Introduction
Cystic adventitial disease (CAD), also called
adventitial cystic disease, is a rare vascular disorder that
involves the arteries and rarely affects the veins, and most
commonly occurs in the popliteal artery of male patients (1,2). Venous
CAD (VCAD) is a rare disease with an incidence of only 0.1% among
all types of vascular disease (3). A
study by Levien and Benn (4)
reported that of the 323 cases of CAD encountered in 1998, only 17
cases (5.3%) had venous system involvement. VCAD frequently occurs
in the venous vessel wall of the proximal joint, and cysts form
between the inner and adventitial membranes (5). The progressive enlargement of a cyst,
which in turn forces the lumen, leads to the formation of a lesion
in the distal vein and causes a series of clinical symptoms. Due to
the low incidence and absence of specific symptoms, the diagnostic
rate of VCAD is low (6). The present
study reported on two cases of VCAD in femoral veins presenting as
an enlarging lower limb swelling and pain, and discussed the
relevant literature.
Case report
Case 1
A 63-year-old male patient presented with pain and
swelling of left the lower limb for one month and was admitted to
the Affiliated Hospital of Jining Medical University (Jining,
China) in July 2017. No obvious causes of the swelling in the left
lower limb were apparent and the patient had experienced persistent
calf pain for one month. The patient was diagnosed with ‘deep vein
thrombosis (DVT) of the left lower limb’ at a local hospital;
however, after treatment with warfarin, the symptoms did not
significantly improve. Hematological examination indicated that the
concentration of plasma D-dimer was normal at 0.1 mg/l (normal
concentration <0.2 mg/l), and blood routine and coagulation
parameters were normal. Color ultrasonography revealed that the
left femoral vein (above the great saphenous vein junction) had a
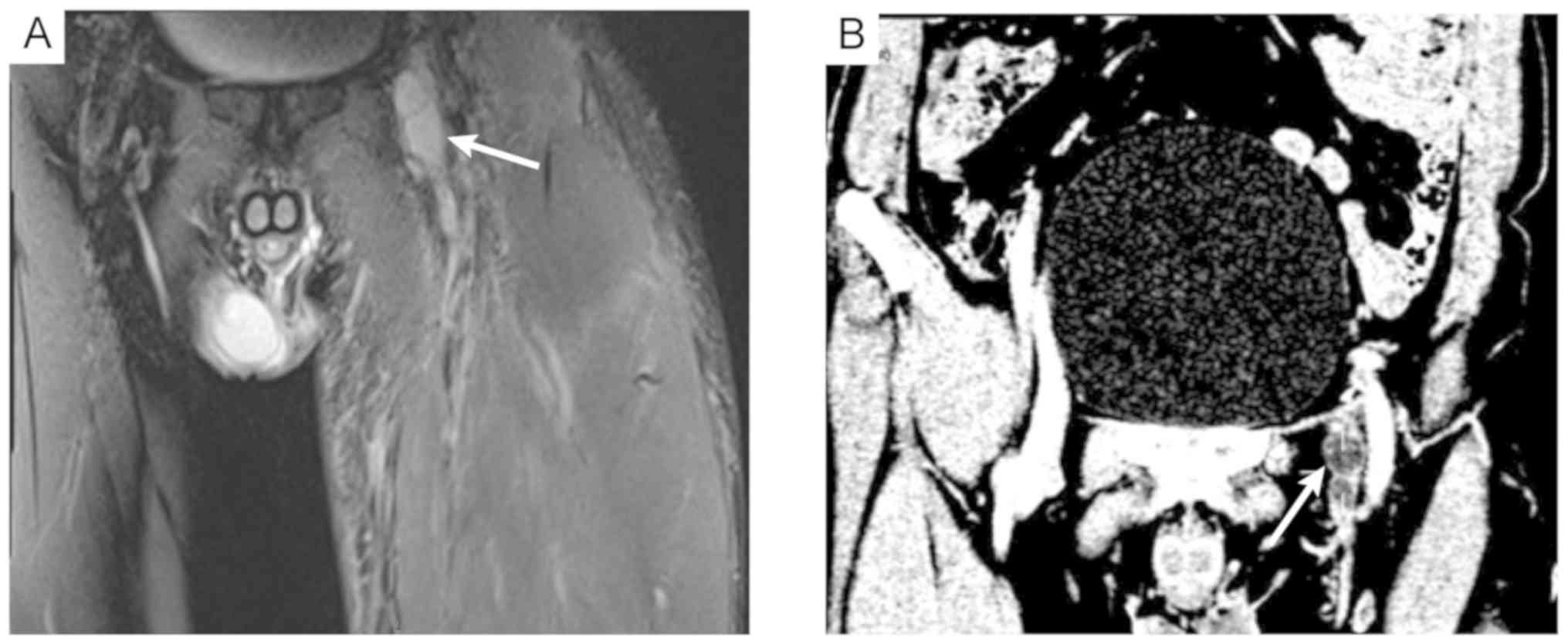
thin lumen and blood flow stagnation. On magnetic resonance imaging
(MRI), slight thickening and abnormal signals of the left femoral
vein were apparent (Fig. 1A). An
enhanced computed tomography (CT) venography scan indicated
low-density shadows of the left femoral vein (Fig. 1B).
