Introduction
Myopic foveoschisis (MF) was first described in 1958
as a posterior retinal detachment without macular hole (1). It is a common complication in patients
with myopia (2). It is
characteristic of a macular intraretinal cleavage in myopic
posterior staphyloma, and cannot be easily detected due to the poor
contrast between the myopic retina and the choroid (3). However, hyporeflective splitting
between the thin and faint reflective outer retina and the thicker,
more reflective inner retina may be detected on an optical
coherence tomography (OCT) scan (4),
and its existence has been increasingly recognized with the arrival
of OCT (5,6). The estimated morbidity of MF ranges
between 8 and 34% in highly myopic eyes (7). The pathogenesis of MF is not clear.
However, vitreous traction, decreased elasticity of the ILM, and a
stretched retina due to staphyloma have been deemed to be possible
causes (8). MF may be formed prior
to macular retinal detachment and macular hole, and cause visual
impairment, particularly when it affects the premacular structure
(9,10). Thus, in order to prevent the
deterioration of the anatomy and function of the retina, and
vision, surgical intervention is required for these patients
(11). The effectiveness of 20G
vitrectomy for MF has previously been demonstrated (12). The positive effect of vitrectomy also
demonstrates that vitreous traction serves an important role in the
development of MF. However, the surgical indications and the
treatment time are not yet clear. Zhang et al (13) reported that MF and visual acuity (VA)
deteriorated in 20 out of 29 eyes during a follow-up period of 31.2
months, and visual prognosis and surgical success rates have been
poor following development of a macular hole in myopic eyes with
posterior staphyloma (14).
Recently, there have been reports about minimally
invasive vitrectomy surgery (MIVS) in treating MF (12). 23-gauge (23G) vitrectomy is one type
of MIVS (15). The advantage of it
is that the incision does not require suturing (16). The evidence also demonstrates that
MIVS results in less inflammation, less discomfort, faster recovery
of VA and, occasionally, a shorter surgery time (12,17). The
ILM can be more easily visualized with brilliant blue (BB) staining
to aid peeling (15).
Removal of traction by ILM peeling is a key
component of numerous vitrectomy procedures (18). However, the evidence supporting the
requirement to peel the ILM is inconsistent. Studies that indicate
good outcomes following ILM peeling (15,19,20) are
countered by those that suggest that outcomes are improved without
ILM peeling, or by methods that reduce the peeling area (21). However, the majority of these studies
are case series that do not directly compare the two methods
(22,23), and those that do, suggest that
peeling the ILM may be preferable (24). The present study hypothesized that
23G vitrectomy with BB-assisted ILM peeling in the eyes of patients
with MF may provide a better outcome compared with 23G vitrectomy
alone. Therefore, the aim of the current study was to compare the
anatomical and visual outcomes of patients with MF treated by 23G
vitrectomy with and without ILM peeling.
Subjects and methods
Study design
The current retrospective cohort study included data
from patients treated with 23G vitrectomy for MF between March 2013
and August 2016 in the Department of Ophthalmology, The Second
Affiliated Hospital of Nanchang University (Nanchang, China).
Patients
Patients were included in the study according to the
following inclusion criteria: i) BCVA>0.4 (BCVA values were
obtained using the logMAR test); ii) presented with metamorphopsia;
iii) OCT examination revealed macular retinoschisis or macular
retinoschisis with macular traction; and iv) refractive error
>-6.0 diopters. The exclusion criteria were as follows: i) Eyes
with an apparent macular hole; ii) eyes with retinal detachment;
iii) eyes with glaucoma; and iv) eyes with choroidal
neovascularization, macular degeneration or submacular
hemorrhage.
The present study was performed in accordance with
the tenets of the Declaration of Helsinki. The current study was
approved by the Ethics Committee of The Second Affiliated Hospital
of Nanchang University [approval no. (2012)095]. The requirement
for written consent was waived by the Ethics Committee.
The patients were grouped to the peeling and
non-peeling groups according to whether they received BB-assisted
ILM peeling during the vitrectomy procedure or not. A total of 60
eyes from 60 patients were included in the study, and there were 30
eyes in each group.
Interventions
Patients in the peeling group underwent 23G pars
plana vitrectomy (ppv) and ILM peeling with gas tamponade
octafluoropropane (C3F8). Patients in the non-peeling group
underwent 23G ppv with gas tamponade (C3F8). In the two groups, if
patients had cataracts, phacoemulsification intraocular lens
implantation (IOL) was performed prior to the posterior segment
operation.
