Introduction
Spinal metastatic tumor is a common metastatic tumor
of many advanced malignant tumors, which is mainly formed by the
primary tumor transferring to the spine through blood or lymph
metastasis (1). Spinal tumors are
often characterized by multiple lesions involving multiple segments
and accompanied by severe pain, which has a serious impact on the
quality of life and health of patients (2). In the past, radiotherapy and
chemotherapy as well as surgery were mainly used for the treatment
of spinal metastases clinically. However, radiotherapy and
chemotherapy for patients not only have a long treatment cycle, but
also have many adverse reactions. Therefore, with the continuous
development of medical technology in recent years, surgery has
gradually become the main method for the treatment of spinal
metastases. However, surgery still has the problems of large
trauma, incomplete resection, and high recurrence rate (3,4).
Therefore, it is of great clinical significance to find a treatment
method with better efficacy and less adverse effects for patients
with spinal metastatic tumors (5).
Radiofrequency ablation is a tumor therapy method
that has been gradually applied clinically in recent years. It
mainly inactivates and damages tumor tissues of patients through
friction heat generated by high-frequency current. It has the
characteristics of less trauma and fewer complications (6). At present, radiofrequency ablation has
achieved good efficacy in the treatment of various metastatic
tumors such as bone metastasis of breast cancer (7), liver metastasis of rectal cancer
(8), and the combination of surgery.
There is also research (9) showing
that patients with spinal metastases have achieved 89 and 70% local
control, respectively, in 3 months and 1 year after percutaneous
radiofrequency ablation.
Although some studies have been reported on the
application of radiofrequency ablation in spinal metastatic tumors,
few studies have been carried out to analyze the effects of
radiofrequency ablation and the influencing factors on the
prognosis of patients. Therefore, in this study, the effects of
radiofrequency ablation assisted with traditional open surgery in
spinal metastatic tumors and the influencing factors on the
prognosis of patients, were analyzed with a view to provide more
basis for clinical treatment of patients with spinal metastatic
tumors.
Materials and methods
General data
A total of 132 patients with spinal metastases from
April 2014 to February 2016 were selected, including 71 male and 61
female patients. Their average age was 57.64±10.29. The patients
were divided into research group and control group according to the
treatment plan accepted by the patients. Sixty-seven patients with
simple surgery were regarded as the control group, and 65 patients
with radiofrequency ablation assisted surgery were the research
group. Inclusion exclusion criteria were as follows: Inclusion
criteria were as follows: Patients diagnosed as spinal metastases
by pathological diagnosis, patients who have undergone primary
tumor resection, patients with an expected survival period of more
than 6 months, and patients with preoperative tolerance to surgery.
Exclusion criteria were as follows: Patients with contraindications
to surgery, patients with unclear primary focus, patients with
severe liver and kidney dysfunction, patients with unclear surgical
indications, patients with serious heart and lung diseases,
patients who did not cooperate with the study, patients with
communication or cognitive impairment. All patients and their
families agreed to participate in the experiment and sign an
informed consent. The study was approved by the Ethics Committee of
Weifang People's Hospital (Weifang, China).
Treatment methods
All patients underwent imaging examination before
surgery to determine the location and number of lesions and cones,
and the degree of cone deterioration and spinal cord compression
were evaluated. The patients in the control group were treated with
simple open cone resection. After general anesthesia, the patients
were placed in prone position. The pathological cones located
before surgery were taken as the center to make a longitudinal
incision. The upper and lower cones of the pathological cones were
fixed and the muscles beside the cones were separated. First,
accessory tumors such as vertebral pedicle or lamina were excised.
Then, unilateral laminectomy and decompression were performed. In
addition, tumor tissues that compressed spinal cord in spinal canal
were excised. In order to better perform bone graft fusion, during
the resection of the affected cone, attention should also be paid
to the removal of its corresponding upper and lower intervertebral
discs. After the resection was completed, bone cement was poured
into the resection site. The resection site was filled with bone
cement. After the bone cement was solidified, the bone threading
needle was pulled out and the operation area was sterilized and
flushed. The drainage tube was placed for negative pressure
drainage. Finally, the incision was closed. Patients in the
research group were assisted with radiofrequency ablation on the
basis of patients in the control group. After cone resection,
UniBlate monopolar needle electrode (RITA1500X type) was introduced
into the pathological cones through vertebral pedicle under X-ray
fluoroscopy, and the initial power was set at 150 W. The ablation
range was set according to the tumor and the pathological degree.