Subsequently, the patient was given symptomatic
treatment, including reduction of the swelling by improving
microcirculation using infrared therapy, and was subjected to open
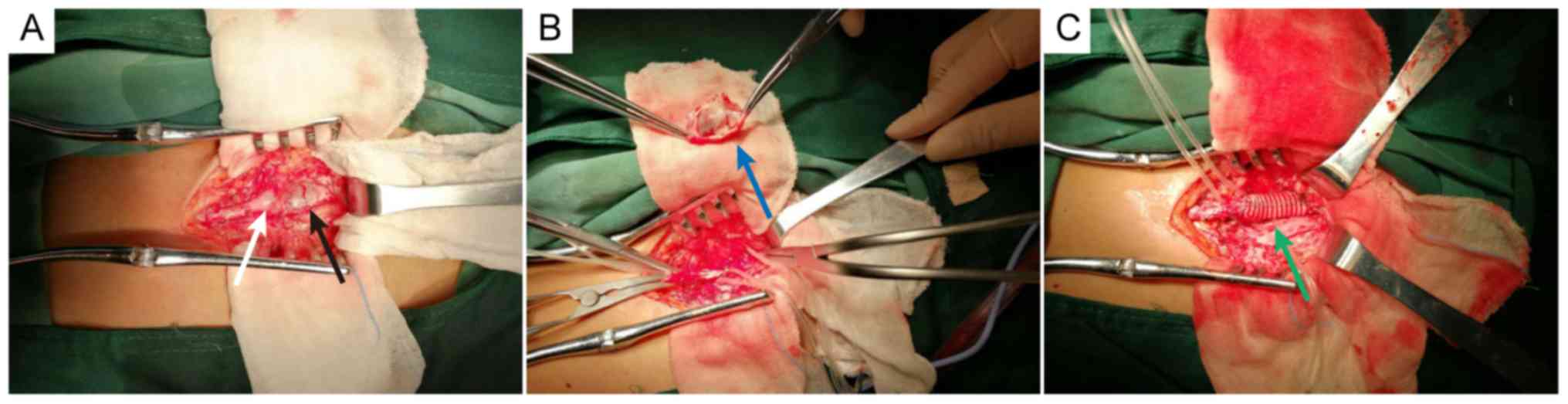
surgical treatment after exclusion of contraindications. During the
operation, two cysts in the femoral vein, which were located ~1 cm
above the confluence of the saphenous and femoral veins, were
identified. The approximate size of the small and the larger cyst
was 2.5 cm × 1.5 cm and 1.5 cm × 1.0 cm, respectively (Fig. 2A). The small cyst was slit and
removed, and the intact endothelium was visible after complete
resection of the large cyst (Fig.
