Introduction
As a disease of the chronic digestive system,
chronic diarrhea is commonly manifested as changes in bowel habits,
diarrhea and abdominal pain as well as abdominal distension in a
few cases. The pathogenesis of the disease is mostly the intestinal
flora imbalance and ectopia, endocrine dysfunction and mental
stress. Besides, excessive mental stress often causes
neuroendocrine dysfunction, with such manifestations as the
secretion disorders of corticotropin-releasing hormone and
adrenocorticotropic hormone (1),
which lead to mental mania or apathy, delusion and depression in
patients and induce the onset of depression in patients.
Increasingly more studies have revealed that
inflammatory cytokines also exert crucial effects in the onset
process of depression. Both in adequate and excessive secretions of
collective anti-inflammatory cytokines are the most important
mechanisms of chronic diarrhea. Excessively secreted inflammatory
cytokines can induce depression, thus resulting in a variety of
symptoms of depression such as sexual hypoactivity, reduced social
activity, slow action and sleep disorders (2), and studies have manifested that the
changes in the level of cytokines have a correlation with the
occurrence of depression in patients (3). The present study aimed to observe the
efficacy of electroacupuncture combined with probiotics in the
treatment of patients with depression and chronic diarrhea and its
influence on cytokines, and to investigate the correlations of
cytokines with the occurrence and prognosis of the disease.
Patients and methods
Study subjects
A total of 104 patients with depression and chronic
diarrhea admitted to The First Clinical Faculty, Guangxi University
of Traditional Chinese Medicine (Nanning, China) from July 2014 to
June 2018 were selected, and they were divided into the observation
group (n=56) and the control group (n=48). The diagnostic criteria
for depression were based on the 10th revision of the International
Statistical Classification of Diseases and Related Health Problems
(4) and the 3rd revision of the
Chinese Classification of Mental Disorders. There were no
statistically significant differences in age, sex, course of the
disease and complication with other underlying diseases between the
two groups of patients (p>0.05).
The present study was approved by the Ethics
Committee of The First Clinical Faculty, Guangxi University of
Traditional Chinese Medicine. The signed informed consents were
obtained from the patients or the guardians.
Treatment methods
Patients in the control group took orally
trimebutine maleate tablets (100 mg/time, 3 times/day) and
meptintin (100 mg/day, and the dose was adjusted according to the
patient's condition and side effects). Patients in the observation
group were treated with electroacupuncture and oral probiotics, 50
mm acupuncture needles were used to acupuncture such acupoints as
Baihui point, Sanyinjiao point and Yanglingquan point. After the
air was obtained, the electroacupuncture machine was connected for
electroacupuncture for 30 min each day. Additionally, the patients
took viable bifidobacterium quadruple tablets (1.5 g/time, 3
times/day) with warm water after meals. Blood was drawn from the
two groups of patients for scale evaluation before and after
treatment.
Scale assessment
The two groups of patients were scored by Hamilton
Depression Rating Scale (HAM-D) before and after treatment.
Criteria for chronic diarrhea: diarrhea ≥3 times/day, thin or
watery stool and no obvious pus and blood accompanied with
abdominal pain, abdominal distension and tenesmus and duration
>3 weeks (5).
Detection methods
The venous blood of patients was taken at admission
and at 3 weeks after treatment. After centrifugation at 6,000 × g,
for 10 min at 4°C, the supernatant was taken, and the changes in
the levels of serum inflammatory cytokines interleukins (ILs) and
the tumor necrosis factor (TNF)-α), norepinephrine (NE) and
brain-derived neurotrophic factor (BDNF) were detected by means of
radioimmunoassay. Fecal flora culture: Approximately 5 g sterile
feces of the patients were taken, diluted with normal saline,
shaken, homogenized, inoculated on the selective medium and
cultured in an incubator at 35°C for 24 h. Finally, the methylene
blue chemical indicator was added and the bacterial colony formed
was counted.
Statistical analysis
Statistical analysis was carried out via SPSS 17.0
(SPSS Inc., Chicago, IL, USA). Data were expressed as mean ± SD.