The temperature of the radiofrequency needle was controlled at
80–100°C. The time of single point ablation is 6–12 min. During
ablation, the blood loss and changes of vital signs of patients
were closely detected. The ablation area was appropriately expanded
to 0.5 cm beyond the edge of the lesions. Bone cement was injected
after ablation. The method was the same as that of the control
group. All patients were treated with cefradine (2 g/12 h) for 3
days after surgery.
Observation indicators
i) The time of operation and intraoperative blood
loss of patients in the two groups were recorded and compared. ii)
Visual analogue pain score (VAS) (10) was evaluated before and 6 months after
surgery of patients in both groups. iii) The Karnofsky (KPS)
(11) scores before and 6 months
after surgery of patients in the two groups were compared. iv) The
Frankel spinal cord injury grading (12) before and 6 months after surgery of
patients in the two groups were compared. v) The complications of
patients in the two groups within 6 months after surgery were
recorded and compared. The complications included bone cement
leakage, hemorrhage, deep venous thrombosis of lower limbs, and
infection. vi) The patients were followed up for 36 months and the
survival rates of the two groups were analyzed. vii) Cox regression
model was used to analyze the factors affecting the prognosis of
patients.
Statistical methods
In this study, the experimental data were
statistically analyzed by SPSS 18.0 software. The counting data
adopted Chi-square test, and the measurement data adopted mean ±
standard deviation. The comparison between the two groups adopted t
test. The experimental images were drawn by GraphPad Prism 6,
correlation analysis was by Pearson's, survival analysis used
Kaplan-Meier survival curve, multivariate analysis of prognostic
risk factors of patients adopted Cox regression model. P<0.05
was considered to indicate a statistically significant
difference.
Results
Comparison of general data
There was no significant difference in sex, age,
number of pathological cones, and nerve involvement of patients
