC score | 91 (0–38) |
| Any plaque | 88 (53.6) |
| Plaque
characteristics |
|
Calcified | 58 (35.4) |
|
Non-calcified | 61 (37.2) |
|
Mixed | 45 (27.4) |
| Severity of
CAD |
| No
CAD | 54 (32.9) |
|
Non-obstructive CAD | 61 (37.2) |
|
Obstructive CAD | 49 (29.9) |
| Number of vessels
with obstructive CAD lesions |
| 1 | 17 (34.7) |
| 2 | 19 (38.8) |
| 3 | 13 (26.5) |
| High-risk CAD | 21 (12.8) |
| Segment involvement
score | 2.36±0.87 |
| Segment stenosis
score | 2.29±0.96 |
| Modified Duke
prognostic score | 1.48±0.68 |
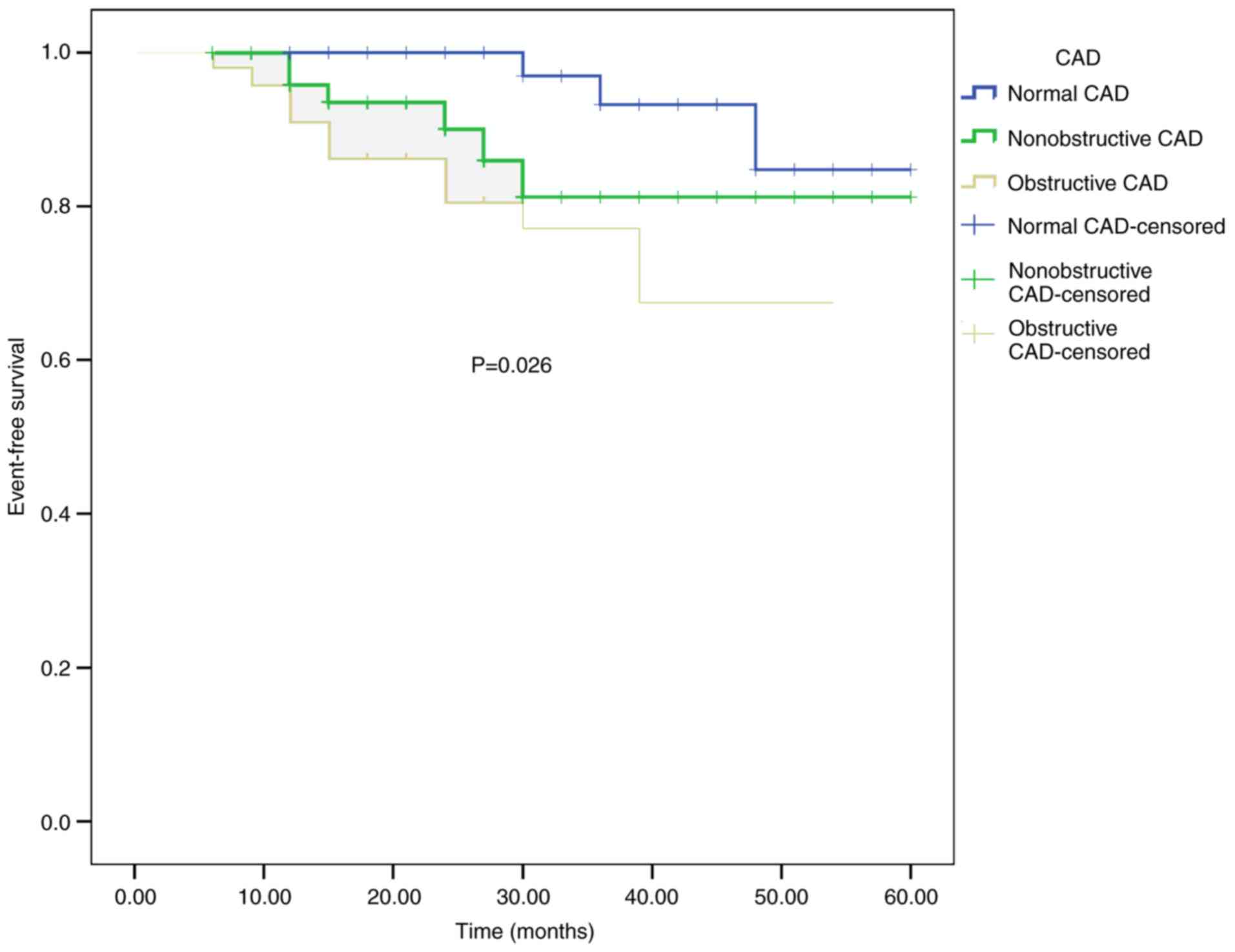
Kaplan-Meier survival curves
During the 5-year follow-up, 20 cardiac events were
recorded in the present study population (3 in the normal coronary
artery, 6 in the non-obstructive CAD and 11 in the obstructive CAD
group). The Kaplan-Meier curves indicated significant differences
in the event-free survival among the groups (P=0.026; Fig. 1).
