Introduction
Hip fracture, especially femoral neck fractures, is
common in elderly patients caused by osteoporosis and trauma
(1). Due to anatomical reasons, the
femoral head is prone to a lack of blood supply after fracture,
resulting in osteonecrosis and bone nonunion (2). Senile femoral neck fractures are mainly
caused by osteoporosis and the incidence of femoral neck fracture
is higher in women than that in men (3). The occurrence of femoral neck fracture
is usually caused by a combination of many factors. The femoral
neck is on the border between the osteoporosis bone and compact
bone where the structure is fragile. In addition, the elderly tend
to have various defects in the body, such as calcium phosphate
imbalance and osteoporosis. Therefore, the elderly are prone to
fracture when exposed to mild external direct or indirect violence,
and osteoporosis is the most significant factor (4).
Hemiarthroplasty is a routine treatment in Garden
III and Garden IV femoral neck fracture. However, a number of
scholars believe that, although the incidence of complications of
cemented hemiarthroplasty is low, it may result in cardiovascular
and cerebrovascular complications (5). Various experts believe that uncemented
hemiarthroplasty has certain advantages in regards to operation
time and intraoperative blood loss (6). Therefore, the use of bone cement or
uncemented hemiarthroplasty fixation is still controversial. This
meta-analysis was designed to collect and analyze randomized
controlled trials (RCTs) to compare the differences between the two
fixation methods in regards to the operation time, intraoperative
blood loss, length of hospital stay, postoperative complications
and postoperative mortality in the treatment of elderly femoral
neck fractures, so as to provide references for the selection of
clinical prosthesis implantation.
Patients and methods
Search strategy
Two reviewers searched databases independently
including Pubmed (https://www.ncbi.nlm.nih.gov/pubmed/), Embase
(https://www.embase.com/), Cochrane Library
(https://www.cochranelibrary.com/), CNKI
(https://www.cnki.net/) and WANFANG (http://www.wanfangdata.com.cn/index.html) databases.
The search terms included ‘Hip fractures’, ‘Femoral fractures,
‘Femoral neck fractures’, ‘Hemiarthroplasty’, ‘Artificial Femoral
head replacement’, ‘Cemented or Cement’, ‘Uncementor without bone
cement’, ‘Noncemented or uncemented’ and ‘Biotype or cementless’.
The retrieval time was from inception to February, 2019.
Inclusion and exclusion criteria
Inclusion criteria included: i) subjects aged 60
years or older with femoral neck fractures; ii) the intervention
measures were cemented or uncemented hemiarthroplasty; iii) the
study type was clinical prospective RCT.
Exclusion criteria included: i) low quality or
non-RCT; ii) studies that failed to obtain original texts or
accurately extract data; iii) subject age <60 years; iv)
repeated literature; v) patients undergoing secondary surgery for
the same disease.
Data extraction and quality
assessment
Two reviewers independently screened the literature
and extracted data. Concerning controversial literature, a third
reviewer decided whether to include a study or not. The data
extracted included baseline data and outcome indicators.
The modified Jadad scale (7) was used to evaluate the quality of the
included studies. Blinding, randomization, concealment allocation
and withdrawal in the study were analyzed respectively. The total
score is 7. Studies with scores more than or equal to 4 are
considered high-quality, and those with scores less than 4 are
considered low-quality. Extremely low-quality studies were excluded
to ensure the reliability of the meta-analysis results.
Outcome indicators
All the outcome indicators are as follows (and
indicated in Table I with small
letters): a) periprosthetic fractures; b) postoperative joint
dislocation; c) time of operation; d) incision infection; e)
intraoperative blood loss; f) length of hospital stay; g)
postoperative cerebrovascular accident; h) postoperative myocardial
infarction; i) postoperative pulmonary infection; j) pulmonary
embolism; k) postoperative urinary tract infection; l)
postoperative deep vein thrombosis; m) mortality within six months
after surgery; n) mortality within one year after surgery.
 | Table IBaseline characteristics of the
included studies. |
Table I
Baseline characteristics of the
included studies.
| Studies First
author, year (Ref.) | Country | No. of patients
(cemented/uncemented) | Mean age
(cemented/uncemented) (years) | Follow-up time
(months) | Outcomes |
|---|
| Deangelis,
2012(9) | USA | 66/64 | 81.8/82.8 | 12 | e,m,n |
| Du, 2014(23) | China | 47/47 | 74.5/74.2 | 12 | a,b,c,d,e,i,k |
| Emery,
1991(10) | UK | 27/26 | 80/81 | 17 | c,d,j,l,n |
| Figved,
2009(11) | Norway | 112/108 | 83.4/83.0 | 12 |
a,b,c,d,e,h,i,j,m,n |
| Inngul,
2015(12) | Sweden | 67/74 | 81.2/81.3 | 12 |
a,b,d,e,h,i,k,m,n |
| Khorami,
2016(14) | Iran | 22/29 | 79/71.7 | 6 | a,b,d,g,k |
| Langslet,
2014(15) | Norway | 111/108 | 83.4/83.0 | 12 | c,e,f,m,n |
| Li, 2017(13) | China | 35/35 | 76.4/77.2 | 6 | a,c,e,f,g,l |
| Ma, 2016(8) | China | 30/30 | 66.2/68.7 | 12 | a,b,c,d,e,f,l |
| Moerman,
2017(16) | Netherland | 110/91 | 84/84 | 12 |
a,b,d,e,g,h,i,j,k,l,n |
| Pan, 2013(18) | China | 38/35 | 70.5/72.2 | - | c,d,e,i,l |
| Parker,
2010(17) | England | 200/200 | 83/83 | 24 |
b,c,d,f,g,h,j,l,n |
| Sonne-Holm,
1983(19) | Denmark | 55/57 | 82.1/82.2 | 12 | m,n |
| Talsnes,
2013(20) | Norway | 162/172 | 84.3/84.0 | 12 | c,e,n |
| Taylor,
2012(21) | New Zealand | 80/80 | 85.3/85.1 | 24 |
a,b,c,d,e,f,g,k,m |
| Vidović,
2015(22) | Croatia | 30/30 | - | 12 | f,n |
Statistical analysis
Meta-analysis of the extracted data was performed
using the RevMan 5.3 software (https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman)
recommended by the Cochrane collaboration (London, UK). We
calculated the odds ratio (OR) and 95% confidence interval (CI) for
the count data, and calculated the weighted mean difference (WMD)
and 95% CI for the measurement data. I2 was used to test
for heterogeneity. P<0.05 and I2>50% indicated the
heterogeneity of each study. We analyzed the cause of the
heterogeneity and used the random effect model for analysis. If
P>0.05 and I2<50%, the heterogeneity of a study
was low and we used the fixed-effect model for analysis. Funnel
plots were used to analyze publication bias of the included
studies. Studies with significant publication bias were
excluded.
Results
Study selection and study
characteristics
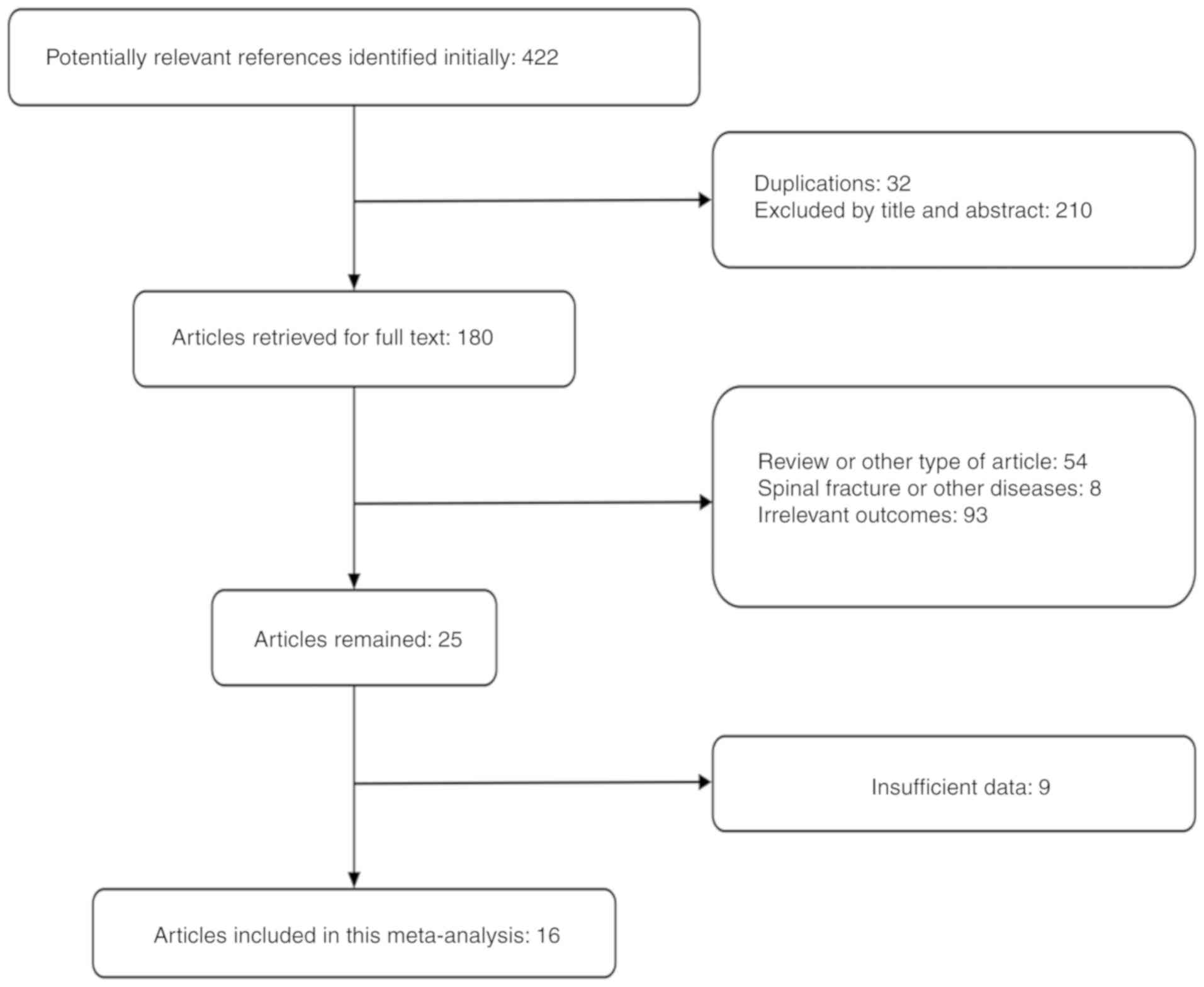
We initially searched 422 articles and finally
included 16 studies (8-23),
including 1,194 cases in the cemented group and 1,190 cases in the
uncemented group. The literature screening process is shown in
Fig. 1. Baseline information of the
included studies is documented in Table
I.