between the two groups (P>0.05) (Table I).
 | Table I.General data. |
Table I.
General data.
| Factors | Research group
n=65 | Control group
n=67 | t/χ2
value | P-value |
|---|
| Sex |
|
| 0.131 | 0.717 |
| Male | 36 (55.38) | 35 (52.24) |
|
|
|
Female | 29 (44.61) | 32 (47.76) |
|
|
| Age (years) |
56.07±10.11 | 57.12±9.85 | 0.547 | 0.604 |
| BMI
(kg/m2) | 22.54±1.48 | 22.37±1.52 | 0.651 | 0.516 |
| Number of
pathological cones |
|
| 0.270 | 0.966 |
| 1
segment | 36 (55.38) | 39 (58.21) |
|
|
| 2
segments | 13 (20.22) | 14 (20.90) |
|
|
| 3
segments | 10 (15.38) | 9
(13.43) |
|
|
| 4
segments | 6 (9.23) | 5 (7.46) |
|
|
| Nerve
involvement |
|
| 0.032 | 0.858 |
| Yes | 31 (47.69) | 33 (49.25) |
|
|
| No | 34 (52.31) | 34 (50.75) |
|
|
| Malignant degree |
|
| 0.280 | 0.869 |
| High | 20 (30.77) | 21 (31.34) |
|
|
|
Moderate | 30 (46.15) | 33 (49.25) |
|
|
| Low | 15 (23.08) | 13 (19.40) |
|
|
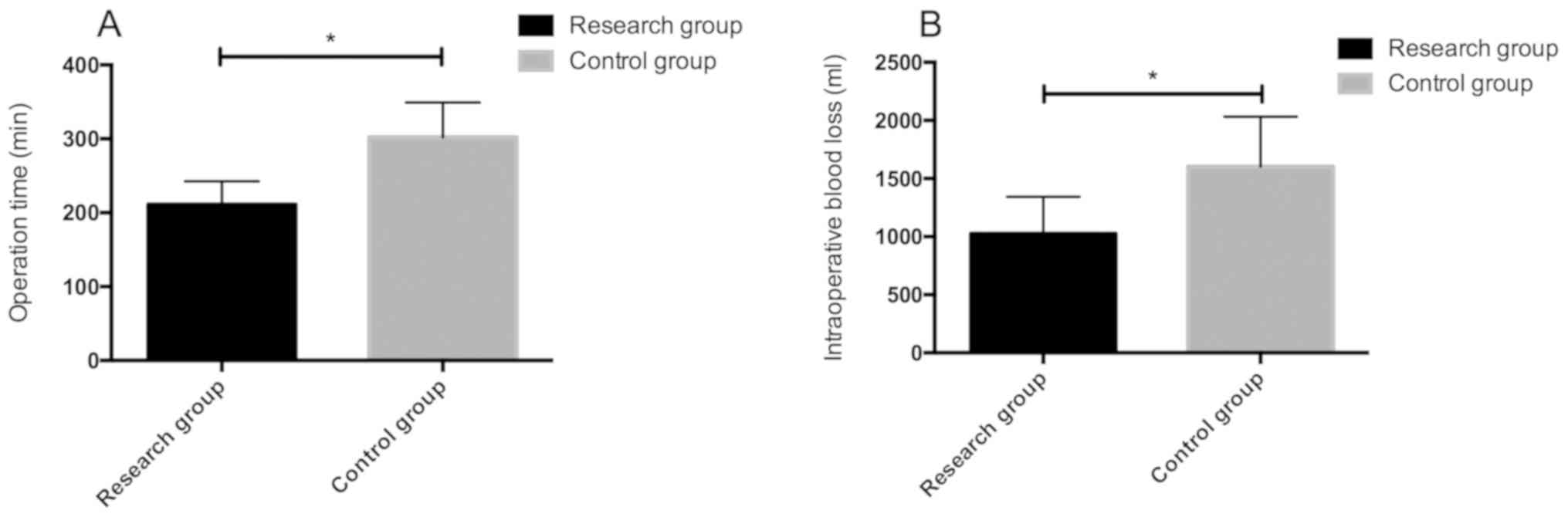
Comparison of time of operation and
intraoperative blood loss of patients between the two groups
The time of operation and intraoperative blood loss
of patients in the research group were 211.13±31.48 min and
1026.72±316.97 ml, respectively, while the time of operation and
intraoperative blood loss of patients in the control group were
302.26±46.75 min and 1603.95±427.51 ml, respectively. The time of
operation and intraoperative blood loss of patients in the research
group were significantly lower than those in the control group,
with statistically significant difference (P<0.05) (Fig. 1).
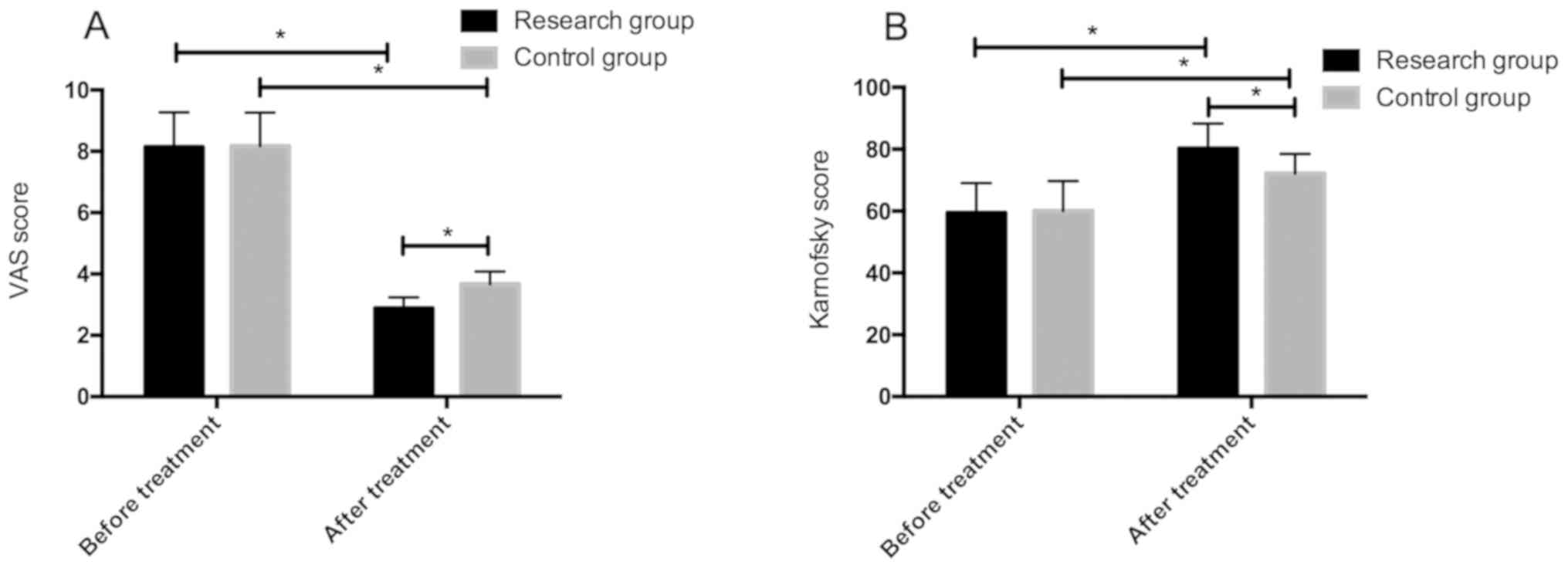
VAS and KPS scores of patients in the
two groups before and after treatment
The VAS and KPS scores of patients in the two groups
before treatment were not significantly different (P>0.05). The
VAS scores of patients in the two groups after treatment were lower
than those before treatment, and KPS scores were significantly
higher than those before treatment. However, the improvement of
patients in the research group was more obvious than that in the
control group, and the difference was statistically significant
(P<0.05) (Fig. 2).