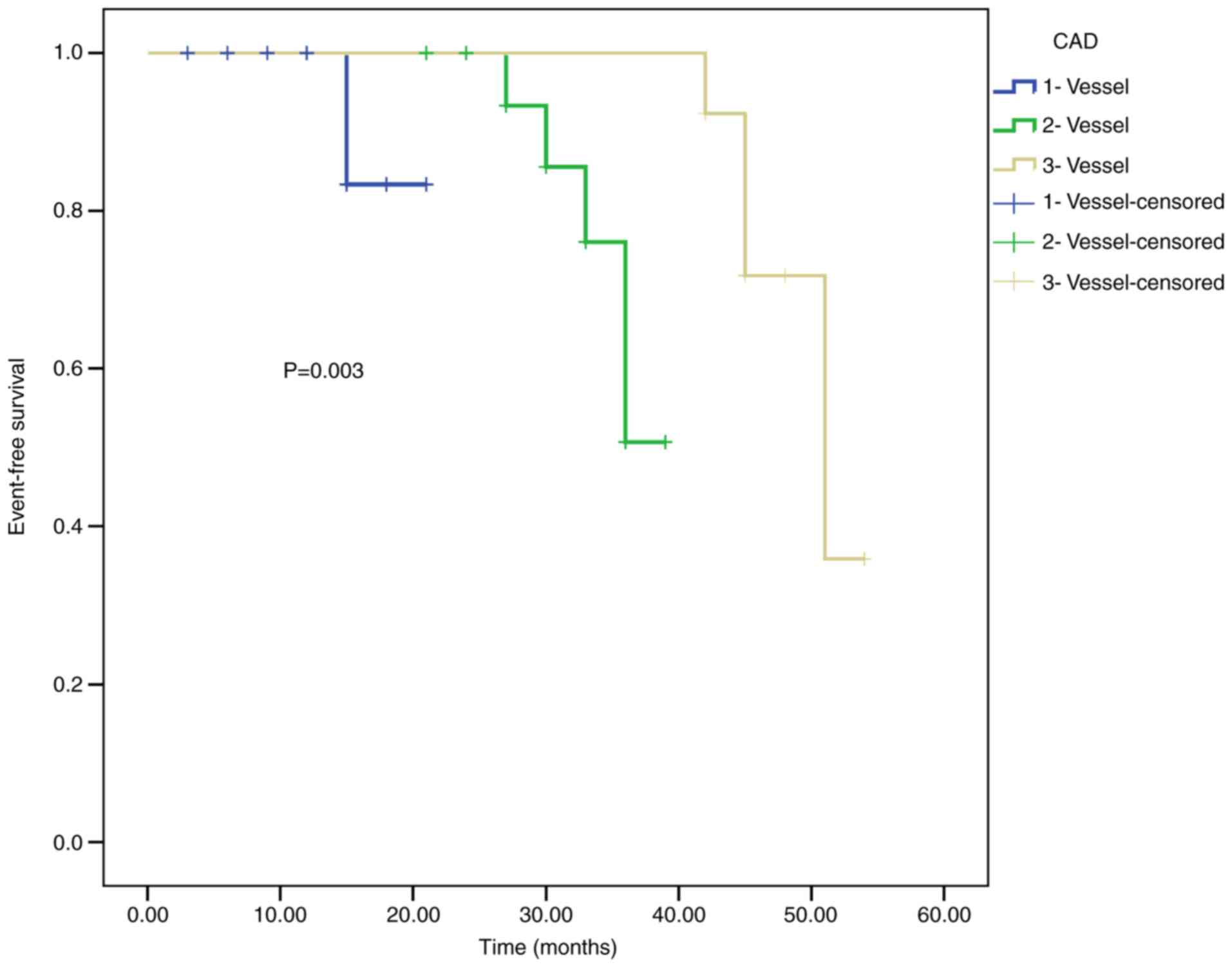
The patients with obstructive CAD comprised 17
patients with 1-vessel CAD, 19 with 2-vessel CAD and 13 with
3-vessel CAD. The survival rate of patients with 1-, 2- and
3-vessel CAD was analyzed (Fig. 2).
