Introduction
An estimated 15-20% of patients with acute
pancreatitis (AP) develop necrosis of pancreatic parenchyma and/or
peripancreatic necrosis (1,2). Pancreatic necrosis is associated with
a mortality rate ranging from 8 to 30% (3). Infected pancreatitis necrosis (IPN) is
typically treated by minimally invasive drainage (MID) or open
necrosectomy (ON) (2,3). Most studies have demonstrated that ON
is associated with high morbidity and mortality (4-11).
MID was indicated to decrease mortality without increasing the
complications of the infection of infection-associated mortality
(12-14).
However, to the best of our knowledge, the long-term follow-up of
pancreatic endocrine and exocrine function and quality of life
(QoL) of patients with IPN has not previously been performed and
the difference of pancreatic function and QoL between patients
undergoing ON and MID is unknown.
Damaged pancreatic acinar cells may recover after
interstitial edematous pancreatitis, improving pancreatic function
(15), and complete recovery of
pancreatic acinar cells has been documented (16). However, a considerable proportion of
patients who recovered from IPN have an impaired endocrine and
exocrine pancreatic function (17).
Thus, the objective of the present study was to determine the
long-term outcomes of patients with IPN treated with ON or MID in
terms of pancreatic function and QoL.
Patients and methods
General information
Patients with IPN who received MID or ON between
January 2000 and February 2015 at Jinling Hospital, Medical School
of Nanjing University (Nanjing, China), were included in the
present study. The patients were divided into the MID and ON groups
based on the interventional approach they received. Demographic
data, time spent in the intensive care unit (ICU), the CT severity
index (CTSI), Acute Physiology and Chronic Health Evaluation
(APACHE) II score and body mass index (BMI) were retrieved from
medical records. For all patients, the evaluation of pancreatic
endocrine and exocrine function and QoL was performed in May 2016.
Written informed consent was obtained from each patient. The
protocol of the present study was approved by the ethics committee
of Jinling Hospital, Medical School of Nanjing University (Nanjing,
China).
The area of pancreatic necrosis was assessed by
experienced radiologists based on the necrotic features in the
contrast-enhanced CT (CECT) images. IPN was diagnosed on the basis
of a positive culture of pancreatic or peripancreatic necrotic
tissue obtained from the first drainage procedure or operation or
the presence of gas in the fluid collected during CECT.
MID consisted of a sequence of three procedures
(18): Percutaneous catheter
drainage (PCD), negative pressure irrigation (NPI) and endoscopic
necrosectomy (ED) via an artificial sinus tract. Image-guided PCD
was considered the first choice for intervention. For this
procedure, pigtail tubes were placed using a CT- or
ultrasound-guided Seldinger puncture technique in the area of
pancreatic necrosis via the retroperitoneum or peritoneum,
depending on the location of IPN and adjacent organs (10). NPI was performed using a ‘double
catheterization cannula’ to ensure continuous irrigation of the
cavity. ED was performed using a 30F electronic gastroscope
inserted through the sinus tract created by double catheterization
cannulas and a snare was used to extract out a large volume of
necrotic tissue that was difficult to be removed by NPI and
PCD.
ON consisted of two steps: First, a laparotomy was
performed through bilateral subcostal incisions for blunt removal
of the necrotic tissue, and double catheterization cannulas or
drainage tubes were then placed for post-operative lavage. The
decision to perform ON or MID was made by multidisciplinary
discussion between surgeons, internist physician and radiologists,
taking into account the area and location of necrosis, abdominal
pressure, vital signs and the patient's preference.
Exclusion criteria
The exclusion criteria were as follows: i) Chronic
pancreatitis; ii) diagnosis of diabetes mellitus (DM) prior to the
IPN episode; iii) chronic diarrhea prior to IPN; iv) intestinal
tuberculosis or Crohn's disease; v) family history of DM; vi)
incomplete medical records; vii) death during hospitalization or
after discharge from hospital; viii) conditions influencing QoL
after discharge, including mental diseases, immune system diseases
and malignant tumors.
Assessment methods and data
collection
Simplified oral glucose tolerance test (19) and fecal elastase-1 (FE-1) test
(BIOSERV Diagnostics GmbH) were used to evaluate the pancreatic
endocrine and exocrine function, respectively. The data on fasting
blood glucose (FBG), free insulin (FINS), fasting
C-reactive-peptide, glycated hemoglobin (HbA1c), 2-h plasma glucose
(PG), 2-h C-reactive peptide and 2-h insulin, were also
collected.
Stool samples were collected for the FE-1 test and
stored at -20˚C. Concentrations of FE-1 in the stool were
interpreted as follows: >200 µg/g stool, normal exocrine
pancreatic function; 100-200 µg/g stool, mild to moderate exocrine
pancreatic function; <100 µg/g stool, severe exocrine pancreatic
dysfunction (20,21).
CT images were used to determine the loss of
pancreas of the patients discharged from hospital. The incidence of
100% loss of the pancreas was compared between the MID and ON
groups.
The standard short form (SF)-36 questionnaire
(22) was used to assess the QoL of
patients. SF-36 consists of 8 sections designed to evaluate 8
domains of health, including physical functioning, physical role
functioning, bodily pain, general health perceptions, vitality,
social role functioning, emotional role functioning and mental
health. Patients completed the questionnaire by themselves or with
help from their families.
