Introduction
As aging increases in society, the incidence of
proximal femoral fractures in the elderly, particularly
intertrochanteric fractures, has seen an increase over the years.
Complications arising from these fractures, including
cardiovascular and cerebrovascular diseases and lung infections,
threaten the health of these patients (1). To reduce such complications, the AO
Foundation recommends intramedullary fixation, including proximal
femoral nail anti-rotation (PFNA), InterTan, and other internal
fixation methods, for the treatment of intertrochanteric fractures.
These methods effectively increase the force arm of the fixation
device. The lag screw or screw blade is inserted into the femoral
head through the femoral neck and intertrochanter; this effectively
increases the firmness of the fixation, particularly for
osteoporotic fragility fractures (2). However, in clinical practice, the screw
may loosen, and in certain cases, the femoral head is cut off,
resulting in surgical failure (3).
Recent studies have indicated that the bone mineral density (BMD),
bone microstructural parameters and poor placement of screws in the
femoral head are significantly associated with surgical failure
(4,5). Among these, the bone microstructure of
the femoral head is the most important factor; in particular,
tension and femoral head pressure of trabecular bones are important
and have a significant guiding function for selection of surgical
techniques (6).
Although the former studies have highlighted the
important association between the femoral head density and the
success of internal fixation, the roles of the BMD of the femoral
head's medial, central and lateral portions have remained to be
fully explored, which make the placement of screws a challenging
task for surgeons.
To improve the success rate of internal fixation,
the present study aimed to examine the BMD of the proximal part of
the femur and provide a theoretical basis for the optimal placement
of the lag screw.
Materials and methods
Patient information
From January 2017 to October 2018, 50 patients with
senile femoral intertrochanteric fractures were selected from the
Department of Trauma and Orthopedics, The Affiliated Hospital of
Guizhou Medical University, (Guizhou, China). Cases with
developmental dysplasia of the hip, femoral head necrosis,
pathological fractures and primary hip fusion were excluded.
The BMD of the proximal part of the injured femur
was measured using quantitative computed tomography (QCT). Among
the patients, 10 were males and 40 were females, all aged between
60 and 97 years, with a mean age of 78.02 years. The AO
classification was 31A1.1-3 type in 13 cases, 31A2.1-3 type in 21
cases and 31A3.1-3 type in 16 cases. The present study was approved
by the ethics committee of The Affiliated Hospital of Guizhou
Medical University, (Guizhou, China). Informed consent was obtained
from all patients and their families.
Measurement area selection
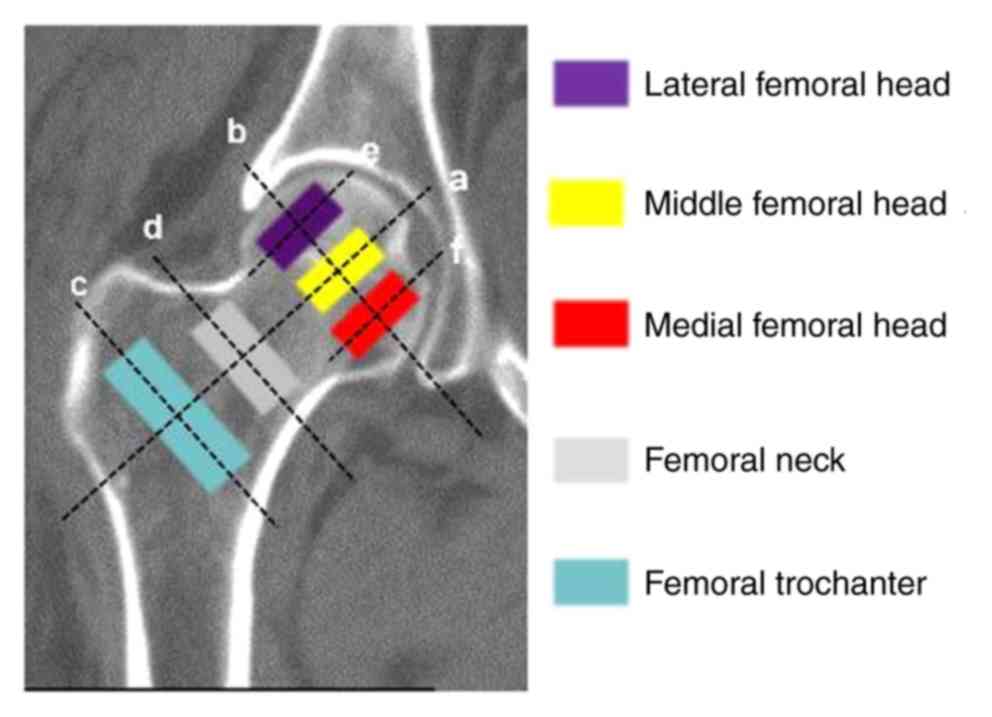
To determine the detection area, six lines were
drawn as follows (Fig. 1): ‘line a’,
a straight line through the longitudinal axis of the femoral neck