All operations were performed by the same
experienced surgeon. The procedure for patients in the peeling and
non-peeling groups was standard three-port 23G pars plana
vitrectomy. To avoid the effects of postoperative cataract
development, phacoemulsification with implantation of an
intraocular lens was performed in the phakic eyes. The vitrectomy
procedure consisted of core vitrectomy, creating a posterior
vitreous detachment, peripheral vitrectomy and shaving of the basal
vitreous body, the entire vitrectomy procedure was performed with
the aid of Resight 700 non-contact wide-angle lenses (+128
Diopters; Resight; Carl Zeiss AG, Oberkochen, Germany). The
residual posterior vitreous was identified using triamcinolone
acetonide (Xudong Haipu Pharmaceuticals, Co., Ltd., Shanghai,
China). The ILM was stained with 0.3 ml BB (Fluoron GmbH, Ulm,
Germany) in all patients of the peeling group, after entirely
removing the posterior hyaloid membrane and epiretinal membrane.
After 60 sec treatment with BB, peeling of the ILM was performed by
23G ILM forceps and a non-contact wide-viewing lens (+60D) for an
area of macular retinoschisis within the major vascular arcade and
staphyloma. To avoid damage to the retina, the point of ILM peeling
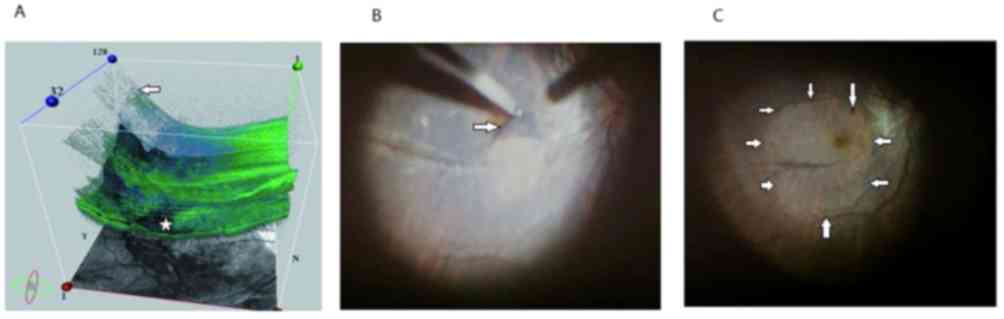
without inner retinoschisis was selected according to 3D analysis
with visualization software on OCT (CIRRUS™ HD
4000-3716-OCT; Carl Zeiss Meditec, Inc., Dublin, CA). In 3D-OCT
prior to vitrectomy, the outer retinoschisis (indicated by the
white arrow) was observed in the macular area and inner
retinoschisis (indicated by the white star) was observed in the
temporal area of the maculae (Fig.
1A). The ILM was stained blue in the intraoperative camera
under a +60D non-contact wide-viewing lens. The point of ILM
peeling was selected in the nasal-inferior area of the maculae
(indicated by white arrow; Fig. 1B).
In the intraoperative camera under a +128D non-contact wide-viewing
lens, no retinal break or hemorrhage was observed in the maculae
following ILM peeling (indicated by white arrows; Fig. 1C).
After peeling ILM, air-gas (16% C3F8) exchange was
performed subsequent to liquid-air exchange. When leakage was found
at the point of sclerotomy, the wound was sutured using 8-0
VICRYL® sutures (Johnson & Johnson, New Brunswick,
NJ, USA). Patients were asked to maintain a face-down position for
1 week.
Evaluations
All patients underwent ophthalmic examinations,
including BCVA and CMT, at baseline and at the final visit. The
examinations were undertaken using the logMAR test, Amsler test,
indirect ophthalmoscopy, slit-lamp biomicroscopy, color fundus
photography, OCT (13,25) and axial length was measured with an
optical biometer (IOL Master; Carl Zeiss AG). When OCT examination
revealed no MF, the MF was considered completely resolved; when OCT
examination revealed MF, and it was not considered to be as severe
as the preoperative diagnosis, the MF was considered partly
resolved. It was positive for Amsler's test when a vacancy or curve
was found by looking at the white spot in the center of Amsler's
grid.