2B). Subsequently, a 30 cm × 10 mm artificial blood vessel was
used to match the end of the femoral vein (Fig. 2C). After various treatments,
including chemotherapy using ceftriaxone (1 g/d; constant
intravenous drip), reducing of the swelling by infrared therapy and
fluid replacement (7), the swelling
of the left lower limb was significantly reduced and the pain
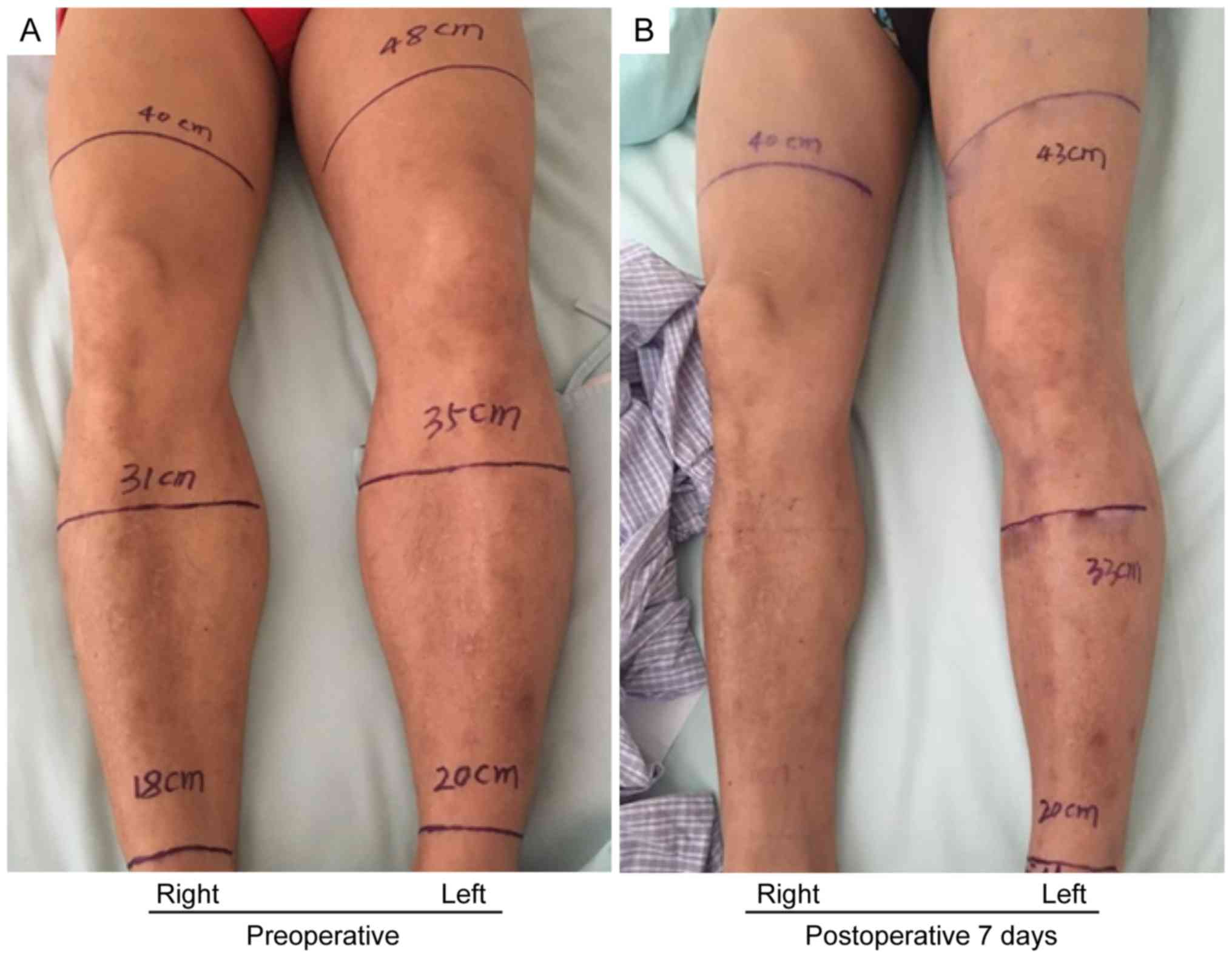
disappeared. The circumference of left lower limb at 10 cm on the
tibia, 10 cm below the tibia and 2 cm on the ankle joint was 48, 35
and 20 cm at the preoperative stage, respectively (Fig. 3A). The circumference of the left