The Students' tests were used to for comparisons of HAM-D score,
intestinal flora, inflammatory cytokines, NE level, BDNF level,
treatment efficacy. P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparison of the HAM-D score between
the two groups of patients
At 3 weeks after treatment, the total HAM-D score of
the two groups of patients was significantly reduced, but no
statistical difference was found between them (p>0.05),
suggesting that both electroacupuncture and maprotiline markedly
improve the depression symptoms of the patients, and the overall
efficacy of them is identical. The univariate analysis demonstrated
that the improvement degrees of sleep disorders and cognitive
impairment in the observation group were evidently higher than
those in the control group (p<0.05) (Table I).
 | Table I.Comparison of the HAM-D score between
the two groups of patients (mean ± SD). |
Table I.
Comparison of the HAM-D score between
the two groups of patients (mean ± SD).
|
| Observation group
(n=56) | Control group
(n=48) |
|---|
|
|
|
|
|---|
| Items | Before treatment | After treatment | Before treatment | After treatment |
|---|
| Total score of
HAM-D | 32.34±5.43 | 15.57±3.79 | 29.34±6.09 | 14.34±4.65 |
| Weight | 2.47±1.08 | 0.89±0.47 | 1.97±2.16 | 1.03±0.66 |
| Sleep disorder | 5.42±2.13 | 1.45±1.34 | 5.86±3.18 |
2.95±2.13a |
|
Anxiety/somatization | 6.36±4.24 | 4.21±1.93 | 5.96±4.67 | 3.84±1.82 |
| Day and night
change | 1.72±0.86 | 0.85±0.47 | 1.57±0.67 | 0.99±0.83 |
| Retardant | 7.48±3.54 | 4.16±2.35 | 6.95±2.64 | 4.67±3.12 |
| Feeling of
despair | 5.36±2.37 | 3.58±1.83 | 4.97±1.86 | 3.74±2.11 |
| Cognitive
disorder | 6.84±3.83 | 3.68±2.85 | 7.46±2.93 |
5.17±2.04a |
Comparison of the intestinal flora
between the two groups of patients
Compared with the intestinal flora in normal
individuals, the enterobacteria were increased significantly, while
lactobacilli and enterococci were decreased (not
shown in results) in patients with chronic diarrhea. After the
treatment, the enterobacteria were reduced, while lactobacilli,
enterococci and other bacteria rose again in the both groups of
patients. Among them, the elevated level of lactobacilli in
the observation group was obviously higher than that in the control
