Introduction
Sepsis is a major health problem and a leading cause
of mortality and critical illness worldwide (1–3). It
presents a syndrome of physiological, pathological and biochemical
abnormalities induced by infection (3). The updated Sepsis-3 criteria defines
sepsis as life-threatening organ dysfunction caused by a
dysregulated host response to infection (3–5). For
clinical operationalization, an increase in sequential organ
failure assessment (SOFA) score of ≥2 points may indicate organ
dysfunction and an associated >10% change of in-hospital
mortality (3). Urosepsis is defined
as sepsis caused by a urogenital tract infection and it may be
caused by urinary tract obstruction or complication following
surgical interventions (6–8). Urolithiasis-associated sepsis, caused
by obstructive upper ureteral calculi or postoperative
complications following percutaneous nephrolithotomy (PCNL),
ureteroscopic lithotripsy (URL) and laparoscopic lithotomy, is a
severe global problem in the field of urology (9–13). To
the best of our knowledge, there is no consensus on whether the
Sepsis-3 criteria are an effective prognostic tool for patients
with urolithiasis-associated sepsis.
A number of studies have evaluated the effectiveness
of Sepsis-3 criteria for predicting in-hospital mortality among
patients with suspected infection that are admitted to the
emergency department (ED) or intensive care unit (ICU) (14–19).
Studies have demonstrated that SOFA scores are superior for
predicting mortality when compared to systemic inflammatory
response syndrome (SIRS) and quick SOFA (qSOFA) criteria (15,18,19).
However, there may be unique differences between urosepsis and
sepsis caused by other factors, particularly
urolithiasis-associated sepsis that develops following surgical
interventions (6–8,20–22). In
addition, there may be differences in the application of Sepsis-3
criteria among different countries and at different levels of
health care. Furthermore, it is clear that urologists are
unfamiliar with the new definition of sepsis when compared with
clinicians working in the ED or ICU.
The aim of the present study was to compare the
effectiveness of Sepsis-3 (SOFA and qSOFA) and SIRS criteria for
predicting in-hospital mortality or prolonged length of ICU stay
(>3 days) among patients with urolithiasis-associated sepsis
that were transferred to the ICU following surgical
interventions.
Materials and methods
Patients and methods
In the present study, the records of all patients
who had been transferred to ICU following surgical interventions
with urolithiasis-associated sepsis in our institution (Xin Hua
Hospital Affiliated to Shanghai Jiao Tong University) from January
2010 to July 2017 were retrospectively reviewed. Due to the lack of
application of SOFA criteria in the urology department, certain
patients were not included. The study population consisted of
patients with urosepsis caused by obstructive upper ureteral or
renal calculi who were transferred to ICU following emergency
surgical decompression (ureteroscopic double J stenting), or
patients with postoperative sepsis following PCNL or URL who were
then transferred to ICU. Due to the lack of critical life-support
device and 24 h care available, patients with suspicious sepsis in
all surgical departments should be transferred to the specialized
surgical intensive care unit (SICU) in Xin Hua Hospital Affiliated
to Shanghai Jiao Tong University. For convenience, the definitions
of ICU and SICU are used interchangeably in the present study. The
Sepsis-3 and SIRS criteria scores were calculated based on the
results of initial laboratory tests and physical examination
performed upon admission to the SICU. Altered mental status, within
the qSOFA criteria, was defined using the Glasgow Coma Scale, with
a score of <15, or any clinical signs, determined by clinicians.
Patients with no complete previous medical record of chronic renal,
liver or respiratory dysfunction, were assigned a baseline SOFA
score of 0 (15). In the present
study, in-hospital mortality was defined as sepsis-associated
mortality at any time during patient hospitalizations. In-hospital
mortality and prolonged length of ICU stay (>3 days) were