lower limb on these locations was 43, 33 and 20 cm at 7 days
postoperatively, respectively, resembling a reduction by 5, 2 and 0
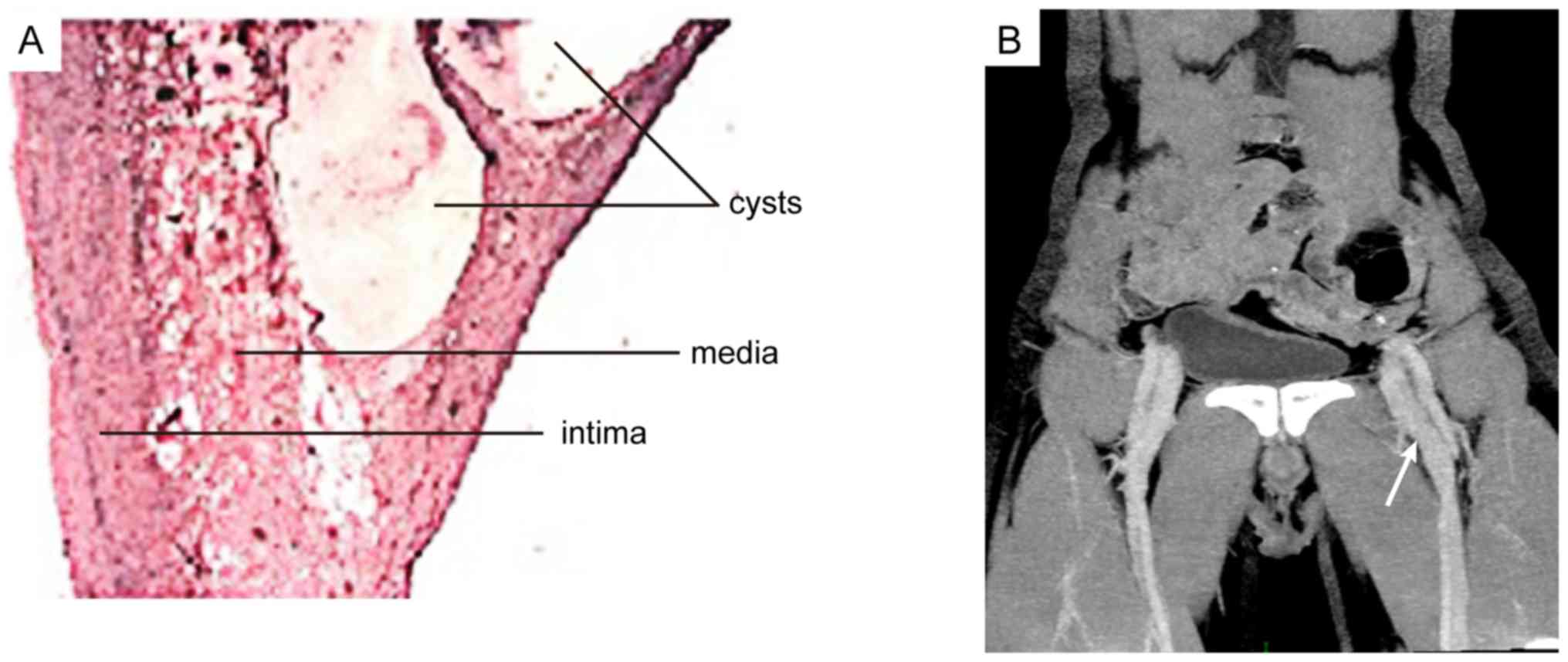
cm, respectively, compared with the preoperative measures (Fig. 3B). A postoperative histological
examination confirmed that the mass was a venous cyst (Fig. 4A). At 7 days after the surgery, the
enhanced CT venography scan revealed patency of the left femoral
vein (Fig. 4B). At the 2-month
follow-up, the circumferences of the patient's left lower limb had
returned to normal compared with 7 days postoperatively.