group, with a statistically significant difference (p<0.05)
(Table II).
 | Table II.Comparison of the intestinal flora
between the two groups of patients (Ig CFU/g, mean ± SD). |
Table II.
Comparison of the intestinal flora
between the two groups of patients (Ig CFU/g, mean ± SD).
|
| Observation group
(n=56) | Control group
(n=48) |
|---|
|
|
|
|
|---|
| Intestinal flora | Before treatment | After treatment | Before treatment | After treatment |
|---|
| Enterobacterium | 13.94±2.83 | 7.54±2.36 | 14.25±3.04 | 8.13±3.62 |
|
Enterococcus | 10.68±2.37 | 7.31±3.17 | 11.53±3.64 | 9.64±3.58 |
| Bacteroides
fragilis | 10.78±6.35 | 10.39±3.22 | 11.23±7.26 |
11.02±3.15a |
|
Lactobacillus | 6.67±1.36 | 9.63±1.37 | 6.96±1.21 | 9.52±3.04 |
|
Bifidobacterium | 9.62±0.95 | 10.04±1.05 | 8.43±1.03 | 9.56±1.85 |
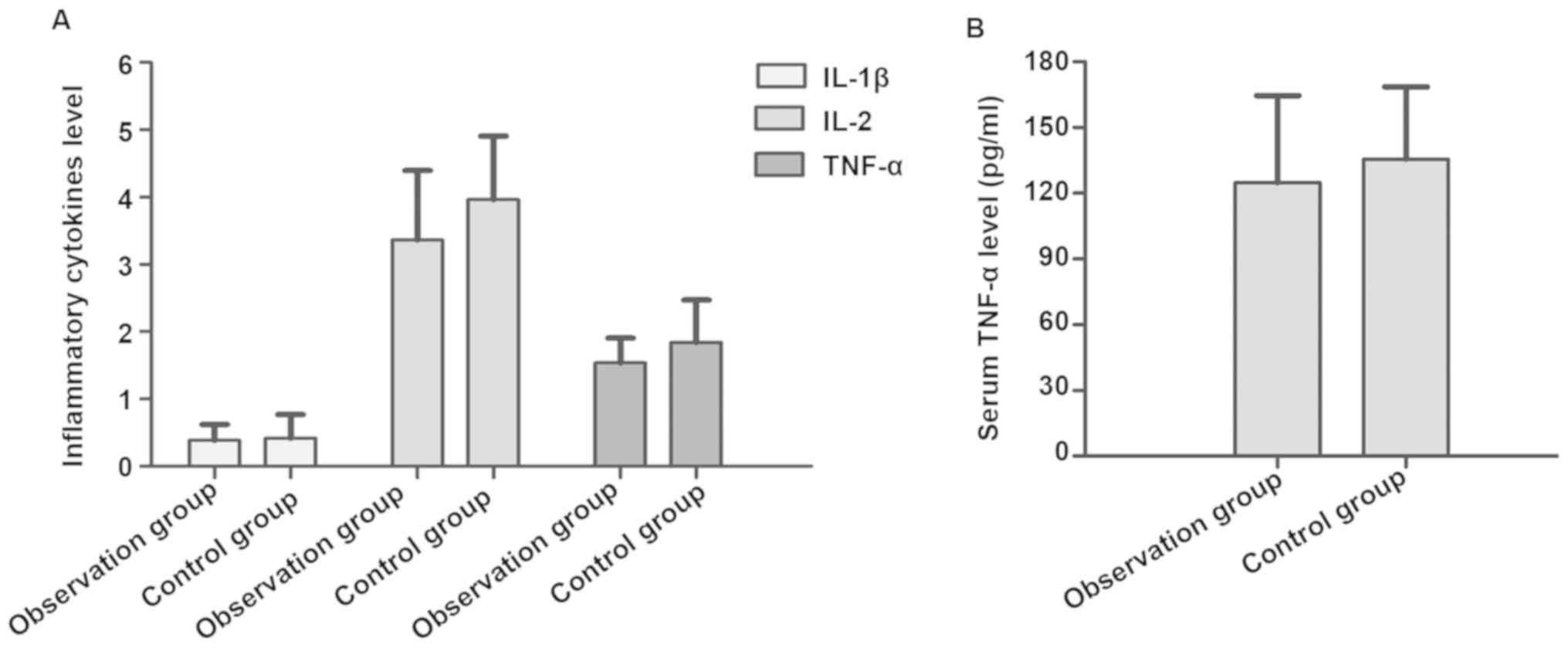
Effects of the cell inflammatory
cytokines between the two groups of patients
Compared with those in normal patients, the serum
inflammatory cytokines in the two groups before treatment were
obviously increased before treatment. The levels of ILs and TNF-α
in serum in the two groups of patients at 3 weeks after treatment
returned to normal. There was no significant difference in the
reduced level of inflammatory cytokines between the two groups
(p>0.05) (Fig. 1A and B).
Comparison of the NE level between the
two groups of patients
Compared with the normal value, before treatment,
the NE levels were significantly increased, while the
5-hydroxytryptamine (5-HT) levels were significantly decreased in
the two groups of patients. At 3 weeks after treatment, the NE
levels were decreased to normal, and the 5-HT levels also returned
to normal in the two groups of patients. Among them, the level of
5-HT in the observation group was higher than that in the control
group, showing a statistically significant difference (p<0.05),
but no significant difference in the NE level was found between the
two groups (p>0.05) (Table
III).
 | Table III.Comparison of the levels of NE and
5-HT before and after treatment between the two groups of
patients. |
Table III.
Comparison of the levels of NE and
5-HT before and after treatment between the two groups of
patients.
