Introduction
Atherosclerosis is a common and complex chronic
inflammatory disease of the vascular wall associated with lipid
deposition and plaque fibrosis (1–3).
Clinically, atherosclerosis is characterized by a marked
dysfunction in lipid homeostasis, slow metabolism and retardation
of signaling pathways that regulate the inflammatory response
(4). Recently, morbidity of patients
with atherosclerotic is increased significantly (5–7). A
number of factors can trigger and sustain atherosclerosis,
including smoke, obesity, arterial hypertension, dyslipidemia and
diabetes mellitus (8). Ultimately,
inflammation plays an important role in the pathogenesis of
atherosclerosis, which has been recognized and confirmed at the
molecular level in numerous animal models (9). In addition, endothelial cell injury in
vascular arterial walls caused by inflammation frequently leads to
the increased risk of atherosclerosis due to pathological changes
and deposition of cholesterol (10).
It is therefore crucial to investigate the association between
inflammation and endothelial cell injury in atherosclerosis.
Pterostilbene
(trans−3,5-dimethoxy-4-hydroxystilbene; Pts), a dimethylated
analog of resveratrol, has been recognized to possess protective
properties against inflammation and various diseases, such as heart
reperfusion injury and atherosclerosis (11–13). Pts
presents antioxidative and anti-apoptotic efficacy in numerous
types of diseases via regulation of intracellular metabolism
(14). Evidence suggests that Pts
plays a role in suppressing the inflammatory response via NF-κB
inactivation in lipopolysaccharide (LPS) or tumor necrosis factor-α
(TNF-α)-induced vascular smooth muscle cells by downregulation of
Toll like receptor 5 expression (13). Data indicate that Pts inhibits smooth
muscle cell migration via the mitogen-activated protein kinase /
matrix metallopeptidase-2 pathway and plays a novel role in the
treatment of atherosclerosis (15).
Pts has also been reported to have anti-inflammatory activity
through the suppression of Akt kinase (16). An additional study suggested that the
pro-atherogenic effect of nuclear factor erythroid 2-related factor
2 (Nrf-2) signaling was primarily mediated by its permissive role
in interleukin (IL)-1 production in the chronic vascular
inflammation that drives atherosclerosis (17). Nrf-2 is known to be a pro-atherogenic
protein in mice, which may be mediated via positive regulation of
CD36 and is a potential targeted therapy for cardiovascular
diseases (18). However, the
association between Pts and Nrf-2 in endothelial cells in vascular
arterial walls has not been clarified.
The purpose of the present study was to explore the
anti-inflammatory activity, and antioxidative and anti-apoptotic
efficacy of Pts in endothelial cells in vascular arterial walls in
an atherosclerosis rat model. The Pts-Nrf2-5′ adenosine
monophosphate activated protein kinase (AMPK) / signal transducer
and activator of transcription 3 (STAT3) signaling pathway was
analyzed in endothelial cells in vascular arterial walls. The
results explained the protective effects of Pts against apoptosis
of endothelial cells in vascular arterial walls, and provided
insight into its potential mechanism and use as an
anti-atherosclerosis treatment.
Materials and methods
Animal study
A total of 24 male Sprague-Dawley rats (age, 8
weeks; weight, 320–350 g) were purchased from Experimental Animal
Center of Shandong University. All rats were kept under 12-h
light-dark cycles at (23±1)°C and (50±5)% humidity, and had free
access to food and water. An atherosclerotic rat model was
established through endothelial injury of the iliac arteries and
feeding with a 2.5% cholesterol diet with 1% glucose
(Sigma-Aldrich, Merck KGaA) for 6 weeks as described previously
(19). The rats were randomly
divided into two experimental groups: i) The control group that
received PBS treatment orally and ii) the experimental group that
orally received Pts (≥99%, purity; 10 mg/kg/day; Great Forest
Biomedical, Ltd.) treatment with a regular diet for 4 weeks. Rats
were sacrificed using cervical dislocation after the 4-week
treatment and an anesthetic (40 mg/kg intravenous pentobarbital;
Sigma-Aldrich; Merck KGaA) was used prior to euthanasia.
Evaluation of inflammatory cytokines
in serum
Peripheral venous blood samples were collected from
experimental rats and serum samples were obtained after
centrifugation at 10,000 × g for 5 min at 4°C and analyzed for
biochemical measurements. The concentrations of monocyte
chemoattractant protein-1 (MCP-1; cat. no. RJE00B), Il-6 (cat. no.
R6000B), IL-1β (cat. no. RLB00) and TNF-α (cat. no. RTA00) were
determined using enzyme linked immunosorbent assay (ELISA) kits
according to the manufacturer's instructions (R&D Systems,
Inc.).
Histopathological and
histomorphometric evaluation of aortic arch
Rats were sacrificed using cervical dislocation on
week 5 as described above. The aortic arch samples (the remaining
samples were stored at −80°C for subsequent use) obtained were
fixed in 10% paraformaldehyde for 12 h at 4°C, washed with PBS,
embed in paraffin, cut into 5-µm thick sections and subjected to
antigen retrieval using eBioscience™ IHC Antigen Retrieval Solution
(cat. no. 00-4955-58, Invitrogen, Thermo Fisher Scientific, Inc.).
Thick longitudinal sections (5-µm) were stained with hematoxylin
and eosin for 15 min at room temperature and images captured under
a light microscope at ×40 magnification. The histopathological and
histomorphometric images were evaluated by three independent
pathologists.
Quantification of atherosclerotic
lesion size
Quantification of lesion size was determined as
described previously (20). Briefly,
tissues were frozen, stored at −80°C, cut at 8-µm intervals and
stained with hematoxylin and 0.5% Oil Red O (Sigma-Aldrich; Merck
KGaA) for 1 h at room temperature. Atherosclerotic lesion area was
quantified using Image-Pro Plus software version 5.0 (Media
Cybernetics).
Cell culture
Human umbilical artery endothelial cells were
purchased from Clonetics Lonza (cat. no. 199041; Lonza Group Ltd.)
and cultured in endothelial growth medium (EGM-2; Lonza Group Ltd.)
in 5% CO2 at 37°C. After a 24-h incubation, cells were
incubated with 0, 0.5, 1.0, 1.5, 2.0, 2.5 and 3.0 mg/ml of Pts for
12 h at 37°C for further analysis.
Cell viability assay
Viability of endothelial cells was measured using
the Cell Counting Kit-8 (CCK-8; Sigma-Aldrich, Merck KGaA). In
brief, endothelial cells were seeded into 6-well plates at a
density of 1×105 cells/ml and incubated with 0.2%
hydrogen peroxide (H2O2) and then treated
with PBS or Pts (2 mg/ml) for 24 h at 37°C. A total of 10 µl of
CCK-8 solution was added to the cells and incubated for 30 min at
37°C. Absorbance at 450 nm was measured using a Microplate Reader
(Bio-Rad Laboratories, Inc.).