The event-free survival rate of patients with 1-vessel CAD was
94.11%, that of patients with 2-vessel CAD was 73.68% and that of
patients with 3-vessel CAD was 61.54%. The results indicated that
the prognosis of patients with 1-vessel CAD was better compared
with that of patients with 2- and 3-vessel CAD (P=0.003).
Multivariate Cox analysis
The results of multivariate Cox analysis are
presented in Table III. It was
observed that HDL cholesterol (HR=1.242, 95% CI: 1.024–1.507,
P=0.028) and triglycerides (HR=1.256, 95% CI: 1.113–1.416,
P<0.001) were independent prognostic factors in patients with
asymptomatic T2DM. The presence of non-obstructive and obstructive
CAD was indicated to be associated with the prognosis of patients
with asymptomatic T2DM (HR=11.132, 95% CI: 1.857–66.742, P=0.008;
HR=7.792, 95% CI: 1.750–34.698, P=0.007, respectively).
 | Table III.Uni- and multivariate Cox regression
analysis of the prognostic biomarkers for asymptomatic patients
with type 2 diabetes mellitus. |
Table III.
Uni- and multivariate Cox regression
analysis of the prognostic biomarkers for asymptomatic patients
with type 2 diabetes mellitus.
| A, Univariate
analysis |
|---|
|
|---|
| Factor | HR | 95% CI | P-value |
|---|
| Sex (male vs.
female) | 2.053 | 1.040–4.053 | 0.038 |
| Duration of DM
(>14 years vs. <14 years) | 1.214 | 1.027–1.436 | 0.023 |
| BMI (>26 vs.
<26) | 1.458 | 1.189–1.787 | <0.001 |
| SBP (>131 mmHg
vs. <131 mmHg) | 1.179 | 1.081–1.285 | <0.001 |
| DBP (>74 mmHg
vs. <74 mmHg) | 1.323 | 1.148–1.525 | <0.001 |
| HbA1c (>7 mmol/l
vs. <7 mmol/l) | 1.573 | 1.165–2.124 | 0.003 |
| Total cholesterol
(>179 mg/dl vs. <179 mg/dl) | 0.805 | 0.739–0.878 | <0.001 |
| Triglyceride
(>134 mg/dl vs. <134 mg/dl) | 1.427 | 1.251–1.627 | <0.001 |
| CTA finding |
| Non-obstructive CAD
vs. no CAD | 23.580 | 21.251–34.854 | 0.010 |
| Obstructive CAD vs.
no CAD | 17.526 | 14.852–28.413 | 0.022 |
|
| B, Multivariate
analysis |
|
| Factor | HR | 95% CI | P-value |
|
| Sex (male vs.
female) | 1.241 | 0.711–2.058 | 0.324 |
| Duration of DM
(>14 years vs. <14 years) | 0.853 | 0.747–1.259 | 0.114 |
| BMI (>26 vs.