|
| Observation group
(n=56) | Control group
(n=48) |
|---|
|
|
|
|
|---|
| Items | Before treatment | After treatment | Before treatment | After treatment |
|---|
| NE (ng/ml) | 0.86±0.57 |
0.59±0.23a | 0.92±0.63 | 0.67±0.31 |
| 5-HT (ng/ml) | 79.58±43.54 |
154.38±59.62a | 82.43±39.84 | 138.56±61.37 |
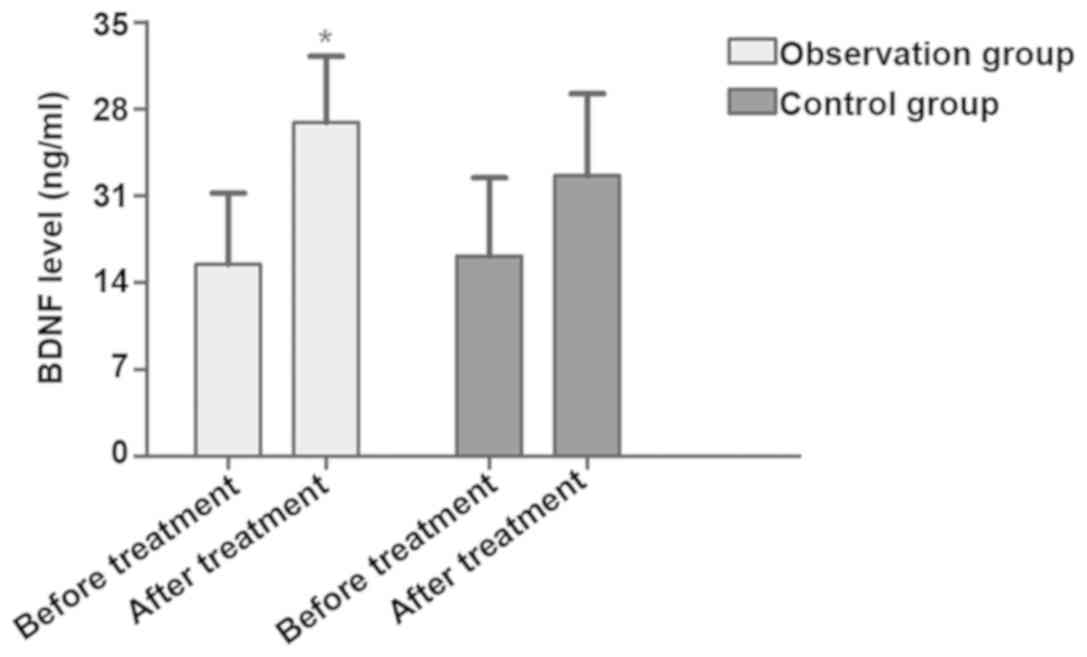
Changes in the BDNF level between the
two groups of patients
Before treatment, the levels of BDNF in the two
groups were significantly lower than the normal value. After
treatment, the levels of BDNF in the two groups were increased, and
the increased level of BDNF in the observation group was higher
than that in the control group (p<0.05) (Fig. 2).
Comparison of the efficacy on chronic
diarrhea between the two groups of patients
At 3 weeks after treatment, the total effective rate
of the observation group was higher than that of the control group,
and the difference was statistically significant (p<0.05)
(Table IV).
 | Table IV.Comparison of the efficacy of chronic
diarrhea between the two groups of patients [n (%)]. |
Table IV.
Comparison of the efficacy of chronic
diarrhea between the two groups of patients [n (%)].
| Groups | Markedly
effective | Effective | Ineffective | Total effective
rate |
|---|
| Observation
(n=56) | 32 | 21 | 3 | 94.64%a |
| Control (n=48) | 23 | 18 | 7 | 85.42% |
Discussion
The faster pace of modern society and the increased
mental stress of people has led to an increased number of mental
diseases, the most common of which is depression. Depression in
patients is usually manifested in the form of sleep disorders,
reduced or regressed social activities, reduced desires, weight
loss, hyperalgesia and autism (6).
Research results have shown that the occurrence of depression in
patients is associated with the excessive secretion of cytokines
(7). It has been confirmed that the
levels of IL-6, TNF-α and IL-1 are elevated in the acute phase of
depression in patients, and can reflect the severity of depression
and partial depression in patients (8). After patients are administered
antidepressant drugs, the levels of serum IL-6 and TNF-α markedly
decline to normal, indicating that cytokines exert certain effects
in the onset of depression (9). The
excessive secretion of inflammatory cytokines during the onset of
depression can lead to insufficient secretion of anti-inflammatory
cytokines in patients, thus causing an
anti-inflammatory/inflammatory imbalance. As a chemokine, IL-8
plays a vital role in the intestinal inflammation. Secreted by
intestinal epithelial cells and macrophages, IL-8 can regulate the
phagocytosis of neutrophils through activation and chemotaxis. The
excessive secretion of IL-8 can induce the systolic dysfunction of
smooth muscle of the intestinal nervous system and influence the
local intestinal neuroimmunoendocrine network system, thus
triggering the intestinal mucosal inflammation (10). In addition, the excessive secretion
of TNF-α stimulates intestinal mucosal epithelial cells, promotes
the proliferation of fibroblasts and causes the degradation of
intestinal mucosa epithelial function (11,12).