Frankel spinal cord injury grading of
patients in the two groups before and after treatment
There was no significant difference in Frankel
grading of patients between the two groups before treatment
(P>0.05). Frankel grading of patients in the two groups after
treatment was significantly improved compared with that before
treatment (P<0.05). There was no significant difference in
Frankel grading after improvement between the two groups
(P>0.05) (Table II).
 | Table II.Frankel spinal cord injury grading of
patients in the two groups before and after treatment. |
Table II.
Frankel spinal cord injury grading of
patients in the two groups before and after treatment.
|
| Before treatment | After treatment |
|
|
|---|
|
|
|
|
|
|
|---|
| Grouping | A | B | C | D | E | A | B | C | D | E | χ2
value | P-value |
|---|
| Research | 0 | 10 | 36 | 19 | 0 | 0 | 5 | 27 | 26 | 7 | 11.04 | 0.012 |
| group n=65 |
| (15.38) | (55.38) | (29.23) |
|
| (7.69) | (41.54) | (40.00) | (10.77) |
|
|
| Control | 0 | 11 | 36 | 20 |
|
| 9 | 27 | 25 | 6 | 8.041 | 0.045 |
| group n=67 |
| (16.42) | (53.73) | (29.85 | 0 | 0 | (13.43) | (40.30) | (37.31) | (8.96) |
|
|
| χ2
value |
|
| 0.043 |
|
|
|
| 1.209 |
|
|
|
|
| P-value |
|
| 0.979 |
|
|
|
| 0.751 |
|
|
|
|
Complications of patients in the two
groups
The number of patients in the research group with
leakage, hemorrhage, deep venous thrombosis of lower limbs, and
infection was 2, 1, 1, and 1, respectively, with a complication
rate of 7.69%. The number of patients in the control group with
leakage, hemorrhage, deep venous thrombosis, and infection was 4,
2, 2, and 3, respectively, with a complication rate of 19.40%. In
addition, the complication rate of patients in the research group
was significantly lower than that of patients in the control group,
with statistically significant difference (P<0.05) (Table III).
 | Table III.Complications of patients in the two
groups. |
Table III.
Complications of patients in the two
groups.
| Factors | Research group
n=65 | Control group
n=67 | χ2
value | P-value |
|---|
| Leakage | 2 (3.08) | 6 (8.96) | 2.002 | 0.157 |
| Hemorrhage | 1 (1.54) | 2 (2.99) | 0.311 | 0.577 |
| Deep venous
thrombosis of lower limbs | 1 (1.54) | 2 (2.99) | 0.311 | 0.577 |
| Infection | 0 | 3 (4.48) | 2.978 | 0.084 |
| Total incidence
rate | 4 (7.69) | 13 (19.40) | 5.162 | 0.023 |
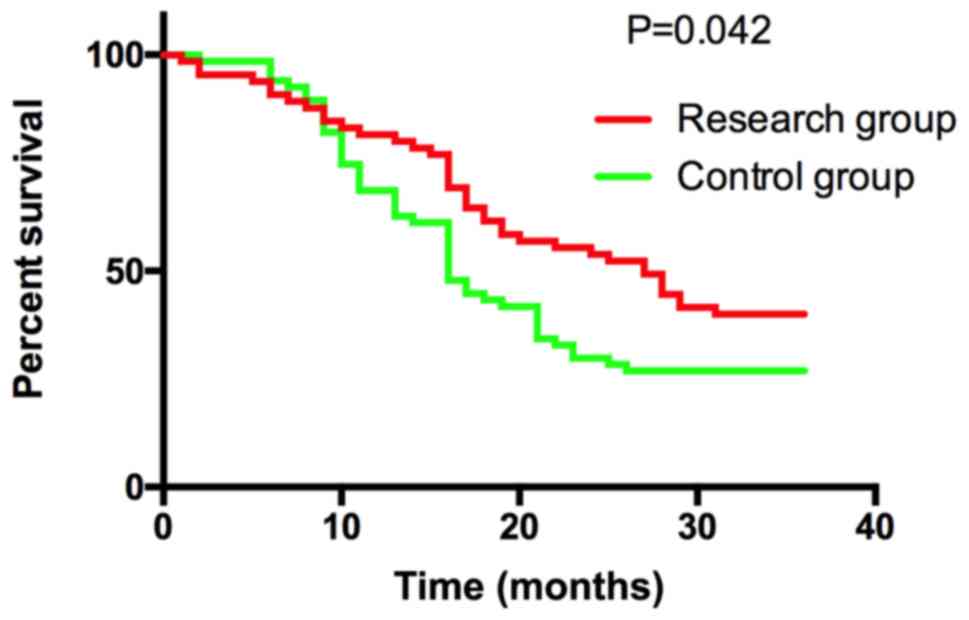
Comparison of recurrence rate and
survival rate of patients between the two groups
During the 36-month follow-up period, there were no
patients who missed the visit. There were 40 patients in the
research group who relapsed, with a recurrence rate of 61.54% in 3
years, and 39 patients died, with a 3-year survival rate of 40.00%
(26/65). There were 55 patients in the control group who relapsed,
