Introduction
Brucellosis is a zoonotic infectious disease caused
by infection with the bacterial genus Brucella.
Brucella are able to localize to phagocytic cells in human
organs including the liver, spleen, bone marrow and brain, thereby
leading to various clinical manifestations (1). Brucella suis (B. suis)
can cause devastating multi-organ diseases in humans, which lead to
severe health complications (2-4).
Previous studies have shown that Brucella has several
strategies to establish chronic infection, including inhibition of
apoptosis in infected mononuclear cells, inhibition of dendritic
cell maturation, and a reduction in the antigen presentation
ability and activation of naïve T-cells (5,6). One
possible strategy for treatment of B. suis infection is the
promotion of apoptosis in host cells. B. suis strain 2 is a
low virulence live-strain vaccine known to improve cellular
immunity and protect animals against infection by heterologous
virulent Brucella (7). The
properties of B. suis strain 2 make it a suitable model for
in vitro study of Brucella.
Mg2+/Mn2+ dependent protein
phosphatase 1A (PPM1A), a member of the serine/threonine
phosphatase family, is known to be a critical regulator of cellular
apoptosis (8). It has been shown
that PPM1A is a key factor in the innate antibacterial and
antiviral response of macrophages, particularly in Mycobacterium
tuberculosis infection (9,10). As
both Brucella and Mycobacterium tuberculosis
effectively function as intracellular parasites, sharing
similarities in their pathogenesis (11,12) it
is hypothesized in the present study that PPM1A may also regulate
apoptosis in B. suis infection.
Microglia, resident immune cells in the brain, are
involved in normal brain development and neuronal recovery
(13). It has been reported that
Brucella infection activates microglia and leads to neuronal loss,
thereby contributing to neurological deficits observed during
neurobrucellosis. In the present study, the role of PPM1A in the
regulation of apoptosis was investigated in BV2 cells, an
immortalized mouse cell line that models microglia, that had been
infected with B. suis strain 2.
Materials and methods
Cell lines and bacteria
Mouse microglia cell line BV2 cells were provided by
American Type Culture Collection and cultured in DMEM (Thermo
Fisher Scientific Inc.) containing 10% FBS (Hyclone; GE Healthcare
Life Sciences), 2 mM glutamine and 200 mM streptomycin/penicillin
(Beijing Solarbio Science and Technology Co., Ltd.) and maintained
in 5% CO2 at 37˚C. B. suis strain 2 was a kind
gift from Professor Xu of Ningxia Medical University (Yinchuan,
China) and was cultured on trypticase soy-agar plates at 37˚C in a
5% CO2 incubator. Individual B. suis strain 2
colonies were seeded in sterilized trypticase soy broth solution at
37˚C in 5% CO2. Bacteria were harvested by
centrifugation for 20 min at 2,000 g at 4˚C and washed twice with
PBS. Bacterial density in the culture was estimated using a
McFarland standards kit (bioMérieux China Ltd.). All experiments
involving bacteria were performed in a biosafety level 2
laboratory.
In vitro infection
BV2 cells (8x105) were grown in six-well
cell culture plates, allowed to reach 60% confluence, and then
exposed to B. suis strain 2 at multiplicity of infection
(MOI) 100 for 1 h in DMEM without antibiotics. Thereafter, BV2
cells were washed extensively, to remove extracellular bacteria.
The infection was maintained for 24 h in the presence of 100 µg/ml
gentamicin, to kill any remaining extracellular bacteria. Medium
and cells were collected for subsequent experiments. BV2 cells were
infected at different intervals (0, 4, 8 and 24 h) for western
blotting and at 24 for the remaining analysis. In addition, BV2
cells were also infected in shRNA experiments.
Cell viability assay
Cell viability was determined using a Cell Counting
Kit-8 (CCK-8) assay according to the manufacturer's protocol
(Nanjing Fengfeng Biomedical Technology Co., Ltd.). In brief,
uninfected BV2 cells were seeded in 96-well cell culture plates at
a density of 1x104 cells/ml and cultured overnight at
37˚C. Cells were treated with SP600125 (MedChemExpress; 5 and 10
µM) and anisomycin (MedChem Express; 0.2, 0.5 and 1 µM) for 24 h.
Cells treated with DMSO served as controls. Subsequently, CCK-8
solution was added to each well and incubated for an additional 4
h. The absorbance at 450 nm was measured using a microplate reader
(BioTek Instruments, Inc.).
Short hairpin (sh)RNA expression
constructs and virus infection
Lentiviral vector GV493 and an shRNA plasmid coding
for PPM1A were purchased from Shanghai Genechem Co., Ltd. The shRNA
targeting PPM1A had the sequence 5'-GAGAGTTATGTCAGAGAAGAA-3'. The
scrambled RNA sequence, used as a control, had the sequence
5'-TTCTCCGAACGTGTCACGT-3'. BV2 cells were infected with viruses
expressing control shRNA or shRNA targeting PPM1A at MOI 50. BV2
cells were used 72 h after transfection, and stable cell lines were
established as previously described and were selected for 5 days
using puromycin (Sigma-Aldrich; Merck KGaA; 2 µg/ml) (14).