Statistical analysis
All statistical analyses were performed with SPSS
software (version 11.0; SPSS Inc., Chicago, IL, USA). Qualitative
data are presented as a value and quantitative data are presented
as the mean ± standard deviation. Qualitative data were analyzed
using a χ2 test or t-'s exact test. Continuous variables
were analyzed using either the Wilcoxon signed-rank test or the
Mann-Whitney test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient demographics
A total of 30 eyes from 30 patients were included in
each group (Table I). The baseline
characteristics were similar between the two groups (all
P>0.05). The mean age of the patients was 43.8±8.0 years in the
peeling group and 42.8±7.8 years in the non-peeling group
(P=0.774). The mean axial length was 28.3±1.2 mm in the peeling
group compared with 28.5±1.2 mm in the non-peeling group (P=0.984).
The mean follow-up duration post-surgery was 16.5±2.0 months in the
peeling group and 16.7±1.9 months in the non-peeling group
(P=0.632). In the peeling group, 23 (76.7%) of the 30 eyes were
phakic prior to surgery and seven (23.3%) eyes were pseudophakic.
In the non-peeling group, 20 (66.7%) eyes were phakic prior to
surgery, and 10 (33.3%) were pseudophakic. The mean preoperative
BCVA (logMAR) was 0.84±0.29 in the peeling group and 0.81±0.30 in
the non-peeling group. The mean preoperative CMT was 458±62.2 µm in
the peeling group and 460±61.1 µm in the non-peeling group. A total
of 10 eyes had posterior staphyloma in the peeling group, and 11
eyes in the non-peeling group.
 | Table I.Baseline characteristics of the
patients. |
Table I.
Baseline characteristics of the
patients.
|
Characteristics | Peeling group
(n=30) | Non-peeling group
(n=30) | P-value | Test |
|---|
| Mean age ± SD,
years (range) | 43.8±8.0 | 42.8±7.8 | 0.774 | Mann-Whitney
test |
| Gender (M/F) | 11/19 | 12/18 | 0.792 | χ2 test |
| Mean AX ± SD, mm
(range) | 28.3±1.24 | 28.5±1.21 | 0.984 | Mann-Whitney
test |
| Preoperative
IOP | 15.3±5.5 | 15.0±5.2 | 0.912 | Mann-Whitney
test |
| Duration of MF ±