considered as adverse outcomes, which the Sepsis-3 and SIRS
criteria may predict.
All patients were examined preoperatively with
urinary ultrasonography or/and computed tomography in the ED or
urology department to evaluate the existence of urolithiasis.
Consistent with previous studies, evidence of infection was
identified through the analysis of radiological studies,
microbiological data or clinical symptoms (14). The diagnosis of urosepsis was
conducted by the patient's primary surgeon or the on-duty senior
surgeon according to SIRS criteria (January 2010 to March 2016) and
SOFA scores (April 2016 to July 2017). In certain circumstances,
the decision was made based on personal experiences of the
clinicians, or conclusions were drawn from a consensus of several
urology experts. Exclusion criteria were as follows: Age, <18
years old; patients who were receiving regular chemotherapy or
immunosuppressant therapy; patients with unidentifiable sources of
infection from the urinary tract; patients with multiple system
infections without an identifiable primary source; patients who did
not undergo any surgical interventions prior to transfer to the
SICU; and patients with incomplete retrospective data for measuring
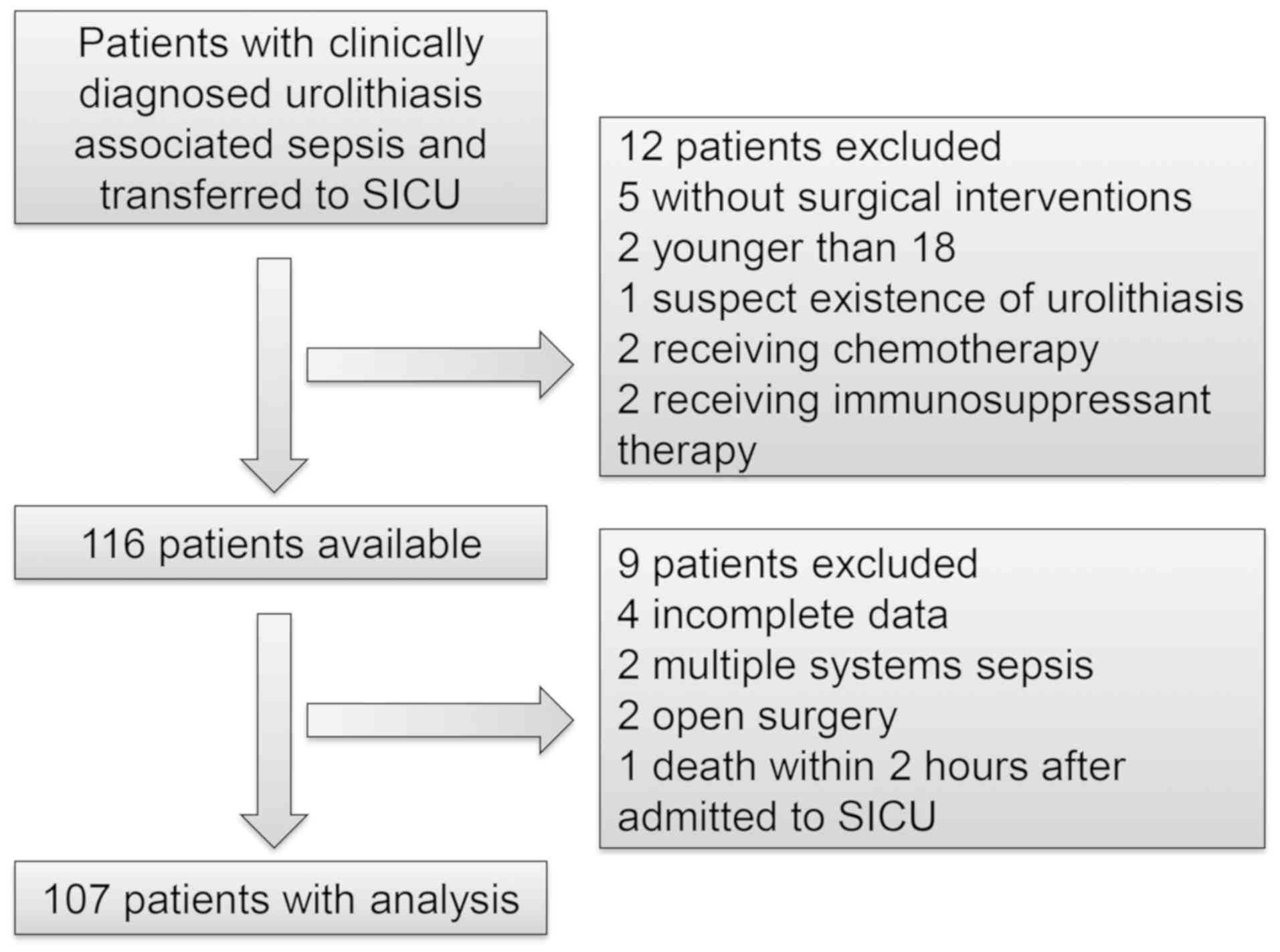
Sepsis-3 and SIRS criteria. The flow diagram of patient enrollment
is presented in Fig. 1.
Surgical procedure
The methods used to perform PCNL, URL and emergency
ureteroscopic double J stenting procedures were analogous with
other previously described methods (11,12,23).
Patients with obstructive urolithiasis and suspected urosepsis, as
diagnosed by the emergency physicians, were transferred to the
urology department. Following assessment of their condition,
patients underwent emergency ureteroscopic double J stenting under
local, spinal or general anesthesia and were then transferred to
SICU. Conversely, following routine PCNL or URL, patients with
suspected postoperative urosepsis were directly transferred to
SICU. Generally, all patients were treated immediately with
appropriate broad-spectrum intravenous antibiotics and
resuscitation with intravenous fluids when the occurrence or
symptoms of sepsis were confirmed. All procedures were performed by
experienced physicians, while emergency ureteroscopic double J
stenting was occasionally performed by younger residents.
Ethics approval and consent to
participate
The Ethics Committee of Xin Hua Hospital Affiliated
to Shanghai Jiao Tong University School of Medicine approved this
retrospective study and permitted the waiver of written informed
consent from patients (approval no., XHEC-D-2018-074). The study
protocol was performed in accordance with the Declaration of
Helsinki.
Statistical analysis
All analyses were performed using SPSS®
(v.19.0; SPSS Software, Inc.), R (v.3.5.1) with RStudio (v.1.1.456)
and MedCalc (v.18.2.1). Data were presented as the mean ± standard
deviation or medians with interquartile ranges for continuous
variables, numbers and proportions for categorical variables.
Comparisons between groups were conducted using χ2 tests
for proportions and unpaired Student's t-tests for normally
distributed data. All P-value analyses were two-sided and P<0.05
was considered to indicate a statistically significant difference.
The predictive performance of SOFA, qSOFA and SIRS for the primary
outcome (in-hospital mortality and prolonged length of ICU stay)
was assessed. Prognostic discrimination was determined by comparing
the area under the receiver operating characteristic curve (AUROC)
for each criterion (SOFA, qSOFA and SIRS) individually (14) as described previously using the Z
statistic. Furthermore, AUROC were adjusted for patient age and
comorbidities using binary logistic regression. The covariables
used included: Age; hypertension; cardiovascular disease; chronic
obstructive pulmonary disease; diabetes mellitus; cerebrovascular
disease; chronic kidney disease; history of malignancy; SIRS; SOFA;
and qSOFA. The categorical covariates included: Hypertension;
cardiovascular disease; chronic obstructive pulmonary disease;
diabetes mellitus; cerebrovascular disease; chronic kidney disease;
history of malignancy; SIRS; SOFA; and qSOFA.