Other studies have manifested that IL-10 also exerts a vital effect
in the intestinal inflammation (13). The intestinal mucosal inflammation
affects the intestinal nervous system and causes abnormal smooth
muscle contraction and sensitivity in the patients, thus leading to
abdominal pain, abdominal distension and changes in bowel habits.
Patients with these symptoms for more than 2 weeks can be diagnosed
with chronic diarrhea.
Furthermore, the occurrence of depression also has
relationships to dysfunction of the central NE, 5-HT and BDNF
(14–16). Research results of Karege et
al (17) and Shimizu et
al (18) revealed that compared
with those in the normal population, the levels of BDNF and 5-HT in
patients with depression are decreased, while the expression level
of NE is higher than the normal value. After the drug treatment,
the levels of BDNF and 5-HT in serum of patients with improved
depression symptoms return to normal, but the level of NE level
declines, indicating that changes in the levels of BDNF, 5-HT and
NE may be associated with depression in patients (18,19). The
treatment for depression has achieved good results, but since drug
treatment brings a variety of side effects to patients, such as
xerostomia, constipation, palpitation and dizziness and the
patients need to take drugs for a long time, the medication
compliance is poor. Electroacupuncture treatment for depression was
implemented in the 20th century with good results (19,20).
This study investigated the efficacy of electroacupuncture combined
with probiotics for patients with depression and chronic diarrhea,
so as to provide a new idea for the improvement of the patients'
traditional treatment regimens.
The results of this study demonstrated that there
was no significant difference in the total HAM-D score between the
control group and the observation group, but the improvement
degrees of sleep disorders and cognitive impairment in the former
were better than that in the latter (p<0.05). After treatment,
the cytokine levels in the two groups of patients were markedly
decreased, and there was no statistical difference between the two
groups (p>0.05). The NE level in patients of the observation
group was not significantly different from that in patients of the
control group, but the change degrees of 5-HT and BDNF in the
observation group were higher than those in the control group
(p<0.05). Moreover, the change degree of intestinal flora
imbalance and the treatment effective rate in the observation group
were higher than those in the control group. The above results
indicate that electroacupuncture combined with probiotics is
superior to traditional drug therapy in the treatment of patients
with depression and chronic diarrhea, and this method is worthy of
further promotion in clinical practice.
Acknowledgements
Not applicable.
Funding
The present study was funded by Guangxi Talent
Highland for Zhuang and Yao Medicine and Combination of Medical
Care and Elderly Care [NoTingFa(2017)44]; funded by Development
Program of High-level Talent Team under Qihuang Project of Guangxi
University of Chinese Medicine (grant no. 2018005); funded by
Guangxi Scholarship Fund of Guangxi Education Department [No. Gui
Jiao Ren (2018)18].
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
WH wrote the manuscript. WH and WG worked on
treatment methods. AH and YF collected and analyzed general data of
patients. YS and YC helped with scale assessment. ZT and YZ
performed radioimmunoassay. WH and GF were responsible for
statistical analysis. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of The First Clinical Faculty, Guangxi University of
Traditional Chinese Medicine (Nanning, China). The signed informed
consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Haraguchi A, Fukuzawa M, Iwami S,
Nishimura Y, Motohashi H, Tahara Y and Shibata S: Night eating
model shows time-specific depression-like behavior in the forced
swimming test. Sci Rep. 8:10812018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Barua CC, Haloi P, Saikia B, Sulakhiya K,
Pathak DC, Tamuli S, Rizavi H and Ren X: Zanthoxylum alatum
abrogates lipopolysaccharide-induced depression-like behaviours in
mice by modulating neuroinflammation and monoamine
neurotransmitters in the hippocampus. Pharm Biol. 56:245–252. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Veltman EM, Lamers F, Comijs HC, Stek ML,
van der Mast RC and Rhebergen D: Inflammatory markers and cortisol
parameters across depressive subtypes in an older cohort. J Affect
Disord. 234:54–58. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Innes K, Hooper J, Bramley M and DahDah P:
Creation of aclinical classification. International statistical
classification of diseases and related health problems--10th
revision, Australian modification (ICD-10-AM). Health Inf Manag.