<26) | 0.910 | 0.779–1.335 | 0.147 |
| SBP(>131 mmHg
vs. <131 mmHg) | 0.887 | 0.698–1.117 | 0.139 |
| DBP(>74 mmHg vs.
<74 mmHg) | 0.696 | 0.559–1.084 | 0.215 |
| HbA1c (>7 mmol/l
vs. <7 mmol/l) | 1.178 | 0.947–1.568 | 0.365 |
| Total cholesterol
(>179 mg/dl vs. <179 mg/dl) | 0.442 | 0.325–1.479 | 0.541 |
| HDL (>52 mg/dl
vs. <52 mg/dl) | 1.242 | 1.024–1.507 | 0.028 |
| Triglyceride
(>134 mg/dl vs. <134 mg/dl) | 1.256 | 1.113–1.416 | <0.001 |
| CTA finding |
| Non-obstructive CAD
vs. no CAD | 11.132 | 1.857–66.742 | 0.008 |
| Obstructive CAD vs.
no CAD | 7.792 | 1.750–34.698 | 0.007 |
Discussion
T2DM, a chronic metabolic disease, is a major health
concern, as it affects >382 million individuals worldwide
(18). CAD is the major cause of
death among patients with T2DM (19,20).
Population-based studies have reported a 2- to 4-fold frequency in
the number of cardiovascular events experienced by patients with
T2DM (21,22). The diagnosis of CAD is commonly
missed or delayed, since the symptoms of CAD are usually absent in
patients with T2DM, which in turn enhances the risk for
cardiovascular events.
Invasive coronary angiography (ICA) is considered
the gold standard for detecting the presence, localization and
severity of CAD. However, it is an invasive method associated with
complications. Furthermore, the procedural cost is substantial.
Coronary CTA is a recently introduced alternative to ICA for the
detection of CAD, and 64-slice multidetector CT has been found
highly effective in the diagnosis of significant coronary stenosis
(23). Liu et al (24) performed a CTA study in 150 T2DM
patients with a follow-up of ≥2 years and the results suggested
that CTA may be used as a non-invasive modality for predicting
high-risk CAD in patients with T2DM. A cross-sectional study by
Ulimoen et al (25) indicated
that coronary CTA had a high sensitivity (100%) and a negative
predictive value (100%) for detecting CAD, suggesting that it is a
reliable method for detecting significant CAD in T2DM and may prove
useful to clinicians. However, few studies have investigated the
prognostic role of CTA in Chinese T2DM patients that are
asymptomatic regarding CAD.
CTA provides detailed information on the morphology
and extent of CAD. The advantage of CTA is that it may be used to
exclude CTA in patients with a low-to-intermediate cardiovascular
risk, which is broadly endorsed by international societies
(26). Due to improvements in CTA
technology, the radiation dose per patient has been decreased to
acceptable levels. Sub-millisievert (mSv) scans with the latest
generation scanners use effectives dose of <1.0 mSv without
compromising the imaging quality (27). The Coronary Artery Evaluation Using
64-Row Multidetector CTA study identified a significant correlation
between CTA and ICA when testing the extent and severity of CAD
(28); this resulted in the
extensive clinical application of CTA. Fujimoto et al
(29) reported that the evaluation
of CTA plaque characteristics may provide an incremental prognostic
value to the number of diseased vessels and the Framingham risk
score (FRS). This evidence suggests a predictive role of CTA for
CAD. Blanke et al (30)
reported that among patients with DM, non-obstructive and
obstructive CAD, as determined by coronary CTA, were associated
with higher rates of all-cause mortality and major adverse
cardiovascular events at 5 years.