The conversion score of each part of the SF-36 was
calculated from the actual score using the following formula
(23): Conversion score=(Actual
score-Probable lowest score)/Probable highest score-Probable lowest
score) x100%.
A higher conversion score indicated a better QoL.
The total QoL score was the sum of the scores for each section of
the questionnaire.
Statistical analysis
Statistical analysis was performed using SPSS 22.0
for Windows (IBM Corp.). Continuous variables were expressed as the
mean ± standard deviation and comparison between groups was
performed using Student's t-test. Categorical variables were
expressed as absolute numbers and comparison between groups was
performed using Fisher's exact test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Baseline characteristics
During the enrollment period, 109 patients with IPN
were admitted to Jinling Hospital. Of these, 101 patients were
included in the present study and 8 were excluded. Among the 8
excluded cases, 6 patients (5.9% of all patients) died during
hospitalization or after being discharged from hospital, including
3 who succumbed to septic shock, 2 who died from major bleeding and
1 from unknown causes. Among the patients included, 40 (39.6%) were
treated with ON and 61 (60.4%) with MID. There were 66 males and 35
females with a median age of 46 years (interquartile range,
41.5-56.0).
There was no difference between the two groups in
terms of age, gender, drinking history, pancreatic necrosis area,
positive blood culture, recurrent pancreatitis and the time from
discharge to follow-up (Table I).
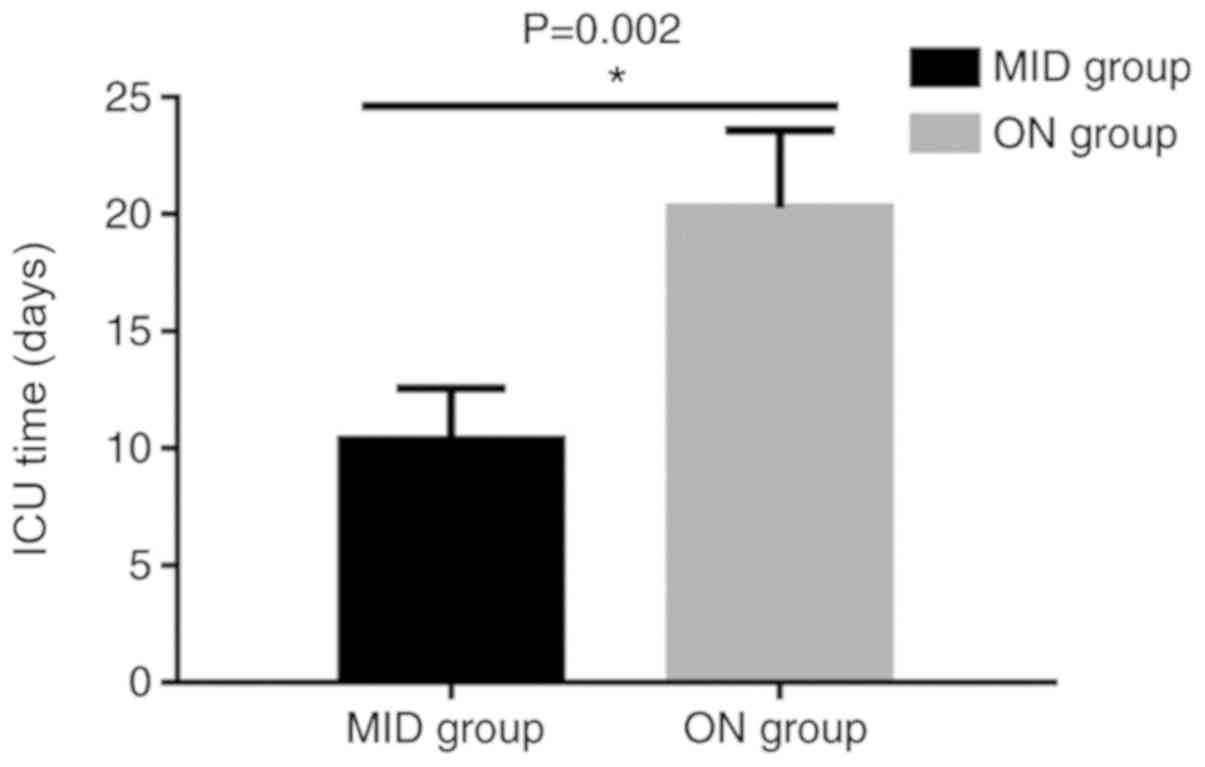
The duration of stay at the ICU in the ON group was longer than
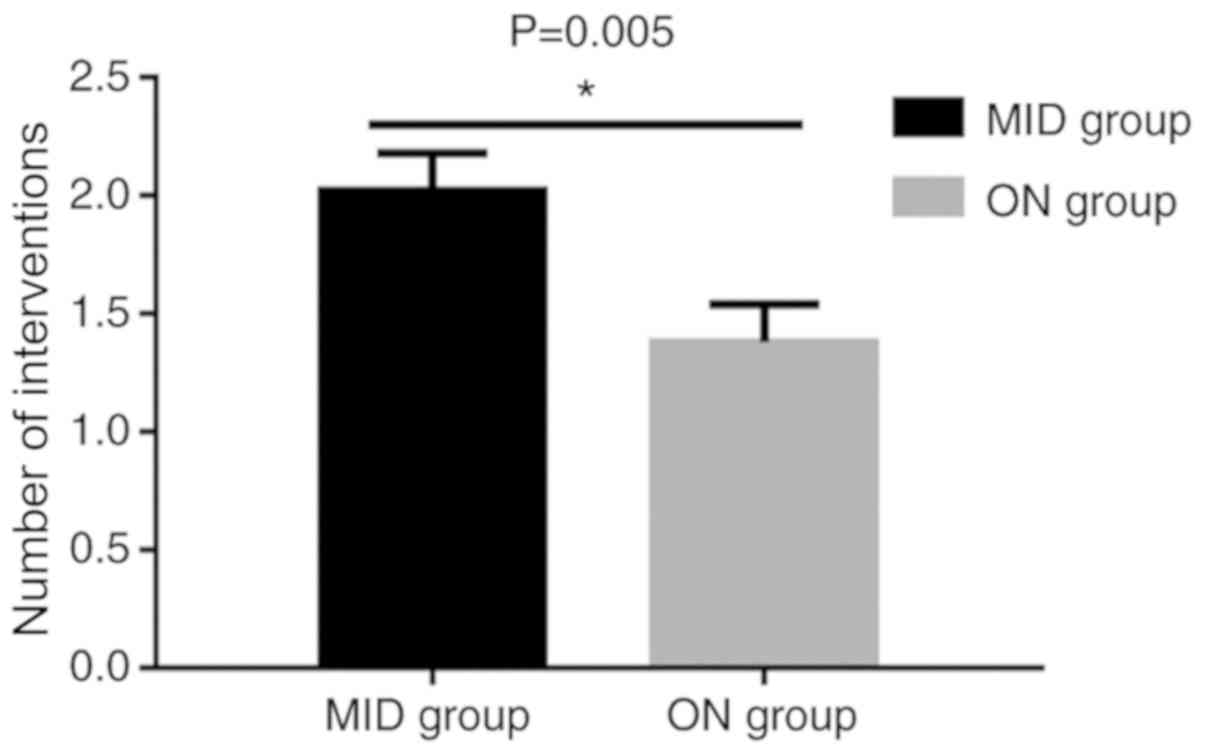
that in the MID group (20.28±3.32 vs. 10.36±2.21, P=0.002; Fig. 1). Patients in the MID group required
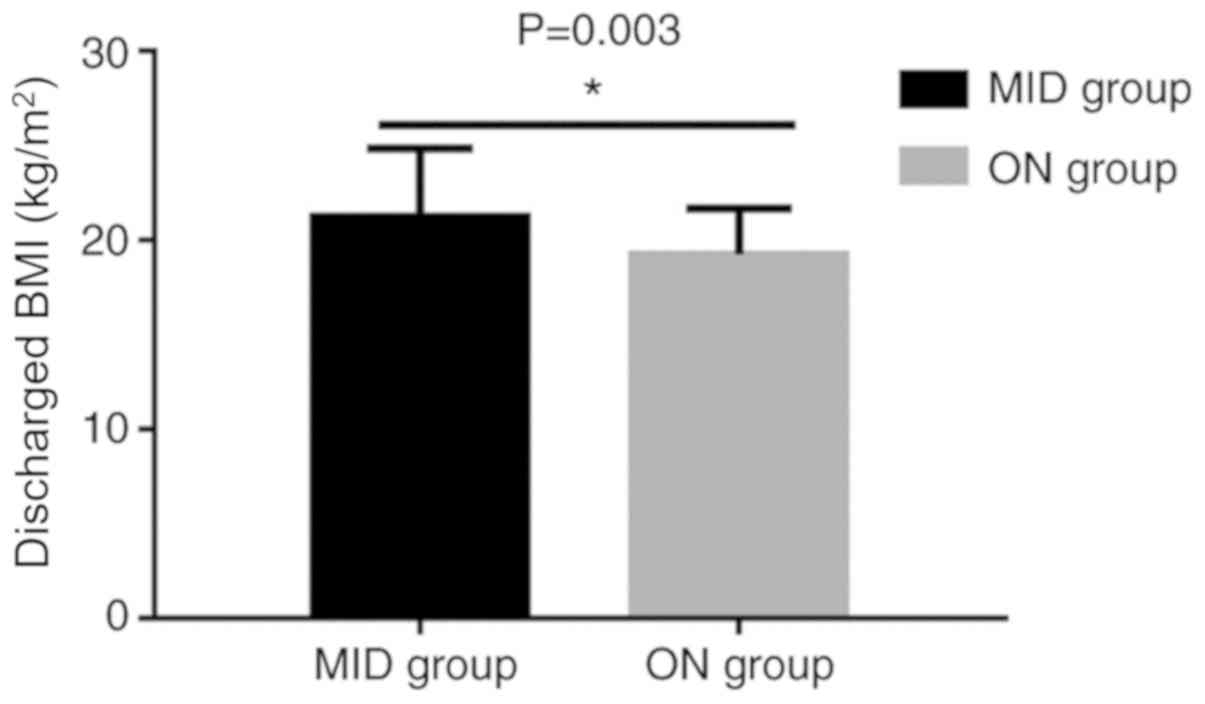
more MID procedures than those in the ON group (P=0.005; Fig. 2). The BMI after discharge was
significantly higher in the MID than in the ON group (21.25±3.60
vs. 19.26±2.42, P=0.003; Fig. 3).