Measurement of levels of nitric oxide
(NO) and reactive oxygen species (ROS)
Endothelial cells (1×105/well) were
seeded into a 6-well plate and incubated with 0.2%
H2O2 to induce oxidative stress and then
treated with PBS or Pts (2 mg/ml) at 37°C for 24 h. Endothelial
cells were harvested and centrifuged at 2,000 × g for 10 min at
4°C. Endothelial cells were collected and lysed with RIPA buffer
(Beyotime Institute of Biotechnology) for subsequent analysis of
enzyme activities. The level of NO was assessed using a commercial
Nitrate/Nitrite Fluorometric Assay kit (cat. no. KA1344; Abnova)
following the manufacturer's protocols. Intracellular ROS
production was analyzed using fluorescent probe DCFH-DA (cat. no.
D6883; Sigma-Aldrich, Merck KGaA) as described previously (21).
Small interfering (si-)RNA-mediated
knockdown
Endothelial cells (1×105/well) were
seeded into a 6-well plate. After 24 h, cells were transfected with
siRNA-Nrf2 (si-Nrf2) forward, 5′-GAGACUACCAUGGUUCCAA(dTdT)-3′ and
reverse, 5′-UUGGAACCAUGGUAGUCUC(dTdT)-3′ or si-RNA control (si-NC)
forward, 5′-CCUACGCCACCAAUUUCGU-3′ and reverse,
5′-ACGAAAUUGGUGGCGUAGG-3′ (Invitrogen, Thermo Fisher Scientific
Ltd.) using Lipofectamine® RNAiMAX (2 µl; cat. no.
13778030; Invitrogen; Thermo Fisher Scientific, Inc.) according to
the manufacturer's instructions (Thermo Fisher Scientific, Inc.).
mRNA expression of Nrf2 was detected by western blot analysis 72-h
after transfection. si-Nrf2-transfected cells were then treated
with PBS or Pts (2 mg/ml) for 24 h at 37°C for further
analysis.
Western blot analysis
A total of 1×107 endothelial cells were
lysed in RIPA buffer (Bio-Rad Laboratories, Inc.). The lysates were
centrifuged at 12,000 × g for 10 min at 4°C. The protein
concentration was quantified using a BCA Protein Assay kit (Pierce,
Thermo Fisher, Ltd.). Protein samples (40 µg) were loaded onto an
SDS-PAGE (12% gel) and transferred onto polyvinylidene difluoride
membranes (Sigma-Aldrich; Merck KGaA). Membranes were blocked with
5% bovine serum albumin (BSA; Sigma-Aldrich; Merck KGaA) and
incubated with the following primary antibodies: Superoxide
dismutase (SOD; 1:1,000; cat. no. ab13534), catalase (CAT; 1:1,000,
cat. no. ab16731), heme oxygenase-1 (HO-1; 1:1,000, cat. no.
ab13243), Nrf2 (1:1,000; cat. no. ab62352), AMPK (1:1,000; cat. no.
ab32047), phosphorylated (p)AMPK (1:1,000; cat. no. ab92701,
Abcam), STAT3 (1:1,000; cat. no. ab68153), pSTAT3 (1:1,000; cat.
no. ab76315) and β-actin (1:1,000; cat. no. ab8226) for 12 h at
4°C. All antibodies were supplied by Abcam. After washing with PBS,
membranes were incubated with HRP-conjugated secondary antibody
(1:2,000; cat. no. ab205718; Abcam) for 2 h at room temperature.
The bands were visualized using an enhanced chemiluminescence
substrate kit (Beyotime Institute of Biotechnology; cat. no.
P0018F). Protein expression was quantified using ImageJ software
(version 4.6.2; National Institutes of Health).
Apoptosis assay
The apoptosis of cells was analyzed using a TUNEL
staining kit (Roche Diagnostics). For tissue, sections were stained
with TUNEL for 2 h at room temperature and analyzed using a
commercial TUNEL staining kit (Roche Diagnostics) according to the
manufacturer's instructions. For cells, 1×104
endothelial cells were fixed with 4% paraformaldehyde and 0.5%
Triton X-100 for 30 min at room temperature, and then incubated
TUNEL for 2 h at room temperature. Cells were washed with PBS three
times and then incubated with 5% DAPI (Sigma-Aldrich; Merck KGaA)
for 30 min at room temperature. Images were captured at ×100
magnification under Aqueous mounting medium (cat. no. ab64230;
Abcam) using a ZEISS LSM 510 confocal microscope with a 488 nm
laser. The apoptosis rate was measured using Developer XD 3.0
(Definiens AG) software version 1.0. Six fields of view were
randomly assessed for each treatment group.
Statistical analysis
All data are expressed as the mean ± SEM.
Statistical analysis was conducted with Student's t-test or one-way
ANOVA followed by Tukey's test using SPSS software (version 17.0;
SPSS, Inc.). P<0.05 was considered to indicate a statistically
significant difference.