SD, months (range) | 6±3.1 | 6±3.3 | 0.964 | Mann-Whitney
test |
| Preoperative BCVA
in logMAR, mean ± SD | 0.84±0.29 | 0.81±0.30 | 0.822 | Mann-Whitney
test |
| Preoperative CMT,
mean ± SD | 458±62.2 | 460±61.1 | 0.229 | Mann-Whitney
test |
| Amsler test
positive, n | 21 | 22 | 0.781 | Mann-Whitney U
test |
| Preoperative lens
status, n |
|
| 0.390 | χ2 test |
| Phakic | 23 | 20 |
|
|
| Pseudophakic | 7 | 10 |
|
|
| Combined cataract
surgery, n | 18 | 16 | 0.594 | Mann-Whitney U
test |
| Duration of
Follow-up ± SD, months (range) | 16.5±2.0 | 16.7±1.9 | 0.632 | Mann-Whitney
test |
| PS, n | 10 | 11 | 0.994 | Mann-Whitney U
test |
Visual and anatomical outcomes
Postoperative Visual acuity (logMAR) improved from
the preoperative BCVA in the peeling and non-peeling group;
however, the differences were not statistically significant
(Table II). At the last follow-up,
the visual acuity was improved in 24 out of 30 eyes (80%) in the
peeling group and 25 eyes (83.3%) in the non-peeling group,
remained unchanged in four (13.3%) eyes in the peeling group and
three (10%) in the non-peeling group, and worsened in two eyes
(6.7%) in the peeling group and two eyes (6.7%) in the non-peeling
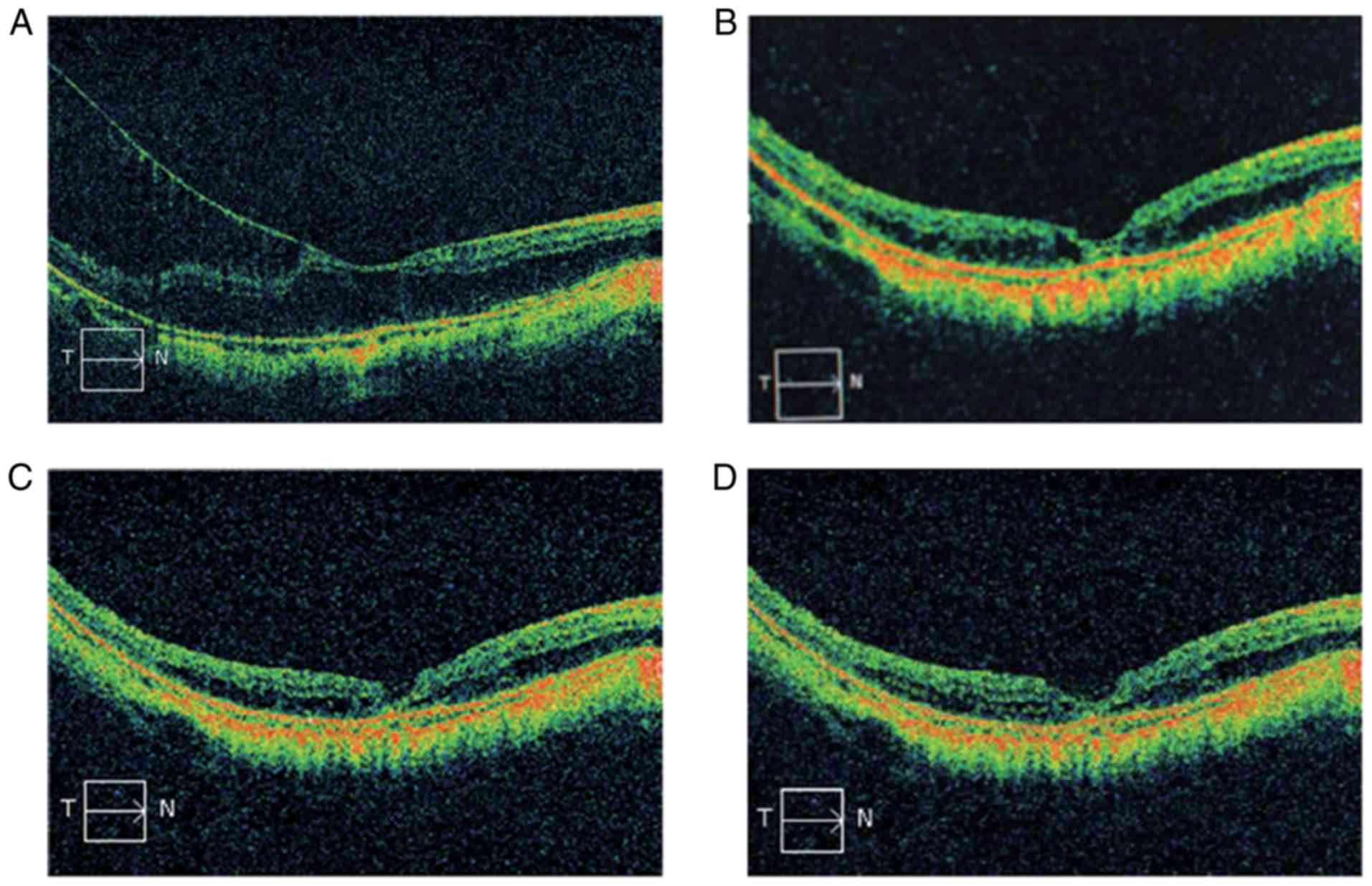
group. The overall difference was not significant (P=0.922). CMT
decreased to 269.3±67.7 µm in the peeling group and 294.4±60.5 µm
in the non-peeling group; this result was significantly different
between the groups, with a greater improvement in the peeling group
(P=0.015). In the peeling group, the foveoschisis on OCT completely
resolved in all 30 eyes within 6 months, and this was only achieved
in 26 eyes in the non-peeling group (Fig. 2). Significant differences were
identified in the rate of CMT changes between the peeling group and
the non-peeling group (P=0.038; Table
II). Significant differences were also identified between the
groups in the Amsler test, which was positive in five eyes in the
peeling group and 13 eyes in the non-peeling group (P=0.024;
Table II).
 | Table II.Postoperative outcomes and
complications. |
Table II.