Results of the meta-analysis
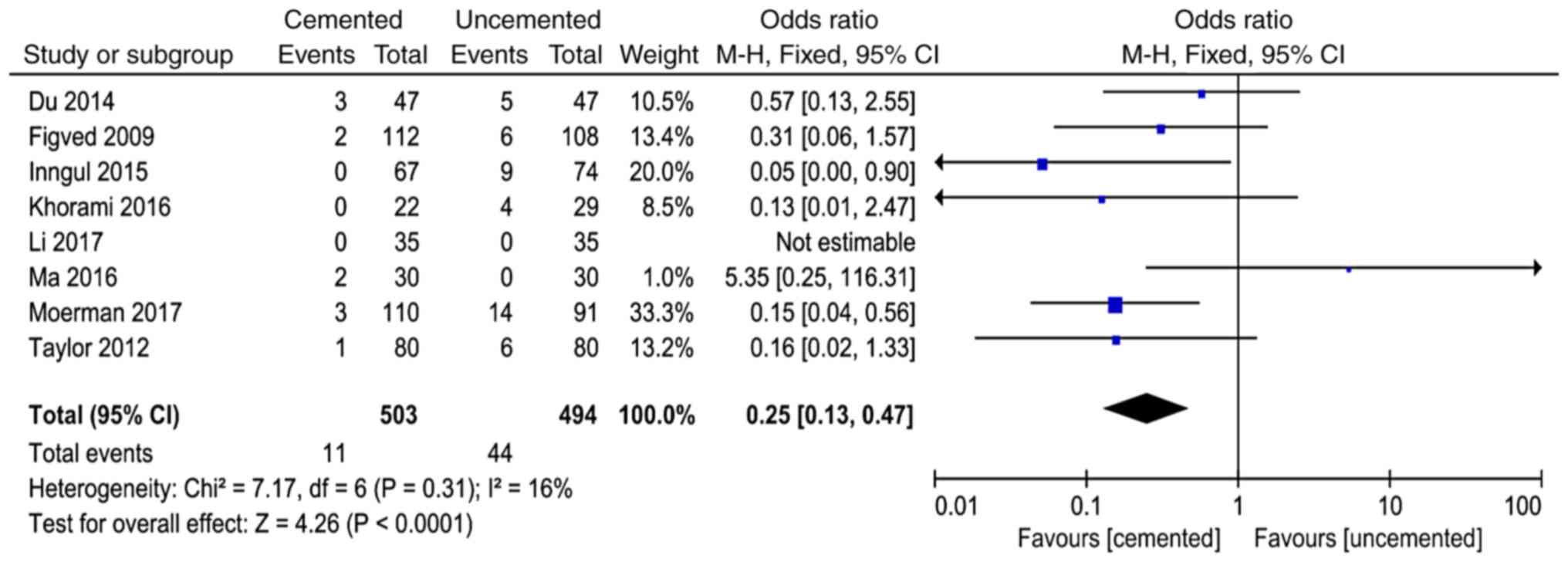
Periprosthetic fractures
A total of 8 studies (8,11-14,16,21,23)
reported periprosthetic fractures and 997 cases were included in
the analysis. There was no significant heterogeneity in the results
of the studies (P=0.31, I2=16%). The fixed-effect model
was used for analysis and the results showed that the incidence of
periprosthetic fractures in the cemented group was lower than that
in the uncemented group (OR=0.25, 95% CI=0.13-0.47, P<0.0001;
Fig. 2).
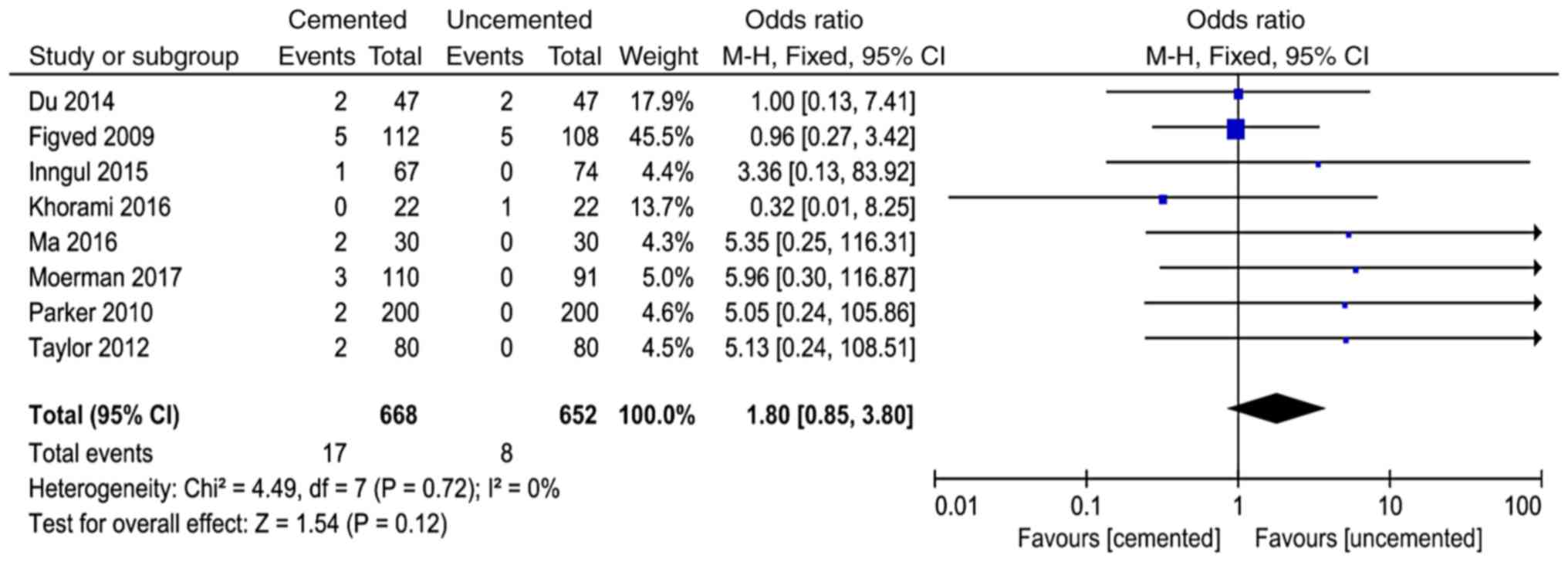
Postoperative joint dislocation
A total of 8 studies in the literature (8,11,12,14,16,17,21,23)
reported postoperative joint dislocation and 1,320 cases were
included in the analysis. There was no significant heterogeneity in
the results of various studies (P=0.72, I2=0%).
The fixed-effect model was used for analysis and the results showed
that there was no significant difference between the two groups in
the incidence of joint dislocation after surgery (OR=1.80, 95%
CI=0.85-3.80, P<0.12; Fig.
3).