and the center of the femoral head; ‘line b’, a straight line
through the midpoint of the femoral head, perpendicular to ‘line
a’; ‘line c’, the line drawn through the femoral intertrochanter,
perpendicular to ‘line a’ (the detection area is selected from the
center of the line, which represents the intertrochanteric BMD);
‘line d’, the line formed perpendicular to ‘line a’ through the
middle of the femoral neck (the detection area is selected from the
center of the line, which represents the BMD of the femoral neck);
‘line e’, a straight line formed perpendicular to ‘line b’ through
three equal points on the outer side of the femoral head (the
detection area is selected from the center of the line,
representing the BMD outside the femoral head); and ‘line f’, the
line formed perpendicular to ‘line b’ through three equal points on
the inner side of the femoral head (the detection area is selected
from the center of the femoral head, representing the BMD of the
internal femoral head). To represent the BMD of the central section
of the femoral head, the detection area was selected from ‘line
b’.
Measurement methods
The SIEMENS 64-row SOMATOM Definition AS and spiral
CT scanner (Siemens AG) were used to scan the bilateral hip bone
structures of the patients, including the acetabular and femoral
proximal bone structures. The original images of the contralateral
hip, including the femoral intertrochanter, neck and head, were
obtained. These images were 400 Hounsfield units (HU) wide, with a
window level of 40 HU, a layer thickness of 1 mm and an interval of
1 mm. The QCT Pro software's ‘QA Exam’ function was used to
calibrate the software accuracy and the scan field uniformity of
the CT equipment. The corresponding scan field uniformity
calibration coefficient and QA phantom calibration data were
obtained to ensure the accuracy of the analysis software. The raw
images of the contralateral side were taken from a picture
archiving and communication system (SIEMENS syngo.plaza; Siemens
AG) and the CT values of the intertrochanteric bone and the femoral
head and neck were measured. The Mindways quantitative QCT BMD
measurement software (QCT Pro 4.2.3; Mindways Software, Inc.) was
used to analyze the test data. When the femoral head was detected,
it was longitudinally divided into three sections: The outer,
central and inner sections. Each section was tested thrice, and
each time, a circular test area of a fixed size (2.43
cm2) was selected. The mean value was recorded as the
final test result and expressed in mg/cm³ (Fig. 1).
Statistical analyses
Statistical analyses were performed using SPSS
software (version 16.0, SPSS, Inc.). First, the Kolmogorov-Smirnov
test was performed to determine whether the data were normally
distributed. If they were identical, one-way analysis of variance
(ANOVA) with Bonferroni's post-hoc test was performed to compare
the differences. If they were not identical, the Kruskal-Wallis
test with Steel-Dwass post-hoc test was used to compare the
differences. The Brown-Forsythe or the Welch values were analyzed
instead of the P-values in case of variance; significance values of
<0.05 were considered to indicate a significant difference.