Postoperative outcomes and
complications.
|
| Peeling group | Non-peeling
group | P-value | Statistics |
|---|
| Postoperative BCVA
in logMAR, mean ± SD | 0.75±0.26 | 0.72±0.25 | 0.863 | Wilcoxon
signed-rank test |
| BCVA changes,
n |
|
| 0.922 | χ2 test |
|
Improved | 24 | 25 |
|
|
|
Unchanged | 4 | 3 |
|
|
|
Worsened | 2 | 2 |
|
|
| Postoperative CMT,
mean ± SD | 269.3±67.7 | 294.4±60.5 | 0.015 | Mann-Whitney
test |
| CMT changes, n |
|
| 0.038 | Fisher's exact
t-test |
|
Completely resolved | 30 | 26 |
|
|
| Partly
resolved | 0 | 4 |
|
|
| Amslertest
positive, n | 5 | 13 | 0.024 | χ2 test |
| Complications |
|
|
| χ2 test |
|
Iatrogenic peripheral retinal
break | 1 | 2 | 0.554 |
|
| Macular
hole | 3 | 2 | 0.643 |
|
| Retinal
detachment | 1 | 1 | 1.0 |
|
| Wound suturation,
n | 2 | 3 | 1.0 | χ2 test |
| Gas tamponade
(C3F8), n | 30 | 30 | 1.0 | χ2 test |
Postoperative complications
The complications were similar between the two
groups (Table II). No serious
complications, such as the iatrogenic macular hole, occurred during
vitrectomy. Aniatrogenic peripheral retinal break developed in one
eye from the peeling group and two eyes from the non-peeling group
during vitrectomy, and the breaks were closed by intraoperative
photocoagulation. A full-thickness macular hole developed in three
eyes from the peeling group and two eyes from the non-peeling group
postoperatively. A 0.3 cc gas injection of 100% C3F8 was performed
in combination with the maintenance of facedown position for 1
week, and the macular holes of the two eyes in the peeling group
and two eyes in the non-peeling group were closed; however, the
macular hole of one eye in the peeling group was not closed, and
fluid-air exchange was performed followed by air-gas (10% C3F8)
exchange to finally close it. Retinal detachment developed in one
eye of the peeling group and one eye of the non-peeling group
post-vitrectomy due to a peripheral retinal break. The patients
underwent the treatment with silicone oil injection and removal
after 3 months; the retina reattached and the foveoschisis
completely resolved. Due to leakage at sclerotomy, the wound was
sutured in two eyes from the peeling group and three eyes from the
non-peeling group.
Discussion
The aim of the present study was to investigate
whether peeling the ILM during 23G vitrectomy was preferable to not
peeling the ILM for patients with MF. The results demonstrated that
BCVA improved in the peeling and non-peeling groups. CMT decreased
more significantly in the peeling group compared with the
non-peeling group. In the peeling group, MF completely resolved in
all eyes of the peeling group, and this was only observed in 87% of
eyes in the non-peeling group. In addition, the postoperative
Amsler test was positive in just five eyes in the peeling group
compared with 13 eyes in the non-peeling group, suggesting that any
metamorphopsia had been resolved (26). Peeling the ILM led to no greater risk
for patients, as complications were similar in the two groups.
Therefore, it may be suggested that peeling the ILM may provide
better outcomes compared with not peeling the ILM in 23-gauge
vitrectomy.
Numerous surgical options for the treatment of
foveoschisis have been reported (27). A number of studies have suggested the
benefits of vitrectomy for the resolution of foveoschisis by
removing vitreoretinal traction (28,29).
However, the evidence supporting the need to peel the ILM is
inconsistent. Sayanagi et al (30) performed vitrectomy and ILM peeling
for persistent MF following primary surgery that did not include
ILM peeling. Favorable anatomical and visual outcomes were
achieved, indicating that ILM peeling may be crucial for the
treatment of MF (31). A number of
studies have reported that vitrectomy combined with ILM peeling
results in better anatomical and visual effect compared with
vitrectomy alone (14,15,19,20,32). On
the other hand, certain studies have demonstrated the effect of
vitrectomy without ILM peeling (21,23,33).
However, the majority of studies that have investigated ILM peeling
are either case series or case reports (34), with very few studies comparing the
two methods (35). The results of
the present study suggested that ILM peeling may be the preferable
method, and this result is consistent with the study which compared
vitrectomy with and without ILM peeling by Taniuchi et al
(24), which additionally
demonstrated that tractional macular detachment developed more
frequently in eyes without ILM peeling. To the best of our
knowledge, the current study was the first to demonstrate improved
rates of metamorphopsia resolution following ILM peeling, which is
a major benefit in terms of the visual outcome. Although ILM
peeling may be a risk factor for iatrogenic macular hole in high
myopia (36), it ensures complete
removal of all macular vitreous traction and reduces retinal
stiffness to better match the posterior staphyloma (27). The thin and semitransparent ILM makes
surgical visualization challenging in patients with ILM peeling.
ILM peeling results in iatrogenic retinal injury involves macular
hole irregularities of the nerve fiber layers and retinal
microbleeds (37).