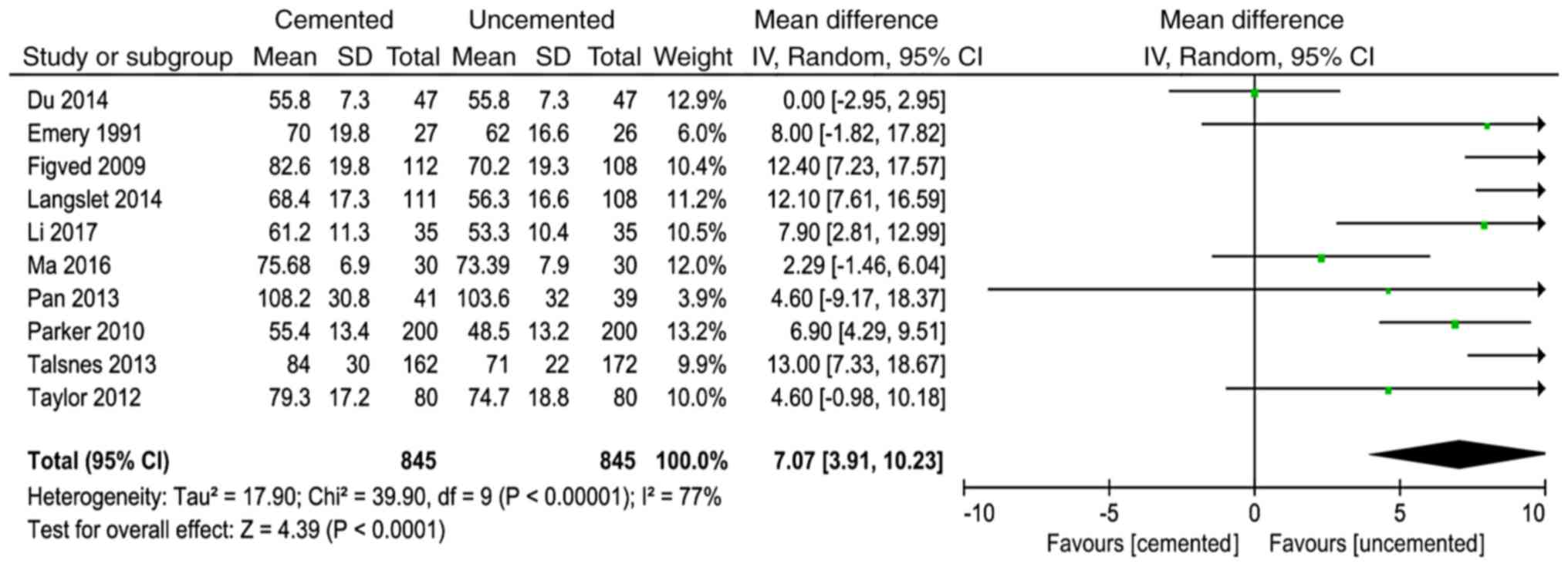
Time of operation
A total of 10 studies (8,10,11,13,15,17,18,20,21,23)
reported time of operation and 1,691 cases were included in the
analysis. There was significant heterogeneity in the results of the
studies (P<0.00001, I2=77%). The random effect model
was used for analysis and the results showed that the time of
operation in the cemented group was longer than that in the
uncemented group (WMD=7.07, 95% CI=3.91-10.23, P<0.0001;
Fig. 4).
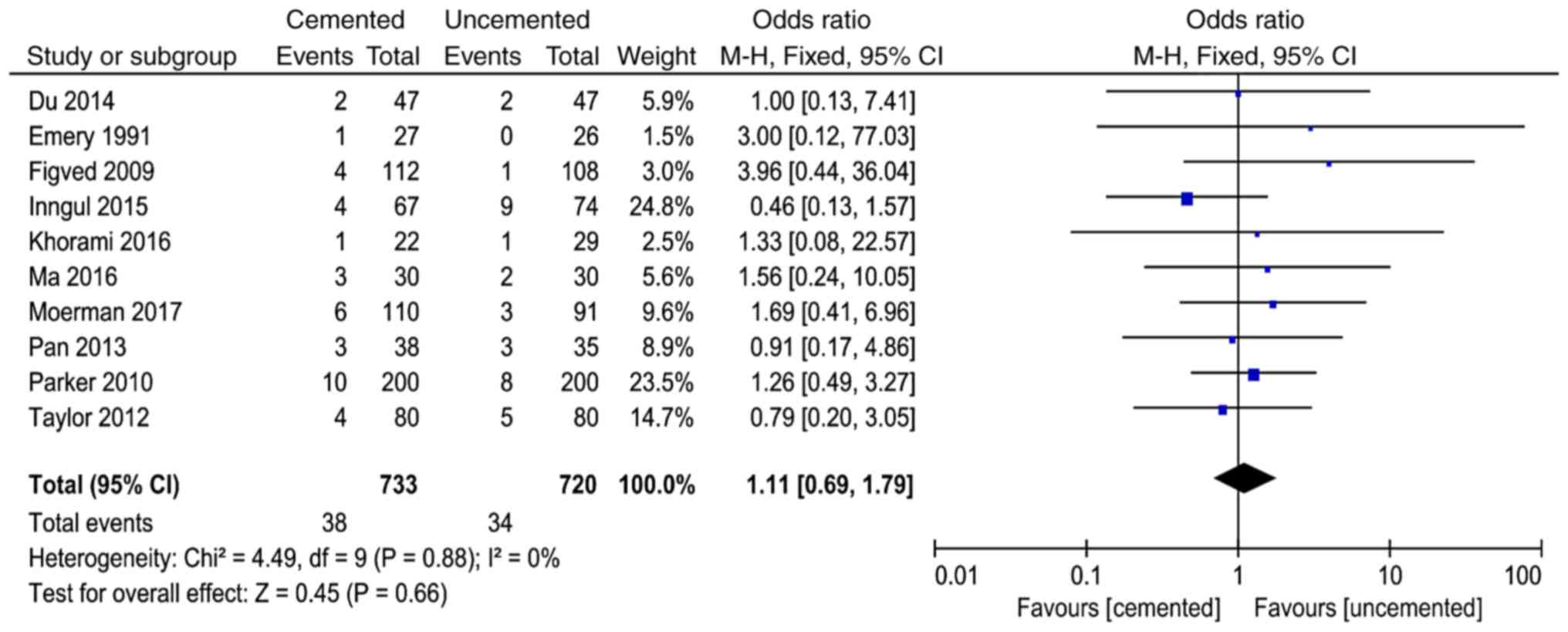
Incision infection
A total of 10 studies (8,10-12,14,16-18,21,23)
reported incision infection and 1,453 cases were included in the
analysis. There was no significant heterogeneity in the results of
the studies (P<0.88, I2=0%). The fixed-effect model
was used for analysis and the results showed that here was no
significant difference between the two groups in the incidence of
incision infection (OR=1.11, 95% CI=0.69-1.79, P=0.66; Fig. 5).
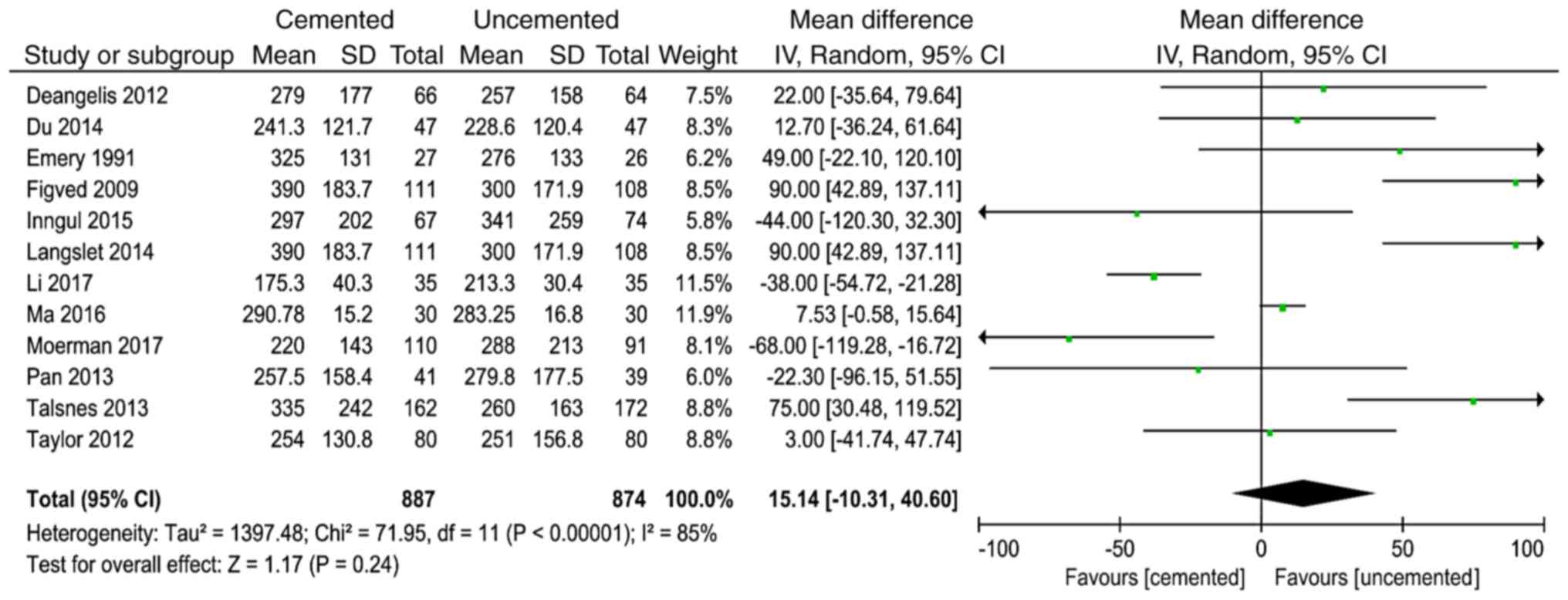
Intraoperative blood loss
A total of 12 studies (8-13,15,16,18,20,21,23)
reported intraoperative blood loss and 1,761 cases were included in
the analysis. There was significant heterogeneity in the results of
the studies (P<0.00001, I2=85%). The random effect
model was used for analysis and the results showed that there was
no significant difference between the two groups in the
intraoperative blood loss (WMD=15.14, 95% CI=-10.31-40.60, P=0.24;
Fig. 6).