Results
Patient characteristics and
outcomes
A total of 107 patients (72 females and 35 males)
enrolled in the study cohort and their results were statistically
analyzed. These included 63 patients that had undergone emergency
ureteroscopic double-J stenting, 20 patients following PCNL and 24
patients following URL. Their detailed baseline characteristics are
summarized in Table I. The overall
in-hospital mortality rate was 8.4% (9/107), and the percentage of
in-hospital mortality or prolonged length of ICU stay (>3 days)
was 72.0% (77/107). The median age was 66 (range, 54–77) years and
32.7% were male. The primary comorbidities included: Hypertension
(46.7%); cardiovascular disease (14.0%); chronic obstructive
pulmonary disease (13.1%); diabetes mellitus (22.4%);
cerebrovascular disease (15.0%); chronic kidney disease (11.2%);
gout (6.5%); and history of malignancy (7.5%). The median of qSOFA
score was 2 (range, 1–3) and 84.1% patients exhibited a qSOFA score
of ≥2. The median of SOFA score was 5 (range, 0–15) and 80.14%
patients exhibited an increase in SOFA score of ≥2. The median of
patients' SIRS criteria was 4 (range, 2–4) and all patients
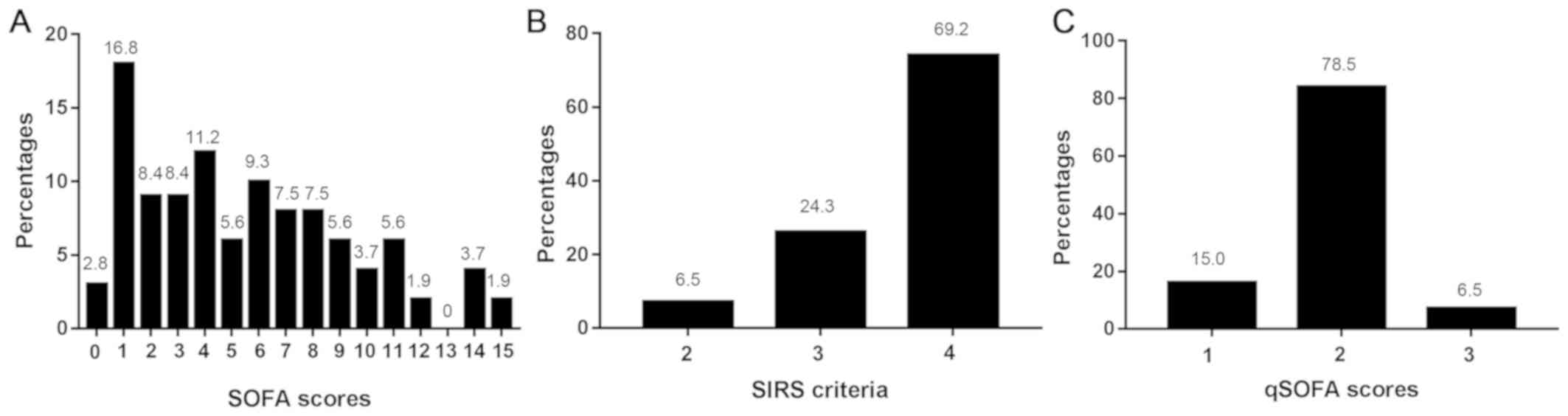
exhibited ≥2 SIRS criteria. The distributions of each score (SOFA,
qSOFA and SIRS) are presented in Fig.
2A-C.
 | Table I.Baseline characteristics. |
Table I.
Baseline characteristics.
| Variable | All patients
(n=107) | Favorable outcome,
SICU stay ≤3 days (n=30) | Adverse outcome,
in-hospital mortality or SICU stay >3 days (n= 77) | P-value |
|---|
| Age, years, median
(IQR), | 66 (54–77) | 64 (54–73) | 67 (54–80) | 0.19 |
| Sex, male, % | 35 (32.7) | 21 (70.0) | 14 (18.2) | <0.001 |
| Surgical procedures,
n (%) |
| PCNL | 20 (18.7) | 6 (20.0) | 14 (18.2) | 0.83 |
|
URL | 24 (22.4) | 6 (20.0) | 18 (23.4) | 0.71 |
| DJ
stent | 63 (58.9) | 18 (60.0) | 45 (58.4) | 0.88 |
| Comorbidities, n
(%) |
|
Hypertension | 50 (46.7) | 12 (40.0) | 38 (49.4) | 0.384 |
|
Cardiovascular disease | 15 (14.0) | 4 (13.3) | 11 (14.3) | 1.0 |
| Chronic
obstructive pulmonary disease | 14 (13.1) | 4 (13.3) | 10 (13.0) | 1.0 |
|
Diabetes mellitus | 24 (22.4) | 5 (16.7) | 19 (24.7) | 0.372 |
|
Cerebrovascular disease | 16 (15.0) | 4 (13.3) | 12 (15.6) | 1.0 |
| Chronic
kidney disease | 12 (11.2) | 5 (16.7) | 7 (9.1) | 0.265 |
|
Gout | 7 (6.5) | 3 (10.0) | 4 (5.2) | 0.64 |
| History
of malignancy | 8 (7.5) | 2 (6.7) | 6 (7.8) | 1.0 |
| Laboratory results,
median (IQR) |
| WBC,
×109/l | 16.21
(11.30–23.54) | 13.95
(7.07–15.51) | 19.60
(13.40–24.80) | <0.001 |
|
C-reactive protein, mg/l | 118 (45–160) | 48 (12–160) | 160 (65–160) | 0.002 |
| PCT,
ng/ml | 17.91
(3.43–96.23) | 2.18
(0.23–7.77) | 29.60
(13.82–100.00) | <0.001 |
| Vital signs |
|
Temperature, °C | 38.5
(38.0–38.9) | 38.65
(38.0–39.0) | 38.5 (38–38.9) | 0.32 |
|
Systolic blood pressure,
mmHg | 78 (72–83) | 84.5 (79–90) | 76 (71–81) | <0.001 |
| Mean
arterial pressure, mmHg | 59.3 (56–63) | 63.3
(60.0–66.3) | 58.3
(55.7–60.3) | <0.001 |
|
Respiratory rate, /min | 27 (23–32) | 26 (22–32) | 27 (23–31) | 0.89 |
| Heart
rate, /min | 114 (103–125) | 116.5
(105–127) | 113 (103–125) | 0.55 |
| Altered
mental status, n (%) | 11 (10.3) | 0 (0) | 11 (14.3) | 0.032 |
| Evaluation
criteria |
|
SOFA | 5 (2–8) | 1 (1–3) | 6 (4–9) | <0.001 |
|
qSOFA | 2 (2–2) | 2 (1–2) | 2 (2–2) | 0.01 |
|
SIRS | 4 (3–4) | 3.5 (3–4) | 4 (4–4) | 0.04 |
| SOFA
≥2, n (%) | 86 (80.4) | 11 (36.7) | 75 (97.4) | <0.001 |
| qSOFA
≥2, n (%) | 90 (84.1) | 21 (70) | 69 (89.6) | 0.034 |
| SIRS
≥2, n (%) | 107 (100) | 30 (100) | 77 (100) | NA |
Comparisons between favorable (n=30)
and adverse outcome groups (n=77)
No difference in the number of patients that had
undergone each type of surgical procedure in the favorable and
adverse outcome groups was observed (PCNL, 20 vs. 18.2%; URL, 20
vs. 23.4%; DJ stent, 60 vs. 58.4%). No significant differences in
age and comorbidities were observed between the two groups.