Flow cytometry
BV2 cells (1x105 cells) were treated with
5 µM SP600125 or 0.2 µM anisomycin at 37˚C for 48 h and stained
with annexin V conjugated to FITC or propidium iodide according to
the manufacturer's protocol (cat. no. BB-4101-1; Nanjing Fengfeng
Biomedical Technology Co., Ltd.). Apoptosis was determined by flow
cytometry using a BD Accuri C6. Data analysis was performed using
BD Accuri CTM 6 software Plus (BD Biosciences).
Western blot analysis
BV2 cells were harvested, washed twice with PBS, and
lysed in RIPA buffer (Nanjing Jiancheng Bioengineering Institute).
Protein concentrations in the lysates were quantified by the
bicinchoninic acid method following the manufacturer's instructions
(Nanjing KeyGen Biotech Co., Ltd.). A total of 30 µg of protein per
sample was loaded and separated on 12% Mini-Protean®
TGX™ gels (Bio-Rad Laboratories, Inc.) and subsequently transferred
onto a polyvinylidene difluoride membrane. Prior to antibody
incubations, the samples were blocked with 5% skimmed milk at room
temperature for 1 h. PPM1A (dilution 1:1,000; cat. no. ab14824),
JNK (dilution 1:1,000; cat. no. ab179461), phosphorylated (p)-JNK
(dilution 1:3,000; cat. no. ab4821), caspase-3 (dilution 1:1,000;
cat. no. ab13847), cleaved caspase-3 (dilution 1:500; cat. no.
ab2302) and GAPDH (dilution 1:1,000; cat. no. ab181602) protein
levels were assessed using specific antibodies (Abcam) at 4˚C