27:31–38. 1997.PubMed/NCBI
|
|
5
|
Liu S and Ren JA: Pathogenesis, diagnosis
and treatment of anemia in inflammatory bowel disease. Zhonghua Wei
Chang Wai Ke Za Zhi. 16:398–400. 2013.(In Chinese). PubMed/NCBI
|
|
6
|
Haack M, Hinze-Selch D, Fenzel T, Kraus T,
Kühn M, Schuld A and Pollmächer T: Plasma levels of cytokines and
soluble cytokine receptors in psychiatric patients upon hospital
admission: Effects of confounding factors and diagnosis. J
Psychiatr Res. 33:407–418. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Levine J, Barak Y, Chengappa KN, Rapoport
A, Rebey M and Barak V: Cerebrospinal cytokine levels in patients
with acute depression. Neuropsychobiology. 40:171–176. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Frommberger UH, Bauer J, Haselbauer P,
Fräulin A, Riemann D and Berger M: Interleukin-6-(IL-6) plasma
levels in depression and schizophrenia: Comparison between the
acute state and after remission. Eur Arch Psychiatry Clin Neurosci.
247:228–233. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Słuzewska A, Rybakowski JK, Laciak M,
Mackiewicz A, Sobieska M and Wiktorowicz K: Interleukin-6 serum
levels in depressed patients before and after treatment with
fluoxetine. Ann N Y Acad Sci. 762:474–476. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Talati M and Hemnes A: Fatty acid
metabolism in pulmonary arterial hypertension: Role in right
ventricular dysfunction and hypertrophy. Pulm Circ. 5:269–278.
2015. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Du Y, Yang M, Wei W, Huynh HD, Herz J,
Saghatelian A and Wan Y: Macrophage VLDL receptor promotes PAFAH
secretion in mother's milk and suppresses systemic inflammation in
nursing neonates. Nat Commun. 3:10082012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Luther J, Gala M, Patel SJ, Dave M, Borren
N, Xavier RJ and Ananthakrishnan AN: Loss of response to anti-tumor
necrosis factor alpha therapy in Crohn's Disease is not associated
with emergence of novel inflammatory pathways. Dig Dis Sci.
63:738–745. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lozovoy MA, Simão AN, Morimoto HK, Iryioda
TM, Panis C, Reiche EM, Borelli SD, Oliveira SR, Cecchini R and
Dichi I: Hypertension is associated with serologically active
disease in patients with systemic lupus erythematosus: Role of
increased Th1/Th2 ratio and oxidative stress. Scand J Rheumatol.
43:59–62. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bai Y, Song L, Dai G, Xu M, Zhu L, Zhang
W, Jing W and Ju W: Antidepressant effects of magnolol in a mouse
model of depression induced by chronic corticosterone injection.
Steroids. 135:73–78. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Karmakar I, Haldar S, Chakraborty M,
Chaudhury K, Dewanjee S and Haldar PK: Regulation of apoptosis
through bcl-2/bax proteins expression and DNA damage by
Zanthoxylum alatum. Pharm Biol. 54:503–508. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
He SC, Wu S, Wang C, Du XD, Yin G, Jia Q,
Zhang Y, Wang L, Soares JC and Zhang XY: Interaction between job
stress and the BDNF Val66Met polymorphism affects depressive
symptoms in Chinese healthcare workers. J Affect Disord.
236:157–163. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Karege F, Perret G, Bondolfi G, Schwald M,
Bertschy G and Aubry JM: Decreased serum brain-derived neurotrophic
factor levels in major depressed patients. Psychiatry Res.
109:143–148. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shimizu E, Hashimoto K, Okamura N, Koike
K, Komatsu N, Kumakiri C, Nakazato M, Watanabe H, Shinoda N, Okada
S and Iyo M: Alterations of serum levels of brain-derived
neurotrophic factor (BDNF) in depressed patients with or without
antidepressants. Biol Psychiatry. 54:70–75. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dong JP, Sun WY, Wang S, Wu ZQ and Liu F:
Clinical observation on head point-through-point electroacupuncture
for treatment of poststroke depression. Zhongguo Zhen Jiu.
27:241–244. 2007.(In Chinese). PubMed/NCBI
|
|
20
|
Liu Q, Li B, Zhu HY, Wang YQ, Yu J and Wu
GC: Glia atrophy in the hippocampus of chronic unpredictable
stress-induced depression model rats is reversed by
electroacupuncture treatment. J Affect Disord. 128:309–313. 2011.
View Article : Google Scholar : PubMed/NCBI
|