However, the percentage of males was significantly increased in the
favorable outcome group. The favorable outcome group also exhibited
significantly decreased white blood cell (WBC) counts (13.95 vs.
19.60×109/l, P<0.001), and levels of C-reactive
protein (48 vs. 160 mg/l, P=0.002) and procalcitonin (2.18 vs.
29.60 ng/ml, P<0.001). Systolic blood pressure (84.5 vs. 76
mmHg, P<0.001) and mean arterial pressure (63.3 vs. 58.3 mmHg,
P<0.001) were significantly decreased in the adverse outcome
group. The level of patients with altered mental state was
significantly increased in the adverse outcome group. The SOFA,
qSOFA scores and SIRS criteria were significantly increased in
adverse outcome groups. In addition, the percentage of patients
with SOFA score ≥2 points and qSOFA ≥2 points was significantly
increased in adverse outcome group. The results for all parameters
are summarized in Table I.
Prognostic performance
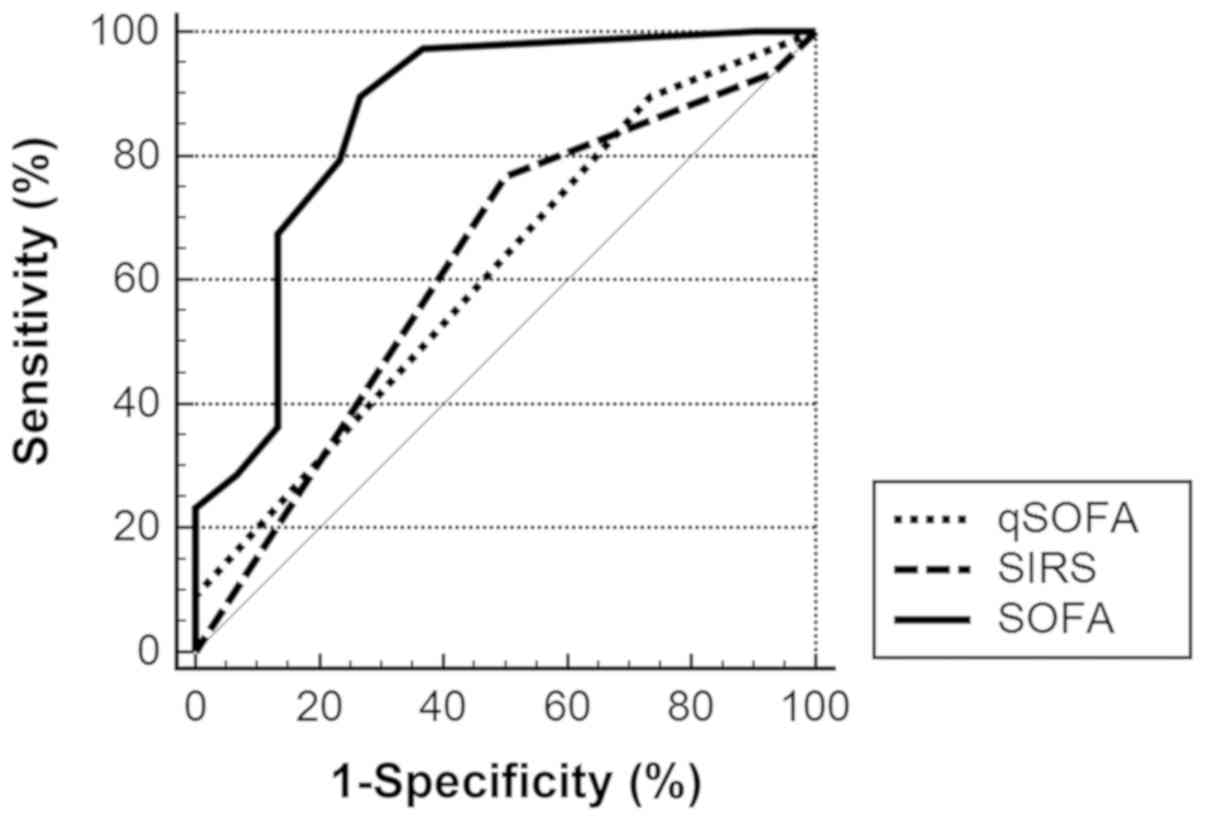
For the prediction of adverse outcomes (in-hospital
mortality or length of ICU stay >3 days), the AUROC values of
qSOFA, SIRS and SOFA were 0.615 [95% confidence interval (CI),
0.516–0.707], 0.625 (95% CI, 0.526–0.716) and 0.860 (95% CI,
0.780–0.920), respectively. SOFA scores were significantly improved
compared with SIRS (0.860 vs. 0.625, P<0.0001) and qSOFA (0.860
vs. 0.615, P=0.0002) for the prediction of adverse outcome. There
was no significant difference between SIRS and qSOFA (0.625 vs.
0.615, P=0.887). SOFA score ≥2 points presented high sensitivity at
97.40% and moderate specificity at 63.33% for prediction. The
cutoff of SIRS was set as >2 criteria (normally ≥2). The
detailed results are summarized in Tables II, III, IV
and Fig. 3.
 | Table II.Crude and adjusted AUROC. |
Table II.