Chromovitrectomy has been developed as a way to
improve the visibility of the ILM, in order to shorten the surgery
duration and reduce iatrogenic retinal trauma (38). A variety of dyes, including trypan
blue, indocyanine green (ICG) and BB, are used to dye the ILM
(39). Though ICG was first used to
peel the ILM in macular surgery, potential side effects have been
reported (40). In the present
study, BB, a relatively new type of dye, was used to dye the ILM.
It selectively stains the ILM and has no toxicity (41–43).
Furthermore, to avoid damage to the retina, the point area without
inner retinoschisis was selected according to the 3D analysis with
a 3D visualization software following OCT.
The present study has certain limitations. The
sample size was quite small, and the patients were not randomized
into groups due to the retrospective nature of the study.
Therefore, there may have been certain bias in the patient
selection. A larger study would be able to provide further evidence
for these results and would allow the data to be analyzed according
to different patient characteristics to evaluate whether different
methods should be used in different patients. Vitrectomy combined
with ILM peeling may solve the issue of vertical and tangent
traction, although it cannot prevent the progress of posterior
staphyloma, which remains an important factor in MF (27). Recently, a number of studies have
shown that posterior scleral reinforcement surgery in the treatment
of MF is effective; it may stabilize the eye axis and improve
visual acuity (44,45). Future studies may further investigate
the therapeutic effect of vitrectomy combined with posterior
scleral reinforcement on MF.
The current retrospective cohort study identified
that 23G vitrectomy with BB-assisted ILM peeling resulted in more
favorable visual and anatomical outcomes in patients with MF
compared with not peeling the ILM.
Acknowledgements
The authors would like to thank the staff involved
in the trial for their efforts in collecting and ensuring the
accuracy and completeness of all data.
Funding
The present study was supported by The Science and
Technology Program of Jiangxi Provincial Health and Family Planning
Commission of China (grant no. 20171073).
Availability of data and materials
All datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XM participated in the literature search, study
design, surgery, data collection, data analysis and data
interpretation, and wrote the manuscript. YC performed the data
collection and analysis, and provided critical revisions. ZY
conceived the study and participated in its design and
coordination, and provided critical revisions. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of The Second Affiliated Hospital of Nanchang University
[approval no. (2012)095].
Patient consent for publication
All patients provided written consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Phillips CI: Retinal detachment at the
posterior pole. Br J Ophthalmol. 42:749–753. 1958. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lim SJ, Kwon YH, Kim SH, You YS and Kwon
OW: Vitrectomy and internal limiting membrane peeling without gas
tamponade for myopic foveoschisis. Graefes Arch Clin Exp
Ophthalmol. 250:1573–1577. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ellabban AA, Tsujikawa A, Matsumoto A,
Yamashiro K, Oishi A, Ooto S, Nakata I, Akagi-Kurashige Y, Miyake
M, Elnahas HS, et al: Three-dimensional tomographic features of
dome-shaped macula by swept-source optical coherence tomography. Am
J Ophthalmol. 155:320–328.e2. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zheng B, Chen Y, Chen Y, Zhao Z, Zhang Z,
Zheng J, You Y, Wang Q and Shen L: Vitrectomy and internal limiting
membrane peeling with perfluoropropane tamponade or balanced saline
solution for myopic foveoschisis. Retina. 31:692–701. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wong TY, Ohno-Matsui K, Leveziel N, Holz
FG, Lai TY, Yu HG, Lanzetta P, Chen Y and Tufail A: Myopic
choroidal neovascularisation: Current concepts and update on
clinical management. Br J Ophthalmol. 99:289–296. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Todorich B, Scott IU, Flynn HW Jr and
Chang S: Macular retinoschisis associated with pathologic myopia.
Retina. 33:678–683. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Meng B, Zhao L, Yin Y, Li H, Wang X, Yang
X, You R, Wang J, Zhang Y, Wang H, et al: Internal limiting
membrane peeling and gas tamponade for myopic foveoschisis: A
systematic review and meta-analysis. BMC Ophthalmol. 17:166–176.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Faghihi H, Hajizadeh F and Riazi-Esfahani
M: Optical coherence tomographic findings in highly myopic eyes. J
Ophthalmic Vis Res. 5:110–121. 2010.PubMed/NCBI
|
|
9
|
García-Ben A, Blanco MJ, Piñeiro A, Mera
P, Rodriguez-Alvarez MX and Capeans C: Relationship between macular
bending and foveoschisis in myopic patients. Optom Vis Sci.