The incidence of whole pancreatic loss was significantly higher in
the ON group (28 vs. 17, P<0.001). The diet, symptoms of
diabetes and the prevalence of pseudocyst and intestinal fistula at
the follow-up were similar between the two groups (Table II).
 | Table IClinical characteristics of the
patients in the MID group and ON group during their hospital
stay. |
Table I
Clinical characteristics of the
patients in the MID group and ON group during their hospital
stay.
| Variables | MID (n=61) | ON (n=40) | P-value |
|---|
| Age (years) | 49.16±1.74 | 48.65±1.87 | 0.845 |
| Sex | | | 0.953 |
|
Male | 40 | 26 | |
|
Female | 21 | 14 | |
| History of
drinking | | | 0.485 |
|
Present | 24 | 13 | |
|
Absent | 37 | 27 | |
| Time interval
(months) | 35±4.74 | 37±3.96 | 0.756 |
| Gallstones | | | 0.244 |
|
Present | 45 | 24 | |
|
Absent | 16 | 16 | |
|
Hypertriglyceridemia | | | 0.161 |
|
Present | 11 | 12 | |
|
Absent | 50 | 28 | |
| Severity | | | 0.768 |
|
Severe | 20 | 12 | |
|
Critical | 41 | 28 | |
| APACHE II
score | 9.89±0.80 | 12.18±1.06 | 0.082 |
| Balthazar
score | 7.37±0.26 | 7.83±0.28 | 0.264 |
| Pre-operative
infection | | | 0.957 |
|
Present | 61 | 40 | |
|
Absent | 0 | 0 | |
| BMI
(kg/m2) prior to IPN | 27.55±4.32 | 27.65±3.33 | 0.905 |
| Duration of ICU
stay (days) | 10.36±2.21 | 20.28±3.32 | 0.002 |
| Organ
dysfunction | | | 1.000 |
|
Present | 40 | 27 | |
|
Absent | 21 | 13 | |
| ARDS | | | 0.404 |
|
Present | 35 | 27 | |
|
Absent | 26 | 13 | |
| AKI | | | 0.839 |
|
Present | 28 | 20 | |
|
Absent | 33 | 20 | |
| ACS | | | 0.259 |
|
Present | 3 | 5 | |
|
Absent | 58 | 38 | |
| Necrotic
areaa | | | |
|
<1/3 | 14 | 12 | 0.489 |
|
1/3-1/2 | 18 | 7 | 0.239 |
|
>1/2 | 29 | 21 | 0.686 |
 | Table IIClinical characteristics of the
patients in the MID group and ON group during the follow-up
time. |
Table II
Clinical characteristics of the
patients in the MID group and ON group during the follow-up
time.
| Variable | MID (n=61) | ON (n=40) | P-value |
|---|
| Physical activity
level based on walking distance (km/day) | | | |
|
<3 | 25 | 14 | 0.546 |
|
3-5 | 10 | 11 | 0.179 |
|
5-10 | 10 | 5 | 0.590 |
|
>10 | 3 | 4 | 0.430 |
|
None | 13 | 6 | 0.604 |
| BMI
(kg/m2) | 21.25±3.60 | 19.26±2.42 | 0.003 |
| Reduced oil
diet | | | 0.801 |
|
Present | 50 | 32 | |
|
Absent | 11 | 8 | |
| Diabetes
symptoms | | | 1.000 |
|
Present | 10 | 7 | |
|
Absent | 51 | 33 | |
| Insulin use | | | 0.709 |
|
Present | 4 | 4 | |
|
Absent | 57 | 36 | |
| Loss of
pancreasa | | | <0.001 |
|
Present | 17 | 28 | |
|
Absent | 44 | 12 | |
| Pseudocyst | | | 0.673 |
|
Present | 3 | 3 | |
|
Absent | 58 | 37 | |
| Intestinal
fistula | | | 0.430 |
|
Present | 3 | 4 | |
|
Absent | 58 | 36 | |
Exocrine and endocrine pancreatic
function and QoL
The parameters reflecting the exocrine pancreatic
function did not differ significantly between the MID and ON
groups. Specifically, the incidence of diarrhea (12/61 vs. 4/40),
abdominal pain (6/61 vs. 3/40), abdominal distention (6/61 vs.
5/40), exogenous trypsin intake (19/61 vs. 10/40) and FE-1
concentration (264.03±22.88 vs. 245.74±30.68 µg/g) in the two
groups was comparable (Table
III). In addition, no statistically significant difference in
endocrine pancreatic function (FBG, FINS, fasting C-peptide, HbA1c,
2-h PG, 2-h insulin and 2-h C-peptide) was observed between the two
groups (Table IV).
 | Table IIIComparison of pancreatic exocrine
function between patients in MID group and ON group. |
Table III
Comparison of pancreatic exocrine
function between patients in MID group and ON group.
| Variable | MID (n=61) | ON (n=40) | P-value |
|---|
| Diarrhea | | | 0.268 |
|
Present | 12 | 4 | |
|
Absent | 49 | 36 | |
| Abodominal
pain | | | 1.000 |
|
Present | 6 | 3 | |
|
Absent | 55 | 37 | |
| Abdominal
distention | | | 0.749 |
|
Present | 6 | 5 | |
|
Absent | 55 | 35 | |
| FE-1 (µg/g) | | | 0.968 |
|
<200 | 12 | 8 | |
|
≥200 | 49 | 32 | |
|
Mean | 264.03±22.88 | 245.74±30.68 | 0.656 |
| Exogenous trypsin
intake | | | 0.653 |
|
Present | 19 | 10 | |
|
Absent | 42 | 30 | |
 | Table IVComparison of pancreatic endocrine
function between patients in MID group and ON group. |
Table IV
Comparison of pancreatic endocrine
function between patients in MID group and ON group.