Crude and adjusted AUROC.
| AUROC | qSOFA | SOFA | SIRS |
|---|
| Crude AUROC, 95%
CI | 0.615
(0.516–0.707) | 0.860
(0.780–0.920) | 0.625
(0.526–0.716) |
| Adjusted AUROC, 95%
CI | 0.713
(0.618–0.797) | 0.940
(0.877–0.977) | 0.722
(0.627–0.804) |
 | Table III.Comparison between crude AUROC. |
Table III.
Comparison between crude AUROC.
| Comparisons | Difference between
areas | 95% confidence
interval | Standard error | Z statistic | P-value |
|---|
| qSOFA vs. SIRS | 0.00996 | −0.128–0.148 | 0.0703 | 0.142 | 0.8874 |
| qSOFA vs. SOFA | 0.246 | 0.117–0.374 | 0.0657 | 3.740 | 0.0002 |
| SIRS vs. SOFA | 0.236 | 0.133–0.338 | 0.0523 | 4.506 | <0.0001 |
 | Table IV.Sensitivity, specificity and
likelihood ratios. |
Table IV.
Sensitivity, specificity and
likelihood ratios.
| Criteria | Sensitivity, % (95%
CI) | Specificity, % (95%
CI) | Positive Predictive
value, % (95% CI) | Negative Predictive
value, % (95% CI) | Positive Likelihood
ratio, % (95% CI) | Negative Likelihood
ratio, % (95% CI) |
|---|
| qSOFA ≥2 | 89.61
(80.6–95.4) | 26.67
(12.3–45.9) | 75.8
(71.4–79.8) | 50.0
(29.2–70.8) | 1.22 (1.0–1.5) | 0.39 (0.2–0.9) |
| qSOFA ≥2 | 97.40
(90.9–99.7) | 63.33
(43.9–80.1) | 87.2
(81.0–91.6) | 90.5
(70.2–97.5) | 2.66 (1.7–4.3) | 0.041
(0.01–0.2) |
| SIRS >2 | 93.51
(85.5–97.9) | 6.67
(0.8–22.1) | 72.0
(69.7–74.2) | 28.6
(7.6–66.1) | 1.00 (0.9–1.1) | 0.97 (0.2–4.8) |
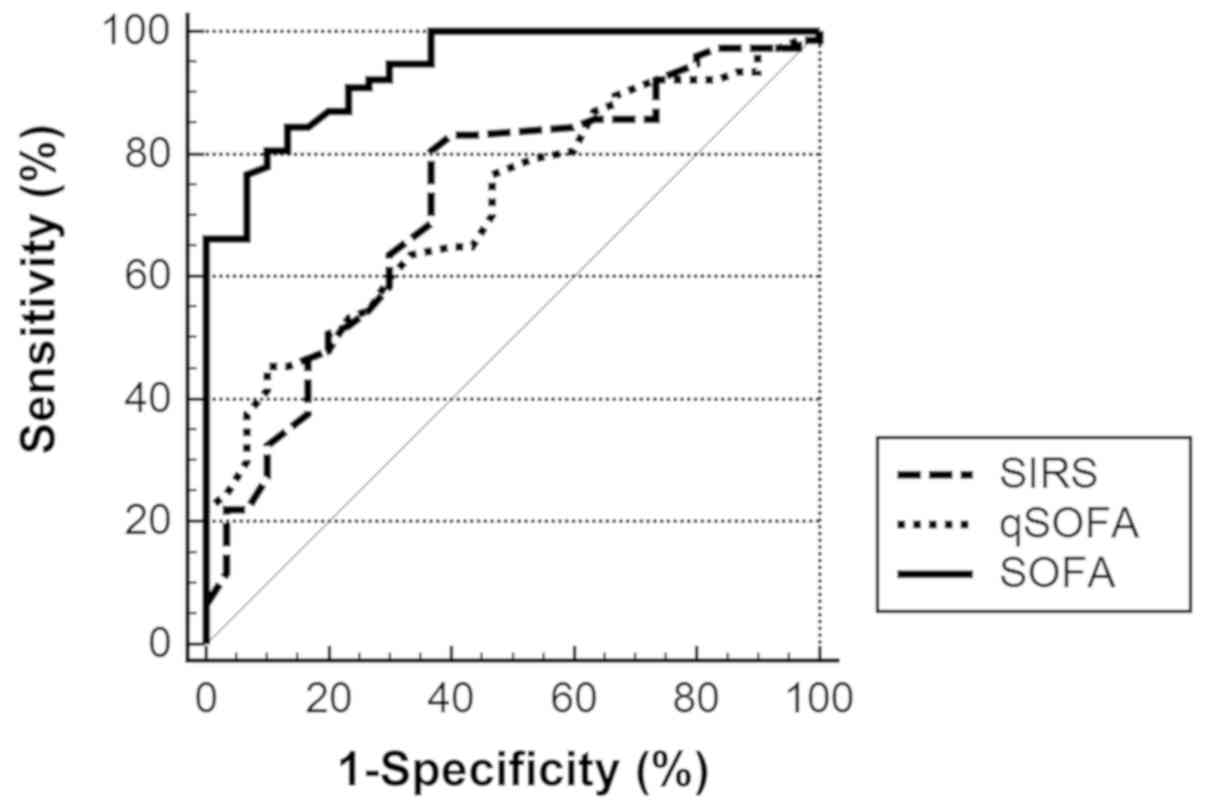
Adjusted AUROC
The AUROC values of the models used to predict
adverse outcomes were adjusted for patient age and comorbidities
using binary logistic regression (Tables SI–III). The adjusted AUROC values of qSOFA,
SIRS and SOFA were 0.713 (95% CI, 0.618–0.797), 0.722 (95% CI,
0.627–0.804) and 0.940 (95% CI, 0.877–0.977), respectively.
Comparing the prognostic value of each criteria using the adjusted
AUROC values yielded similar results as the comparisons using the
crude AUROC values. SOFA was significantly improved compared with
SIRS and qSOFA for the prediction of adverse outcomes, and no
significant difference between SIRS and qSOFA was observed. The
detailed results are described in Tables II, V
and Fig. 4.
 | Table V.Comparison between adjusted
AUROC. |
Table V.