Results
Heterogeneity test
The Kolmogorov-Smirnov test indicated that the
homodyne data of the femoral neck, femoral intertrochanter and each
of the three parts of the femoral head were identical. However,
data of the femoral head was not normally distributed. Therefore,
one-way ANOVA was used to compare the differences between the
femoral neck and head, and among the three sections of the femoral
head. The Kruskal-Wallis test was used for comparison between
femoral head and neck, femoral head and intertrochanter.
BMD analysis
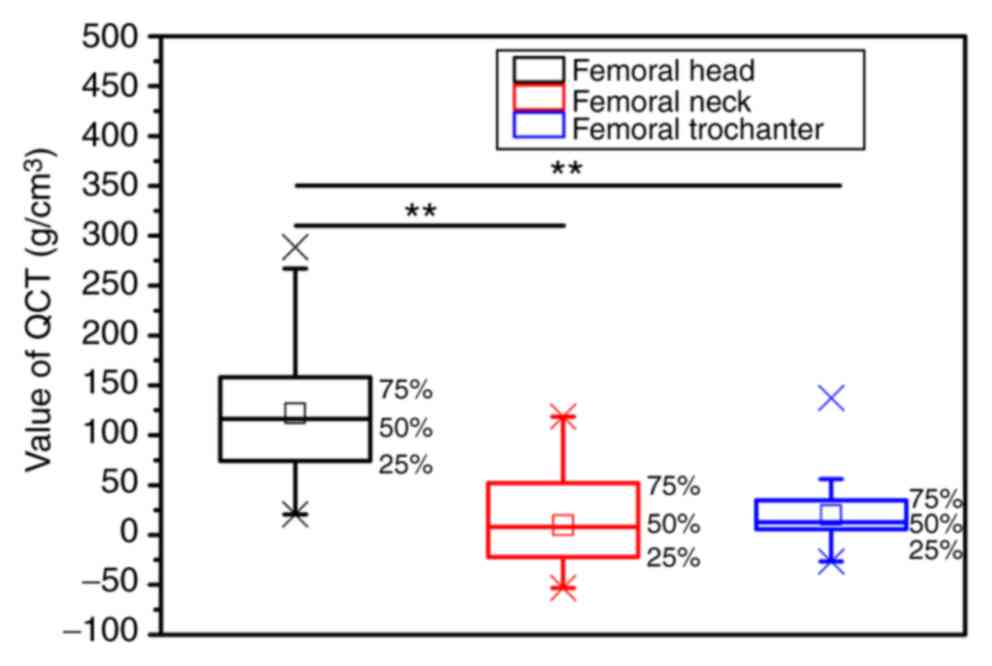
The BMD of the femoral head was the highest,
followed by that of the femoral intertrochanter, and the BMD of the
femur neck was the lowest (Fig. 2).