| Variable | MID (n=61) | ON (n=40) | P-value |
|---|
| FBG | 5.95±1.44 | 6.91±2.85 | 0.055 |
| HBA1c (%) | 5.96±1.04 | 6.49±1.88 | 0.073 |
| FINS | 7.24±0.81 | 9.98±1.83 | 0.130 |
| Fasting
C-peptide | 1.41±0.70 | 2.07±0.55 | 0.160 |
| 2-h insulin | 34.03±3.32 | 43.40±7.25 | 0.194 |
| 2-h C-reactive
peptide | 5.21±0.38 | 5.33±0.53 | 0.859 |
| 2-h PG | 11.54±8.09 | 11.98±6.61 | 0.777 |
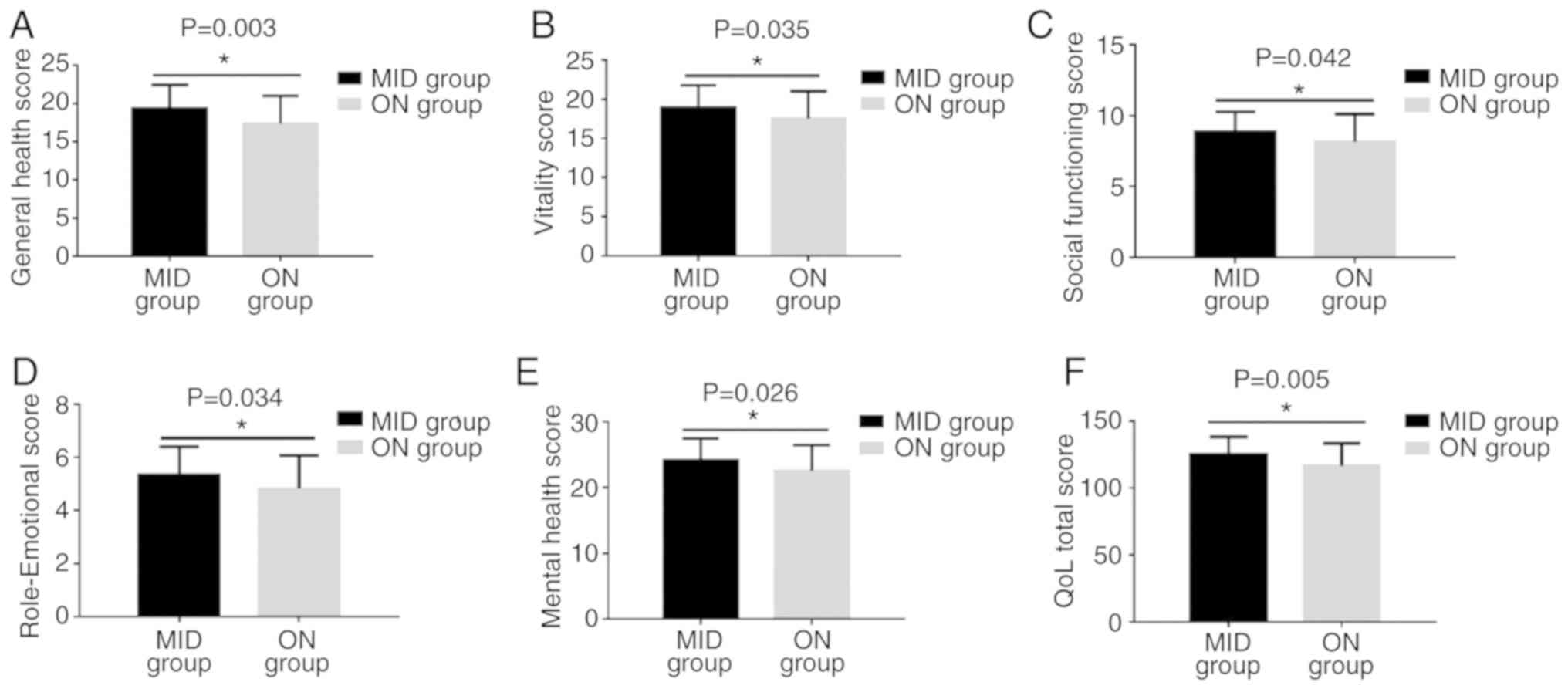
As outlined in Table
V and Fig. 4, the results of
the assessment with the QoL questionnaire indicated significant
differences between the two groups in terms of general health
perception (19.39±3.07 vs. 17.37±3.63, P=0.003; Fig. 4A), vitality (18.93±2.88 vs.
17.57±3.47, P=0.035; Fig. 4B),
social role functioning (8.85±1.43 vs. 8.15±1.98, P=0.042; Fig. 4C), emotional role functioning
(5.33±1.07 vs. 4.82±1.25, P=0.034; Fig.