91:497–506. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mateo C, Gómez-Resa MV, Burés-Jelstrup A
and Alkabes M: Surgical outcomes of macular buckling techniques for
macular retinoschisis in highly myopic eyes. Saudi J Ophthalmol.
27:235–239. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
García-Layana A, García-Arumí J,
Ruiz-Moreno JM, Arias-Barquet L, Cabrera-López F and Figueroa MS: A
review of current management of vitreomacular traction and macular
hole. J Ophthalmol. 2015:8096402015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gómez-Resa M, Burés-Jelstrup A and Mateo
C: Myopic traction maculopathy. Dev Ophthalmol. 54:204–212. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang T, Zhu Y, Jiang CH and Xu GZ:
Long-term follow-up of vitrectomy in patients with pathologic
myopic foveoschisis. Int J Ophthalmol. 10:277–284. 2017.PubMed/NCBI
|
|
14
|
Kumagai K, Furukawa M, Ogino N and Larson
E: Factors correlated with postoperative visual acuity after
vitrectomy and internal limiting membrane peeling for myopic
foveoschisis. Retina. 30:874–880. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Figueroa MS, Ruiz-Moreno JM, Gonzalez del
Valle F, Govetto A, de la Vega C, Plascencia RN, Contreras I and
Medina JL: Long-term outcomes of 23-gauge pars plana vitrectomy
with internal limiting membrane peeling and gas tamponade for
myopic traction maculopathy: A prospective study. Retina.
35:1836–1843. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Arevalo JF, Berrocal MH, Arias JD and
Banaee T: Minimally invasive vitreoretinal surgery: Is sutureless
vitrectomy the future of vitreoretinal surgery? J Ophthalmic Vis
Res. 6:136–144. 2011.PubMed/NCBI
|
|
17
|
Fujii GY, De Juan E Jr, Humayun MS, Chang
TS, Pieramici DJ, Barnes A and Kent D: Initial experience using the
transconjunctival sutureless vitrectomy system for vitreoretinal
surgery. Ophthalmology. 109:1814–1820. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ohta K, Sato A, Senda N and Fukui E:
Comparisons of foveal thickness and slope after macular hole
surgery with and without internal limiting membrane peeling. Clin
Ophthalmol. 12:503–510. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
VanderBeek BL and Johnson MW: The
diversity of traction mechanisms in myopic traction maculopathy. Am
J Ophthalmol. 153:93–102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hwang JU, Joe SG, Lee JY, Kim JG and Yoon
YH: Microincision vitrectomy surgery for myopic foveoschisis. Br J
Ophthalmol. 97:879–884. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ho TC, Yang CM, Huang JS, Yang CH, Yeh PT,
Chen TC, Ho A and Chen MS: Long-term outcome of foveolar internal
limiting membrane nonpeeling for myopic traction maculopathy.
Retina. 34:1833–1840. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shimada N, Sugamoto Y, Ogawa M, Takase H
and Ohno-Matsui K: Fovea-sparing internal limiting membrane peeling
for myopic traction maculopathy. Am J Ophthalmol. 154:693–701.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Qi Y, Duan AL, Meng X and Wang N:
Vitrectomy without inner limiting membrane peeling for macular
retinoschisis in highly myopic eyes. Retina. 36:953–956. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Taniuchi S, Hirakata A, Itoh Y, Hirota K
and Inoue M: Vitrectomy with or without internal limiting membrane
peeling for each stage of myopic traction maculopathy. Retina.
33:2018–2025. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Faes L, Bodmer NS, Bachmann LM, Thiel MA
and Schmid MK: Diagnostic accuracy of the Amsler grid and the
preferential hyperacuity perimetry in the screening of patients
with age-related macular degeneration: Systematic review and
meta-analysis. Eye (Lond). 28:788–796. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tranos P, Koukoula S, Charteris DG,
Perganda G, Vakalis A, Asteriadis S, Georgalas I and Petrou P: The
role of internal limiting membrane peeling in epiretinal membrane
surgery: A randomised controlled trial. Br J Ophthalmol.