In the present study, 164 patients with asymptomatic
T2DM were enrolled, and CTA was performed to detect coronary
stenosis in all of them. The patients were classified into three
groups, based on the coronary CTA results: Normal coronary artery
group, obstructive CAD group (≥50% stenosis) and non-obstructive
CAD group (<50% stenosis). Significant differences in age, sex,
duration of DM, family history of CAD, previous stroke, total
cholesterol, LDL cholesterol and triglycerides were observed among
the three groups (all P<0.05). After a 5-year follow-up, 20
events were observed in the study population (3 for normal coronary
artery, 6 for the non-obstructive CAD and 11 for the obstructive
CAD group). The Kaplan-Meier curve indicated that the event-free
survival of subjects in the normal coronary artery group was the
highest among all participants (P=0.026). This result was
consistent with the study by Kang et al (31), which revealed that asymptomatic
patients with T2DM and normal coronary arteries, non-obstructive
CAD or coronary CTA exhibit excellent clinical outcomes over a
follow-up period of >5 years, whereas prognosis is worse in
patients with obstructive CAD (30).
Further Cox analysis demonstrated that non-obstructive and
obstructive CAD may serve as prognostic indicators for T2DM
patients that are asymptomatic. In addition, it was revealed that
the event-free survival rate in patients with 1-vessel CAD was
94.11%, that in patients with 2-vessel CAD was 73.68% and that
associated with 3-vessel CAD was 61.54%, indicating that the
prognosis of patients with 1-vessel CAD was better compared with
that of patients with 2- and 3-vessel CAD (P=0.003).
The results of the present study demonstrated that
coronary CTA testing may predict the prognosis of asymptomatic T2DM
patients. However, the present study had limitation: the sample
size was relatively small. Large-scale studies should be performed
in the future to confirm these results. Furthermore, only Chinese
patients examined at one hospital were enrolled in the present
study, and multiple-center studies are required to validate the
present results.
In conclusion, the results of coronary CTA may serve
as prognostic indicators for asymptomatic T2DM patients. The
event-free survival of patients with normal coronary arteries was
markedly higher compared with that of patients with non-obstructive
and obstructive CAD. Furthermore, the prognosis of patients with
1-vessel CAD is better compared with that of patients with 2- and
3-vessel CAD.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All the datasets generated and analyzed in the
present study are included in this published manuscript/are
available from the corresponding author on reasonable request.
Authors' contributions
QN designed the current study. PT, XZ and ML
performed the experiments. PT, MZL and WL analyzed the data. PT and
XZ drafted the manuscript. ML, WL, and QN revised the
manuscript.
Ethics approval and consent to
participate
The present study was approved by the ethics
committee of Weifang Traditional Chinese Hospital (Weifang, China).
Written informed consent was provided by all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
King H, Aubert RE and Herman WH: Global
burden of diabetes, 1995–2025: Prevalence, numerical estimates, and
projections. Diabetes Care. 21:1414–1431. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
International diabetes federation, .
International diabetes federation. 2013.
|
|
3
|
Young LH, Wackers FJ, Chyun DA, Davey JA,
Barrett EJ, Taillefer R, Heller GV, Iskandrian AE, Wittlin SD,
Filipchuk N, et al: Cardiac outcomes after screening for
asymptomatic coronary artery disease in patients with type 2
diabetes: The DIAD study: A randomized controlled trial. JAMA.
301:1547–1555. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Goraya TY, Leibson CL, Palumbo PJ, Weston
SA, Killian JM, Pfeifer EA, Jacobsen SJ, Frye RL and Roger VL:
Coronary atherosclerosis in diabetes mellitus: A population-based
autopsy study. J Am Coll Cardiol. 40:946–953. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hu FB, Stampfer MJ, Haffner SM, Solomon
CG, Willett WC and Manson JE: Elevated risk of cardiovascular
disease prior to clinical diagnosis of type 2 diabetes. Diabetes
Care. 25:1129–1134. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Grundy SM, Benjamin IJ, Burke GL, Chait A,
Eckel RH, Howard BV, Mitch W, Smith SC Jr and Sowers JR: Diabetes
and cardiovascular disease: A statement for healthcare
professionals from the American heart association. Circulation.