4D), mental health (24.21±3.31 vs. 22.57±3.91, P=0.026;
Fig. 4E) and total QoL score
(125.12±13.16 vs. 116.50±16.94, P=0.005; Fig. 4F). However, physical functioning
(26.77±3.29 vs. 25.75±4.04, P=0.168), physical role functioning
(6.77±1.67 vs. 6.20±1.69, P=0.099) and bodily pain (10.78±1.46 vs.
10.60±1.52, P=0.556) did not differ significantly between the MID
and ON groups.
 | Table VComparison of QoL between patients in
the MID group and ON group. |
Table V
Comparison of QoL between patients in
the MID group and ON group.
| Item | MID (n=61) | ON (n=40) | P-value |
|---|
| Physical
functioning | 26.77±3.29 | 25.75±4.04 | 0.168 |
| Physical role
functioning | 6.77±1.67 | 6.20±1.69 | 0.099 |
| Bodily pain | 10.78±1.46 | 10.60±1.52 | 0.556 |
| General health
perception | 19.39±3.07 | 17.37±3.63 | 0.003 |
| Vitality | 18.93±2.88 | 17.57±3.47 | 0.035 |
| Social role
functioning | 8.85±1.43 | 8.15±1.98 | 0.042 |
| Emotional role
functioning | 5.33±1.07 | 4.82±1.25 | 0.034 |
| Mental health | 24.21±3.31 | 22.57±3.91 | 0.026 |
| Total QoL
score | 125.12±13.16 | 116.50±16.94 | 0.005 |
Discussion
Several studies indicated that MID is the preferred
method for the treatment of IPN. The present study demonstrated
that the patients in the MID group had a higher BMI at the
follow-up than those in the ON group, while no significant
difference was present prior to the intervention. This result
indicates that MID is able to affect metabolism and nutrition. ON
thoroughly removes necrotic tissue but may lead to loss of
pancreatic tissue. The time spent at the ICU by patients subjected
to ON was longer than that of patients who received MID
(P<0.05). However, it cannot be determined whether MID is
directly able to reduce the time at the ICU, since the patients
treated with ON had typically more severe IPN or organ failure,
requiring treatment for a longer duration. Furthermore, patients
subjected to MID required an increased frequency of MID procedures
than the patients in the ON group. Patients with AP may develop
prediabetes and/or DM after being discharged from hospital
(24). Impairment of the endocrine
function of the pancreas after AP is associated with a decreased
level of plasma insulin after fasting glucose stimulus and it
occurs more frequently in patients recovering from severe AP (SAP)
(25). The pancreas is a key organ
in glucose homeostasis and the development of DM as a result of
pancreatic necrosis after AP has been reported (26). Although numerous studies
demonstrated that AP, and SAP in particular, may impair pancreatic
endocrine function (12), there was
no significant difference in this function between the MID and ON
groups of the present study. As documented in a previous study by
our group, the extent of pancreatic necrosis, wall of necrosis and
insulin resistance are independent risk factors for new-onset DM
after AP (27), and this risk is
increased in patients with simultaneous pancreatic necrosis and
persistent organ failure (28).
Thus, pancreatic necrosis may have a critical role in the
impairment of pancreatic endocrine function. The interventional
methods to remove the necrotic tissue have a limited effect on
diabetes after AP. There was also no significant difference in the
exocrine function of the pancreas between the MID and ON groups of
patients.
Several studies verified the validity and
reliability of the SF-36 questionnaire for the evaluation of QoL
(29-35).
The physical functioning aspect of the QoL questionnaire was
improved during the first year of recovery from the acute
necrotizing pancreatitis (36). The
total QoL score among patients with SAP after five years was
comparable to that of the normal population (37). Numerous complications after IPN,
including incisional hernia, gastrointestinal fistulas,
intra-abdominal bleeding and diabetes, affected the QoL. Certain
patients in the MID group required repeated acupuncture and
placement of multiple drainage tubes, which may make them feel less
comfortable than patients undergoing ON. The present study did not
identify any significant differences in physical functioning,
physical role functioning and bodily pain between the two groups.
However, MID provided a significant benefit over ON in terms of
general health, vitality, social functioning, emotional role
functioning and mental health. It is worth mentioning that it is
not possible to exclude the possibility that these differences are
derived from a difference in initial disease severity between
groups. These results indicate that although MID and ON have a
similar impact on physical indices, they have a different impact on
mental and social indices. This is probably due to the fact that
patients that underwent MID had a better QoL post-surgery. MID
resulted in better general health, vitality and mental health as
compared with ON. The reason for this difference may be the fact
that patients treated with ON suffered from the abdominal incision,
reduced BMI and severe pancreatic complications. These
complications obviously affected their mental and social
functioning. Accordingly, patients in the MID group had higher
total QoL scores than patients undergoing ON.
The major limitation of the present study is its
retrospective design. A prospective randomized controlled study
will be necessary to determine the advantages and disadvantages of
ON and MID for patients with IPN. Another limitation is that the
sample size of the present study is relatively small. Future
studies including a larger number of patients are required.
Furthermore, the present study was a single-center study. A
multi-center study or a meta-analysis including data from more
centers will provide more convincing conclusions in the future.
In conclusion, the present study demonstrated that
patients with IPN who received MID achieved a better QoL than those
treated with ON. However, the endocrine and exocrine functions of
the pancreas were similar in the two groups.
Acknowledgements
Not applicable.