overnight. Horseradish peroxidase-conjugated goat anti-mouse
polyclonal antibody (dilution 1:5,000; Santa Cruz Biotechnology,
Inc.; cat. no. sc-2031) was used as the secondary antibody for 30
min at room temperature. The blot was developed using Western
Lightning Ultra chemiluminescent substrate (Bio-Rad Laboratories,
Inc.) in an EpiChemi3 darkroom (UVP, LLC). Image Lab 3.0 software
used to analyze the results (Bio-Rad Laboratories, Inc.).
DAPI staining
BV2 cells were seeded on six-well plates at a
density of 5x105 cells/ml and cultured overnight at
37˚C. Cells were fixed in 4% paraformaldehyde at room temperature
for 1 h. After washing with PBS and air-drying for 3 min at room
temperature, cells were stained with DAPI at room temperature for 1
min and images were captured using fluorescence microscopy
immediately (x200 magnification, 6 random field were viewed).
Statistical analysis
All data are presented as the mean ± SD from at
least three independent experiments. Graphpad Prism 7.0 (GraphPad
Software, Inc.) was used for the analysis. Comparisons between
indicated groups were performed using one-way analysis of variance
followed by Tukey's post-hoc test. P<0.05 was considered to
indicate a statistically significant difference.
Results
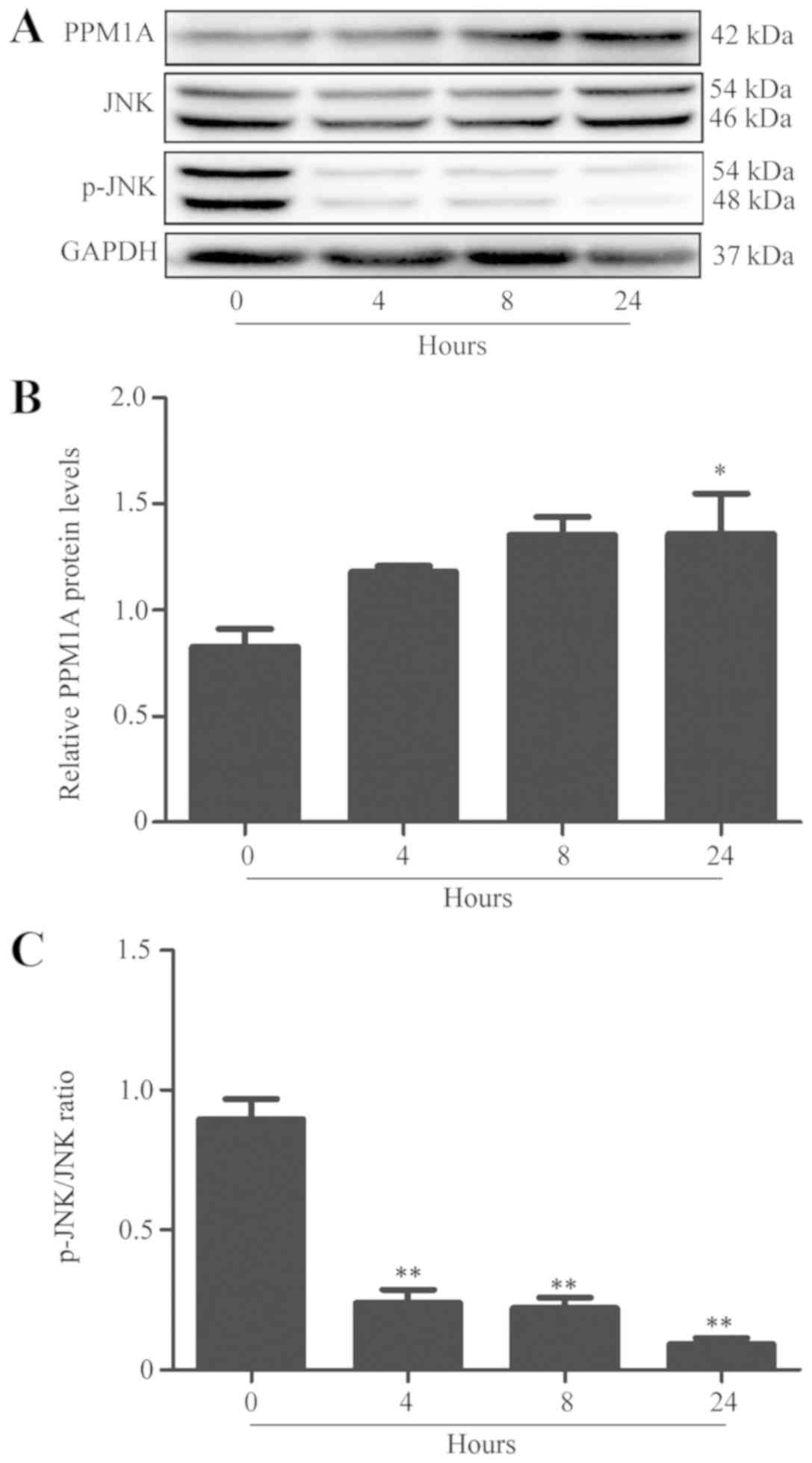
Increased expression of PPM1A and
reduced phosphorylation of JNK are observed in B. suis strain