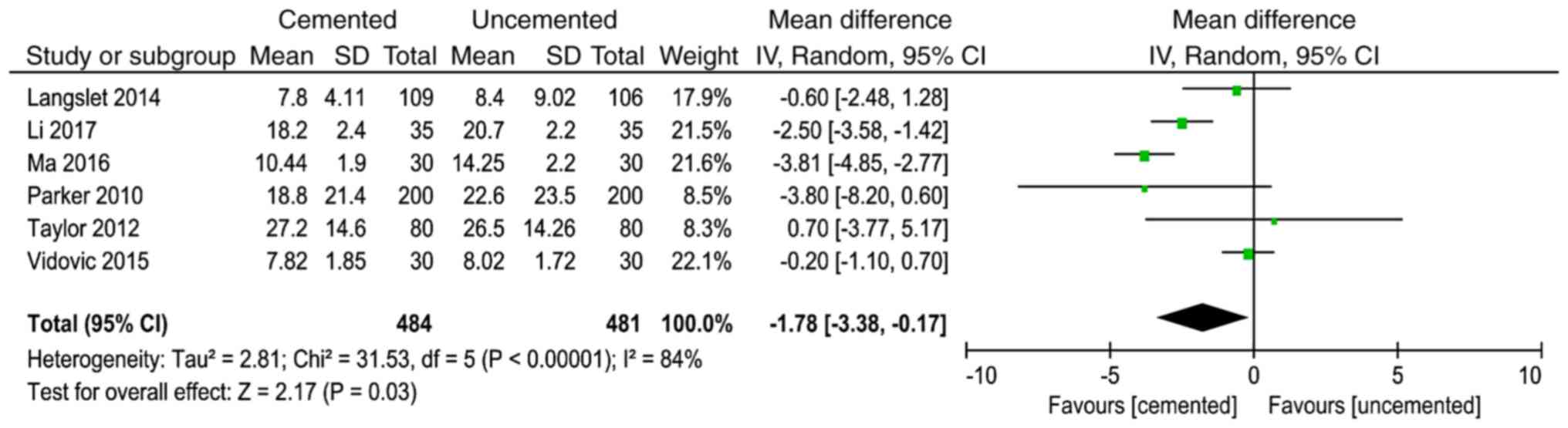
Length of hospital stay
A total of 6 studies (8,13,15,17,21,22)
reported the length of hospital stay and 968 cases were included in
the analysis. There was significant heterogeneity in the results of
the studies (P<0.00001, I2=84%). The random effect
model was used for analysis and the results showed that the length
of hospital stay in the cemented group was less than that in the
uncemented group (WMD=-1.78, 95% CI=-13.38--0.17, P=0.03) (Fig. 7).
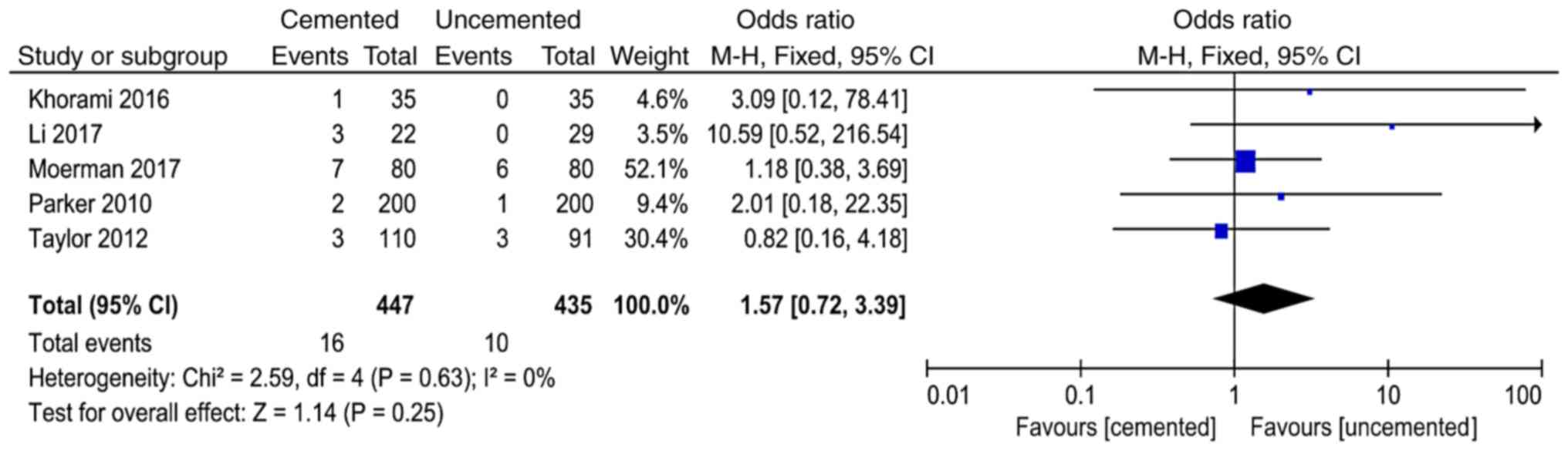
Postoperative cerebrovascular
accident
A total of 5 studies (13,14,16,17,21)
reported postoperative cerebrovascular accident and 882 cases were
included in the analysis. There was no significant heterogeneity in
the results of the studies (P=0.63, I2=0%). The
fixed-effect model was used for analysis and the results showed
that there was no significant difference between the two groups in
the postoperative cerebrovascular accident (OR=1.57, 95%
CI=0.72-3.39, P=0.25; Fig. 8).
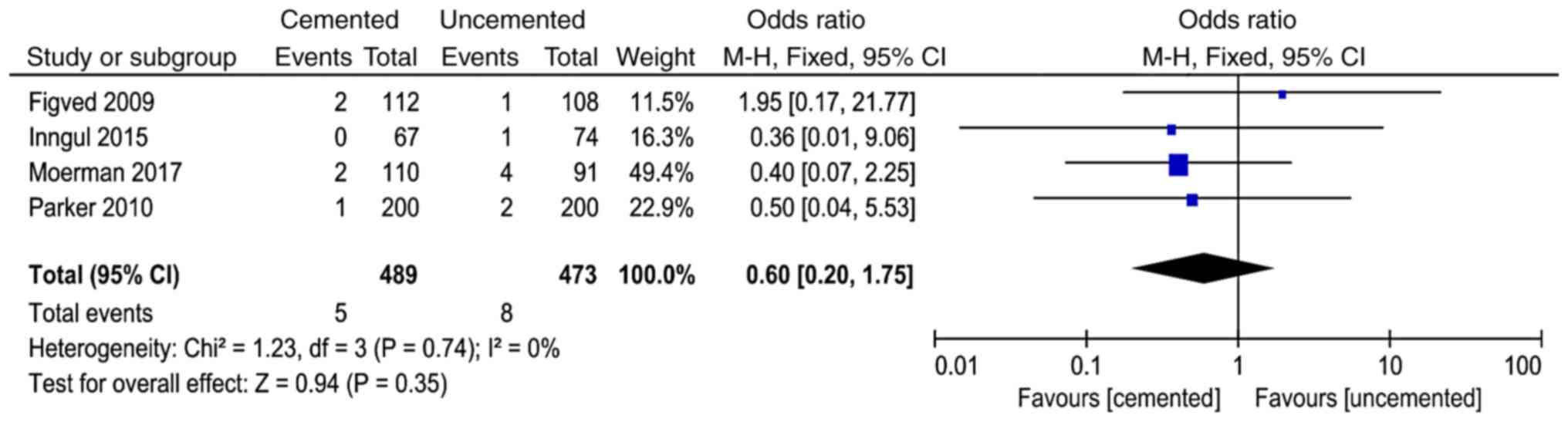
Postoperative myocardial
infarction
A total of 4 studies (11,12,16,17)
reported postoperative myocardial infarction and 962 cases were
included in the analysis. There was no significant heterogeneity in
the results of the studies (P=0.74, I2=0%). The
fixed-effect model was used for analysis and the results showed
that there was no significant difference between the two groups in
the postoperative myocardial infarction (OR=0.60, 95% CI=0.20-1.75,
P=0.35; Fig. 9).