Funding
The present study was supported by grants from the
Natural Science Foundation of Zhejiang Province, China (grant no.
LY18H150005), The Science and Technology Foundation of Zhejiang
Province, China (grant no. 2013C37022), The Key Research and
Development Program Foundation of Jiangsu Province of China (grant
no. BE2016749) and The National Natural Science Foundation of China
(grant nos. 81670588 and 81570584).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JT, JL, QX, and JZ designed the study. YY, QX, LK,
ZT and WL collected the data and performed statistical analysis.
QX, WL and JT wrote the manuscript. All authors read and reviewed
the final version of the manuscript.
Ethics approval and consent to
participate
The experimental protocol was approved by the Ethics
Committee of the Jinling Hospital (Nanjing, China). Written
informed consent was obtained from all patients.
Patient consent for publication
Written informed consent regarding the publication
of clinical data was obtained from every patient enrolled in this
study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Banks PA, Bollen TL, Dervenis C, Gooszen
HG, Johnson CD, Sarr MG, Tsiotos GG and Vege SS: Acute Pancreatitis
Classification Working Group. Classification of acute
pancreatitis-2012: Revision of the Atlanta classification and
definitions by international consensus. Gut. 62:102–111.
2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Besselink MG, van Santvoort HC,
Boermeester MA, Nieuwenhuijs VB, van Goor H, Dejong CH,
Schaapherder AF and Gooszen HG: Dutch Acute Pancreatitis Study
Group. Timing and impact of infections in acute pancreatitis. Br J
Surg. 96:267–273. 2009.PubMed/NCBI View
Article : Google Scholar
|
|
3
|
Banks PA and Freeman ML: Practice
Parameters Committee of the American College of Gastroenterology.
Practice guidelines in acute pancreatitis. Am J Gastroenterol.
101:2379–2400. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Working Group IAP/APA Acute Pancreatitis
Guidelines. IAP/APA evidence-based guidelines for the management of
acute pancreatitis. Pancreatology. 13 (Suppl 2):e1–e15.
2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Working Party of the British Society of
Gastroenterology; Association of Surgeons of Great Britain and
Ireland; Pancreatic Society of Great Britain and Ireland;
Association of Upper GI Surgeons of Great Britain and Ireland. UK
guidelines for the management of acute pancreatitis. Gut. 54 (Suppl
3):iii1–iii9. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Traverso LW and Kozarek RA: Pancreatic
necrosectomy: Definitions and technique. J Gastrointest Surg.
9:436–439. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Werner J, Feuerbach S, Uhl W and Büchler
MW: Management of acute pancreatitis: From surgery to
interventional intensive care. Gut. 54:426–436. 2005.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Babu RY, Gupta R, Kang M, Bhasin DK, Rana
SS and Singh R: Predictors of surgery in patients with severe acute
pancreatitis managed by the step-up approach. Ann Surg.
257:737–750. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Carter CR, McKay CJ and Imrie CW:
Percutaneous necrosectomy and sinus tract endoscopy in the
management of infected pancreatic necrosis: An initial experience.
Ann Surg. 232:175–180. 2000.PubMed/NCBI View Article : Google Scholar
|
|
10
|
van Santvoort HC, Besselink MG, Bakker OJ,
Hofker HS, Boermeester MA, Dejong CH, van Goor H, Schaapherder AF,
van Eijck CH, Bollen TL, et al: A step-up approach or open
necrosectomy for necrotizing pancreatitis. N Engl J Med.
362:1491–1502. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Parikh PY, Pitt HA, Kilbane M, Howard TJ,
Nakeeb A, Schmidt CM, Lillemoe KD and Zyromski NJ: Pancreatic
necrosectomy: North American mortality is much lower than expected.
J Am Coll Surg. 209:712–719. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liu L, Yan H, Liu W, Cui J, Wang T, Dai R,
Liang H, Luo H and Tang L: Abdominal paracentesis drainage does not
increase infection in severe acute pancreatitis: A prospective
study. J Clin Gastroenterol. 49:757–763. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Ai X, Qian X, Pan W, Xu J, Hu W, Terai T,
Sato N and Watanabe S: Ultrasound-guided percutaneous drainage may
decrease the mortality of severe acute pancreatitis. J
Gastroenterol. 45:77–85. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Greenberg JA, Hsu J, Bawazeer M, Marshall
J, Friedrich JO, Nathens A, Coburn N, May GR, Pearsall E and McLeod
RS: Clinical practice guideline: Management of acute pancreatitis.
Can J Surg. 59:128–140. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bozkurt T, Maroske D and Adler G: Exocrine
pancreatic function after recovery from necrotizing pancreatitis.
Hepatogastroenterology. 42:55–58. 1995.PubMed/NCBI
|
|
16
|
Ibars EP, Sánchez de Rojas EA, Quereda LA,
Ramis RF, Sanjuan VM and Peris RT: Pancreatic function after acute
biliary pancreatitis: Does it change? World J Surg. 26:479–486.