Results
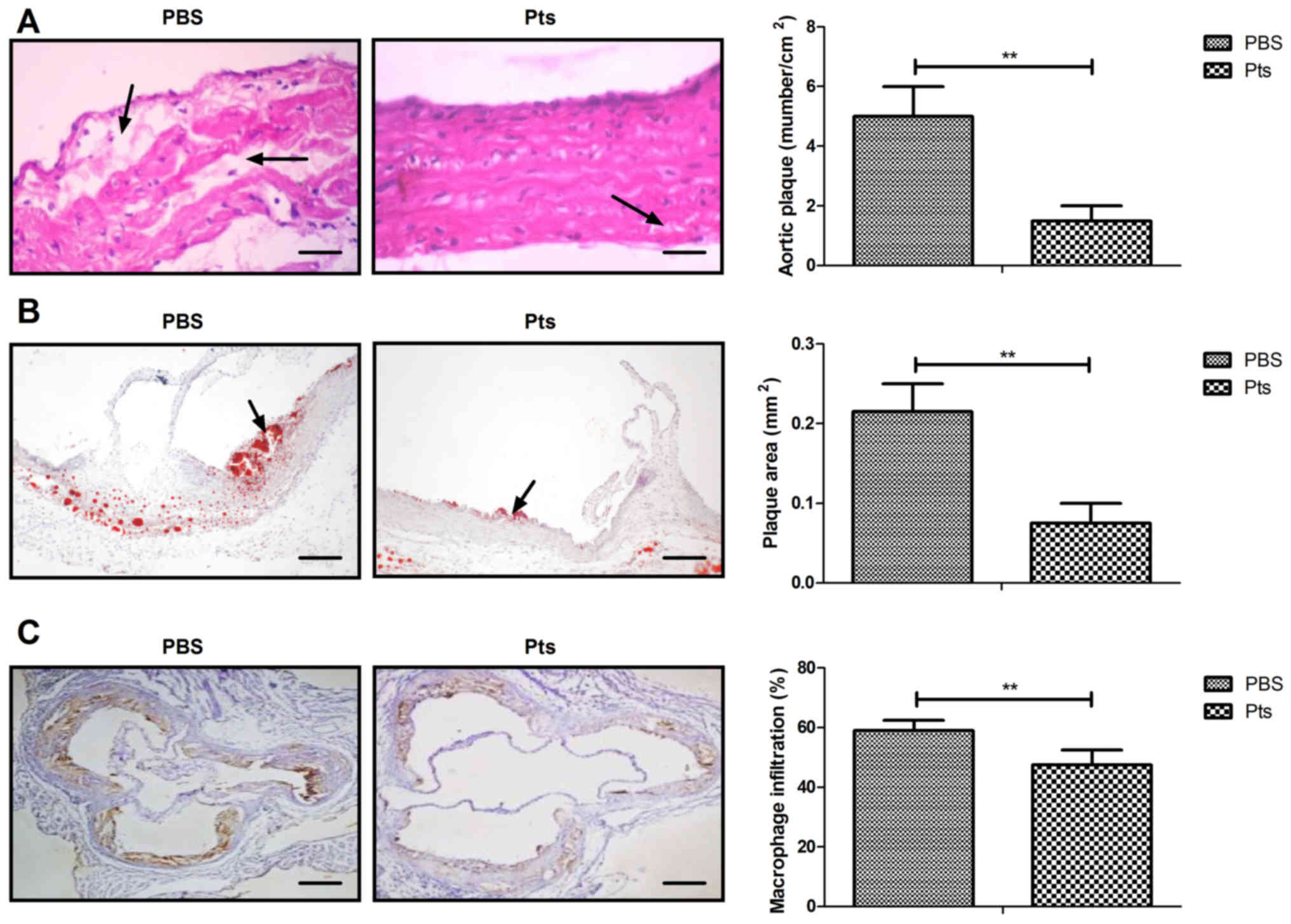
Pts improves symptoms of
atherosclerosis in a rat atherosclerosis model
Symptoms of atherosclerosis were recorded in rats of
both the Pts and PBS group. The results showed that Pts
administration attenuated atherogenesis when compared with control
(Fig. 1A). Administration of Pts
reduced the area of aortic plaques and macrophage infiltration in
the atherosclerotic rat model (Fig. 1B
and C). Pts administration suppressed apoptosis of the vascular
arterial wall in an atherosclerosis rat model (Fig. 1D).
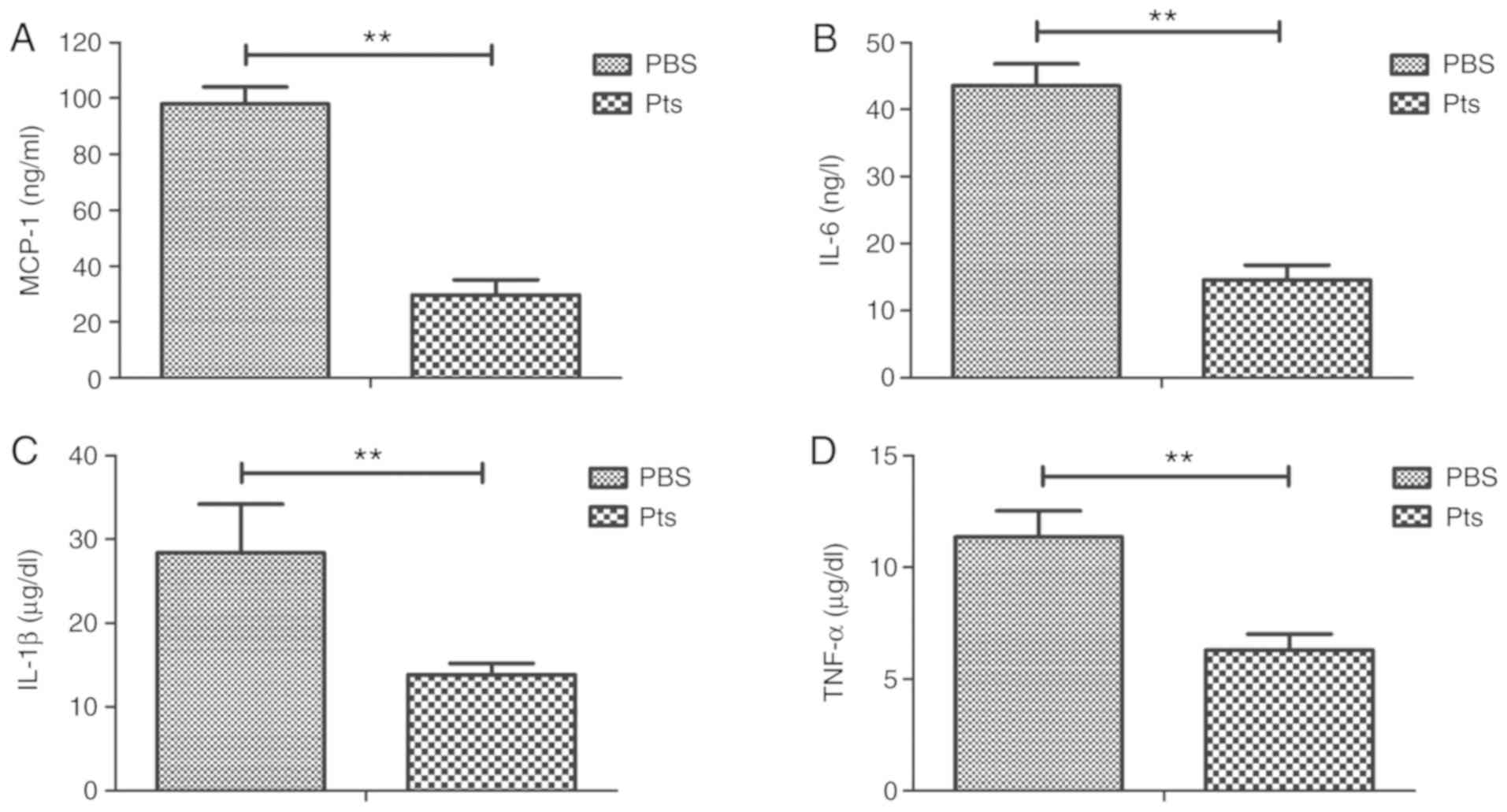
Pts suppresses the inflammatory
response in an atherosclerosis rat model
Inflammatory cytokines play a crucial role in
regulating the inflammatory response in atherosclerosis. Serum
levels of inflammatory cytokines including MCP-1, IL-6, IL-1β and
TNF-α were examined to determine whether Pts could regulate their
expression. In vivo results showed that Pts administration
corresponded with decreased serum levels of MCP-1, IL-6, IL-1β and
TNF-α (Fig. 2A-D).