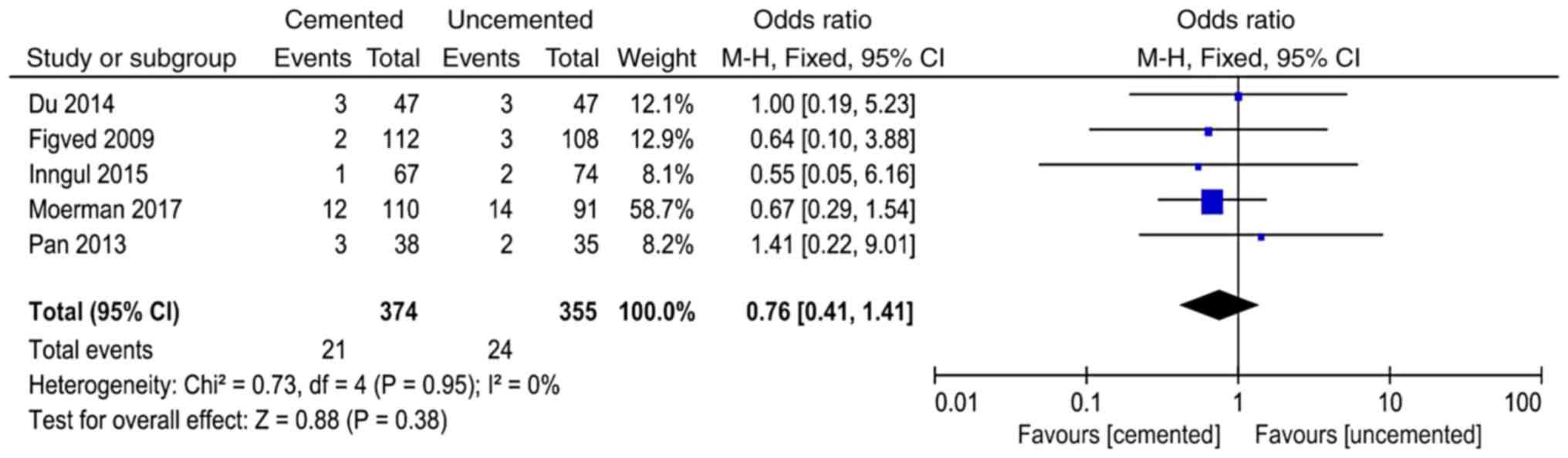
Postoperative pulmonary infection
A total of 5 studies (11,12,16,18,23)
reported postoperative pulmonary infection and 729 cases were
included in the analysis. There was no significant heterogeneity in
the results of the studies (P=0.74, I2=0%). The
fixed-effect model was used for analysis and the results showed
that there was no significant difference between the two groups in
the postoperative pulmonary infection (OR=0.76, 95% CI=0.41-1.41,
P=0.38; Fig. 10).
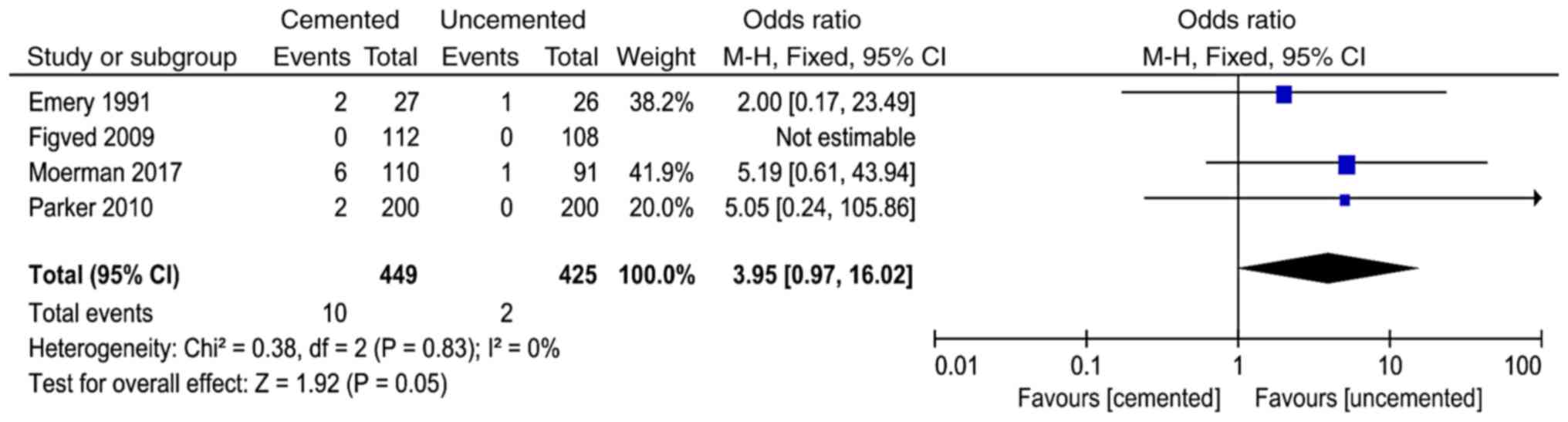
Pulmonary embolism
A total of 4 studies (10,11,16,17)
reported pulmonary embolism and 874 cases were included in the
analysis. There was no significant heterogeneity in the results of
the studies (P=0.83, I2=0%). The fixed-effect model was
used for analysis and the results showed that there was no
significant difference between the two groups in the pulmonary
embolism (OR=3.95, 95% CI=0.97-16.02, P=0.05; Fig. 11).
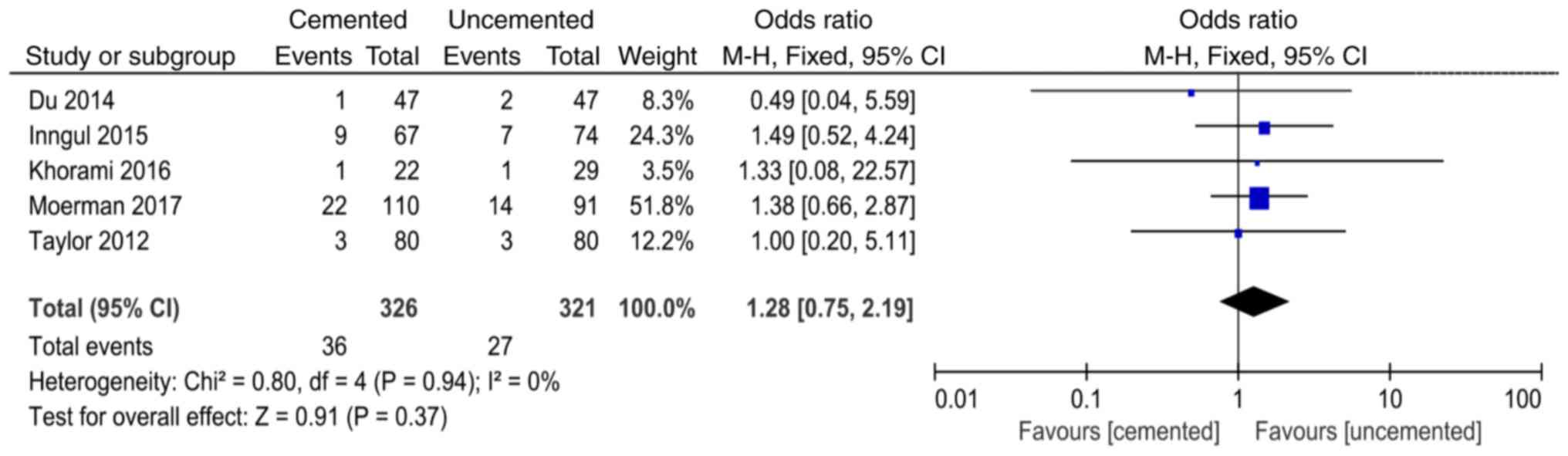
Postoperative urinary tract
infection
A total of 5 studies (12,14,16,21,23)
reported postoperative urinary tract infection and 647 cases were
included in the analysis. There was no significant heterogeneity in
the results of the studies (P=0.94, I2=0%). The
fixed-effect model was used for analysis and the results showed
that there was no significant difference between the two groups in
the postoperative urinary tract infection (OR=1.28, 95%
CI=0.75-2.19, P=0.37; Fig. 12).
Postoperative deep vein
thrombosis
A total of 6 studies (8,10,13,16-18)
reported postoperative deep vein thrombosis and 857 cases were
included in the analysis. There was no significant heterogeneity in
the results of the studies (P=0.96, I2=0%). The
fixed-effect model was used for analysis and the results showed
that there was no significant difference between the two groups in
the postoperative deep vein thrombosis (OR=1.17, 95% CI=0.47-2.89,
P=0.74; Fig. 13).