Comparison between adjusted
AUROC.
| Comparisons | Difference between
areas | 95% confidence
interval | Standard error | Z statistic | P-value |
|---|
| qSOFA vs. SIRS | 0.00844 | −0.102–0.119 | 0.0564 | 0.150 | 0.8811 |
| qSOFA vs. SOFA | 0.227 | 0.134–0.319 | 0.0473 | 4.800 | <0.0001 |
| SIRS vs. SOFA | 0.218 | 0.118–0.319 | 0.0513 | 4.254 | <0.0001 |
Discussion
To the best of our knowledge, the present study was
the first to validate and compare the prognostic performance of
Sepsis-3 and SIRS criteria in patients with urolithiasis-associated
sepsis. However, it remains unknown whether Sepsis-3 and SIRS
criteria are good prognostic tools for in-hospital mortality or
prolonged ICU stay in these specific patients, particularly those
that have undergone modern urologic endoscopic lithotripsy
procedures. Considering the size of the study population,
in-hospital mortality or prolonged ICU stays (>3 days) were set
as the primary outcomes, which may be considered as secondary
outcomes for other large-scale studies. SOFA score, SIRS criteria
and qSOFA score have been validated and compared in several
previous studies involving patients with suspected infection
admitted to ICU or ED (14,15) for their prognostic accuracy. These
large-scale prospective studies demonstrated the advantages of the
Sepsis-3 criteria compared with SIRS. However, a previous study has
indicated that SIRS was associated with organ dysfunction and
mortality, so it would be premature to entirely discard this
criteria (19). qSOFA criteria
demonstrated high specificity in a prospective ED database
(19); however, poor sensitivity may
limit its utility as a bedside screening method. Several statements
were provided by the Surviving Sepsis Guideline panel on early
management and resuscitation for sepsis or septic shock patients in
a recent update (24). However, this
study population was primarily characterized using the Sepsis-1
guidelines (24). This previous
definition of sepsis included: Sepsis; severe sepsis; and septic
shock (24). Therefore, a number of
studies have established these guidelines without re-unification of
the new definition of sepsis and septic shock (24). It takes time to validate, accept and
incorporate novel definitions into general practice among
clinicians and policymakers. Furthermore, previous studies may
focus on the universal prognostic tool for all sepsis derived from
different systems. For the purposes of the present study, it was
considered more important to verify the prognostic accuracy of
patients with urolithiasis-associated sepsis only. In addition, the
aim of the present study was to evaluate the effectiveness of
Sepsis-3 and SIRS criteria among patients following surgical
interventions. It is likely that the composition of these patients
may differ from ordinary patients in the ED or ICU.
In sepsis, disease-specific severity scores may have
excellent prognostic performance, as the classifications were
derived from databases of these specific diseases (16). It is therefore apparent that qSOFA,
SOFA and SIRS criteria, which were developed for general infectious
diseases (16), may differ from
urosepsis or specific urolithiasis-associated sepsis severity
classifications. Unfortunately, there were no valid and specific
severity classifications used for patients with
urolithiasis-associated sepsis in the present study. However, a
uniform standard or classification of different infectious diseases
may be a convenient tool for clinicians to utilize, particularly
outside of ICU or ED. Urologists may be unfamiliar with the new
definition and scale scores of Sepsis. Therefore, enhancing
awareness of the new Sepsis-3 classification system is important,
as it may profoundly affect clinicians and their patients.
In the present study, the prognostic performance
(crude AUROC) of qSOFA, SIRS and SOFA for predicting adverse
outcomes (in-hospital mortality or length of ICU stay >3 days)
were 0.615 (95% CI, 0.516–0.707), 0.625 (95% CI, 0.526–0.716) and
0.860 (95% CI, 0.780–0.920), respectively. Following adjustment for
patient age and comorbidities, the values increased to 0.713 (95%
CI, 0.618–0.797), 0.722 (95% CI, 0.627–0.804) and 0.940 (95% CI,
0.877–0.977) for qSOFA, SIRS and SOFA, respectively. The results of
the assessment of prognostic accuracy were similar to those
described in recent studies (17,19). Due
to the lack of accurate baseline risk models for in-hospital
mortality or ICU stay of >3 days, the present study attempted to
adjust the model according to several common clinical criteria,
including age and comorbidities. In addition, the crude and
adjusted AUROC values of SOFA (0.860 and 0.940, respectively) were
slightly increased compared with other previous studies (14–17).
This may be due to the small and specific study population of the
present study or limitations of the study itself. Compared with
qSOFA and SIRS, SOFA exhibited a significantly higher sensitivity
and specificity. Although the complexity of SOFA scores may hinder
its utilization, it remains an accurate and efficient tool for
prognostic prediction within or outside the ICU and ED. The
sensitivity and specificity values of the SOFA score were
sufficient for the clinical application. In addition, no
significant difference in the effectiveness of SIRS and qSOFA
criteria to predict prognosis among patients with
urolithiasis-associated sepsis was observed.
The validity of SIRS criteria as a prognostic tool
has been widely challenged. In addition, its poor sensitivity as
diagnostic criteria has been criticized for a number of years. SIRS
criteria may unable to predict organ dysfunction with mortality in
ED patients with suspected infections (25). By contrast, the application of SIRS
criteria was associated with an increased 30-day mortality rate
among patients who had blood cultures performed from the ED
(26). However, the new definition
of Sepsis-3 has abandoned this calibration of SIRS criteria and
there is greater emphasis on scoring organ dysfunction (1). In the present study, the prognostic
accuracies between SIRS and qSOFA were equivalent. Although there
have been certain studies that compared the prognostic
effectiveness between SIRS and qSOFA, the results are controversial
and contradictory (14,15,17,27,28). It
is possible that neither are superior for predicting the prognosis
of patients with suspected sepsis.
The present study focused on prognoses in patients
with suspected urolithiasis-associated sepsis following surgical
interventions. Patients with suspected urosepsis but without
surgical interventions, such as emergency decompression for
obstructive urolithiasis, may exhibit significantly different
pathophysiology and outcome. In addition, based on evidence from an
American nationwide in-patient study, urgent decompression has been
directly associated with a decrease in mortality in patients with
sepsis and ureteral calculi (29).