Case 2
A 57-year-old male was admitted to the Affiliated
Hospital of Jining Medical University (Jining, China) due to ‘right
lower limb pain and swelling for half a month’. Color
ultrasonography revealed a cystic echo below the bifurcation of the
femoral artery. The size of the cyst was 1.7 cm × 1.4 cm × 1.6 cm
with a clear boundary. Hematological examination indicated that the
concentration of plasma D-dimer was significantly increased at 1.35
mg/l (normal concentration <0.2 mg/l), and blood routine and
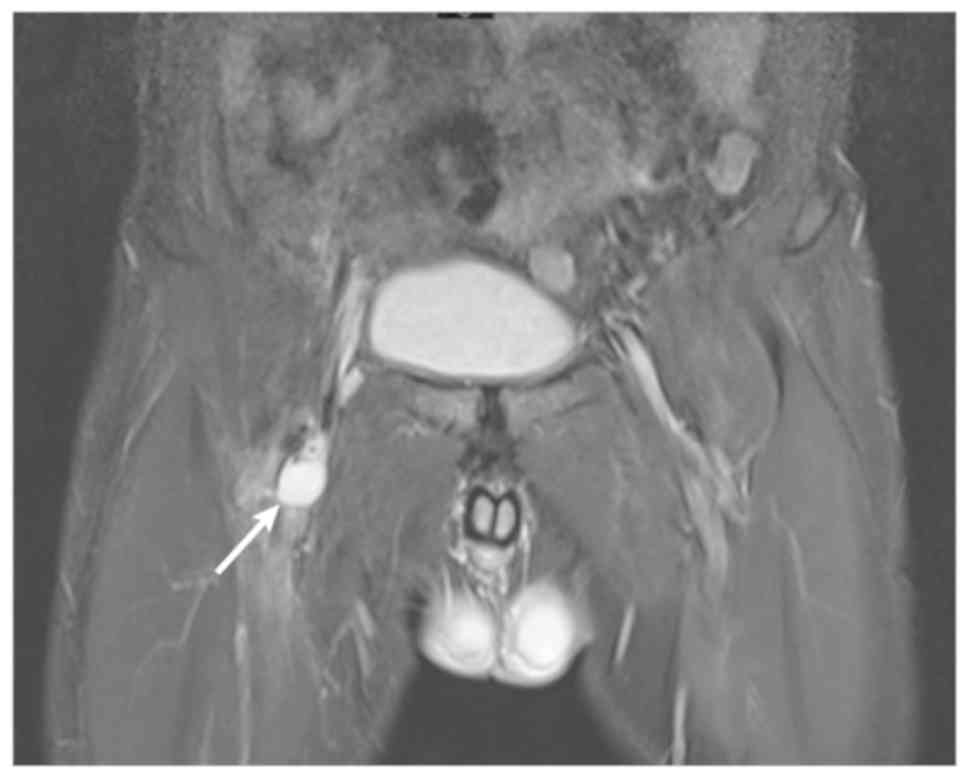
coagulation parameters were normal. MRI revealed a cystic
abnormality signal in the right groin, indicating the expansion and
effusion of the iliopsoas sac (Fig.
5). After preoperative examination, open surgical treatment was
performed. During the operation, a cyst (~2 cm in diameter) was
located behind the right femoral artery, causing the right femoral
vein to move inward and downward. The cyst was closely attached to
the wall of the right femoral vein and was difficult to separate.
Forcible separation may cause massive bleeding of the femoral vein.
Therefore, part of the cyst wall was slit, and a yellow jelly-like
substance was removed. Postoperative pathology confirmed that the
mass was a venous cyst. The patient's pain and swelling disappeared
after postoperative treatment with infrared therapy and fluid
replacement, and no obvious abnormalities remained at the 2-month
follow-up.