with a recurrence rate of 82.09% in 3 years, and 49 patients died,
with a 3-year survival rate of 28.36% (19/67). The 3-year
recurrence rate of patients in the research group was significantly
lower than that in the control group, and the survival rate was
significantly higher than that in the control group, with
statistically significant difference (P<0.05) (Fig. 3).
Single analysis of poor prognosis in
patients with spinal metastasis tumor
We divided patients into death group (88 cases) and
survival group (44 cases) according to their 3-year survival
conditions. We analyzed the clinical and pathological data of
patients in the two groups. The results showed that the number of
pathological cones, visceral metastasis, nerve involvement,
malignant degree, and radiofrequency ablation treatment may be the
factors affecting the poor prognosis of patients (P<0.05)
(Table IV).
 | Table IV.Single analysis of poor prognosis in
patients with spinal metastasis tumor. |
Table IV.
Single analysis of poor prognosis in
patients with spinal metastasis tumor.
| Factors | Survival group
n=44 | Death group
n=88 | t/χ2
value | P-value |
|---|
| Sex |
|
| 0.061 | 0.805 |
|
Male | 21 (47.73) | 40 (45.45) |
|
|
|
Female | 23 (52.27) | 48 (54.55) |
|
|
| Age (years) | 57.15±9.27 | 56.42±9.68 | 0.414 | 0.679 |
| Number of
pathological cones |
|
| 18.71 | <0.001 |
| 1
segment | 36 (81.82) | 39 (44.32) |
|
|
| 2
segments | 6 (13.64) | 21 (23.86) |
|
|
| 3
segments | 2 (4.54) | 17 (19.32) |
|
|
| 4
segments | 0 | 11 (12.51) |
|
|
| Visceral
metastasis |
|
| 7.443 | 0.006 |
|
Yes | 12 (27.27) | 46 (52.27) |
|
|
| No | 32 (72.73) | 42 (47.73) |
|
|
| Nerve
involvement |
|
| 5.475 | 0.019 |
|
Yes | 15 (34.09) | 49 (55.68) |
|
|
| No | 23 (52.27) | 39 (44.32) |
|
|
| Malignant
degree |
|
| 10.74 | 0.005 |
|
High | 8
(18.18) | 33 (37.50) |
|
|
|
Moderate | 20 (45.45) | 43 (48.86) |
|
|
|
Low | 16 (36.36) | 12 (13.64) |
|
|
| Radiofrequency
ablation therapy |
|
| 11.88 | <0.001 |
|
Yes | 31 (70.45) | 34 (38.64) |
|
|
| No | 13 (29.55) | 54 (61.36) |
|
|
Multivariate analysis of poor
prognosis in patients with spinal metastasis tumor
Through single factor analysis, we found that the
number of pathological cones, visceral metastasis, nerve
involvement, malignant degree, and radiofrequency ablation therapy
might be factors that affect the poor prognosis of patients. Then
we assigned values to the single factors that have differences
(Table V) and further included the
single factors that have differences into Cox risk proportion model
for analysis. The results showed that the number of pathological
cones, visceral metastasis, malignant degree, and radiofrequency
ablation therapy were independent risk factors that affect the poor
prognosis of patients. More details are shown in Table VI.
 | Table V.Assignments. |
Table V.