In terms of surgery, a number of studies have reviewed the risk
factors for the occurrence of postoperative sepsis and mortality
following endourological treatment: Presence of kidney stones;
large stone burden; female sex; diabetes mellitus; renal
insufficiency; high pressure in the collecting system; and long
surgery times were identified to be risk factors for sepsis
following operation (9–11,30). Wu
et al (12) demonstrated an
association between the early marked decrease in WBC count and
uroseptic shock induced by upper urinary tract endoscopic
lithotripsy. However, there was no unified, widely accepted and
standardized criteria for predicting the prognosis of these
patients. Therefore, the prognostic accuracy of the generic
criteria for these specific patients was validated in the present
study. The results demonstrated that the SOFA score was a
preferable prognostic tool for patients with
urolithiasis-associated sepsis following surgical interventions.
Prognostic performances of SOFA were validated by a large
retrospective cohort analysis of adult patients with suspected
infection in Australia and New Zealand (15). Among 184,875 patients, SOFA exhibited
significantly greater prognostic accuracy for adverse outcome
(in-hospital mortality) compared with SIRS criteria or qSOFA
scores, with a crude AUROC value of 0.753 (15). However, in a second international
prospective cohort study, among patients admitted to the ED with
suspected infection, the use of qSOFA exhibited greater prognostic
accuracy for mortality (in-hospital) compared with Sepsis-1
criteria (SIRS and severe sepsis) (14). These results indicated that the
Sepsis-3 criteria (SOFA and qSOFA) should be recommended in the ED
setting. The results of the present study suggest that urologists
should consider the SOFA score of patients with
urolithiasis-associated sepsis when considering prognoses. The
prognostic performance of SOFA for in-hospital mortality or
prolonged ICU stay (>3 days) among patients with
urolithiasis-associated sepsis transferred to ICU following
surgical interventions was significantly increased compared with
those of qSOFA and SIRS.
The present study had a number of limitations.
Firstly, it was a single-center retrospective study with
unavoidable selection bias. In addition, due to the limited
clinical data, only the patients transferred to SICU following
surgical interventions were included in the analysis, in spite of
routine institutional (Xin Hua Hospital Affiliated to Shanghai Jiao
Tong University) regulations, which state that all patients with
suspected sepsis in surgical departments should be transferred to
SICU. The decision for transfer to SICU is generally made by the
primary surgeon of the patient or the senior on-duty surgeon, and
it may have been affected by previous experiences of the
clinicians. In addition, the diagnostic criteria of sepsis were
changed following the proposal of Sepsis-3, a new diagnostic
definition of sepsis, in 2016 (3).
In addition, different types of surgical interventions may lead to
different outcomes; therefore, the sample patient population was
not homogeneous. However, Sepsis-3 and SIRS criteria are generic
diagnostic and prognostic tools used for different types of sepsis,
derived from different systems. Therefore, the heterogeneity of
patients observed in the present study was considered to be
acceptable, however, it should be taken into consideration as it
may have affected the results. In addition, the study population
size was small; therefore, the outcome may be inaccurate and
affected by random error. To validate the results of the present
study, a multi-center prospective study is required.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was funded by Shanghai Municipal
Commission of Health and Family Planning Grant (grant no.
201440314), Shanghai Municipal Commission of Science and Technology
Grant (grant no. 17441905602), National Natural Science Fund for
Young Scholars (grant no. 81802522) and Shanghai Sailing Program
(grant no. 18YF1415200).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YH and JD supervised the project. JD designed the
study. BS, FS, KX, LS and JG collected the data. BS, HT, NW and YW
performed statistical analyses. YH performed surgical procedures.
BS, JD and FS wrote the manuscript. YW and JD corrected the
language of manuscript.
Ethics approval and consent to
participate
Written informed consent was provided by each
patient prior to surgery. The Ethics Committee of Xin Hua Hospital
Affiliated to Shanghai Jiao Tong University School of Medicine
approved the retrospective study and permitted the waiver of
written informed consent from patients (approval no.,
XHEC-D-2018-074). The study protocol was also in accordance with
the Declaration of Helsinki.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gotts JE and Matthay MA: Sepsis:
Pathophysiology and clinical management. BMJ. 353:i15852016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cohen J, Vincent JL, Adhikari NK, Machado
FR, Angus DC, Calandra T, Jaton K, Giulieri S, Delaloye J, Opal S,
et al: Sepsis: A roadmap for future research. Lancet Infect Dis.
15:581–614. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Singer M, Deutschman CS, Seymour CW,
Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche
JD, Coopersmith CM, et al: The third international consensus
definitions for sepsis and septic shock (Sepsis-3). JAMA.
315:801–810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shankar-Hari M, Phillips GS, Levy ML,
Seymour CW, Liu VX, Deutschman CS, Angus DC, Rubenfeld GD and
Singer M; Sepsis Definitions Task Force, : Developing a new
definition and assessing new clinical criteria for septic shock:
For the third international consensus definitions for sepsis and
septic shock (Sepsis-3). JAMA. 315:775–787. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Seymour CW, Liu VX, Iwashyna TJ,
Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM,
Shankar-Hari M, Singer M, et al: Assessment of clinical criteria
for sepsis: For the third international consensus definitions for
sepsis and septic shock (Sepsis-3). JAMA. 315:762–774. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dreger NM, Degener S, Ahmad-Nejad P,
Wöbker G and Roth S: Urosepsis-etiology, diagnosis and treatment.
Dtsch Arztebl Int. 112:837–848. 2015.PubMed/NCBI
|
|
7
|
Wagenlehner FM, Pilatz A, Weidner W and
Naber KG: Urosepsis: Overview of the diagnostic and treatment
challenges. Microbiol Spectr. 32015.doi:
10.1128/microbiolspec.UTI-0003-2012.
|
|
8
|
Wagenlehner FM, Lichtenstern C, Rolfes C,
Mayer K, Uhle F, Weidner W and Weigand MA: Diagnosis and management
for urosepsis. Int J Urol. 20:963–970. 2013.PubMed/NCBI
|
|
9
|
Michel MS, Trojan L and Rassweiler JJ:
Complications in percutaneous nephrolithotomy. Eur Urol.
