Introduction
Adult congenital megacolon (ACM), also known as
adult Hirschsprung's disease (1), is
relatively rare; only ~300 cases were reported in the literature
prior to 2016 (2). ACM frequently
presents with bowel obstruction as the initial symptom (3). Affected patients usually have a history
of constipation. Bowel obstruction in adults always occurs in
complex clinical situations and is frequently combined with
comorbidities, including bowel tumors, volvulus, hernias,
hypertension or diabetes mellitus. Thus, treatment poses a great
clinical challenge (4). Surgical
intervention is required, and to avoid recurrence, a sufficient
amount of bowel should be removed, particularly the aganglionic
segment (2). The present study
reports on a case of a 56-year-old patient with ACM, fecal
impaction and diabetic nephropathy.
Case report
A 56-year-old male patient with a history of chronic
constipation presented to the emergency department of Yinzhou
Peoples' Hospital (Ningbo, China) in February 2018. The patient had
experienced vague abdominal distention for several days. Prior to
admission, chronic bowel obstruction had been diagnosed at another
hospital. Auxiliary examination with a barium enema had indicated a
dilated bowel loop with a transition zone in the distal sigmoid
colon. The patient denied any similar conditions among his family
members. The patient's history of constipation started in childhood
and remained untreated, but his severe constipation had begun 6
years previously. Furthermore, the patient had a 10-year history of
diabetes mellitus and regularly took insulin; his fasting blood
glucose concentration was reasonably controlled at 8.0–9.0
mmol/l.
After admission to our department, the patient's
vital signs were normal. Physical examination revealed a soft
abdomen with slight distension and tympanic percussion sounds but
without local tenderness or rebound pain. The patient's bowel
sounds were hypoactive and an anal examination revealed no masses.
Laboratory data indicated elevated levels of creatinine, blood urea
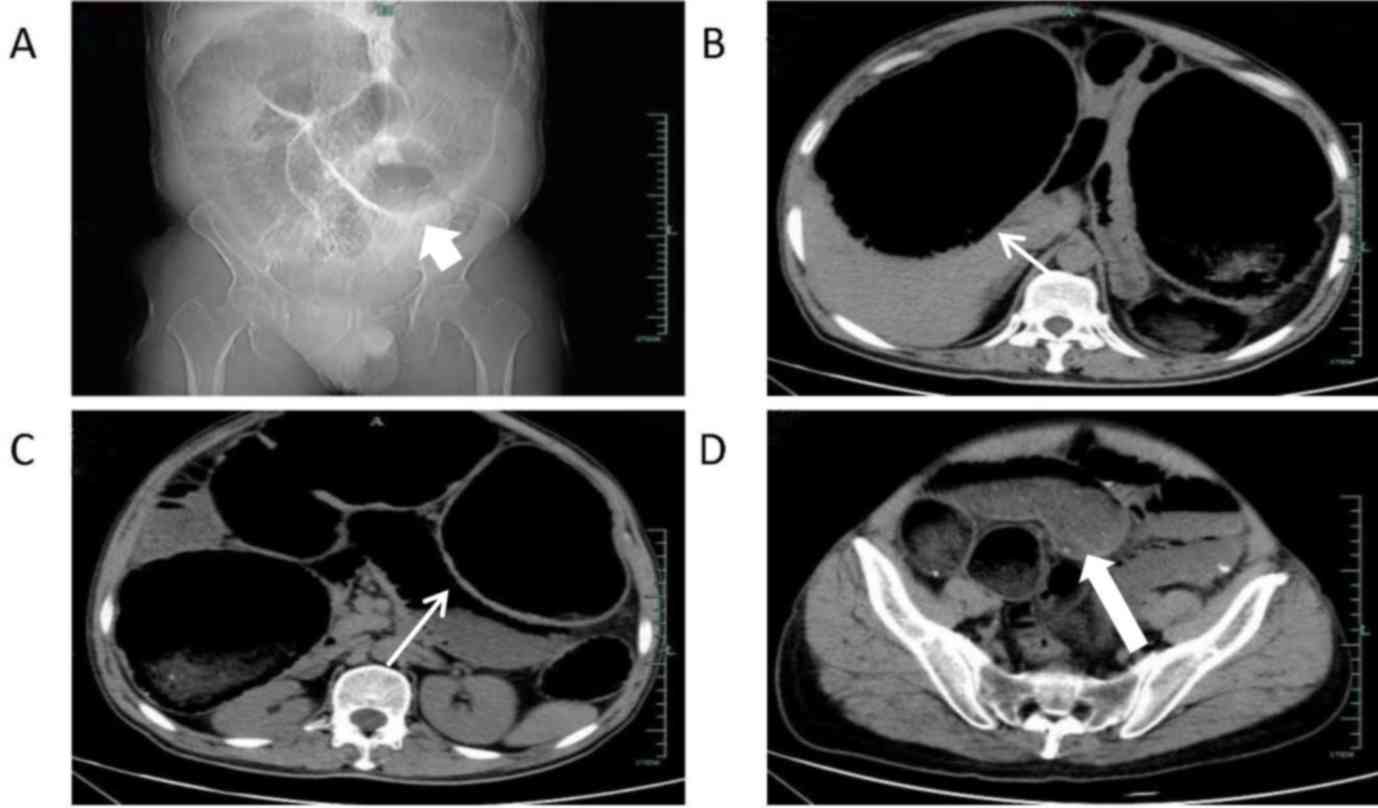
nitrogen, glucose and potassium. Abdominal computed tomography (CT)
revealed a dilated bowel with a typical ‘coffee bean sign’
(5). The dilated bowel extended from
the jejunum to the sigmoid colon and a transition zone was observed
in the distal sigmoid colon. The stomach was severely compressed in
the left upper quadrant. Large amounts of feces had accumulated
inside the colon (Fig. 1).
Initial treatment included gastrointestinal
decompression, fluid infusion and insulin to decrease the blood
glucose level, which subsequently became well controlled.