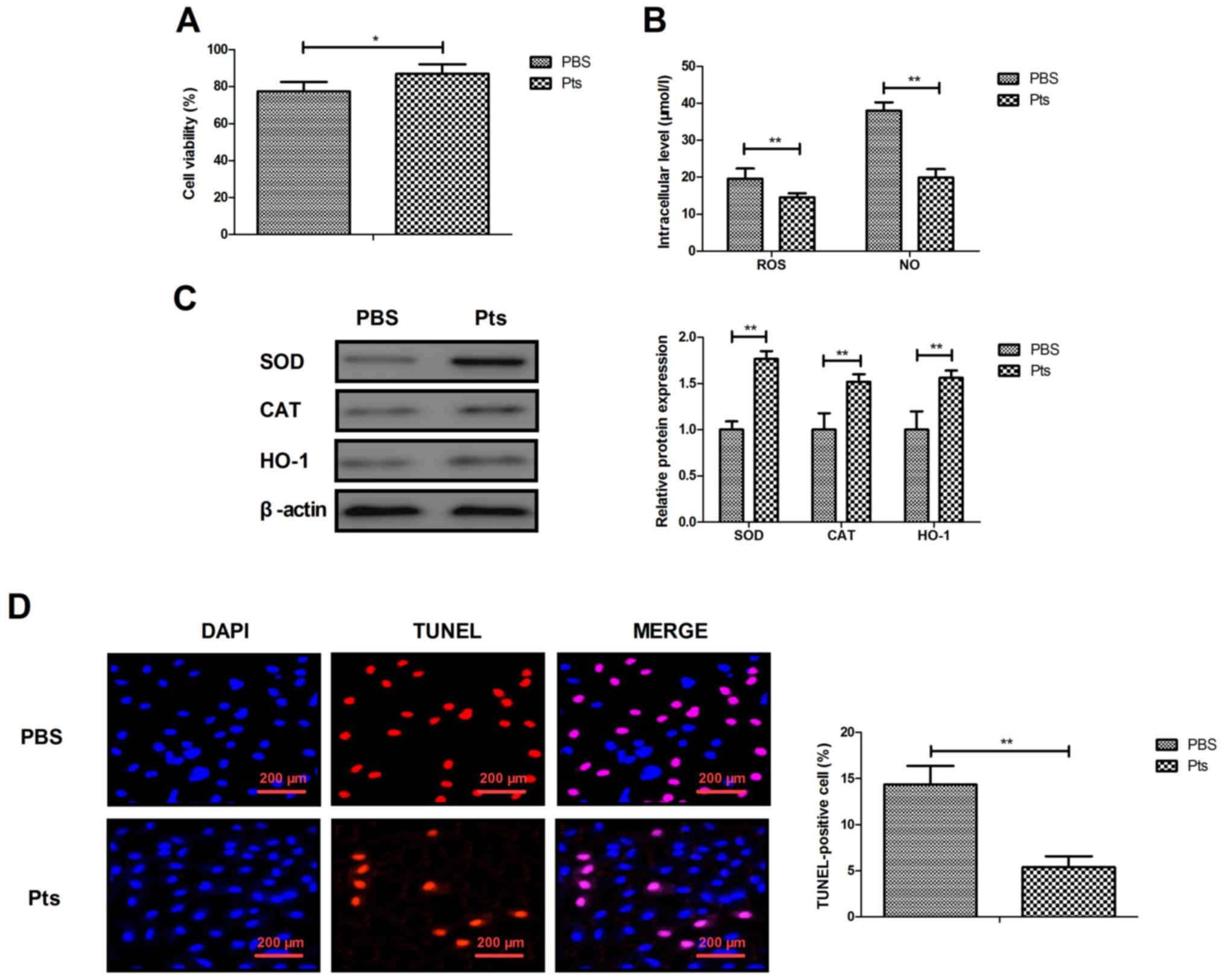
Pts decreases
H2O2-induced cytotoxicity in cultured
endothelial cells
The protective effects of Pts on endothelial cells
were investigated in vitro. The dose of 2.0 mg/ml Pts showed
the optimal protective effect on H2O2-induced
cytotoxicity in endothelial cells (Fig.
S1). The results showed that Pts administration decreased
H2O2-induced cytotoxicity compared with the
PBS group (Fig. 3A). Oxidative
stress injury-associated ROS production and NO generation was
reduced by Pts, and the expression levels of antioxidant proteins
SOD, CAT and HO-1 were upregulated by Pts in these endothelial
cells (Fig. 3B and C). Apoptosis of
endothelial cells was reduced after Pts treatment when compared
with control (Fig. 3D).