These differences were statistically significant (P<0.01). Among
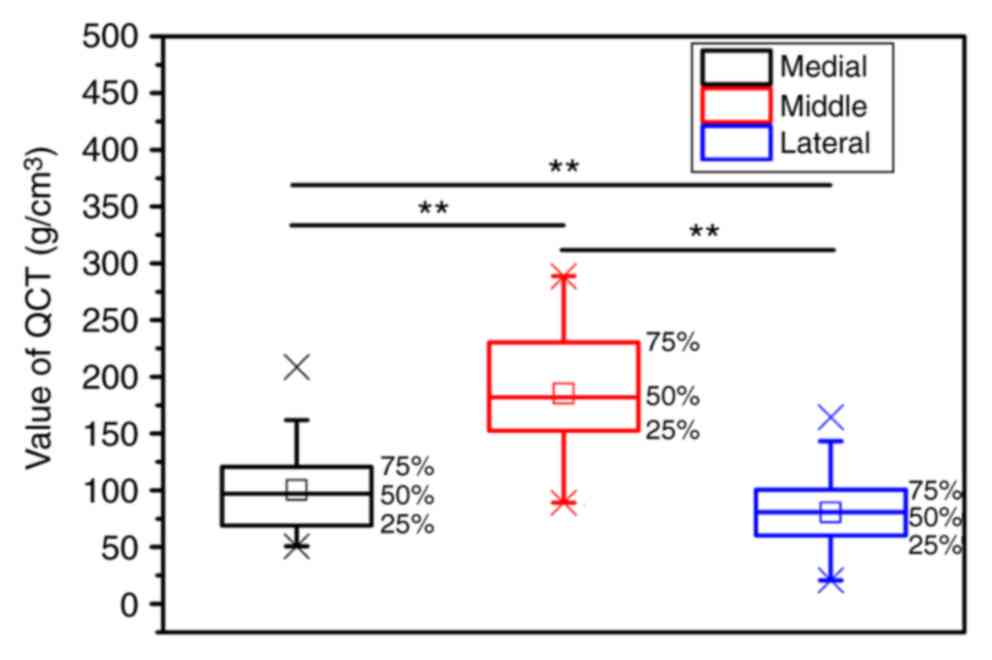
the femoral head sections, BMD analysis revealed that the lateral
and the inner sections were similar (P>0.05). The results
suggested that the BMD of the central section was the largest and
the medial and lateral bone densities were significantly smaller
(P<0.05; Fig. 3). In summary, the
tensile trabecular bone density was significantly less than the
pressure trabecular bone density (P<0.05).
Discussion
The high surgical failure of proximal femoral
fractures has drawn public attention. Patients with fixation
failures are more likely to suffer a reduction in the quality of
life upon discharge with a consequent increase in social dependency
(7). There are various reasons for
the high incidence and the device design is mostly accountable.
Born et al (8) reported that
the small-contact interface between the PFNA spiral blade and the
femoral skull, at 75 cm2, is not conducive for riveting
between the internal fixation device and the femoral skull. A
biomechanical study by Bonnaire et al (9) suggested that a novel design of the
central loading device may increase the load-bearing capacity and
thus help to reduce the cutting-out phenomenon. More importantly,
surgeon-dependent factors, including suboptimal positioning of the
device, has a significant role in fixation failure (10). Except for the above reasons, an
increasing amount of studies have revealed that BMD is highly
positively correlated with the stability of the internal fixation.
Konstantinidis et al (11)
indicated that when the femoral head volumetric BMD (vBMD) was
<250 mg/cm3, five out of nine patients developed a
screw cut, but when the vBMD was >250 mg/cm3, only 1
of 21 patient developed a screw cut. When the BMD decreases, the
structural model index (SMI) increases, the trabecular bone changes
in shape from a plate to a rod and the fixation strength of the
intraosseous screw is weakened. Kang et al (12) performed a multiple linear regression
analysis, indicating that the SMI is negatively correlated with the
stability of the embedded internal fixation. Further research has
revealed that lag screw placement in the femoral head is closely
associated with the stability of the internal fixation device.
To prevent the screw from being cut off, certain
researchers have advocated placing the lag screw under the femoral
head. Through biomechanical studies and finite element analyses,
Kuzyk et al, Goffin et al and Bessho et al
(13-15)
revealed that when the lag screw was located below the center of
the femoral neck, greater axial compression, torsional shear
resistance and minimal load deformation were observed, indicating
that this position was the most conducive for internal fixation.