Mortality within six months after
surgery
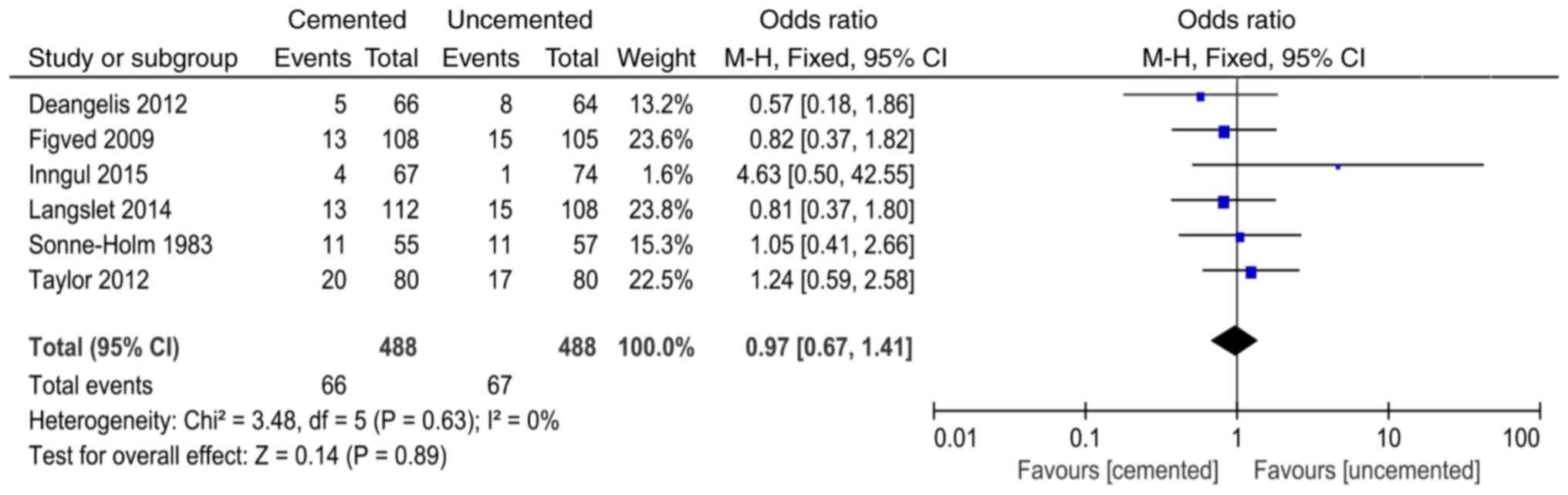
A total of 6 studies (9,11,12,15,19,21)
reported mortality within six months after surgery and 976 cases
were included in the analysis. There was no significant
heterogeneity in the results of the studies (P=0.63,
I2=0%). The fixed-effect model was used for analysis and
the results showed that there was no significant difference between
the two groups in the mortality within six months after surgery
(OR=0.97, 95% CI=0.67-1.41, P=0.89; Fig. 14).
Mortality within one year after
surgery
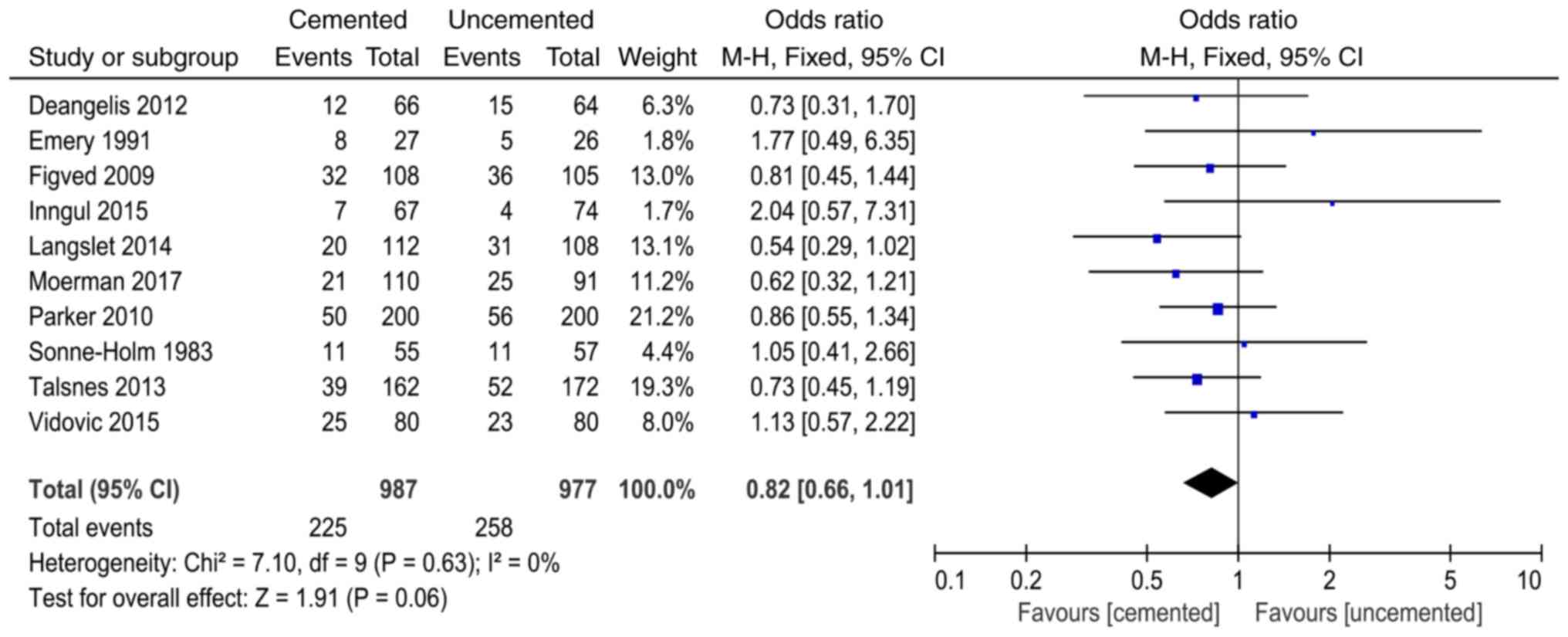
A total of 10 studies (9-12,15-17,19,20,22)
reported mortality within one year after surgery and 1964 cases
were included in the analysis. There was no significant
heterogeneity in the results of the studies (P=0.63,
I2=0%). The fixed-effect model was used for analysis and
the results showed that there was no significant difference between
the two groups in the mortality within one year after surgery
(OR=0.82, 95% CI=0.66-1.01, P=0.06; Fig. 15).
Publication bias and quality
assessment
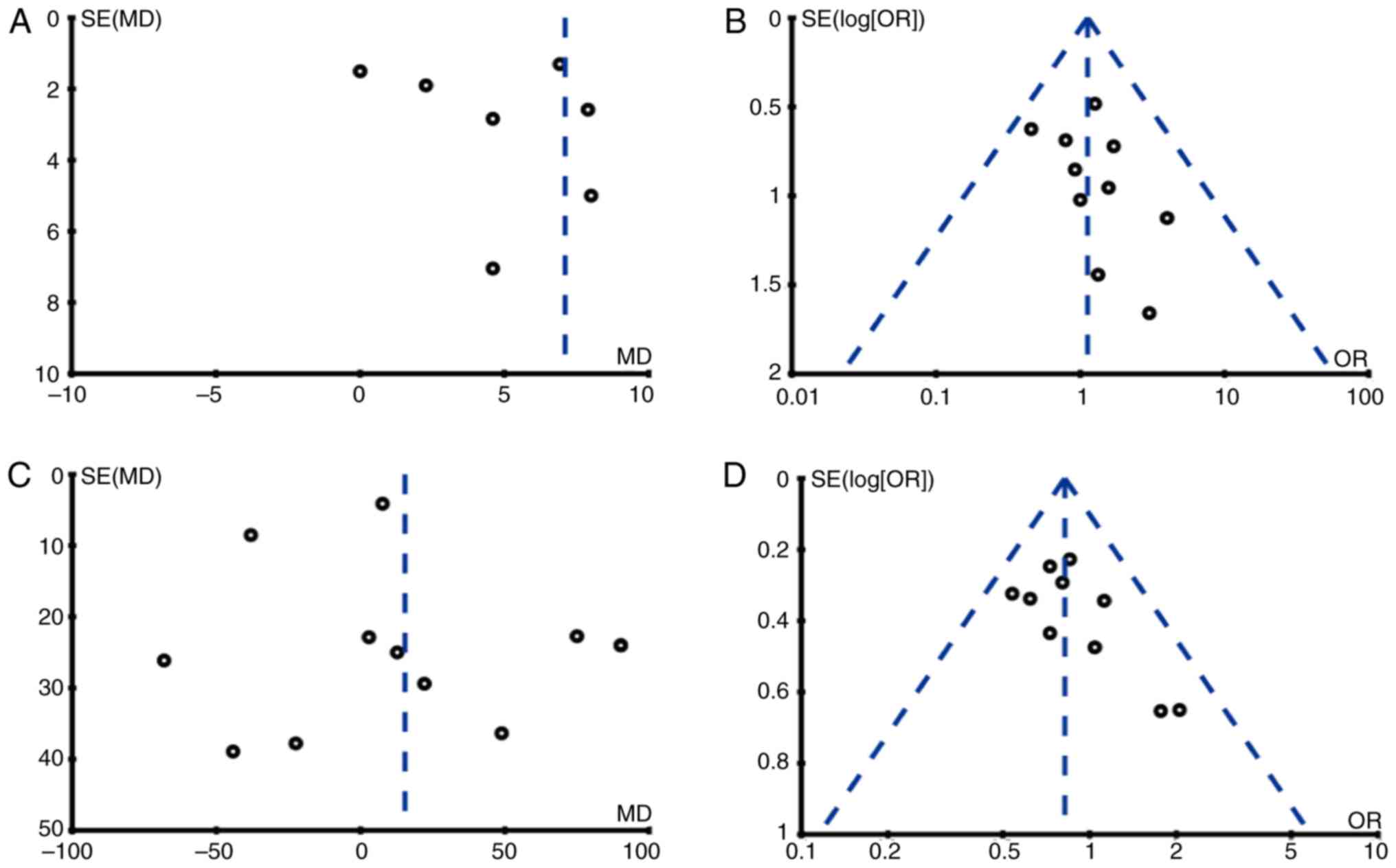
We conducted publication bias analysis on outcome
indicators of 10 studies by funnel plots and the results showed
that there was publication bias in the result of time of operation
and the other 3 funnel plots had good symmetry, indicating no
obvious publication bias (Fig. 16).