100:1134–1146. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Park GM, Lee SW, Cho YR, Kim CJ, Cho JS,
Park MW, Her SH, Ahn JM, Lee JY, Park DW, et al: Coronary computed
tomographic angiographic findings in asymptomatic patients with
type 2 diabetes mellitus. Am J Cardiol. 113:765–771. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Petcherski O, Gaspar T, Halon DA, Peled N,
Jaffe R, Molnar R, Lewis BS and Rubinshtein R: Diagnostic accuracy
of 256-row computed tomographic angiography for detection of
obstructive coronary artery disease using invasive quantitative
coronary angiography as reference standard. Am J Cardiol.
111:510–515. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Andreini D, Pontone G, Mushtaq S, Bertella
E, Conte E, Baggiano A, Veglia F, Agostoni P, Annoni A, Formenti A,
et al: Prognostic value of multidetector computed tomography
coronary angiography in diabetes: Excellent long-term prognosis in
patients with normal coronary arteries. Diabetes Care.
36:1834–1841. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cho I, Chang HJ, Sung JM, Pencina MJ, Lin
FY, Dunning AM, Achenbach S, Al-Mallah M, Berman DS, Budoff MJ, et
al: Coronary computed tomographic angiography and risk of all-cause
mortality and nonfatal myocardial infarction in subjects without
chest pain syndrome from the CONFIRM Registry (coronary CT
angiography evaluation for clinical outcomes: An international
multicenter registry). Circulation. 126:304–313. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hadamitzky M, Hein F, Meyer T, Bischoff B,
Martinoff S, Schömig A and Hausleiter J: Prognostic value of
coronary computed tomographic angiography in diabetic patients
without known coronary artery disease. Diabetes Care. 33:1358–1363.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Krul MM, Bogaard K, Knol RJ, van Rossum
AC, Knaapen P, Cornel JH and van der Zant FM: Coronary artery
disease in patients with atypical chest pain with and without
diabetes mellitus assessed with coronary CT angiography. BMJ Open
Diabetes Res Care. 2:e0000042014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
American Diabetes Association: Diagnosis
and classification of diabetes mellitus. Diabetes Care. 33 (Suppl
1):S62–S69. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Raff GL, Abidov A, Achenbach S, Berman DS,
Boxt LM, Budoff MJ, Cheng V, DeFrance T, Hellinger JC and Karlsberg
RP; Society of Cardiovascular Computed Tomography, : SCCT
guidelines for the interpretation and reporting of coronary
computed tomographic angiography. J Cardiovasc Comput Tomogr.
3:122–136. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
European Society of Hypertension-European
Society of Cardiology Guidelines Committee, . 2003 European society
of hypertension european society of cardiology guidelines for the
management of arterial hypertension. J Hypertens. 21:1011–1053.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Agatston AS, Janowitz WR, Hildner FJ,
Zusmer NR, Viamonte M Jr and Detrano R: Quantification of coronary
artery calcium using ultrafast computed tomography. J Am Coll
Cardiol. 15:827–832. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Choo EH, Kim JJ, Hwang BH, Choi IJ, Chang
M, Lim S, Koh Y, Park HJ, Kim PJ, Lee SH, et al: Status of
hypertension and coronary stenosis in asymptomatic type 2 diabetic
patients: Analysis from coronary computed tomographic angiography
registry. Int J Cardiol. 174:282–287. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
IDF Diabetes Atlas 6th Edition, .
International Diabetes Federation; Brussels: 2013, https://www.idf.org/diabetesatlas
|
|
19
|
Lorber D: Importance of cardiovascular
disease risk management in patients with type 2 diabetes mellitus.
Diabetes Metab Syndr Obes. 7:169–183. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stamler J, Vaccaro O, Neaton JD and
Wentworth D: Diabetes, other risk factors, and 12-yr cardiovascular
mortality for men screened in the multiple risk factor intervention
trial. Diabetes Care. 16:434–444. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Becker A, Bos G, de Vegt F, Kostense PJ,
Dekker JM, Nijpels G, Heine RJ, Bouter LM and Stehouwer CD:
Cardiovascular events in type 2 diabetes: Comparison with
nondiabetic individuals without and with prior cardiovascular
disease. 10-year follow-up of the Hoorn study. Eur Heart J.