Laboratory tests indicated that the creatinine and blood urea
nitrogen levels decreased several days later and the hyperkalemia
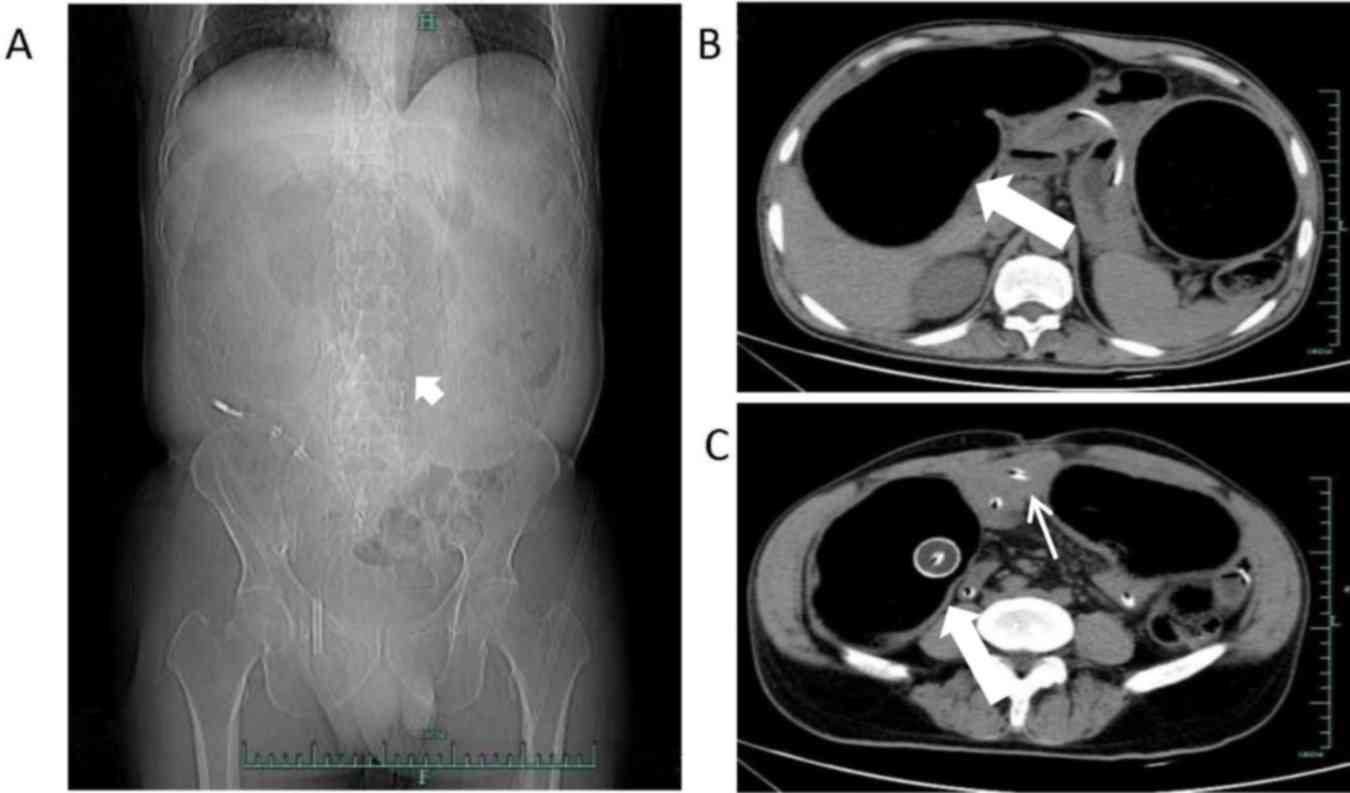
resolved. The patient's bowel movements also returned. Abdominal CT
suggested that the dilated small bowel had decreased in size at 1
week after admission (Fig. 2).
However, the patient's abdomen remained distended without
improvement.
At 10 days after admission, the patient's abdominal
condition suddenly worsened. Severe distention with rebound
tenderness was noted and emergency laparotomy was required. During
the operation, a severely dilated bowel was encountered, extending
from the ascending colon to the sigmoid colon. The most dilated
bowel segment was >15 cm in diameter (Fig. 3). Numerous hard fecaliths were
observed in the descending colon and sigmoid colon, and the colonic
lumen was obstructed. No perforation or tumor mass was palpable in
the gastrointestinal tract. The portion of colon from the ileocecal
junction to the terminal sigmoid colon was removed in a terminal
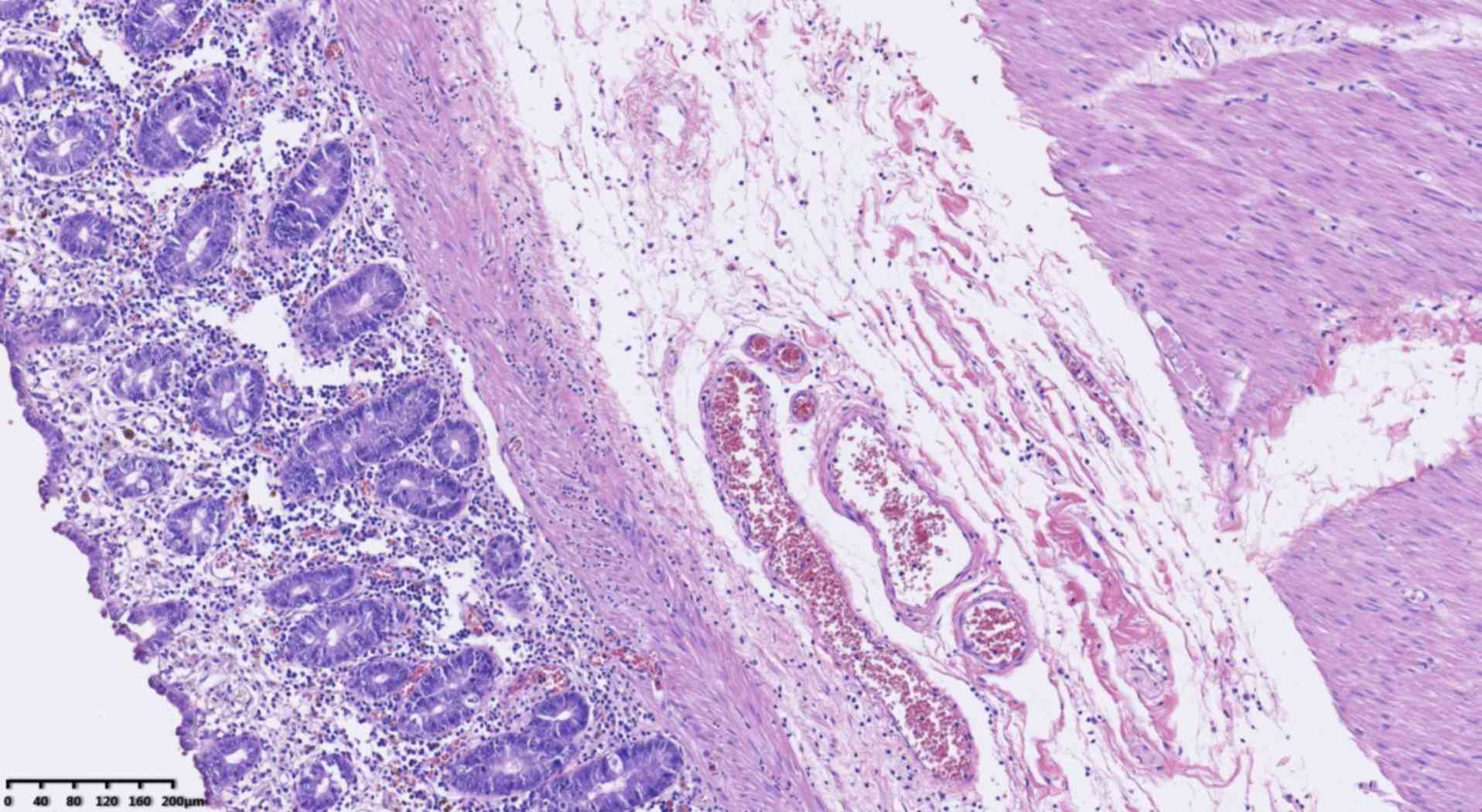
ileostomy. Post-operative pathologic examination revealed the
absence of ganglion cells in the submucosa and myenteric plexux of
the bowel and confirmed the previous diagnosis (Fig. 4). After the operation, the patient