However, even when surgeons strictly follow these techniques,
internal fixation failure cannot be avoided. Therefore, in the
present study, the BMD was used as a decisive factor, and the BMD
of the femoral intertrochanter, neck and head in elderly patients
with intertrochanteric fractures were measured. The femoral head
was further divided into three equal sections: The medial, central
and lateral sections. Their BMDs were measured to provide a
theoretical basis of the optimal position of the lag screws or
spiral inserts of internal fixation devices, including the PFNA and
InterTan. Numerous methods are available for detecting BMD;
dual-energy X-ray absorptiometry is the most traditionally applied
method, but its disadvantage is that it only provides the BMD of
two-dimensional structures and cannot accurately and
comprehensively display the complete BMD (16). A QCT, on the other hand, is able to
detect the BMD of a three-dimensional structure more accurately
(17). Although previous studies
have used QCT to detect the BMD in patients with hip fractures,
these studies have focused on the association between BMD and the
incidence of proximal femoral fractures, without further
investigation into their treatment (18-21).
The trabecular bone in the femoral head is divided
into the pressure and tension trabecular bones. Pressure trabeculae
grow mainly in the central and medial regions of the femoral head,
from the lower side of the femoral neck to its medial side; these
bear the pressure load. The tension trabeculae begin from the upper
side of the femoral neck and grow to its inside and below the
femoral head. Regarding the tension load, the pressure and tension
trabecular bones cross each other in the central region of the
femoral head, enhancing the weight-bearing function of the tension
trabecular bone (22). Dendorfer
et al (23) indicated that
the compressive elastic modulus, ultimate strength and yield
strength of the pressure trabecular bone were larger than those of
the tensile trabecular bone.
First, the present study indicated that, among the
BMDs of the three proximal femur portions, that of the femoral neck
is the lowest. This may be due to the presence of the Ward's
triangle in the femoral neck, consisting of the tension trabecular
bone, the pressure trabecular bone and the gap formed by the
partial tension trabecular bone, all of which are mainly filled by
fatty bone marrow. The mean BMD between the femoral trochanters was
slightly higher than that of the femoral neck, as the
intertrochanteric region is mainly composed of partial pressure
trabecular bone and the femur. As no obvious cavity was present, it
may be hypothesized that the grip force of the screw on the femoral
intertrochanter was greater than that on the femoral neck. This
suggests the importance of bone integrity of the femoral
intertrochanter in fracture fixation. If no appropriate surgical
method is selected, the internal fixation may fail, as the BMD of
the intertrochanter may be too low, or the outer wall of the
interior rotor may break, resulting in reduction of the screw's
holding force. The BMD between the femoral intertrochanter and neck
was significantly less than that of the femoral skull, with the BMD
of the latter being equivalent to the mean densities of the medial,
central and lateral sections. This is mainly due to the femoral
head being composed of the pressure and tension trabecular bones
with no cavity, and the long-term pressure and tensile loads cause
the femoral head BMD to be significantly higher than that of the
other two. Since BMD appeared to be positively correlated with the
stability of the internal fixation, this observation indicates that
the femoral head has the highest holding force on the lag screw.
Therefore, when the fracture is fixed internally, the screw that
fixes the fracture must reach the femoral head to obtain the
maximum grip force and reduce the risk of failure. This is
consistent with the results of a mechanical study by Baumgaertner
et al (24) on BMD, i.e., the
screw-fixed apex moment must be <25 mm to achieve the optimal
fixation effect.
A comparative analysis of the BMD of the medial,
central and lateral trabecular bones of the femoral head revealed
that the mean BMD of the lateral part was lower than that of the
medial part. This is due to the presence of a portion of the
tension trabecular bone in the medial side of the femoral head.
This bone has a lesser load on the hip than the pressure trabecular
bone, as the lower limb mainly has a bearing role, resulting in a
lower skeletal BMD of the tension trabecular bone than that of the
pressure trabecular bone (25).
However, this difference was not statistically significant,
indicating that the holding force generated by the two parts of the
screw was not significantly different. This demonstrates that the
lag screw mainly has a supporting role. Therefore, a deeper
placement of the lag screw (deeper than the biomechanical
requirement) inside the femoral head may be recommended. The BMD of
the two other regions of the femoral head was significantly lower
than that of the trabecular bone in the central section. This is
due to the femoral head pressure and tension trabecular bones
intersecting in this area, where the pressure trabecular bone is
mainly located, resulting in the highest skeletal BMD in the
central part (26). This indicates
that during internal fixation of fractures, the screw is best
placed in the central section of the femoral head, where it is able
to obtain the maximum holding force.