2002.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Appelros S, Lindgren S and Borgström A:
Short and long term outcome of severe acute pancreatitis. Eur J
Surg. 167:281–286. 2001.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tong Z, Ke L, Li B, Li G, Zhou J, Shen X,
Li W, Li N and Li J: Negative pressure irrigation and endoscopic
necrosectomy through man-made sinus tract in infected necrotizing
pancreatitis: A technical report. BMC Surg. 16(73)2016.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rämö JT, Kaye SM, Jukarainen S, Bogl LH,
Hakkarainen A, Lundbom J, Lundbom N, Rissanen A, Kaprio J,
Matikainen N and Pietiläinen KH: Liver fat and insulin sensitivity
define metabolite profiles during a glucose tolerance test in young
adult twins. J Clin Endocrinol Metab. 102:220–231. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Dominici R and Franzini C: Fecal
elastase-1 as a test for pancreatic function: A review. Clin Chem
Lab Med. 40:325–332. 2002.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Martínez J, Laveda R, Trigo C, Frasquet J,
Palazón JM and Pérez-Mateo M: Fecal elastase-1 determination in the
diagnosis of chronic pancreatitis. Gastroenterol Hepatol.
25:377–382. 2002.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
22
|
Adorno ML and Brasil-Neto JP: Assessment
of the quality of life through the SF-36 questionnaire in patients
with chronic nonspecific low back pain. Acta Ortop Bras.
21:202–207. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Bagheri Z, Jafari P, Mahmoodi M and
Dabbaghmanesh MH: Testing whether patients with diabetes and
healthy people perceive the meaning of the items in the Persian
version of the SF-36 questionnaire similarly: A differential item
functioning analysis. Qual Life Res. 26:835–845. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Das SL, Singh PP, Phillips AR, Murphy R,
Windsor JA and Petrov MS: Newly diagnosed diabetes mellitus after
acute pancreatitis: A systematic review and meta-analysis. Gut.
63:818–831. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Malecka-Panas E, Gasiorowska A,
Kropiwnicka A, Zlobinska A and Drzewoski J: Endocrine pancreatic
function in patients after acute pancreatitis.
Hepatogastroenterology. 49:1707–1712. 2002.PubMed/NCBI
|
|
26
|
Tim LO and Segal I: Exocrine pancreatic
function in patients with idiopathic necrosis of the femoral head.
S Afr Med J. 54:441–442. 1978.PubMed/NCBI
|
|
27
|
Tu J, Zhang J, Ke L, Yang Y, Yang Q, Lu G,
Li B, Tong Z, Li W and Li J: Endocrine and exocrine pancreatic
insufficiency after acute pancreatitis: Long-term follow-up study.
BMC Gastroenterol. 17(114)2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tu J, Yang Y, Zhang J, Yang Q, Lu G, Li B,
Tong Z, Ke L, Li W and Li J: Effect of the disease severity on the
risk of developing new-onset diabetes after acute pancreatitis.
Medicine (Baltimore). 97(e10713)2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Donnally CJ III, Gupta A, Bensalah K,
Tuncel A, Raman J, Pearle MS and Lotan Y: Longitudinal evaluation
of the SF-36 quality of life questionnaire in patients with kidney
stones. Urol Res. 39:141–146. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Fujio S, Arimura H, Hirano H, Habu M,
Bohara M, Moinuddin FM, Kinoshita Y and Arita K: Changes in quality
of life in patients with acromegaly after surgical remission-A
prospective study using SF-36 questionnaire. Endocr J. 64:27–38.
2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gardikiotis I, Manole A and Azoicăi D:
Quality of life with mastectomy for breast cancer, in terms of
patients' responses of SF-36 questionnaire. Rev Med Chir Soc Med
Nat Iasi. 119:529–535. 2015.PubMed/NCBI
|
|
32
|
Iudici M, Cuomo G, Vettori S, Avellino M
and Valentini G: Quality of life as measured by the short-form 36
(SF-36) questionnaire in patients with early systemic sclerosis and
undifferentiated connective tissue disease. Health Qual Life
Outcomes. 11(23)2013.PubMed/NCBI View Article : Google Scholar
|
|
33
|
López-Pérez P, Miranda-Novales G,
Segura-Méndez NH, Del Rivero-Hernández L, Cambray-Gutiérrez C and
Chávez-García A: Study of quality of life in adults with common
variable immunodeficiency by using the questionnaire SF-36. Rev
Alerg Mex. 61:52–58. 2014.PubMed/NCBI(In Spanish).
|
|
34
|
Shu J, Lo S, Phillips M, Sun F, Seldin DC,
Berenbaum I, Berk JL and Sanchorawala V: Depression and anxiety in
patients with AL amyloidosis as assessed by the SF-36
questionnaire: Experience in 1226 patients. Amyloid. 23:188–193.
2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Pezzilli R, Morselli-Labate AM, Frulloni
L, Cavestro GM, Ferri B, Comparato G, Gullo L and Corinaldesi R:
The quality of life in patients with chronic pancreatitis evaluated
using the SF-12 questionnaire: A comparative study with the SF-36
questionnaire. Dig Liver Dis. 38:109–115. 2006.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wright SE, Lochan R, Imrie K, Baker C,
Nesbitt ID, Kilner AJ and Charnley RM: Quality of life and
functional outcome at 3, 6 and 12 months after acute necrotising
pancreatitis. Intensive Care Med. 35:1974–1978. 2009.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Halonen KI, Pettilä V, Leppäniemi AK,
Kemppainen EA, Puolakkainen PA and Haapiainen RK: Long-term
health-related quality of life in survivors of severe acute
pancreatitis. Intensive Care Med. 29:782–786. 2003.PubMed/NCBI View Article : Google Scholar
|