101:719–724. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Alkabes M and Mateo C: Macular buckle
technique in myopic traction maculopathy: A 16-year review of the
literature and a comparison with vitreous surgery. Graefes Arch
Clin Exp Ophthalmol. May. 256:863–877. 2018.
|
|
28
|
Ikuno Y, Sayanagi K, Soga K, Oshima Y,
Ohji M and Tano Y: Foveal anatomical status and surgical results in
vitrectomy for myopic foveoschisis. Jpn J Ophthalmol. 52:269–276.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Elwan MM, Abd Elghafar AE, Hagras SM, Abou
Samra WA and Saleh SM: Long-term outcome of internal limiting
membrane peeling with and without foveal sparing in myopic
foveoschisis. Eur J Ophthalmol. 29:69–74. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sayanagi K, Ikuno Y and Tano Y:
Reoperation for persistent myopic foveoschisis after primary
vitrectomy. Am J Ophthalmol. 141:414–417. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Seppey C and Wolfensberger TJ: Vitrectomy
with fovea-sparing internal limiting membrane peeling for myopic
foveoschisis. Klin Monbl Augenheilkd. 234:497–500. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mii M, Matsuoka M, Matsuyama K, Otsu Y and
Nishimura T: Favorable anatomic and visual outcomes with 25-gauge
vitrectomy for myopic foveoschisis. Clin Ophthalmol. 8:1837–1844.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Spaide RF and Fisher Y: Removal of
adherent cortical vitreous plaques without removing the internal
limiting membrane in the repair of macular detachments in highly
myopic eyes. Retina. 25:290–295. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ikuno Y, Sayanagi K, Ohji M, Kamei M, Gomi
F, Harino S, Fujikado T and Tano Y: Vitrectomy and internal
limiting membrane peeling for myopic foveoschisis. Am J Ophthalmol.
137:719–724. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Liu HJ and Bi XJ: Vitrectomy combined with
internal limiting membrane peeling for treating foveoschisis in
high myopia. Int Eye Sci. 10:1871–1872. 2014.
|
|
36
|
Kwok AK, Lai TY and Yip WW: Vitrectomy and
gas tamponade without internal limiting membrane peeling for myopic
foveoschisis. Br J Ophthalmol. 89:1180–1183. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Sanisoglu H, Sevim MS, Aktas B, Sevim S
and Nohutcu A: Outcomes of 23-gauge pars plana vitrectomy and
internal limiting membrane peeling with brilliant blue in macular
hole. Clin Ophthalmol. 5:1177–1183. 2011.PubMed/NCBI
|
|
38
|
Shukla D, Kalliath J, Neelakantan N,
Naresh KB and Ramasamy K: A comparison of brilliant blue G, trypan
blue, and indocyanine green dyes to assist internal limiting
membrane peeling during macular hole surgery. Retina. 31:2021–2025.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Farah ME, Maia M, Penha FM and Rodrigues
EB: The use of vital dyes during vitreoretinal
surgery-chromovitrectomy. Dev Ophthalmol. 55:365–375. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yonekawa Y, Abbey AM, Shah AR, Thomas BJ
and Capone A Jr: Endoilluminator phototoxic maculopathy associated
with combined ICG-assisted epiretinal membrane and internal
limiting membrane peeling. Clin Ophthalmol. 8:2501–2506. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Badaró E, Moraes-Filho M, Maia M, Penha
FM, Novais EA, Souza-Lima RA, Hirai F, Meyer CH, Farah ME and
Rodrigues EB: Retinal biocompatibility of brilliant blue g with
deuterated water for chromovitrectomy. J Ophthalmic Vis Res.
9:204–209. 2014.PubMed/NCBI
|
|
42
|
Januschowski K, Mueller S, Spitzer MS,
Schramm C, Doycheva D, Bartz-Schmidt KU and Szurman P: Evaluating
retinal toxicity of a new heavy intraocular dye, using a model of
perfused and isolated retinal cultures of bovine and human origin.
Graefes Arch Clin Exp Ophthalmol. 250:1013–1022. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Enaida H, Hisatomi T, Hata Y, Ueno A, Goto
Y, Yamada T, Kubota T and Ishibashi T: Brilliant blue G selectively
stains the internal limiting membrane/brilliant blue G-assisted
membrane peeling. Retina. 26:631–636. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zhu SQ, Zheng LY, Pan AP, Yu AY, WangQ M
and Xue AQ: The efficacy and safety of posterior scleral
reinforcement using genipin cross-linked sclera for macular
detachment and retinoschisis in highly myopic eyes. Br J
Ophthalmol. 5:210–216. 2016.
|
|
45
|
Zhu Z, Ji X, Zhang J and Ke G: Posterior
scleral reinforcement in the treatment of macular retinoschisis in
highly myopic patients. Clin Exp Ophthalmol. 37:660–663. 2009.
View Article : Google Scholar : PubMed/NCBI
|