received persistent gastrointestinal decompression, fluid infusion
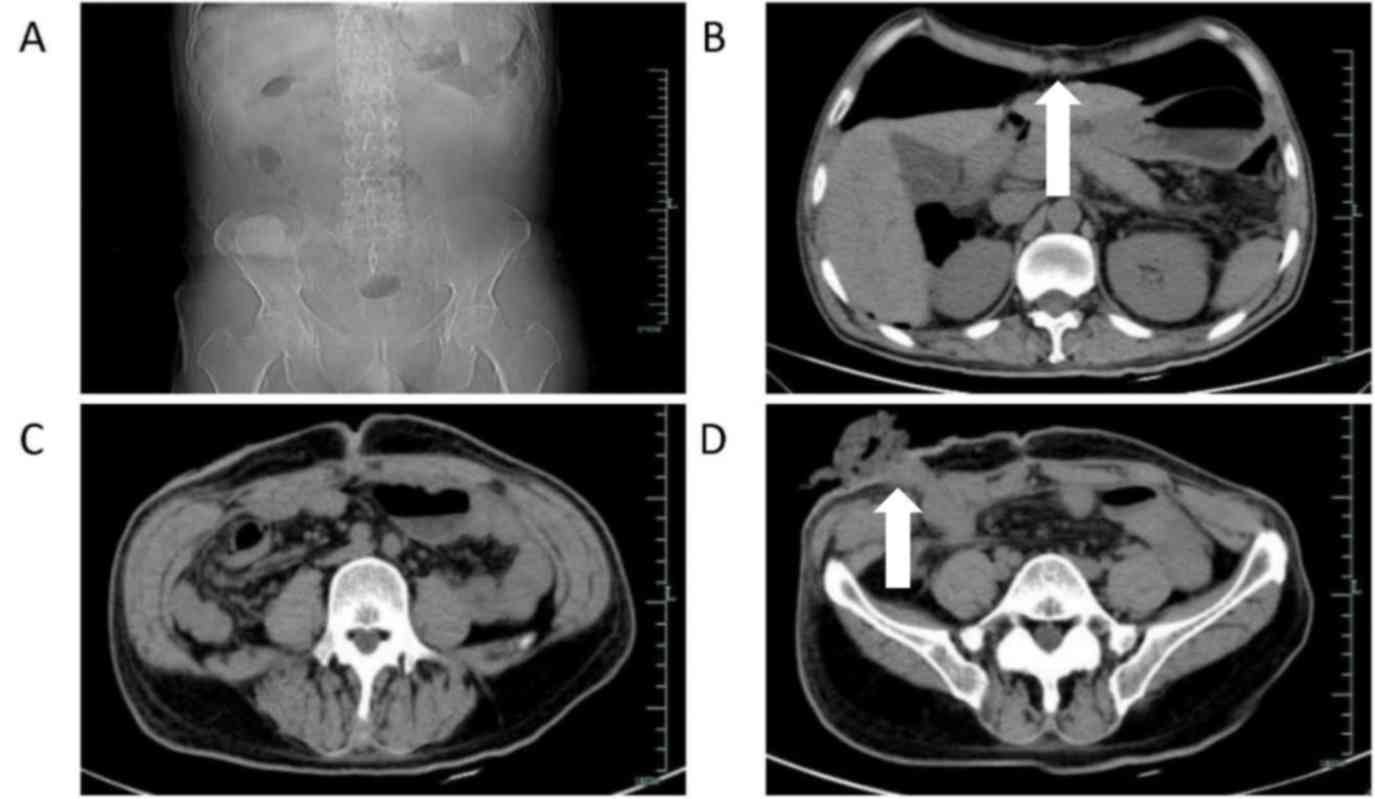
and blood glucose control. Abdominal CT re-examination indicated
good recovery (Fig. 5).
Post-operative blood tests indicated normal creatinine, blood urea
nitrogen and glucose levels. No post-operative complications
occurred, the patient was discharged in good physical condition and
took follow-ups every 3 months (ongoing), without any
disorders.
Discussion
ACM is a rare condition (6). Rosin et al (7) first reported ACM in 1950. Studies have
indicated that affected patients are >10 years old at the time
of diagnosis (2), the incidence of
ACM is 1/2,000 to 1/5,000 in live births, and the sex ratio
(male:female) is 3:1 to 4:1 (8,9). In
China, ACM is defined as occurring in patients aged >14 years
(10) with a colonic condition
caused by the absence of ganglion cells in the submucosa or
myenteric plexus of the bowel. Chronic constipation or abdominal
distension begins to appear at a young age in most patients, but
most patients do not undergo treatment, as symptoms are mild. The
condition frequently aggravates as the patient ages (11). Bowel obstruction is always the
primary symptom at that time. ACM may be misdiagnosed as idiopathic
megacolon, Chagas disease, inflammatory bowel disease, bowel
volvulus or colorectal tumor.
In China, ACM has been divided into the following
six phenotypes according to the affected bowel region: i) Common
type: The total rectum and sigmoid colon are affected. ii)
Super-short-segment type: Only the terminal rectum is affected.
iii) Short-segment type: The terminal rectum to the rectal ampulla
is affected. iv) Long-segment type: The rectum to the descending
colon and even the transverse colon is affected. v) Total colon
type: The rectum, total colon and the last 10 cm of the terminal
ileum are affected. vi) Total bowel type: Further intestinal
segments may be affected on the basis of the total colon type. Li
and Chen (12) reported on 36 cases
of ACM: 23 were of the common type, 7 of the short-segment type, 3
of the super-short-segment type, 1 was of the total colon type and
2 could not be classified. The patient in the present case had
total colon-type ACM.
The diagnosis of ACM should be made in considering a
history of illness, symptoms, laboratory examination and
histopathological examination. This is important, as patients with
idiopathic megacolon may also be constipated and have a dilated
colon, whereas patients with Chagas disease may also develop an
absence of ganglion cells in the submucosal and myenteric layers.