The quality assessment of all included studies is shown in Table II. All the results are greater than
4 points, indicating that the quality of the included studies is
good.
 | Table IIModified Jadad scale. |
Table II
Modified Jadad scale.
| Studies First
author, year (Ref.) | Blinding | Randomization | Concealment
allocation | Withdrawal | Total scores |
|---|
| Deangelis,
2012(9) | 2 | 2 | 1 | 1 | 6 |
| Du, 2014(23) | 2 | 2 | 1 | 1 | 6 |
| Emery,
1991(10) | 2 | 2 | 1 | 1 | 6 |
| Figved,
2009(11) | 2 | 2 | 2 | 1 | 7 |
| Inngul,
2015(12) | 2 | 1 | 1 | 1 | 5 |
| Khorami,
2016(14) | 1 | 2 | 1 | 1 | 5 |
| Langslet,
2014(15) | 2 | 2 | 2 | 1 | 7 |
| Li, 2017(13) | 1 | 1 | 1 | 1 | 4 |
| Ma, 2016(8) | 1 | 2 | 2 | 1 | 6 |
| Moerman,
2017(16) | 2 | 1 | 1 | 1 | 5 |
| Pan, 2013(18) | 2 | 2 | 1 | 1 | 6 |
| Parker,
2010(17) | 1 | 1 | 1 | 1 | 4 |
| Sonne-Holm,
1983(19) | 1 | 2 | 2 | 1 | 6 |
| Talsnes,
2013(20) | 1 | 2 | 1 | 1 | 5 |
| Taylor,
2012(21) | 2 | 2 | 1 | 1 | 6 |
| Vidović,
2015(22) | 2 | 1 | 1 | 1 | 5 |
Discussion
Hemiarthroplasty is one of the most important
methods to resolve unstable femoral neck fractures in elderly
patients. Some scholars believe that the incidence of complications
of cemented hemiarthroplasty is low, but it may result in
cardiovascular and cerebrovascular complications (24). Some scholars believe that the
uncemented prosthesis has certain advantages in operation time and
intraoperative blood loss, but the pain appears earlier (25). Due to the differences among
countries, regions, patients and races, as well as the differences
in surgical techniques, there is no unified conclusion on these
issues in clinical practice. At present, there is no unified
consensus and guidelines on how to select prostheses for
hemiarthroplasty. Therefore, the present meta-analysis adopted
currently available data to provide a theoretical basis for the
clinical treatment of femoral neck fractures.
The meta-analysis results showed that the choice of
bone cement as prosthesis could reduce intraoperative and
postoperative fracture around the prosthesis. The main reasons were
that the cemented hemiarthroplasty stability depends on the contact
scope of prosthesis and medullary cavity and close degree. Surgeons
continuously tap cemented hemiarthroplasty in order to maintain the
stability of the prosthesis, which could lead to femur fractures.
If the prosthesis is not stable, the possibility of loosening of
the prosthesis may increase during postoperative functional
exercise and the loose prosthesis is unable to disperse the
surrounding stress well, which may lead to fracture around the
prosthesis in the process of loading on the ground. As cemented
hemiarthroplasty is effectively filled with bone cement, surgeons
can easily ensure the area where the prosthesis fits into the
medullary cavity during the process of striking the prosthesis,
thus reducing the possibility of fracture around the prosthesis. In
addition, the effects of the two surgical methods on periprosthetic
fractures are very different. This may be affected by some
confounding factors, such as the different drugs that patients may
take. Therefore, we need to take this result with caution.
Although there was no obvious difference in the
result of joint dislocation between the cemented and uncemented
groups, surgeons tend to only have one chance to handle cement. If
the prosthesis position is poor, it is difficult to adjust the
position again. However, the uncemented hemiarthroplasty is easy to
pull out, thus surgeons can adjust the anteversion angle and thus
avoid joint dislocation after surgery due to the unsuitable angle.
There are many reasons for dislocation after hip arthroplasty, such
as age, combined limb or mental disease, approach, diameter of the
artificial femoral head, surgical history, placement of prosthesis
and improper handling; all of which are risk factors for
dislocation after hip arthroplasty. However, whether the selection
of prosthesis is a risk factor requires further analysis of large
sample data.
Hemiarthroplasty with bone cement shank as
prosthesis was found to increase the operation time but did not
increase the intraoperative blood loss and infection rate. Azegami
et al (26) point out in
their meta-analysis that the cemented group had more intraoperative
blood loss than the uncemented group, but this study showed no
significant difference between the two groups in intraoperative
blood loss. Studies included in this study were of high quality and
the number of included cases was large, thus it was more
convincing. Although the bone cement groups have an increased
chance of bleeding, bone cement is able to immediately close the
medullary cavity, thus reducing intraoperative blood loss. The
uncemented group avoids the time required to prepare and place the
cement, but the closure of the medullary cavity is not immediate.
The above reasons explain why the two groups have no significant
difference in the intraoperative blood loss. Infection is one of
the most serious complications for surgeons and an increase in
operation time may increase the risk of surgical infection.
However, bone cement contains antibiotics that can be released
slowly, which may play an important role in the prevention of
infection and thus reduce the risk of infection. The operation time
of the uncemented group was short, which was significant in
reducing the risk of infection, but there is no coating on
uncemented hemiarthroplasty to prevent infection, which may be the
reason why there was no significant difference in the postoperative
infection rate between the two groups. The skill level of the
surgeon and the patient's race and disease status may lead to the
heterogeneity of the results. Although this analysis could not
completely eliminate the heterogeneity, it still has clinical
reference value because of the large number of included cases.
Hemiarthroplasty with bone cement shank as
prosthesis could reduce the length of hospital stay, which is of
great significance for patients and their family burden. Previous
meta-analyses did not analyze the length of hospital stay of
patients. In this study, the length of hospital stay was analyzed
and it was found that hemiarthroplasty with bone cement shank as
prosthesis could significantly reduce the length of hospital stay
and thus reduce the burden on the family. Considering the reasons,
cemented hemiarthroplasty could provide patients with good
functional recovery in the short term. Cemented hemiarthroplasty
could fill the gap between the bone marrow cavity and artificial
prosthesis by bone cement. According to proper pressure, bone
cement can be embedded into the gap of bone trabecula so that the
interlacing between bone trabecula and bone cement could be formed,
thus making the fixation of cemented hemiarthroplasty more firm.
Therefore, most patients undergoing cemented hemiarthroplasty have
a short time in bed after surgery and patients can get out of bed
in a short period of time and recover quickly after surgery. The
uncemented hemiarthroplasty has a porous structure on its surface.
After implantation into the human body, it mainly relies on the
growth of bone tissue to form a tight biological fixation between
the bone and the prosthesis surface. The bone growth period of the
biological prosthesis is relatively long and the stability of the
early postoperative period is poor, thus the postoperative time in
bed of the patient is relatively long.
Although the incidence of pulmonary embolism in the
uncemented group was significantly lower than that in the cemented
group, the incidence of postoperative pulmonary infection, urinary
tract infection and lower limb deep vein thrombosis were not
reduced. The incidence of pulmonary embolism is consistent with the
study of Borghi et al (27).
Among the 1,640 patients, the incidence of pulmonary embolism after
total hip replacement with cemented hemiarthroplasty was 2.4%,
while the incidence of pulmonary embolism after total hip
replacement with uncemented prosthesis was 0.34%. In the process of
prosthesis implantation, when bone cement is filled into the
intramedullary cavity, intramedullary pressure increases rapidly,
leading to fat, bone marrow and air entering the circulatory system
and forming an embolism. Bone cement itself also acts on the
calcium channel of vascular smooth muscle and then relaxes blood
vessels, resulting in lower blood pressure. At the same time, the
polymerization of bone cement generates heat and local high
temperature could rapidly damage the vascular endothelium, further
causing thrombosis (14).