Although the present study performed BMD
measurements of the proximal femoral structures and a theoretical
analysis of the holding power of the screw, it still has certain
shortcomings. The overlapping tension and pressure trabecular bones
in the central region of the femoral head cannot be
well-distinguished from an anatomical point of view. Furthermore,
due to the fracture, it was not possible to measure the BMD of the
proximal femur on the injured side; only the BMD on the healthy
side was determined. Finally, post-operative follow-up was not
performed in the present study. These points therefore require
further investigation.
In conclusion, the location of internal fixation in
proximal femoral fractures cannot be determined using a single
method, and it is required to consider various factors. Therefore,
the present study used QCT to detect differences in the BMD in
various regions of the proximal femur and provided a novel
theoretical reference for the placement of lag screws.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural
Science Foundation of China (grant nos. 81472132, 81572183,
81672220 and 91849114) and the Priority Academic Program
Development of Jiangsu Higher Education Institutions.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
GL, JG, XZ, CW and QY collected the QCT data and
searched the literature. GL, JG, HY and JZ analyzed and interpreted
the data. GL and JG assembled the figures and wrote the manuscript.
HY and JZ designed the study and obtained the funding. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
All of the experimental procedures were approved by
the Ethics Committee of the First Affiliated Hospital of Soochow
University (Suzhou, China) and were in strict accordance with
Declaration of Helsinki (1964). Informed consent to participate in
the study was obtained from the patients and their families.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mundi S, Pindiprolu B, Simunovic N and
Bhandari M: Similar mortality rates in hip fracture patients over
the past 31 years. Acta Orthop. 85:54–59. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kristek D, Lovric I, Kristek J, Biljan M,
Kristek G and Sakic K: The proximal femoral nail antirotation
(PFNA) in the treatment of proximal femoral fractures. Coll
Antropol. 34:937–940. 2010.PubMed/NCBI
|
|
3
|
Steiner JA, Ferguson SJ and Van Lenthe GH:
Computational analysis of primary implant stability in trabecular
bone. J Biomech. 48:807–815. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Grechenig S, Gänsslen A, Gueorguiev B,
Berner A, Müller M, Nerlich M and Schmitz P: PMMA-augmented SI
screw: A biomechanical analysis of stiffness and pull-out force in
a matched paired human cadaveric model. Injury. 46 (Suppl
4):S125–S128. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Schiuma D, Plecko M, Kloub M, Rothstock S,
Windolf M and Gueorguiev B: Influence of peri-implant bone quality
on implant stability. Med Eng Phys. 35:82–87. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Van Rietbergen B, Van Huiskes R, Eckstein
F and Rüegsegger P: Trabecular bone tissue strains in the healthy
and osteoporotic human femur. J Bone Miner Res. 18:1781–1788.
2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Broderick JM, Bruce-Brand R, Stanley E and
Mulhall KJ: Osteoporotic hip fractures: The burden of fixation
failure. ScientificWorldJournal. 2013(515197)2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Born CT, Karich B, Bauer C, von Oldenburg
G and Augat P: Hip screw migration testing: First results for hip
screws and helical blades utilizing a new oscillating test method.
J Orthop Res. 29:760–766. 2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bonnaire F, Weber A, Bösl O, Eckhardt C,
Schwieger K and Linke B: ‘Cutting out’ in pertrochanteric
fractures-problem of osteoporosis? Unfallchirurg. 110:425–432.
2007.(In German). PubMed/NCBI View Article : Google Scholar
|
|
10
|
Audigé L, Hanson B and Swiontkowski MF:
Implant-related complications in the treatment of unstable
intertrochanteric fractures: Meta-analysis of dynamic screw-plate
versus dynamic screw-intramedullary nail devices. Int Orthop.