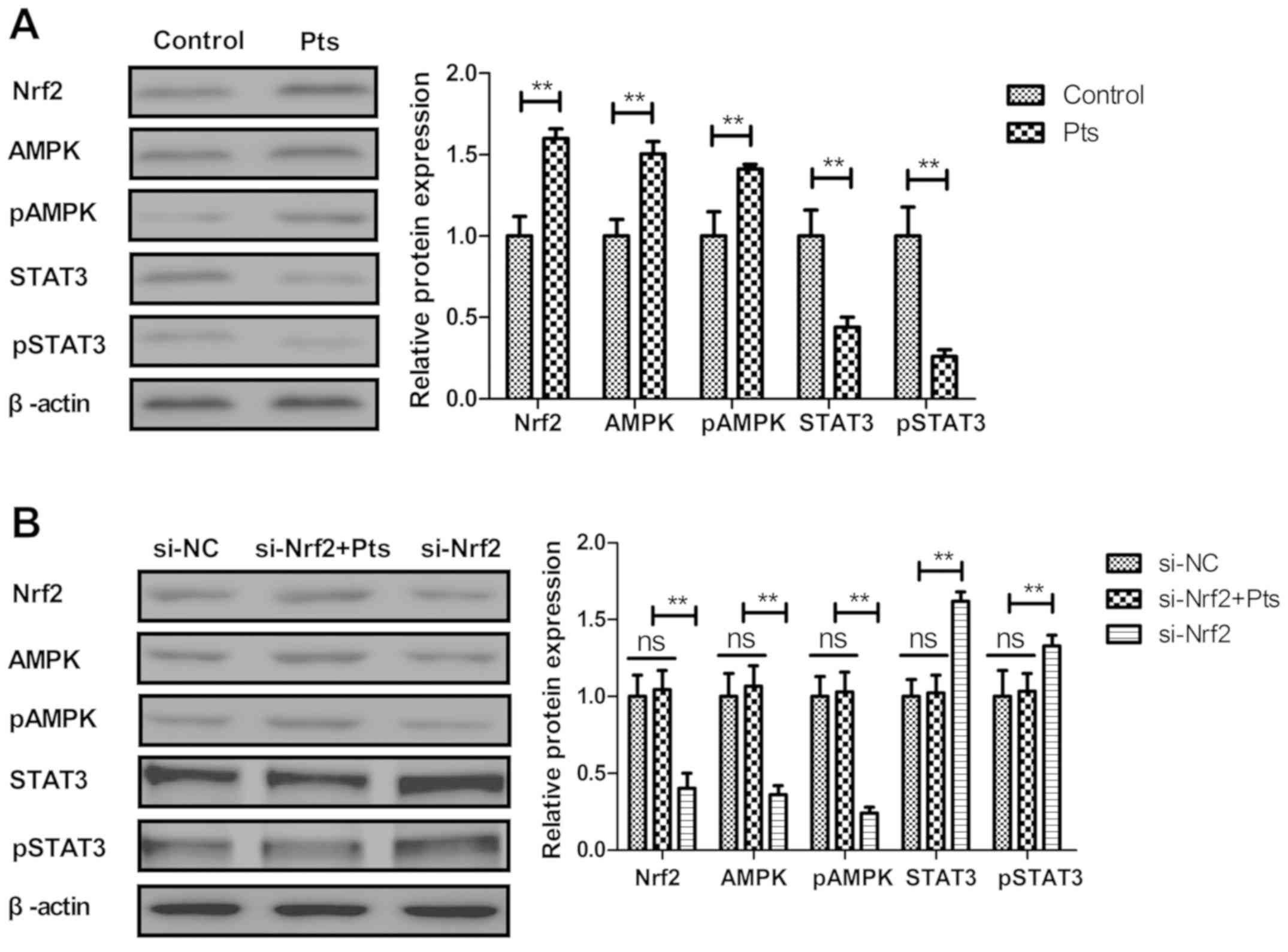
Pts inhibits the Nrf2-mediated
AMPK/STAT3 pathway in cultured endothelial cells
The Nrf2-mediated AMPK/STAT3 pathway was analyzed in
cultured endothelial cells. Pts administration increased Nrf2,
STAT3 and AMPK expression in endothelial cells (Fig. 4A). Knockdown of Nrf2 (si-Nrf2)
abolished Pts-regulated AMPK and pAMPK and increased STAT3 and
pSTAT3 levels in endothelial cells (Fig.
4B). The results revealed that knockdown of Nrf2 increased Nrf2
expression and increased the ratio of p-Nrf2/t-Nrf2 in endothelial
cells (Fig. S2).
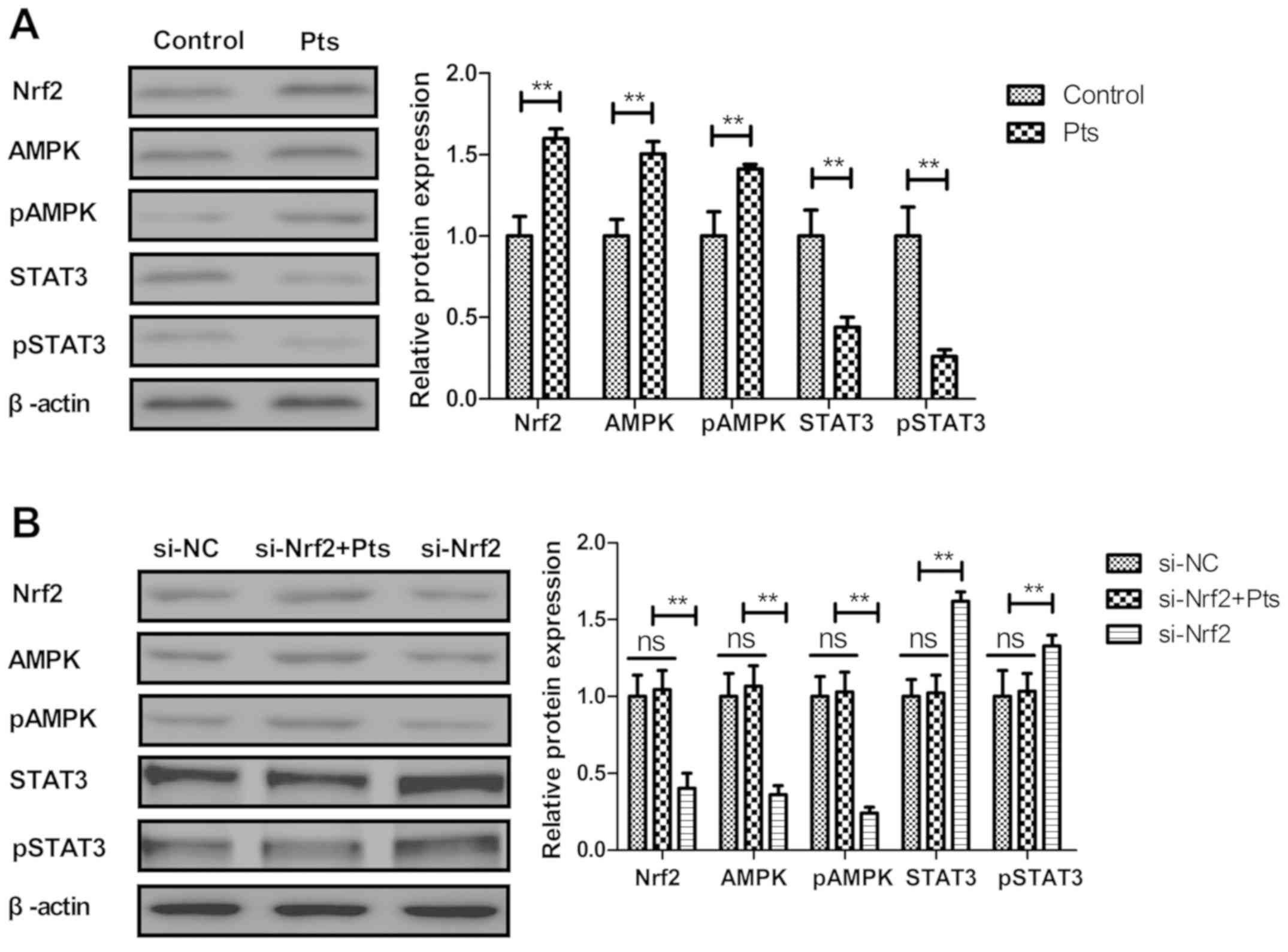 | Figure 4.Pts inhibits the Nrf2-mediated
AMPK/STAT3 pathway in endothelial cells. (A) Effect of Pts on Nrf2,
AMPK, pAMPK, STAT3 and pSTAT3 levels in endothelial cells. (B)
Effects of Nrf2 knockdown on Pts-regulated AMPK, pAMPK, STAT3 and
pSTAT3 levels in endothelial cells. **P<0.01. AMPK, 5′ adenosine
monophosphate-activated protein kinase; Nrf2, nuclear factor
erythroid 2-related factor 2; p, phosphorylated; Pts,
pterostilbene; STAT3, signal transducer and activator of
transcription 3; ns, not significant; NC, negative control; si,
small interfering RNA. |
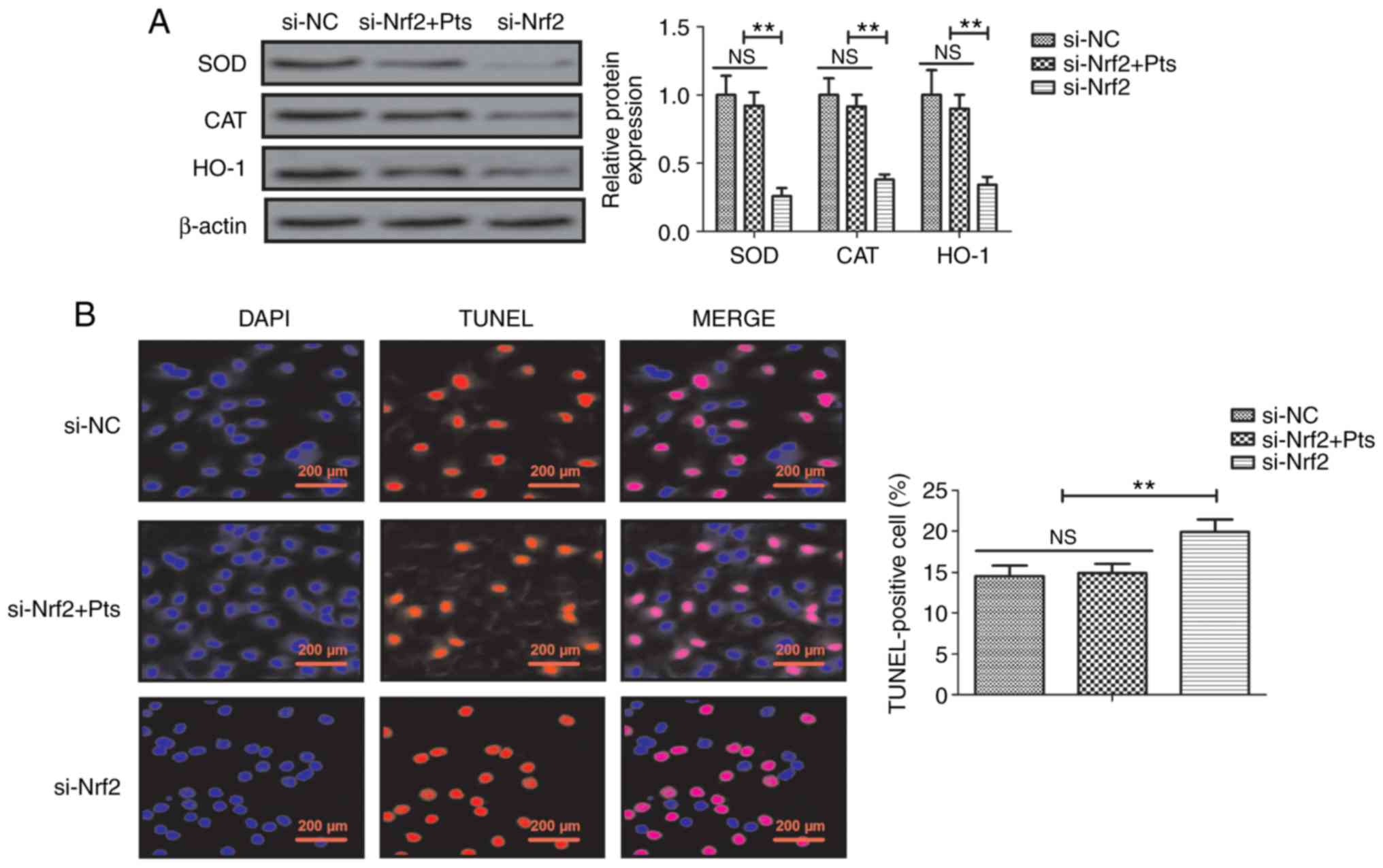
Knockdown of Nrf2 reduces
Pts-regulated oxidative stress prevention of injury and apoptosis
in endothelial cells
The role of Nrf2 knockdown was further investigated
in Pts-regulated oxidative stress injury and apoptosis in
endothelial cells. The results demonstrated that si-Nrf2 decreased
SOD, CAT and HO-1 protein expression compared with si-NC and that
there was no significant difference between si-NC and si-Nrf2+ Pts
group in endothelial cells (Fig.
5A). Similarly, knockdown of Nrf2 increased apoptosis of
endothelial cells and reduced Pts-induced prevention of apoptosis
in endothelial cells when compared with the si-NC group (Fig. 5B).
Discussion
Pts is a stilbene belonging to a family of
polyphenols reported to have anti-inflammatory effects in
fructose-fed diabetic and acute renal ischemia reperfusion injury