Other diseases, including colorectal cancer and bowel volvulus,
always manifest as bowel obstruction. According to López Ruiz et
al (2), the diagnosis of ACM
should be made using barium enema, anorectal manometry and rectal
biopsy. Qi and Zhang (9) indicated
that a barium enema is one of the most important techniques for
diagnosing megacolon, with an accuracy of ~90%. The most important
finding on barium enema is the existence of a transition zone
between the proximal dilated bowel and distal aganglionic bowel
(normal or narrow). A pre-operatively determined radiological
transition zone has potential value for identification of the
length of resected bowel in patients with ACM, as well as high
predictive value for the diagnosis of ACM (13). The level of the radiological
transition zone is a useful predictor of actual disease involvement
in older patients and infants (13).
The absence of a transition zone does not exclude the diagnosis of
ACM. The case of the present study did not receive a barium enema,
as he had already received one at another hospital prior to
admission, but also because of his severely dilated bowel loop,
which had a high risk of perforation. Anorectal manometry in
another hospital prior to admission to Yinzhou Peoples' Hospital
indicated a lack of relaxation of the internal anal sphincter in
response to rectal distension. In addition, the diagnosis of ACM
should be confirmed with a rectal biopsy of a narrow segment (93%
sensitivity and 100% specificity) (14). In the present case, the patient had a
lifelong history of constipation and barium enema at another
hospital revealed a dilated bowel loop; rectal biopsy was performed
to attain a definitive diagnosis. CT is also useful, as it may
reveal the transition zone and may be used to exclude certain other
diseases with similar symptoms, including colorectal tumors,
volvulus, bowel adhesion, idiopathic megacolon and toxic megacolon.
Although abdominal CT may assist in the diagnosis, pathologic
examination is the gold standard for obtaining a definitive
diagnosis (9). In the present case,
the patient finally underwent surgery and the diagnosis of ACM was
confirmed with the help of pathologic examination, which revealed
the absence of ganglion cells in the submucosal and myenteric
layers of the colon.
ACM is a special type of neuronal intestinal
malformation that not only manifests as ganglion cell deficiency
but also as various abnormalities, including hypoganglionosis,
immaturity of ganglion cells and non-classifiable dysganglionosis
(15). However, the pathogenesis of
ACM remains to be fully elucidated. ACM is likely caused by the
absence of ganglion cells in the affected segment of bowel,
particularly in the distal segment. This is the result of a lack of
migration of neuroblasts from the neural crest to the large
intestine during the embryonic period. The neural crest is a unique
structure that may differentiate into numerous tissue types
including ganglion cells. On completion of migration, neural crest
cells differentiate into diverse cell types, including neurons and
glia of the sensory, sympathetic and parasympathetic ganglia, and
neuroendocrine cells. Diseases arising from the neural crest are
particularly diverse in their clinical presentations and include
digestive, endocrinologic, neurological and cutaneous symptoms. To
contribute to enteric nervous system development, neural crest
cells must leave the neural tube, migrate to and enter the gut, and
then begin their migration along the hindgut. These events are
regulated by molecular and cellular mechanisms that are not
completely understood. Other proposed mechanisms include defects in
neuroblast differentiation and accelerated destruction of ganglion
cells in the intestine (16).
Mechanisms including RET gene mutation (17,18) have
been widely accepted. The RET proto-oncogene is the major gene
causing this type of disease; however, RET mutations only account
for 20 and 50% of sporadic and familial cases, respectively
(19). Different human and animal
genetic studies have identified six associated genes: The RET
proto-oncogene, the genes encoding SOX10, endothelin-converting
enzyme, endothelin B receptor gene, endothelin 3 and glial cell
line-derived neurotrophic factor. Microenvironmental factors also
have a role in the pathogenesis of aganglionosis (19). In the present case, it was suggested
to the patient to undergo RET gene detection analysis; however, he
declined due to limited economic resources.