2-infected BV2 cells
The expression of PPM1A and JNK proteins was
evaluated by western blot analysis in BV2 cells at 4, 8 and 24 h
post-B. suis strain 2 infection. The results indicated that
PPM1A expression was significantly increased and phosphorylation of
JNK was significantly reduced in a time-dependent manner compared
with control shRNA-infected cells (Fig.
1).
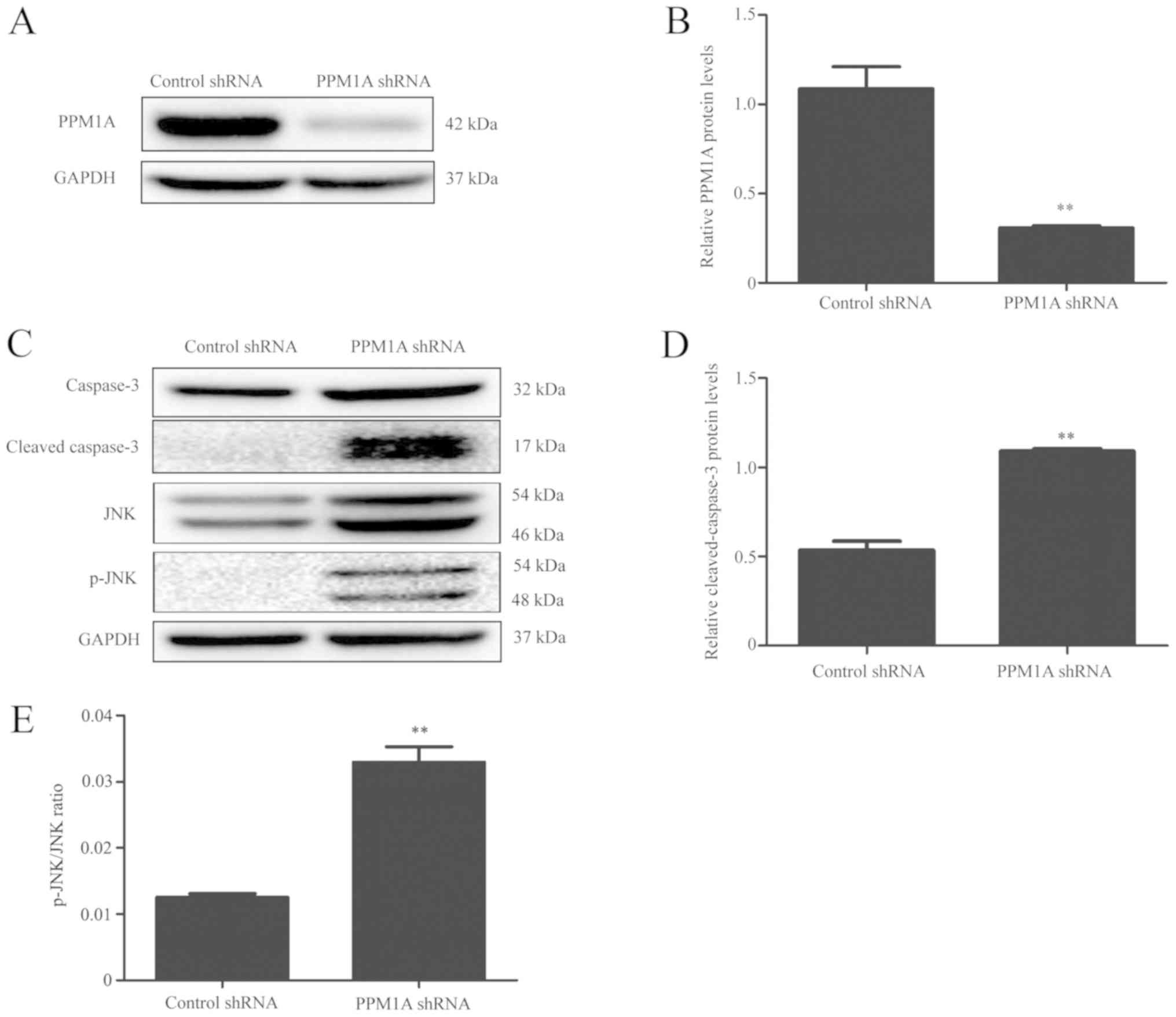
PPM1A knockdown promotes
caspase-dependent apoptosis in uninfected BV2 cells
To further characterize the role of PPM1A in
apoptosis regulation, RNA interference was used to knock down PPM1A
expression in BV2 cells. The results indicated that PPM1A protein
levels in cells transfected with shRNA specific for PPM1A were
significantly reduced compared with those transfected with control
shRNA (Fig. 2A and B). This suggested that shRNA targeting
PPM1A mRNA could effectively knockdown PPM1A expression at a
translational level. Compared with control shRNA cells, the protein
expression levels of cleaved caspase-3 were markedly increased in
PPM1A shRNA-transfected BV2 cells (Fig.
2C and D). Collectively, these
results suggested that knockdown of PPM1A promoted
caspase-dependent apoptosis in BV2 cells.
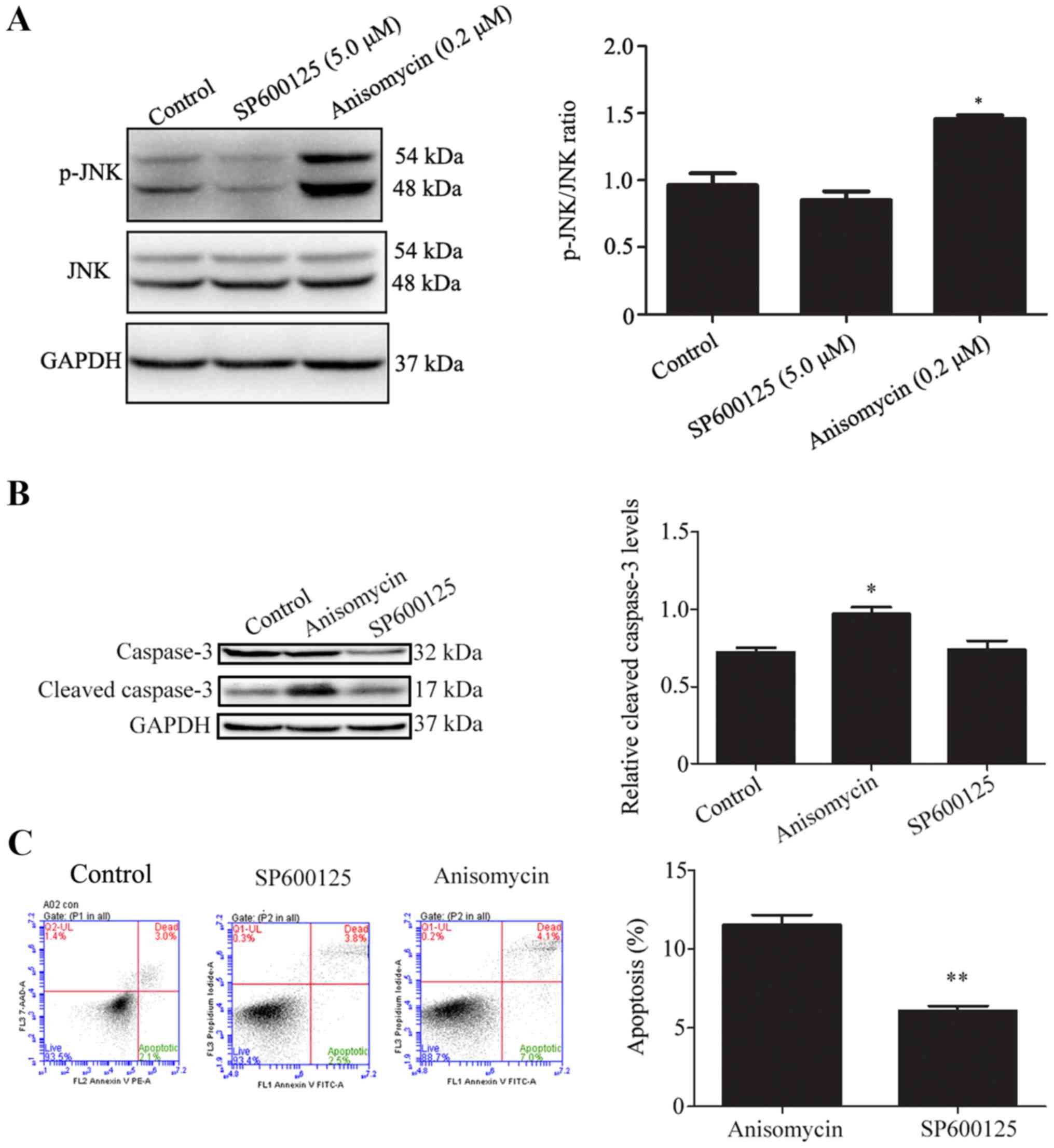
Activation of JNK signaling promotes
apoptosis in BV2 cells
To determine whether JNK signaling was involved in