Assignments.
| Factors | Assignment |
|---|
| No. of pathological
cones | 1 segment=1, 2
segments=2, 3 segments=3, 4 segments=4 |
| Visceral
metastasis | Not transferred=1,
transferred=2 |
| Malignant
degree | Low=1, moderate=2,
high=3 |
| Radiofrequency
ablation | Yes=1, no=2 |
| Nerve
involvement | No=1, yes=2 |
| Living
conditions | Survival=1,
death=2 |
 | Table VI.Multivariate analysis of poor
prognosis in patients with spinal metastasis tumor. |
Table VI.
Multivariate analysis of poor
prognosis in patients with spinal metastasis tumor.
| Independent
variable | β | SE | Wald | P-value | OR | 95% CI |
|---|
| No. of pathological
cones | 1.171 | 0.482 | 5.543 | 0.014 | 3.229 | 2.819–7.531 |
| Visceral
metastasis | 1.085 | 0.544 | 11.176 | 0.001 | 6.082 | 1.085–8.039 |
| Malignant
degree | 1.077 | 0.536 | 11.168 | 0.001 | 6.084 | 1.076–8.031 |
| Radiofrequency
ablation | 1.238 | 0.455 | 7.208 | 0.004 | 3.452 | 2.117–7.307 |
| Nerve
involvement | 0.927 | 1.169 | 0.624 | 0.472 | – | – |
Discussion
Spine is a high incidence site for malignant tumor
metastases. Spinal metastatic tumors will lead to intractable pain
and nerve compression and other symptoms, which will have a serious
impact on the quality of life of patients (13). At present, the treatment of spinal
metastases mainly focuses on nerve compression of patients and pain
relief. In the past, conservative methods such as radiotherapy,
chemotherapy, and palliative treatment were mainly adopted to treat
spinal metastases, but the efficacy was not good (14). Therefore, it is of great clinical
significance to find a treatment method with better efficacy for
patients with spinal metastases.
In the present study, we analyzed the clinical
efficacy of simple surgery and radiofrequency ablation assisted
surgery in the treatment of spinal metastases and the impact on the
prognosis of patients. This research was carried out due to the
continuous development of surgical techniques in recent years, and
surgery has gradually become the main method for the treatment of
spinal metastases (15). Previous
studies (16) have shown that
surgical treatment can better improve the neurological function of
patients with spinal metastases, and it is considered to be
superior to radiotherapy and chemotherapy in relieving pain of
patients. However, simple cone resection not only has great trauma
to the patients, but also leads to a higher recurrence rate for
some tumors that are difficult to be excised (17). Radiofrequency ablation is a thermal
ablation technique gradually applied in tumor treatment in recent
years, and friction heat can be generated by alternating current,
so as to perform targeted ablation on tumors, which is beneficial
to local control of metastatic lesions (18). The results of our study show that the
time of operation and intraoperative blood loss of patients in the
research group are significantly lower than those in the control
group, which suggests that we can effectively reduce the time of
operation and blood loss when radiofrequency ablation is used to
assist surgery.
Previous studies (19,20) have
shown that one of the advantages of radiofrequency ablation is that
it can coagulate tumor microvessels locally through thermal
ablation, which is conducive to reducing the density of blood
vessels and the amount of bleeding during surgery, and is also
conducive to surgical operation so as to shorten the time of
operation, which proves and explains our results. Then the VAS, KPS
scores, and Frankel grading of patients in the two groups before
and after surgery were compared. The results showed that the VAS,
KPS scores, and Frankel grading of patients in the two groups after
treatment were significantly improved compared with those before
treatment. However, the VAS and KPS scores of patients in the
research group were more improved than those in the control group,
and there was no significant difference in the improved number of
Frankel grading. This suggests that surgery has a good effect on
the neurological function recovery of patients with spinal
metastases, but if assisted with radiofrequency ablation, it can
more effectively relieve pain of patients and promote the
functional recovery of patients.
Previous research (18) have indicated that when radiofrequency
ablation and surgery are combined, radiofrequency ablation can
create ablation gaps in the pathological cones, which is conducive
to the injection of bone cement and the reduction of leakage rate,
thus relieving the pain of patients. In addition, there is also
research (21) showing that the pain
relief rate for patients with spinal metastases can reach 100% when
radiofrequency ablation and surgery are combined. This is
consistent with our conclusion. The complications and 3-year
survival rate of patients in the two groups were compared. The
results showed that the incidence rate of complications of patients
in the research group was significantly lower than that of the
control group, and the 3-year recurrence rate was significantly
lower than that of the control group. The 3-year survival rate was
significantly higher than that of the control group. This suggests
that the application of radiofrequency ablation in the surgical
operation of spinal metastases is beneficial to reduce the
occurrence of postoperative complications and tumor recurrence and
prolong the survival time of the patients. Previous research
(22) have indicated that
radiofrequency ablation can directly act on the tumor itself, and
ablation technology can cause coagulation necrosis of the tumor,
which can enhance the efficacy of the surgery and reduce
recurrence.