Surgical intervention is always a necessary part of
treatment. López Ruiz et al (2) reported that the surgical approach
depends on the length of the aganglionic area, the length and
reversibility of the colonic dilatation and the nutritional status
of the patient. Usually, a longer duration of the obstruction is
associated with more complications. This is due to a large amount
of stool accumulating in the bowel cavity, leading to bowel
dilation and thereby increasing the risk of bowel necrosis,
perforation, abdominal infection and volvulus. Therefore, surgical
decompression must be performed. Sufficient decompression may
decrease post-operative complications. A shorter duration of bowel
obstruction is associated with a lower probability of bacterial
translocation. In the present case, the patient underwent
gastrointestinal decompression upon admission, and surgery was then
performed. The patient also had a 10-year history of diabetes
mellitus. Upon admission to our department, the patient's blood
glucose, creatinine, blood urea nitrogen and potassium levels were
elevated; therefore, an endocrinology consultation was immediately
performed to guide treatment. No post-operative complications
occurred. Selection of the surgical method should depend on the
patient's actual condition and the surgeon's skills. The length of
the resected bowel is not only determined using radiological tests
but also by pathologic examination. In the present case, the
patient had a long history of illness, and the dilated bowel
extended from the ileocecal junction to the sigmoid colon; this is
why the patient underwent total colectomy with end ileostomy, as
pathologic examination indicated a normal incisal margin. With
advancements in surgical skills and equipment, novel treatment
methods, including transanal surgery and laparoscopic
megacolonectomy, are being increasingly accepted by surgeons
(20). Transanal surgery has the
advantage of minimal invasion (21),
whereas laparoscopic megacolonectomy changes a traditional
operation into laparoscopy, thereby greatly decreasing operative
injury, and it is suited for any type of megacolon. This method has
therefore become popular for the surgical treatment of ACM
(22).
In summary, ACM is a rare but fatal alimentary tract
malformation with a complex etiopathogenesis and presentation, and
associated complications are usually present. Surgeons should make
an accurate diagnosis based on the history of illness, symptoms,
laboratory test results and radiologic findings. Surgical
intervention is always needed, and prior to surgery, the patient's
general condition (blood pressure, blood glucose and other
parameters) should be regulated to decrease the risk of
post-operative complications. A sufficient amount of bowel should
be removed, including the aganglionic segment. The length of the
resected bowel should be determined using not only radiologic tests
but also frozen-section pathologic examination. Emergency total
colectomy with end ileostomy is the gold standard procedure
(23). Patients with ACM require
particular attention, and timely diagnosis and individualized
treatment may accelerate the recovery process.
Acknowledgements
The authors thank Dr Angela Morben for editing the
English draft of this manuscript.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
KD conceived the case report. MZ treated the
patient, made substantial contributions to the acquisition of data,
and was involved in drafting the manuscript and revising it
critically.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
publication.
Competing interests
The authors declare that they have no competing
interets.
References
|
1
|
Fortea-Sanchís C, Martínez-Ramos D,
Rivadulla-Serrano I, Daroca-José JM, Paiva-Coronel G and
Salvador-Sanchís JL: Hirschprung's disease in adults. Rev Esp
Enferm Dig. 103:150–151. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
López Ruiz JA, Tallón Aguilar L, Sánchez
Moreno L, López Pérez J, Pareja Ciuró F, Oliva Mompeán F and
Padillo Ruiz FJ: Hirschsprung disease with debut in adult age as
acute intestinal obstruction: Case report. Rev Esp Enferm Dig.
108:742–746. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lou Z, Meng RG, Yu ED, Liu LJ, Hao LQ,
Wang HT and Fu CG: Diagnosis and surgical treatment of adult
Hirschsprung's disease. Zhonghua Wei Chang Wai Ke Za Zhi.