rats (14,22). Previously, Nrf2 was reported to play
a pivotal role in inflammasome activation and oxidative stress
(18). An additional study reported
that Pts ameliorated streptozotocin-induced diabetes through
enhancement of antioxidant signaling pathways mediated by Nrf2
(23). Notably, Pts was shown to
inhibit high fat-induced atherosclerosis inflammation via
regulation of the NF-κB signaling pathway in experimental mice
(13). The current study aimed to
clarify the therapeutic mechanism of Pts action on endothelial
cells in the atherosclerotic rat. The results revealed that Pts
administration attenuated atherogenesis, aortic plaque formation,
macrophage infiltration, oxidative stress and apoptosis of vascular
arterial walls in an atherosclerosis rat model. Data suggested that
Pts decreased oxidative stress and inhibited apoptosis via an
Nrf2-mediated AMPK/STAT3 signaling pathway in endothelial cells,
which ameliorated atherosclerosis.
Inflammation plays a key role in the pathogenesis of
atherosclerosis and has gained considerable attention in clinical
practice (24). MCP-1 is expressed
by endothelial cells and has been reported to play an important
role in the pathogenesis of atherosclerosis and to influence cell
growth within the atherosclerotic lesion (25). In the current study Pts reduced the
serum level of MCP-1 in a rat model of atherosclerosis. Release of
the pro-inflammatory cytokine IL-6 affects the histological
features of plaque composition (26). In addition, studies have found that
proinflammatory IL-1 family cytokine production was increased in
atherosclerosis patients due to a reduction in wall shear stress
(27). Further findings suggested
that TNF-inhibitory intervention should be added to conventional
therapy as a novel strategy for treating the elderly patients with
atherosclerosis (28). In the
current study Pts administration effectively decreased serum levels
of IL-6, IL-1β and TNF-α, indicating that Pts may reduce the
apoptosis of endothelial cells by modulating the expression of
inflammatory cytokines.