Discussion
In 1947, Atkins and Key (8) first reported on a cystic disease that
occurred in the external iliac artery, and Mentha (9) reported on a cystic disease in the
venous system (small saphenous vein) in 1963, whereas neither
article described the causes of VCAD. To date, the etiology of VCAD
has remained elusive. The following hypotheses regarding the
occurrence of VCAD have been made: i) The ‘Repeat Traumatic Theory’
(4,10), suggests that due to joint movement,
the blood vessels in the proximal joint are repeatedly stretched,
resulting in damage to the vessel wall. The accumulation of such
tiny wounds causes chronic degeneration of the wall and the gradual
formation of a cyst; ii) During embryonic development, certain
poorly differentiated mesenchymal cells with mucin secretion
function in adjacent joints are incorrectly implanted into the
adventitia, and these cells gradually begin to secrete mucin and
eventually form a cyst (11); iii)
Ectopic implantation of ganglion cyst (12) and iv) Systemic connective tissue
lesions (2).
The clinical manifestations of VCAD are not
specific. Most patients present with unilateral limb swelling and
the onset is usually slow (up to several months or even one year)
(2). When VCAD occurs in a
superficial blood vessel, the cyst may be localized by palpitation
during the examination (6). In
previously reported cases, cysts were mostly located in the groin
(3,13). In the present study, the two cases
presented with unilateral limb swelling and slow disease onset,
which was consistent with the clinical manifestations of VCAD. The
diagnosis for VCAD mainly relies on data of the medical imaging
examination. Angiography may determine the degree of lumen
stenosis, but it is difficult to observe the structure of the cyst.
Compared with angiography for the diagnosis of VCAD, ultrasound, CT
and MRI are more advantageous, which may allow for observation of
the cyst structure and facilitate the diagnosis (14). Compared with MRI and ultrasound,
enhanced CT venography scan may provide oblique images taken from
different angles, comprehensively evaluate the shape and degree of
the cyst and provide a basis for its treatment (15,16). In
the present study, the preoperative data from the enhanced CT had
an important role in the diagnosis and treatment of VCAD.
At present, the therapeutic methods for VCAD mostly
comprise surgical treatment. The major surgical methods are as
follows: Cyst incision, cyst wall resection, cyst puncture and
drainage, and cyst and vascular resection + artificial/autologous
vascular transplantation (17,18).
There are significant differences in recurrence rates depending on
the type of surgery. Bascone et al (17) analyzed the medical records of 45
patients diagnosed with VCAD between January 1947 and March 2016,
and determined that the recurrence rate in patients with cyst
incision and cyst wall resection was 20.0%, while the recurrence
rate in patients with cyst and vascular resection +
artificial/autologous vascular transplantation was 14.3%, and the
recurrence rate in patients with cyst puncture and drainage was as
high as 83.3%. The overall recurrence rate of VCAD is ~26.7%. For
patients with VCAD, the root cause of vascular compression cannot
be relieved by interventional surgery. If the vascular stent is
required to cross the joint, the stent may be displaced or
morphologically changed due to joint activity, and the blood vessel
will again appear narrow (19).
Therefore, VCAD is less commonly treated by vascular interventional
therapy. Furthermore, certain reports suggest that cyst drainage
and sclerotherapy may also have high clinical efficacy (19,20).
VCAD is a rare vascular disease, and the underlying
causes remain elusive. Medical imaging examination is of high
significance in the diagnosis of VCAD. Preoperative CT
three-dimensional reconstruction may provide guidance for surgical
treatment. In clinical practice, for patients with suspected DVT,
VCAD should be considered when patients have no evidence of vein
thrombosis, and further imaging examination is required to confirm
the diagnosis. At present, only few domestic studies on VCAD are
available. As the knowledge of this disease deepens, it is likely
that a larger quantity of VCAD cases are reported in the future,
the etiology and pathogenesis of VCAD will gradually be elucidated
and its treatment will become standardized.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
PL, JWY, CM, GDW, TJ and ZQS performed the surgery.
PL, BY and YHZ collected and analyzed the data. PL, BY and ZQS
prepared the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethical Board
of the Affiliated Hospital of Jining Medical University and
performed in accordance with the Declaration of Helsinki (2000).
Written informed consent was obtained from all participants.