8:304–305. 2005.(In Chinese). PubMed/NCBI
|
|
4
|
Doodnath R and Puri P: A systematic review
and meta-analysis of Hirschsprung's disease presenting after
childhood. Pediatr Surg Int. 26:1107–1110. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wu S, Sun X, Yu Y and Shen Y:
Hirschsprung's disease-related sigmoid vulvulus complicated with
refractory hypertension. Am J Case Rep. 19:467–471. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shitta AH, Ugwu BT, Peter SD, Ozoilo KN,
Adighije PF and Omolabake BI: Hirschsprung's disease in an adult: A
case report. J West Afr Coll Surg. 4:121–126. 2014.PubMed/NCBI
|
|
7
|
Rosin JD, Bargen JA and Waugh JM:
Congenital megacolon of a man 54 years of age: Report of case. Proc
Staff Meet Mayo Clin. 25:710–715. 1950.PubMed/NCBI
|
|
8
|
Qiu JF, Shi YJ, Hu L, Fang L, Wang HF and
Zhang MC: Adult Hirschsprung's disease: Report of four cases. Int J
Clin Exp Pathol. 6:1624–1630. 2013.PubMed/NCBI
|
|
9
|
Qi Z and Zhang W: Adult congenital
megacolon with bowel obstruction: A case report. Chin J
Gastroenterol Hepatolt. 26:1131–1132. 2017.(In Chinese).
|
|
10
|
Ding SQ, Chen YT, Ding YJ, Fang L, Wang HF
and Zhang MC: Diagnosis and surgical management of adult
Hirschsprung disease. Zhonghua Wei Chang Wai Ke Za Zhi. 9:53–55.
2006.(In Chinese). PubMed/NCBI
|
|
11
|
Kim HJ, Kim AY, Lee CW, Yu CS, Kim JS, Kim
PN, Lee MG and Ha HK: Hirschsprung disease and hypoganglionosis in
adults: Radiologic findings and differentiation. Radiology.
247:428–434. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Li F and Chen Y: Diagnosis and surgical
treatment of adult Hirschsprung's disease. Chin J Gen Surg.
9:452–454. 2000.(In Chinese).
|
|
13
|
Chen X, Xiaojuan W, Zhang H, Jiao C, Yu K,
Zhu T and Feng J: Diagnostic value of the preoperatively detected
radiological transition zone in Hirschsprung's disease. Pediatr
Surg Int. 33:581–586. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Arshad A, Powell C and Tighe MP:
Hirschsprung's disease. BMJ. 345:e55212012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Holschneiderd AM, Meier-Ruge W and Ure BM:
Hirschsprung's disease and allied disorders-a review. Eur J Pediatr
Surg. 4:260–266. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fu CG, Muto T, Masaki T and Nagawa H:
Zonal adult Hirschsprung's disease. Gut. 39:765–767. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Edery P, Lyonnet S, Muligan LM, Pelet A,
Dow E, Abel L, Holder S, Nihoul-Fékété C, Ponder BA and Munnich A:
Mutations of the RET proto-oncogene in Hirschsprung disease.
Nature. 367:378–380. 1994. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Romeo G, Ronchetto P, Yin L, Barone V,
Seri M, Ceccherini I, Pasini B, Bocciardi R, Lerone M, Kääriäinen
H, et al: Point mutations affecting the tyrosine kinase domain of
the RET proto-oncogene in Hirschsprung's disease. Nature.
367:377–378. 1994. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Martuccielb G, Ceccherim I, Lerong M and
Jasonni V: Pathogenesis of Hirschsprung's disease. J Pediatr Surg.
55:1017–1025. 2000.
|
|
20
|
He X, Xu D and Li L: Congenital megacolon
with Laporoscopic-assisted treatment: 20 cases report. J
Laporoscopic surg. 14:55–56. 2009.
|
|
21
|
Wang G: The treatment progession and micro
invasive surgery of Congenital megacolon. Chin J Pediatr surg.
23:103–104. 2003.(In Chinese).
|
|
22
|
Jarry J and Faucheron JL: Laparoscopic
rectosigmoid resection with transanal colonic pull-through and
delayed coloanal anastomosis: A new approach to adult Hirschsprung
disease. Dis Colon Rectum. 54:1313–1319. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Miniello S, Marzaioli R, Balzanelli MG,
Dantona C, Lippolis AS, Barnabà D and Nacchiero M: Toxic megacolon
in ulcerative rectocolitis. Current trends in clinical evaluation,
diagnosis and treatment. Ann Ital Chir. 85:45–49. 2014.PubMed/NCBI
|