24:1406–1413. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Schramm TK, Gislason GH, Køber L,
Rasmussen S, Rasmussen JN, Abildstrøm SZ, Hansen ML, Folke F, Buch
P, Madsen M, et al: Diabetes patients requiring glucose-lowering
therapy and nondiabetics with a prior myocardial infarction carry
the same cardiovascular risk: A population study of 3.3 million
people. Circulation. 117:1945–1954. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Janne d'Othée B, Siebert U, Cury R, Jadvar
H, Dunn EJ and Hoffmann U: A systematic review on diagnostic
accuracy of CT-based detection of significant coronary artery
disease. Eur J Radiol. 65:449–461. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu D, Jia H, Liu W, Ma D, Tan G, He W, Fu
Y and Wang LX: Value of multi-detector computed tomography
angiography in predicting acute cardiac events in patients with
type 2 diabetes. Exp Ther Med. 7:917–922. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ulimoen GR, Ofstad AP, Endresen K,
Gullestad L, Johansen OE and Borthne A: Low-dose CT coronary
angiography for assessment of coronary artery disease in patients
with type 2 diabetes-a cross-sectional study. BMC Cardiovasc
Disord. 15:1472015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Taylor AJ, Cerqueira M, Hodgson JM, Mark
D, Min J, O'Gara P, Rubin GD; American College of Cardiology
Foundation Appropriate Use Criteria Task Force; Society of
Cardiovascular Computed Tomography; American College of Radiology,
; et al: ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010
appropriate use criteria for cardiac computed tomography. A report
of the American College of Cardiology Foundation Appropriate Use
Criteria Task Force, the Society of Cardiovascular Computed
Tomography, the American College of Radiology, the American Heart
Association, the American Society of Echocardiography, the American
Society of Nuclear Cardiology, the North American society for
cardiovascular imaging, the society for cardiovascular angiography
and interventions, and the society for cardiovascular magnetic
resonance. J Am Coll Cardiol. 56:1864–1894. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Achenbach S, Marwan M, Ropers D, Schepis
T, Pflederer T, Anders K, Kuettner A, Daniel WG, Uder M and Lell
MM: Coronary computed tomography angiography with a consistent dose
below 1 mSv using prospectively electrocardiogram-triggered
high-pitch spiral acquisition. Eur Heart J. 31:340–346. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Miller JM, Rochitte CE, Dewey M,
Arbab-Zadeh A, Niinuma H, Gottlieb I, Paul N, Clouse ME, Shapiro
EP, Hoe J, et al: Diagnostic performance of coronary angiography by
64-row CT. N Engl J Med. 359:2324–2336. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fujimoto S, Kondo T, Takamura K, Baber U,
Shinozaki T, Nishizaki Y, Kawaguchi Y, Matsumori R, Hiki M,
Miyauchi K, et al: Incremental prognostic value of coronary
computed tomographic angiography high-risk plaque characteristics
in newly symptomatic patient. J Cardiol. 67:538–544. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Blanke P, Naoum C, Ahmadi A, Cheruvu C,
Soon J, Arepalli C, Gransar H, Achenbach S, Berman DS, Budoff MJ,
et al: In the present study, we enrolled 164 asymptomatic patients
with T2DM and performed CTA to detect coronary stenosis on all of
them. JACC Cardiovasc Imaging. 9:1280–1288. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kang SH, Park GM, Lee SW, Yun SC, Kim YH,
Cho YR, Park HW, Suh J, Yang DH, Kang JW, et al: Long-term
prognostic value of coronary CT angiography in asymptomatic type 2
diabetes mellitus. JACC Cardiovasc Imaging. 9:1292–1300. 2016.
View Article : Google Scholar : PubMed/NCBI
|