For a long time, the prognosis of spinal metastases
has been a difficult clinical problem. Although we found in
previous studies that the use of radiofrequency ablation may affect
the prognosis of patients, it still needs further confirmation in
subsequent experiments. Therefore, we analyzed the factors that
affected the prognosis of patients with spinal metastases. The
results showed that the number of pathological cones, visceral
metastasis, malignant degree, and radiofrequency ablation therapy
were independent risk factors that affected the prognosis of
patients with spinal metastases. Previous studies (23) have indicated that the malignant
degree of the tumor itself will have a direct impact on the
prognosis of patients. There is also research (24) that organ metastasis of tumor is an
important factor affecting poor prognosis of tumor patients.
Moreover, for patients with spinal metastases, a larger number of
cones means a greater treatment risk and a longer postoperative
recovery time, which will also have an important impact on the
prognosis of patients (25).
However, radiofrequency ablation is proposed for the first time in
our study as a protective factor for the prognosis of patients with
spinal metastases, which needs further research in the future.
Collectively, radiofrequency ablation assisted
surgery can effectively improve the clinical efficacy of patients
with spinal metastases, reduce the postoperative complications and
recurrence rate of patients, and prolong the survival time of
patients compared with simple surgical treatment. Moreover, the
malignant degree of tumors, the presence or absence of organ
metastasis and the number of pathological cones are independent
risk factors leading to poor prognosis of patients. The application
of radiofrequency ablation is a protective factor for the prognosis
of patients. In our opinion, patients conforming to the principles
of surgical treatment should be recommended the use of
radiofrequency ablation assisted surgery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ML observed indicators and wrote the manuscript,
interpreted and analyzed the data. YZ designed the study and
performed the experiment. XZ was responsible for the analysis and
discussion of the data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Weifang People's Hospital (Weifang, China). Patients who
participated in this research had complete clinical data. Signed
informed consents were obtained from the patients and/or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang J, Fang Z, Lang N, Yuan H, Su MY and
Baldi P: A multi-resolution approach for spinal metastasis
detection using deep Siamese neural networks. Comput Biol Med.
84:137–146. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Roser S, Maharaj MM, Taylor MA, Kuru R,
Hansen MA and Ferch R: Vertebrectomy in metastatic spinal tumours:
A 10 year, single-centre review of outcomes and survival. J Clin
Neurosci. 68:218–223. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gharzai LA, Beeler WH, Hayman JA, Mancini
B, Jagsi R, Pierce L, Moran JM, Dominello MM, Boike T, Griffith K,
et al Michigan Radiation Oncology Quality Consortium, :
Recommendations for single faction radiation therapy and
stereotactic body radiation therapy in palliative treatment of bone
metastases: A statewide practice patterns survey. Pract Radiat
Oncol. 9:e541–e548. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pennington Z, Ahmed AK, Cottrill E,
Westbroek EM, Goodwin ML and Sciubba DM: Intra- and interobserver
reliability of the Spinal Instability Neoplastic Score system for
instability in spine metastases: A systematic review and
meta-analysis. Ann Transl Med. 7:2182019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schaub SK, Tseng YD, Chang EL, Sahgal A,
Saigal R, Hofstetter CP, Foote M, Ko AL, Yuh WTC, Mossa-Basha M, et
al: Strategies to mitigate toxicities from stereotactic body
radiation therapy for spine metastases. Neurosurgery. 85:729–740.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang Y, Zhang MB, Luo YK, Li J, Zhang Y
and Tang J: Effect of chronic lymphocytic thyroiditis on the
efficacy and safety of ultrasound-guided radiofrequency ablation
for papillary thyroid microcarcinoma. Cancer Med. 8:5450–5458.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Leto G: Current status and future
directions in the treatment of bone metastases from breast cancer.