51:899–906. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Koras O, Bozkurt IH, Yonguc T, Degirmenci
T, Arslan B, Gunlusoy B, Aydogdu O and Minareci S: Risk factors for
postoperative infectious complications following percutaneous
nephrolithotomy: A prospective clinical study. Urolithiasis.
43:55–60. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Çıtamak B, Altan M, Bozacı AC, Koni A,
Doğan HS, Bilen CY, Şahin A and Tekgül S: Percutaneous
nephrolithotomy in children: 17 Years of experience. J Urol.
195:1082–1087. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wu H, Zhu S, Yu S, Ding G, Xu J, Li T,
Qiao L, Chen Y, Yan J, Cheng X, et al: Early drastic decrease in
white blood count can predict uroseptic shock induced by upper
urinary tract endoscopic lithotripsy: A translational study. J
Urol. 193:2116–2122. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hu M, Zhong X, Cui X, Xu X, Zhang Z, Guan
L, Feng Q, Huang Y and Hu W: Development and validation of a
risk-prediction nomogram for patients with ureteral calculi
associated with urosepsis: A retrospective analysis. PLoS One.
13:e02015152018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Freund Y, Lemachatti N, Krastinova E, Van
Laer M, Claessens YE, Avondo A, Occelli C, Feral-Pierssens AL,
Truchot J, Ortega M, et al: Prognostic accuracy of sepsis-3
criteria for in-hospital mortality among patients with suspected
infection presenting to the emergency department. JAMA.
317:301–308. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Raith EP, Udy AA, Bailey M, McGloughlin S,
MacIsaac C, Bellomo R and Pilcher DV: Australian and New Zealand
Intensive Care Society (ANZICS) Centre for Outcomes and Resource
Evaluation (CORE): Prognostic accuracy of the SOFA score, SIRS
criteria and qSOFA score for in-hospital mortality among adults
with suspected infection admitted to the intensive care unit. JAMA.
317:290–300. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tokioka F, Okamoto H, Yamazaki A, Itou A
and Ishida T: The prognostic performance of qSOFA for
community-acquired pneumonia. J Intensive Care. 6:462018.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Singer AJ, Ng J, Thode HC Jr, Spiegel R
and Weingart S: Quick SOFA scores predict mortality in adult
emergency department patients with and without suspected infection.
Ann Emerg Med. 69:475–479. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Park HK, Kim WY, Kim MC, Jung W and Ko BS:
Quick sequential organ failure assessment compared to systemic
inflammatory response syndrome for predicting sepsis in emergency
department. J Crit Care. 42:12–17. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Williams JM, Greenslade JH, McKenzie JV,
Chu K, Brown AFT and Lipman J: Systemic inflammatory response
syndrome, quick sequential organ function assessment, and organ
dysfunction: Insights from a prospective database of ED patients
with infection. Chest. 151:586–596. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Luo X, Yang X, Li J, Zou G, Lin Y, Qing G,
Yang R, Yao W and Ye X: The procalcitonin/albumin ratio as an early
diagnostic predictor in discriminating urosepsis from patients with
febrile urinary tract infection. Medicine (Baltimore).
97:e110782018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wu H, Wang Z, Zhu S, Rao D, Hu L, Qiao L,
Chen Y, Yan J, Chen X, Wan SP, et al: Uroseptic shock can be
reversed by early intervention based on leukocyte count 2 h
post-operation: Animal model and multicenter clinical cohort study.
Inflammation. 41:1835–1841. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wagenlehner FM, Tandogdu Z and Bjerklund
Johansen TE: An update on classification and management of
urosepsis. Curr Opin Urol. 27:133–137. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Türk C, Petřík A, Sarica K, Seitz C,
Skolarikos A, Straub M and Knoll T: EAU guidelines on
interventional treatment for urolithiasis. Eur Urol. 69:475–482.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rhodes A, Evans LE, Alhazzani W, Levy MM,
Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally
ME, et al: Surviving sepsis campaign: International guidelines for
management of sepsis and septic shock: 2016. Crit Care Med.
45:486–552. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shapiro N, Howell MD, Bates DW, Angus DC,
Ngo L and Talmor D: The association of sepsis syndrome and organ
dysfunction with mortality in emergency department patients with
suspected infection. Ann Emerg Med. 48:583–590.e1. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lindvig KP, Nielsen SL, Henriksen DP,
Jensen TG, Kolmos HJ, Pedersen C, Vinholt PJ and Lassen AT:
Mortality and prognostic factors of patients who have blood
cultures performed in the emergency department: A cohort study. Eur
J Emerg Med. 23:166–172. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Finkelsztein EJ, Jones DS, Ma KC, Pabón
MA, Delgado T, Nakahira K, Arbo JE, Berlin DA, Schenck EJ, Choi AM
and Siempos II: Comparison of qSOFA and SIRS for predicting adverse
outcomes of patients with suspicion of sepsis outside the intensive
care unit. Crit Care. 21:732017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ho KM and Lan NS: Combining quick
sequential organ failure assessment with plasma lactate
concentration is comparable to standard sequential organ failure
assessment score in predicting mortality of patients with and
without suspected infection. J Crit Care. 38:1–5. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Borofsky MS, Walter D, Shah O, Goldfarb
DS, Mues AC and Makarov DV: Surgical decompression is associated
with decreased mortality in patients with sepsis and ureteral
calculi. J Urol. 189:946–951. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
de la Rosette J, Denstedt J, Geavlete P,
Keeley F, Matsuda T, Pearle M, Preminger G and Traxer O; CROES URS
Study Group, : The clinical research office of the endourological
society ureteroscopy global study: Indications, complications, and
outcomes in 11,885 patients. J Endourol. 28:131–139. 2014.
View Article : Google Scholar : PubMed/NCBI
|