Patient consent for publication
The patients have provided informed consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lezotte J, Le QP, Shanley C and Hans S:
Adventitial cystic disease: Complicated and uncomplicated. Ann Vasc
Surg. 46:370.e13–370.e15. 2018. View Article : Google Scholar
|
|
2
|
Li S, King BN, Velasco N, Kumar Y and
Gupta N: Cystic adventitial disease-case series and review of
literature. Ann Transl Med. 5:3272017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Scott MF, Gavin T and Levin S: Venous
cystic adventitial disease presenting as an enlarging groin mass.
Ann Vasc Surg. 28:489.e15–8. 2014. View Article : Google Scholar
|
|
4
|
Levien LJ and Benn CA: Adventitial cystic
disease: A unifying hypothesis. J Vasc Surg. 28:193–205. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen Y, Sun R, Shao J, Li Y and Liu C: A
contemporary review of venous adventitial cystic disease and three
case reports. Phlebology. 30:11–16. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim YK, Chun HJ, Hwang JK, Kim JI, Kim SD,
Park SC and Moon IS: Adventitial cystic disease of the common
femoral vein presenting as deep vein thrombosis. Asian J Surg.
39:178–181. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Manning MW, Dunkman WJ and Miller TE:
Perioperative fluid and hemodynamic management within an enhanced
recovery pathway. J Surg Oncol. 116:592–600. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Atkins HJ and Key JA: A case of myxomatous
tumour arising in the adventitia of the left external iliac artery;
case report. Br J Surg. 34:4261947. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mentha C: Mucoid degeneration of veins. J
Cardiovasc Surg (Torino). 4:591–594. 1963.(In French). PubMed/NCBI
|
|
10
|
Desy NM and Spinner RJ: The etiology and
management of cystic adventitial disease. J Vasc Surg. 60:235–245.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dix FP, McDonald M, Obomighie J, Chalmers
N, Thompson D, Benbow EW and Smyth JV: Cystic adventitial disease
of the femoral vein presenting as deep vein thrombosis: A case
report and review of the literature. J Vasc Surg. 44:871–874. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Spinner RJ, Desy NM, Agarwal G, Pawlina W,
Kalra M and Amrami KK: Evidence to support that adventitial cysts,
analogous to intraneural ganglion cysts, are also joint-connected.
Clin Anat. 26:267–281. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim HK, Hwang D, Park S, Jeong WJ, Seo AN
and Huh S: Cystic disease of the groin presenting as compression of
a femoral vessel. Vasc Specialist Int. 32:124–128. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mousa AY, Alhalbouni S, Abu-Halimah S,
Gill G, Sadek B, Nanjundappa A, Hass SM and Aburahma AF: Cystic
adventitial disease of the common femoral vein: A case report and
review of the literature. Vasc Endovascular Surg. 47:569–572. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wu X, Lun Y, Jiang H, Gang Q, Duan Z, Xin
S and Zhang J: Cystic adventitial disease of the common femoral
vessels: Report of 2 cases and literature review. Vasc Endovascular
Surg. 48:325–328. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Seo JY, Chung DJ and Kim JH: Adventitial
cystic disease of the femoral vein: A case report with the CT
venography. Korean J Radiol. 10:89–92. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bascone C, Iqbal M, Narh-Martey P,
Szuchmacher M, Cicchillo M and Krishnasastry KV: Venous adventitial
cystic disease: A review of 45 cases treated since 1963. Int J Vasc
Med. 2016:52876972016.PubMed/NCBI
|
|
18
|
Takizawa K, Osawa H, Kojima A, Abraham SJK
and Hosaka S: Cystic adventitial disease of popliteal artery with
venous aneurysm of popliteal vein: Two-year follow-up after
surgery. Case Rep Vasc Med. 2017:48734742017.PubMed/NCBI
|
|
19
|
Johnson JM, Kiankhooy A, Bertges DJ and
Morris CS: Percutaneous image-guided aspiration and sclerosis of
adventitial cystic disease of the femoral vein. Cardiovasc
Intervent Radiol. 32:812–816. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Roth JA, Kearney P and Wittmann CJ: Cystic
adventitial degeneration of the common femoral artery. Arch Surg.
112:210–212. 1977. View Article : Google Scholar : PubMed/NCBI
|