Clin Exp Pharmacol Physiol. 46:968–971. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
van Amerongen MJ, van der Stok EP,
Fütterer JJ, Jenniskens SFM, Moelker A, Verhoef C, Grünhagen DJ and
de Wilt JHW: Results after simultaneous surgery and RFA liver
ablation for patients with colorectal carcinoma and synchronous
liver metastases. Eur J Surg Oncol. Jul 7–2019.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wallace AN, Tomasian A, Vaswani D,
Vyhmeister R, Chang RO and Jennings JW: Radiographic local control
of spinal metastases with percutaneous radiofrequency ablation and
vertebral augmentation. AJNR Am J Neuroradiol. 37:759–765. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cooke ME, Welch T, Gusakov O and Tornetta
P III: Are continuous femoral nerve catheters beneficial for pain
management after operative fixation of tibial plateau fractures? A
randomized controlled trial. J Orthop Trauma. 33:e447–e451. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Barbetta C, Allgar V, Maddocks M, Ribeiro
C, Wilcock A, Currow DC, Phillips J and Johnson MJ:
Australia-modified Karnofsky Performance Scale and physical
activity in COPD and lung cancer: An exploratory pooled data
analysis. BMJ Support Palliat Care. Jul 11–2019.(Epub ahead of
print). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Capaul M, Zollinger H, Satz N, Dietz V,
Lehmann D and Schurch B: Analyses of 94 consecutive spinal cord
injury patients using ASIA definition and modified Frankel score
classification. Paraplegia. 32:583–587. 1994.PubMed/NCBI
|
|
13
|
Buergy D, Sharfo AW, Heijmen BJ, Voet PW,
Breedveld S, Wenz F, Lohr F and Stieler F: Fully automated
treatment planning of spinal metastases - A comparison to manual
planning of Volumetric Modulated Arc Therapy for conventionally
fractionated irradiation. Radiat Oncol. 12:332017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hamad A, Vachtsevanos L, Cattell A,
Ockendon M and Balain B: Minimally invasive spinal surgery for the
management of symptomatic spinal metastasis. Br J Neurosurg.
31:526–530. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Guzik G: Oncological and functional
results of the surgical treatment of vertebral metastases in
patients with multiple myeloma. BMC Surg. 17:922017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Patchell RA, Tibbs PA, Regine WF, Payne R,
Saris S, Kryscio RJ, Mohiuddin M and Young B: Direct decompressive
surgical resection in the treatment of spinal cord compression
caused by metastatic cancer: A randomised trial. Lancet.
366:643–648. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
de Ruiter GC, Nogarede CO, Wolfs JF and
Arts MP: Quality of life after different surgical procedures for
the treatment of spinal metastases: Results of a single-center
prospective case series. Neurosurg Focus. 42:E172017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kam NM, Maingard J, Kok HK, Ranatunga D,
Brooks D, Torreggiani WC, Munk PL, Lee MJ, Chandra RV and Asadi H:
Combined vertebral augmentation and radiofrequency ablation in the
management of spinal metastases: An update. Curr Treat Options
Oncol. 18:742017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Griessenauer CJ, Salem M, Hendrix P,
Foreman PM, Ogilvy CS and Thomas AJ: Preoperative embolization of
spinal tumors: A systematic review and meta-analysis. World
Neurosurg. 87:362–371. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Stephenson MB, Glaenzer B and Malamis A:
Percutaneous minimally invasive techniques in the treatment of
spinal metastases. Curr Treat Options Oncol. 17:562016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Toyota N, Naito A, Kakizawa H, Hieda M,
Hirai N, Tachikake T, Kimura T, Fukuda H and Ito K: Radiofrequency
ablation therapy combined with cementoplasty for painful bone
metastases: Initial experience. Cardiovasc Intervent Radiol.
28:578–583. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang GW, Han XX, Ma YL, Duo J, Yang JL and
Liao ZC: Radiofrequency ablation combined with subtotal corpectomy
for spinal metastases. Chin J Orthop. 31:938–943. 2011.(In
Chinese).
|
|
23
|
Hu H, Yang HL, Wang GL, Chen KW, Zhou QS
and Zhou M: The decision-making and survival prediction role of
Tomita score in the management spinal metastases. Chin J Spin Spin
Cord. 22:673–677. 2012.(In Chinese).
|
|
24
|
Hibberd CS and Quan GMY: Accuracy of
preoperative scoring systems for the prognostication and treatment
of patients with spinal metastases. Int Sch Res Notices.
2017:13206842017.PubMed/NCBI
|
|
25
|
Pointillart V, Vital JM, Salmi R, Diallo A
and Quan GM: Survival prognostic factors and clinical outcomes in
patients with spinal metastases. J Cancer Res Clin Oncol.
137:849–856. 2011. View Article : Google Scholar : PubMed/NCBI
|