Antioxidative and anti-inflammatory efficacy
contributes to Pts anti-atherosclerosis activity and it has been
confirmed to regulate endothelial function in a rat model (29). In addition, the excessive release of
ROS leads to enhanced lipid peroxidation, aggravated
atherosclerosis and oxidative stress (30). Furthermore, SOD has potential
beneficial effects with respect to the development of
atherosclerosis (31). A reduction
in NO generation leads to an improvement in LPS-induced apoptosis
in RAW 264.7 macrophages (32).
Previous studies have also found that atherosclerosis is a chronic
inflammatory cardiovascular disease and is characterized by an
increased ROS and NO production in arterial endothelial cells
(30,33). In the current study the efficacy of
Pts was reported in preventing oxidative stress injury. In
addition, Pts treatment decreased ROS and NO production in
endothelial cells, which further improved the endothelium function
and may be regarded as a therapeutic drug for the treatment of
atherosclerosis. These findings may be attributed to the
antioxidative efficacy of Pts, due to Nrf2-mediated signal
transduction in endothelial cells.
Nrf2 is essential for cholesterol crystal-induced
inflammasome activation and exacerbation of atherosclerosis
(17). Nrf2-mediated pathways are
associated with antioxidant defense in atherosclerosis (34). AMPK-dependent phosphorylation of
sterol regulatory element-binding protein may offer therapeutic
strategies to atherosclerosis (35–37).
Furthermore, inhibition of STAT3 activation may be a potential
therapeutic target in the treatment of atherosclerosis (38). In the current study, in vivo
assays revealed that Pts treatment attenuated atherogenesis,
reduced the number and area of aortic plaques and macrophage
infiltration, and suppressed oxidative stress and apoptosis of
vascular arterial walls in atherosclerosis rat model. In
vitro assays showed that Pts regulated oxidative stress injury
and apoptosis via Nrf2-mediated AMPK/STAT3 pathway in endothelial
cells.
In conclusion, the key findings of the current study
are that Pts may be an efficient drug in endothelial cells in the
pathology of atherosclerosis. The results indicated that the
protective effects of Pts may be associated with the regulation of
Nrf2-mediated AMPK/STAT3 pathway, which provides a potential novel
anti-atherosclerosis agent for patients.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by the Foundation of
Jiangsu Provincial Commission of Health and Family Planning (grant
no. QNRC2016353), and the National Key Research and Develeopment
Program of China (grant no. 2016YFE0126000).
Availability of data and materials
The datasets used and/or analyzed during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
TT designed and conceived the current study, and
provided intellecutal content. ZD performed statistical analysis
and wrote/revised the manuscript. JX collected and analyzed the
data, prepared the figures and revised the manuscript. JL and SZ
established the rat model and revised the manuscript. XZ and HZ
performed the literature search and generated the rat model. YW
collected the data and approved the final manuscript for
publication.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Yangzhou University.
Patient consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Okuyama H, Hamazaki T, Hama R, Ogushi Y,
Kobayashi T, Ohara N and Uchino H: A critical review of the
consensus statement from the European Atherosclerosis Society
Consensus Panel 2017. Pharmacology. 101:184–218. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Henrot P, Foret J, Barnetche T, Lazaro E,
Duffau P, Seneschal J, Schaeverbeke T, Truchetet ME and Richez C:
Assessment of subclinical atherosclerosis in systemic lupus
erythematosus: A systematic review and meta-analysis. Joint Bone
Spine. 85:155–163. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Martins P, Castela E, Rocha G, Sena C and
Seiça R: Premature atherosclerosis in HIV-infected pediatric
patients: Literature review and clinical approach. Acta Med Port.
30:742–749. 2017.(In Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhao TX and Mallat Z: Targeting the immune
system in atherosclerosis: JACC State-of-the-art review. J Am Coll
Cardiol. 73:1691–1706. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Parolin M, Dassie F, Martini C, Mioni R,
Russo L, Fallo F, Rossato M, Vettor R, Maffei P and Pagano C:
Preclinical markers of atherosclerosis in acromegaly: A systematic
review and meta-analysis. Pituitary. 21:653–662. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Song P, Xia W, Zhu Y, Wang M, Chang X, Jin
S, Wang J and An L: Prevalence of carotid atherosclerosis and
carotid plaque in Chinese adults: A systematic review and
meta-regression analysis. Atherosclerosis. 276:67–73. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stachyra K, Kiepura A and Olszanecki R:
Air pollution and atherosclerosis - a brief review of mechanistic
links between atherogenesis and biological actions of inorganic
part of particulate matter. Folia Med Cracov. 57:37–46.
2017.PubMed/NCBI
|
|
8
|
Fava C and Montagnana M: Atherosclerosis
is an inflammatory disease which lacks a common anti-inflammatory
therapy: How human genetics can help to this issue. A narrative
review. Front Pharmacol. 9:552018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hartman J and Frishman WH: Inflammation
and atherosclerosis: A review of the role of interleukin-6 in the
development of atherosclerosis and the potential for targeted drug
therapy. Cardiol Rev. 22:147–151. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Patel TN, Shishehbor MH and Bhatt DL: A
review of high-dose statin therapy: Targeting cholesterol and
inflammation in atherosclerosis. Eur Heart J. 28:664–672. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang W, Ding XQ, Gu TT, Song L, Li JM, Xue
QC and Kong LD: Pterostilbene and allopurinol reduce
fructose-induced podocyte oxidative stress and inflammation via
microRNA-377. Free Radic Biol Med. 83:214–226. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lv M, Liu K, Fu S, Li Z and Yu X:
Pterostilbene attenuates the inflammatory reaction induced by
ischemia/reperfusion in rat heart. Mole Med Rep. 11:724–728. 2015.
View Article : Google Scholar
|
|
13
|
Zhang Y: Pterostilbene, a novel natural
plant conduct, inhibits high fat-induced atherosclerosis
inflammation via NF-kappaB signaling pathway in Toll-like receptor
5 (TLR5) deficient mice. Biomed Pharmacother. 81:345–355. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gao D, Jing S, Zhang Q and Wu G:
Pterostilbene protects against acute renal ischemia reperfusion
injury and inhibits oxidative stress, inducible nitric oxide
synthase expression and inflammation in rats via the Toll-like
receptor 4/nuclear factor-κB signaling pathway. Exp Ther Med.