apoptosis, uninfected BV2 cells were treated with the JNK inhibitor
SP100625 or JNK activator anisomycin. The CCK-8 assay showed that
treatment with SP600125 at 5 µM or anisomycin at 0.2 µM had no
significant effect on BV2 cell viability compared with DMSO-treated
cells (data not shown). Western blot analysis showed that SP100625
appeared to reduce and anisomycin markedly increased the levels of
JNK phosphorylation in BV2 cells (Fig.
3A). In comparison to vehicle treated cells, the levels of
cleaved caspase-3 were significantly increased in BV2 cells treated
with anisomycin, but not altered in those treated with SP100625
(Fig. 3B). To further investigate
the effects of JNK signaling modulation on apoptosis in BV2 cells,
flow cytometry analysis was performed to detect apoptosis in BV2
cells treated with SP600125 or anisomycin. Treatment with
anisomycin significantly increased apoptosis levels in BV2 cells
compared with that of the SP600125 treated cells (Fig. 3C).
Knockdown of PPM1A induces activation
of JNK signaling in BV2 cells
To investigate whether PPM1A regulates JNK
phosphorylation, the protein levels of JNK and p-JNK were measured
using western blot analysis in BV2 cells transfected with PPM1A
shRNA. The results indicated that the level of p-JNK in PPM1A shRNA
transfected cells was significantly higher than that in control
shRNA transfected cells (Fig. 2E),