There was no significant difference in mortality
between the two groups for 6 months and 1 year after surgery, which
corroborated the results of Azegami et al (26). Due to the general advanced age of the
patients, preoperative basic diseases, such as cardiovascular and
cerebrovascular diseases, hypertension, diabetes, and lung diseases
may result in death. The use of bone cement may be a factor in
mortality, but large sample RCTs are required for analysis.
At present, more and more types of prostheses are
applied in the clinic, including biological prostheses, cemented
hemiarthroplasty and various new materials. 3D printing technology
is also being used in hemiarthroplasty (5,6).
Different prostheses have their own advantages and disadvantages.
Therefore, we need to design appropriate surgical methods for
different patients.
To sum up, in hemiarthroplasty, the cemented group
had a long operation time and high incidence of pulmonary embolism,
but had an obviously reduced incidence of intraoperative and
postoperative fracture around the prosthesis and reduced length of
hospital stay. There was no significant difference in incidence of
death, lower extremity deep vein thrombosis, joint dislocation,
intraoperative blood loss, postoperative lung infection, urinary
tract infection and incision infection between the two groups.
However, the included studies did not analyze the effect of gender.
Given the gender difference in senile osteoporosis, gender may also
be one of the factors affecting the two surgical approaches.
Therefore, gender should be analyzed as an independent factor in
subsequent clinical studies. The studies included in this
meta-analysis had high quality, but due to the limitation of sample
size, a larger sample size and higher quality RCTs should be used
for further demonstration.
In conclusion, compared with the uncemented group,
the cemented group had an extended operation time and a high
incidence of pulmonary embolism, but had an advantage in reducing
the prosthesis fracture around the intraoperative and postoperative
and short length of hospital stay and had no increased rate of
mortality, lower extremity deep vein thrombosis, joint dislocation
rate, intraoperative blood loss and postoperative incidence of
lung, urinary tract and incision.
Acknowledgements
We thank Dr An Yang (The Second People's Hospital of
Hefei) for the assistance in contributing to the literature search
process.
Funding
The present meta-analysis was funded by Beijing
Bethune Medical Scientific Research Fund (N054EN).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
XK designed the study, collected the data and
analyzed the data. XK prepared the manuscript and approved the
final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Collin PG, D'Antoni AV, Loukas M, Oskouian
RJ and Tubbs RS: Hip fractures in the elderly-: A clinical anatomy
review. Clin Anat. 30:89–97. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
2
|
LeBlanc KE, Muncie HL Jr and LeBlanc LL:
Hip fracture: Diagnosis, treatment, and secondary prevention. Am
Fam Physician. 89:945–951. 2014.
|
|
3
|
Leal J, Gray AM, Prieto-Alhambra D, Arden
NK, Cooper C, Javaid MK and Judge A: REFReSH study group: Impact of
hip fracture on hospital care costs: A population-based study.
Osteoporos Int. 27:549–558. 2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Florschutz AV, Langford JR, Haidukewych GJ
and Koval KJ: Femoral neck fractures: Current management. J Orthop
Trauma. 29:121–129. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Caldwell L, Chan CM, Sanders JO and
Gorczyca JT: Detection of femoral neck fractures in pediatric
patients with femoral shaft fractures. J Pediatr Orthop.
37:e164–e167. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Slobogean GP, Stockton DJ, Zeng BF, Wang
D, Ma B and Pollak AN: Femoral neck shortening in adult patients
under the age of 55 years is associated with worse functional
outcomes: Analysis of the prospective multi-center study of hip
fracture outcomes in China (SHOC). Injury. 48:1837–1842.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Jadad AR, Moore RA, Carroll D, Jenkinson
C, Reynolds DJ, Gavaghan DJ and McQuay HJ: Assessing the quality of
reports of randomized clinical trials: Is blinding necessary?
Control Clin Trials. 17:1–12. 1996.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ma C, Jiang F, Huang C and Liu Z: Contrast
of effect and prognosis of artificial hip joint maken by
biomaterials and bone-cement for femoral neck fracture. Jianyan
Yixue Yu Linchuang. 13:1826–1828. 2016.
|
|
9
|
Deangelis JP, Ademi A, Staff I and Lewis
CG: Cemented versus uncemented hemiarthroplasty for displaced
femoral neck fractures: A prospective randomized trial with early
follow-up. J Orthop Trauma. 26:135–140. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Emery RJ, Broughton NS, Desai K, Bulstrode
CJ and Thomas TL: Bipolar hemiarthroplasty for subcapital fracture
of the femoral neck. A prospective randomised trial of cemented
Thompson and uncemented Moore stems. J Bone Joint Surg Br.
73:322–324. 1991.PubMed/NCBI
|
|
11
|
Figved W, Opland V, Frihagen F, Jervidalo
T, Madsen JE and Nordsletten L: Cemented versus uncemented
hemiarthroplasty for displaced femoral neck fractures. Clin Orthop
Relat Res. 467:2426–2435. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Inngul C, Blomfeldt R, Ponzer S and
Enocson A: Cemented versus uncemented arthroplasty in patients with
a displaced fracture of the femoral neck: A randomised controlled
trial. Bone Joint J. 97-B:1475–1480. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Li J: Comparison of the effects and
complications of biotype and cement-based artificial hip prosthesis
in the treatment of femoral neck fracture in the elderly. Clin Med
Chin. 33:1127–1130. 2017.(In Chinese).
|
|
14
|
Khorami M, Arti H and Aghdam AA: Cemented
versus uncemented hemiarthroplasty in patients with displaced
femoral neck fractures. Pak J Med Sci. 32:44–48. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Langslet E, Frihagen F, Opland V, Madsen
JE, Nordsletten L and Figved W: Cemented versus uncemented
hemiarthroplasty for displaced femoral neck fractures: 5-year
followup of a randomized trial. Clin Orthop Relat Res.
472:1291–1299. 2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Moerman S, Mathijssen NMC, Niesten DD,
Riedijk R, Rijnberg WJ, Koëter S, Kremers van de Hei K,
Tuinebreijer WE, Molenaar TL, Nelissen RGHH and Vochteloo AJH: More
complications in uncemented compared to cemented hemiarthroplasty
for displaced femoral neck fractures: A randomized controlled trial
of 201 patients, with one year follow-up. BMC Musculoskelet Disord.
18(169)2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Parker MI, Pryor G and Gurusamy K:
Cemented versus uncemented hemiarthroplasty for intracapsular hip
fractures: A randomised controlled trial in 400 patients. J Bone
Joint Surg Br. 92:116–122. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pan S: Comparison of the effects of
cemented and uncemented hemiarthroplasty in the treatment of
displaced femoral neck fractures. Chin J Postgrad Med. 36:41–43.
2013.
|
|
19
|
Sonne-Holm S, Dyrbye M, Walter S and
Jensen JS: Bone scintigraphy in Moore hemiarthroplasty with and
without cement following femoral neck fractures. A controlled
study. Acta Orthop Scand. 54:194–197. 1983.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Talsnes O, Hjelmstedt F, Pripp AH,
Reikerås O and Dahl OE: No difference in mortality between cemented
and uncemented hemiprosthesis for elderly patients with cervical
hip fracture. A prospective randomized study on 334 patients over
75 years. Arch Orthop Trauma Surg. 133:805–809. 2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Taylor F, Wright M and Zhu M:
Hemiarthroplasty of the hip with and without cement: A randomized
clinical trial. J Bone Joint Surg Am. 94:577–583. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Vidović D, Punda M, Daraboš N,
Bekavac-Bešlin M, Bakota B and Matejčić A: Regional bone loss
following femoral neck fracture: A comparison between cemented and
cementless hemiarthroplasty. Injury. 46 (Suppl 6):S52–S56.
2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Du Z: Analysis of the effect of cemented
and uncemented artificial double femoral head replacement. Chin Med
Eng. 29–30. 2014.
|
|
24
|
Sprague S, Slobogean GP, Scott T, Chahal M
and Bhandari M: Young femoral neck fractures: Are we measuring
outcomes that matter? Injury. 46:507–514. 2015.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Grosso MG, Danoff JR, Padgett DE, Iorio R
and Macaulay WB: The cemented unipolar prosthesis for the
management of displaced femoral neck fractures in the dependent
osteopenic elderly. J Arthroplasty. 31:1040–1046. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Azegami S, Gurusamy KS and Parker MJ:
Cemented versus uncemented hemiarthroplasty for hip fractures: A
systematic review of randomised controlled trials. Hip Int.
21:509–517. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Borghi B and Casati A: Rizzoli Study Group
on Orthopaedic Ananesthesia: Thromboembolic complications after
total hip replacement. Int Orthop. 26:44–47. 2002.PubMed/NCBI View Article : Google Scholar
|