15:1029–1035. 2018.PubMed/NCBI
|
|
15
|
Lin HC, Hsieh MJ, Peng CH, Yang SF and
Huang CN: Pterostilbene inhibits vascular smooth muscle cells
migration and matrix metalloproteinase-2 through modulation of MAPK
pathway. J Food Sci. 80:H2331–H2335. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Park ES, Lim Y, Hong JT, Yoo HS, Lee CK,
Pyo MY and Yun YP: Pterostilbene, a natural dimethylated analog of
resveratrol, inhibits rat aortic vascular smooth muscle cell
proliferation by blocking Akt-dependent pathway. Vascul Pharmacol.
53:61–67. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Freigang S, Ampenberger F, Spohn G, Heer
S, Shamshiev AT, Kisielow J, Hersberger M, Yamamoto M, Bachmann MF
and Kopf M: Nrf2 is essential for cholesterol crystal-induced
inflammasome activation and exacerbation of atherosclerosis. Eur J
Immunol. 41:2040–2051. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sussan TE, Jun J, Thimmulappa R, Bedja D,
Antero M, Gabrielson KL, Polotsky VY and Biswal S: Disruption of
Nrf2, a key inducer of antioxidant defenses, attenuates
ApoE-mediated atherosclerosis in mice. PLoS One. 3:e37912008.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chernukha IM, Fedulova LV, Kotenkova EA,
Takeda S and Sakata R: Hypolipidemic and anti-inflammatory effects
of aorta and heart tissues of cattle and pigs in the
atherosclerosis rat model. Anim Sci J. 89:784–793. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chai JT, Biasiolli L, Li L, Alkhalil M,
Galassi F, Darby C, Halliday AW, Hands L, Magee T, Perkins J, et
al: Quantification of lipid-rich core in carotid atherosclerosis
using magnetic resonance T2 mapping: Relation to clinical
presentation. JACC Cardiovasc Imaging. 10:747–756. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bombaca ACS, Viana PG, Santos ACC, Silva
TL, Rodrigues ABM, Guimarães ACR, Goulart MOF, da Silva Júnior EN
and Menna-Barreto RFS: Mitochondrial disfunction and ROS production
are essential for anti-Trypanosoma cruzi activity of
beta-lapachone-derived naphthoimidazoles. Free Radical Biol Med.
130:408–418. 2018. View Article : Google Scholar
|
|
22
|
Kosuru R, Kandula V, Rai U, Prakash S, Xia
Z and Singh S: Pterostilbene decreases cardiac oxidative stress and
inflammation via activation of AMPK/Nrf2/HO-1 pathway in
fructose-fed diabetic rats. Cardiovasc Drugs Ther. 32:147–163.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Elango B, Dornadula S, Paulmurugan R and
Ramkumar KM: Pterostilbene ameliorates streptozotocin-induced
diabetes through enhancing antioxidant signaling pathways mediated
by Nrf2. Chem Res Toxicol. 29:47–57. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Geovanini GR and Libby P: Atherosclerosis
and inflammation: Overview and updates. Clin Sci (Lond).
132:1243–1252. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lin J, Kakkar V and Lu X: Impact of MCP-1
in atherosclerosis. Curr Pharm Des. 20:4580–4588. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bernberg E, Ulleryd MA, Johansson ME and
Bergström GM: Social disruption stress increases IL-6 levels and
accelerates atherosclerosis in ApoE−/− mice.
Atherosclerosis. 221:359–365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Grebe A, Hoss F and Latz E: NLRP3
Inflammasome and the IL-1 pathway in atherosclerosis. Circ Res.
122:1722–1740. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Park KY and Heo TH: Critical role of TNF
inhibition in combination therapy for elderly mice with
atherosclerosis. Cardiovasc Ther. 35:352017. View Article : Google Scholar
|
|
29
|
Zhou Q, Han X, Li R, Zhao W, Bai B, Yan C
and Dong X: Anti-atherosclerosis of oligomeric proanthocyanidins
from Rhodiola rosea on rat model via hypolipemic,
antioxidant, anti-inflammatory activities together with regulation
of endothelial function. Phytomedicine. 51:171–180. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wu T, Peng Y, Yan S, Li N, Chen Y and Lan
T: Andrographolide ameliorates atherosclerosis by suppressing
pro-inflammation and ROS generation-mediated foam cell formation.
Inflammation. 41:1681–1689. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Décordé K, Ventura E, Lacan D, Ramos J,
Cristol JP and Rouanet JM: An SOD rich melon extract Extramel
prevents aortic lipids and liver steatosis in diet-induced model of
atherosclerosis. Nutr Metab Cardiovasc Dis. 20:301–307. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yao Y, Liu K, Zhao Y, Hu X and Wang M:
Pterostilbene and 4′-Methoxyresveratrol inhibited
lipopolysaccharide-induced inflammatory response in RAW264.7
macrophages. Molecules. 23:232018. View Article : Google Scholar
|
|
33
|
Mitra R, O'Neil GL, Harding IC, Cheng MJ,
Mensah SA and Ebong EE: Glycocalyx in atherosclerosis-relevant
endothelium function and as a therapeutic target. Curr Atheroscler
Rep. 19:632017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Dai G, Vaughn S, Zhang Y, Wang ET,
Garcia-Cardena G and Gimbrone MA Jr: Biomechanical forces in
atherosclerosis-resistant vascular regions regulate endothelial
redox balance via phosphoinositol 3-kinase/Akt-dependent activation
of Nrf2. Circ Res. 101:723–733. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zeng Y, Li C, Guan M, Zheng Z, Li J, Xu W,
Wang L, He F and Xue Y: The DPP-4 inhibitor sitagliptin attenuates
the progress of atherosclerosis in apolipoprotein-E-knockout mice
via AMPK- and MAPK-dependent mechanisms. Cardiovasc Diabetol.
13:322014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Fullerton MD, Steinberg GR and Schertzer
JD: Immunometabolism of AMPK in insuliresistance and
atherosclerosis. Mol Cell Endocrinol. 366:224–234. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Li Y, Xu S, Mihaylova MM, Zheng B, Hou X,
Jiang B, Park O, Luo Z, Lefai E, Shyy JY, et al: AMPK
phosphorylates and inhibits SREBP activity to attenuate hepatic
steatosis and atherosclerosis in diet-induced insulin-resistant
mice. Cell Metab. 13:376–388. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Vasamsetti SB, Karnewar S, Kanugula AK,
Thatipalli AR, Kumar JM and Kotamraju S: Metformin inhibits
monocyte-to-macrophage differentiation via AMPK-mediated inhibition
of STAT3 activation: Potential role in atherosclerosis. Diabetes.
64:2028–2041. 2015. View Article : Google Scholar : PubMed/NCBI
|