27:197–203. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Konstantinidis L, Papaioannou C, Blanke P,
Hirschmüller A, Südkamp N and Helwig P: Failure after
osteosynthesis of trochanteric fractures. Where is the limit of
osteoporosis? Osteoporos Int. 24:2701–2706. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kang SR, Bok SC, Choi SC, Lee SS, Heo MS,
Huh KH, Kim TI and Yi WJ: The relationship between dental implant
stability and trabecular bone structure using cone-beam computed
tomography. J Periodontal Implant Sci. 46:116–127. 2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kuzyk PR, Zdero R, Shah S, Olsen M,
Waddell JP and Schemitsch EH: Femoral head lag screw position for
cephalomedullary nails: A biomechanical analysis. J Orthop Trauma.
26:414–421. 2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Goffin JM, Pankaj P and Simpson AH: The
importance of lag screw position for the stabilization of
trochanteric fractures with a sliding hip screw: A subject-specific
finite element study. J Orthop Res. 31:596–600. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bessho M, Ohnishi I, Matsumoto T, Ohashi
S, Matsuyama J, Tobita K, Kaneko M and Nakamura K: Prediction of
proximal femur strength using a CT-based nonlinear finite element
method: Differences in predicted fracture load and site with
changing load and boundary conditions. Bone. 45:226–231.
2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Watts NB: Fundamentals and pitfalls of
bone densitometry using dual-energy X-ray absorptiometry (DXA).
Osteoporos Int. 15:847–854. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Shim VB, Pitto RP and Anderson IA:
Quantitative CT with finite element analysis: Towards a predictive
tool for bone remodelling around an uncemented tapered stem. Int
Orthop. 36:1363–1369. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Black DM, Bouxsein ML, Marshall LM,
Cummings SR, Lang TF, Cauley JA, Ensrud KE, Nielson CM and Orwoll
ES: Osteoporotic Fractures in Men (MrOS) Research Group: Proximal
femoral structure and the prediction of hip fracture in men: A
large prospective study using QCT. J Bone Miner Res. 23:1326–1333.
2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Cheng X, Li J, Lu Y, Keyak J and Lang T:
Proximal femoral density and geometry measurements by quantitative
computed tomography: Association with hip fracture. Bone.
40:169–174. 2007.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Cheng XG, Lowet G, Boonen S, Nicholson PH,
Brys P, Nijs J and Dequeker J: Assessment of the strength of
proximal femur in vitro: Relationship to femoral bone mineral
density and femoral geometry. Bone. 20:213–218. 1997.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cody DD, Divine GW, Nahigian K and
Kleerekoper M: Bone density distribution and gender dominate
femoral neck fracture risk predictors. Skeletal Radiol. 29:151–161.
2000.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Cui WQ, Won YY, Baek MH, Lee DH, Chung YS,
Hur JH and Ma YZ: Age-and region-dependent changes in
three-dimensional microstructural properties of proximal femoral
trabeculae. Osteoporos Int. 19:1579–1587. 2008.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Dendorfer S, Maier HJ, Taylor D and Hammer
J: Anisotropy of the fatigue behaviour of cancellous bone. J
Biomech. 41:636–641. 2008.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Baumgaertner MR, Curtin SL, Lindskog DM
and Keggi JM: The value of the tip-apex distance in predicting
failure of fixation of peritrochanteric fractures of the hip. J
Bone Joint Surg Am. 77:1058–1064. 1995.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Jang IG and Kim IY: Computational study of
wolff's law with trabecular architecture in the human proximal
femur using topology optimization. J Biomech. 41:2353–2361.
2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Li B and Aspden RM: Material properties of
bone from the femoral neck and calcar femorale of patients with
osteoporosis or osteoarthritis. Osteoporos Int. 7:450–456.
1997.PubMed/NCBI View Article : Google Scholar
|