suggesting that PPM1A knockdown activates JNK signaling in BV2
cells.
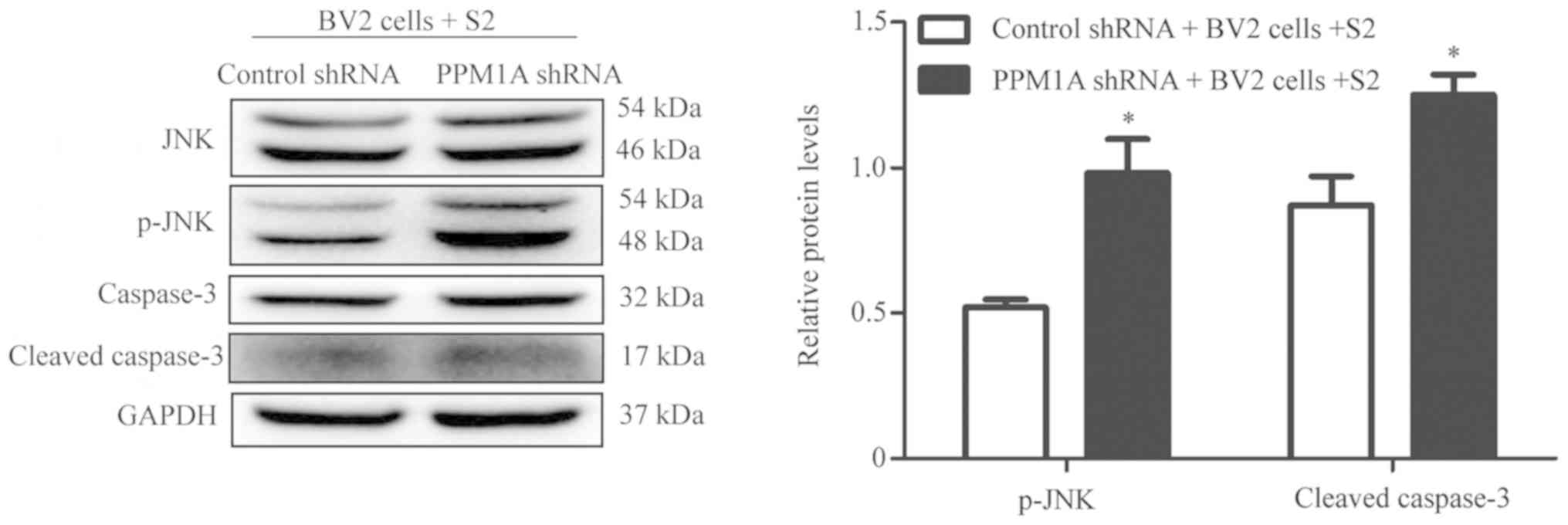
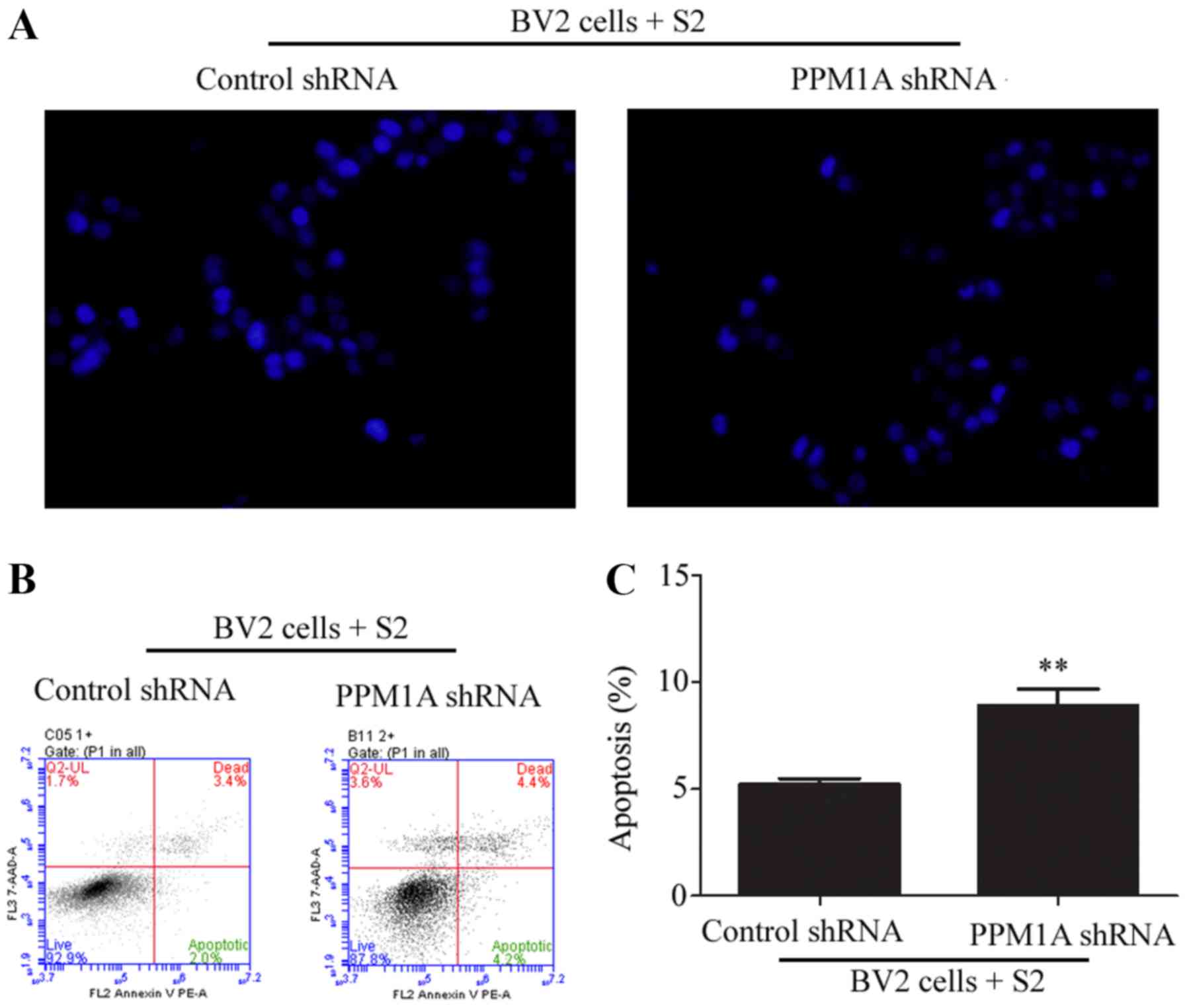
Knockdown of PPM1A promotes apoptosis
in BV2 cells infected with B. suis strain 2
The protein levels of JNK, p-JNK, caspase-3 and
cleaved caspase-3 were assessed in BV2 cells infected with B.
suis strain 2 and transfected with PPM1A shRNA. As shown in
Fig. 4, PPM1A shRNA significantly
increased the ratios of p-JNK/JNK and the expression levels of
cleaved caspase-3 in BV2 cells infected with B. suis strain
2 compared with control cells. Additionally, flow cytometry
analysis showed that PPM1A shRNA significantly increased the level
of apoptosis in BV2 cells infected with B. suis strain 2
compared with cells treated with control shRNA (Fig. 5A and B). Taken together, these data suggest that
knockdown of PPM1A promotes apoptosis in BV2 cells infected with
B. suis strain 2.
Discussion
Brucella is an intracellular parasite, which
previously, the authors of the current study have reported that the
outer membrane protein of Brucella inhibits host cell
apoptosis (15), facilitating the
replication of bacteria within the cell. In the present study,
knockdown of PPM1A promoted apoptosis in BV2 cells infected with
B. suis strain 2. Therefore, it is plausible to propose that
PPM1A reduces intracellular replication of B. suis strain 2
by inducing apoptosis in BV2 cells.
Protein phosphatases are enzymes that catalyze the
dephosphorylation of protein molecules in contrast to protein
kinases, which phosphorylate proteins. PPM1A is a protein
phosphatase, widely present in eukaryotic cells. PPM1A participates
in the regulation of the cell cycle, apoptosis, antiviral and other
related biological functions (16-18).
In the present study, PPM1A was upregulated in BV2 cells infected
with B. suis strain 2, and knockdown of PPM1A shown to
promote apoptosis. PPM1A may be a potential target to promote the
apoptosis of Brucella-infected cells. In addition, JNK was
suggested to be a substrate for PPM1A, and increased
phosphorylation of JNK can promote apoptosis. These findings
indicate that the PPM1A-JNK pathway may be involved in the
regulation of BV2 apoptosis after B. suis strain 2
infection. Based on these results, a further study will be focused
on the screening of drugs that inhibit PPM1A in vitro and
observation of whether these drugs can enhance the efficacy of
antibacterial therapy.
Brucellosis is more severe in humans than in
domestic animals and causes a variety of clinical symptoms
(3), including central nervous
system infection related symptoms (19,20). The
incidence of brucellosis is higher in areas of intensive
agriculture and animal husbandry, including Ningxia, China
(21,22).
Brucella is a common zoonotic pathogen that
can survive and proliferate within several types of phagocytic and
non-phagocytic cells. Phagocytic cells are the main host and
Brucella can inhibit apoptosis of these cells (23). In the absence of effective
antibiotics treatment, 50% of brucellosis cases become chronic and
cause multiple organ damage, including neurological disorders, bone
destruction and cardiovascular damage (24,25).
Meningitis is a common cause of fatality in brucellosis (26,27).
Improving antibiotic treatment and reducing infection recurrence is
the ultimate goal in brucellosis treatment. In the current study,
the PPM1A-JNK pathway was revealed to be involved in the regulation
of BV2 cell apoptosis after B. suis strain 2 infection.
Whether PPM1A knockdown can reduce bacterial replication by
promoting apoptosis needs to be further explored.
There are several limitations to the present study.
Whether only B. suis strain 2-infected BV2 cells undergo
apoptosis by PPM1A protein expression knockdown has not been
elucidated, as it is difficult to distinguish B. suis strain
2-infected BV2 cells from uninfected cells. Additionally, the
similarity between the B. suis strain 2 vaccine used in the
present study and wild-type Brucella has not been confirmed
by sequencing results. This study may inspire the development of
new Brucella treatments that promote the apoptosis of host
cells, so as to reduce the recurrence of infection.
Acknowledgements
Not applicable.
Funding
The current study was supported by grants from the
National Natural Science Foundation of China (grant no. 31660030)
and the First Class Discipline Construction Project in Colleges and
Universities of Ningxia (grant no. NXYLXK2017A05).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JY, GW, HL and ZW conceived and designed the
experiments. JY, GW, and HL conducted all the experiments. WZ and
BG contributed to the design of parts of the study and collected
and analyzed some of the data. All authors read and approved the
final manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Vollmar P, Zange S, Zöller L, Erkel J and
Robert Thoma B: Brucellosis, an overview and current aspects. Dtsch
Med Wochenschr. 141:1014–1018. 2016.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
2
|
Zheng R, Xie S, Lu X, Sun L, Zhou Y, Zhang
Y and Wang K: A systematic review and meta-analysis of epidemiology
and clinical manifestations of human brucellosis in China. Biomed
Res Int. 2018(5712920)2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Galinska EM and Zagorski J: Brucellosis in
humans-etiology, diagnostics, clinical forms. Ann Agric Environ
Med. 20:233–238. 2013.PubMed/NCBI
|
|
4
|
Pelerito A, Cordeiro R, Matos R, Santos
MA, Soeiro S, Santos J, Manita C, Rio C, Santo M, Paixão E, et al:
Human brucellosis in portugal-retrospective analysis of suspected
clinical cases of infection from 2009 to 2016. PLoS One.
12(e0179667)2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Elfaki MG, Alaidan AA and Al-Hokail AA:
Host response to brucella infection: Review and future perspective.
J Infect Dev Ctries. 9:697–701. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Miller CN, Smith EP, Cundiff JA, Knodler
LA, Bailey Blackburn J, Lupashin V and Celli J: A brucella type iv
effector targets the cog tethering complex to remodel host
secretory traffic and promote intracellular replication. Cell Host
Microbe. 22:317–329. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Carvalho TF, Haddad JP, Paixão TA and
Santos RL: Meta-Analysis and advancement of brucellosis
vaccinology. PLoS One. 11(e0166582)2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Schaaf K, Smith SR, Duverger A, Wagner F,
Wolschendorf F, Westfall AO, Kutsch O and Sun J: Mycobacterium
tuberculosis exploits the PPM1A signaling pathway to block host
macrophage apoptosis. Sci Rep. 7(42101)2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sun J, Schaaf K, Duverger A, Wolschendorf
F, Speer A, Wagner F, Niederweis M and Kutsch O: Protein
phosphatase, Mg2+/Mn2+-dependent 1A controls the innate antiviral
and antibacterial response of macrophages during HIV-1 and
mycobacterium tuberculosis infection. Oncotarget. 7:15394–15409.
2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Xiang W, Zhang Q, Lin X, Wu S, Zhou Y,
Meng F, Fan Y, Shen T, Xiao M, Xia Z, et al: PPM1A silences
cytosolic RNA sensing and antiviral defense through direct
dephosphorylation of MAVS and TBK1. Sci Adv.
2(e1501889)2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Siqueira MDS, Ribeiro RM and Travassos LH:
Autophagy and its interaction with intracellular bacterial
pathogens. Front Immunol. 9(935)2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Li Y, Wei C, Xu H, Jia J, Wei Z, Guo R,
Jia Y, Wu Y, Li Y, Qi X, et al: The immunoregulation of Th17 in
host against intracellular bacterial infection. Mediators Inflamm.
19(6587296)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Heppner FL, Ransohoff RM and Becher B:
Immune attack: The role of inflammation in alzheimer disease. Nat
Rev Neurosci. 16:358–372. 2015.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Yang J, Zhang J, Xu T, Wang Y and Wang Z:
Establishment of BV2 cell line with steady knockdown of
Mg2+/Mn2+-dependent protein phosphatase
1A(PPM1A). Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 34:818–823.
2018.PubMed/NCBI(In Chinese).
|
|
15
|
Ma QL, Liu AC, Ma XJ, Wang YB, Hou YT and
Wang ZH: Brucella outer membrane protein Omp25 induces microglial
cells in vitro to secrete inflammatory cytokines and inhibit
apoptosis. Int J Clin Exp Med. 8:17530–17535. 2015.PubMed/NCBI
|
|
16
|
Smith SR, Schaaf K, Rajabalee N, Wagner F,
Duverger A, Kutsch O and Sun J: The phosphatase PPM1A controls
monocyte-to-macrophage differentiation. Sci Rep.
8(902)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wang Y, Dow EC, Liang YY, Ramakrishnan R,
Liu H, Sung TL, Lin X and Rice AP: Phosphatase PPM1A regulates
phosphorylation of thr-186 in the Cdk9 T-loop. J Biol Chem.
283:33578–22584. 2008.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sun W, Yu Y, Dotti G, Shen T, Tan X,
Savoldo B, Pass AK, Chu M, Zhang D, Lu X, et al: PPM1A and PPM1B
act as IKKbeta phosphatases to terminate TNFalpha-induced
IKKbeta-NF-kappaB activation. Cell Signal. 21:95–102.
2009.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Levy J, Shneck M, Marcus M and Lifshitz T:
Brucella meningitis and papilledema in a child. Eur J Ophthalmol.
15:818–820. 2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Haji-Abdolbagi M, Rasooli-Nejad M, Jafari
S, Hasibi M and Soudbakhsh A: Clinical and laboratory findings in
neurobrucellosis: Review of 31 cases. Arch Iran Med. 11:21–25.
2008.PubMed/NCBI
|
|
21
|
Li YJ, Li XL, Liang S, Fang LQ and Cao WC:
Epidemiological features and risk factors associated with the
spatial and temporal distribution of human brucellosis in China.
BMC Infect Dis. 13(547)2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lai S, Zhou H, Xiong W, Gilbert M, Huang
Z, Yu J, Yin W, Wang L, Chen Q, Li Y, et al: Changing epidemiology
of human brucellosis, China, 1955-2014. Emerg Infect Dis.
23:184–194. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Deng Y, Liu X, Duan K and Peng Q: Research
progress on brucellosis. Curr Med Chem. 26:5598–5608. 2018.
|
|
24
|
Tu L, Liu X, Gu W, Wang Z, Zhang E, Kahar
A, Chu G and Zhao J: Imaging-assisted diagnosis and characteristics
of suspected spinal brucellosis: A retrospective study of 72 cases.
Med Sci Monit. 24:2647–2654. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sabzi F and Faraji R: Brucella
pericarditis: A forgotten cause of chest pain. Caspian J Intern
Med. 8:116–118. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Olsen SC and Palmer MV: Advancement of
knowledge of brucella over the past 50 years. Vet Pathol.
51:1076–1089. 2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Moreno E and Moriyon I: Brucella
melitensis: A nasty bug with hidden credentials for virulence. Proc
Natl Acad Sci USA. 99:1–3. 2002.PubMed/NCBI View Article : Google Scholar
|