Introduction
Diabetic nephropathy (DN) is one of the main
complications of diabetic microangiopathy and one of the main
causes of uremia. The morbidity and mortality of DN in diabetic
patients are both high, which is a serious threat to their quality
of life and health (1,2). Clinically, the early symptoms of DN
onset are not obvious, and the indicator changes are usually not
obvious in routine detection, therefore difficult to detect.
However, in the late stage, the disease progresses very quickly,
and the liver and kidney functions also decline rapidly, which will
also lead to poor prognosis due to lack of timely treatment
(3,4). Therefore, for DN patients, early
diagnosis and timely treatment have important clinical
significance.
Vitamin D binding protein (VDBP) belongs to the
binding protein albumin family. It is mainly synthesized by liver
and then reabsorbed by proximal tubular epithelial cells after
glomerular filtration (5). Previous
studies confirmed that urine VDBP was a new biomarker of
tubulointerstitial injury independent of proteinuria, and it mainly
appeared in the early stage of inflammatory reaction and
tubulointerstitial fibrosis and had high sensitivity to renal
inflammation (6). Inflammation
played a vital role in the pathogenesis of DN (7). In addition, previous studies found
that abundant miRNA expression could be seen in kidney tissues of
DN patients, and reported that its expression could reflect the
condition of patients to a certain extent, and that miRNA and DN
were closely related (8).
miR-155-5p is a miRNA that plays an important regulatory role in
the development and progression of tumors, and its diagnostic and
prognostic value in tumors has also been confirmed (9). Previous study also discovered that
miR-155-5p was highly expressed in DN, and it was considered that
its expression was tied to the severity of DN patients (10).
However, there is relatively scarce research on the
diagnostic value of VDBP and miR-155-5p in DN at present, so we
explored the diagnostic value of VDBP and miR-155-5p in DN, and
analyzed the correlation between VDBP and urinary microalbumin
(mAlb) (11), which is the main
basis indicator for DN diagnosis to provide more reference
schemes.
Patients and methods
General information
From April 2015 to January 2017, 145 patients with
type 2 diabetes were selected as research targets, including 75
male patients and 70 female patients. Their average age was
(68.02±5.33) years, including 71 DN patients (DN group) and 74
non-DN patients (diabetes group). Inclusion criteria were as
follows: Patients who met the diagnostic criteria for type 2
diabetes of the American Diabetes Association (12). Patients diagnosed as DN by
pathological (biopsy) diagnosis were included in DN group.
Exclusion criteria were as follows: patients with primary renal
diseases, other diabetic complications, ketoacidosis or other
metabolic diseases; patients who had used immunosuppressive agents
or nephrotoxic drugs in the recent past; patients with malignant
tumors, severe infectious diseases, other severe diabetic
complications; patients who refused to participate in the
study.
The study was approved by the Ethics Committee of
HwaMei Hospital (Ningbo, China). All patients and their families
agreed to participate in the study and signed informed consents
were obtained from the patients and/or their guardians.
Indicator detection RT-PCR detection
of miR-155-5p expression
Venous blood (3 ml) of all patients was drawn on an
empty stomach, and then centrifuged for 10 min at 8,000 x g at 4˚C.
Serum was taken for detection, and total RNA in serum was extracted
with TRIzol reagent (15596018; Thermo Fisher Scientific). The
purity and concentration of RNA were detected with ultraviolet
spectrophotometer, and then 5 µg of total RNA was taken,
respectively, and reverse transcription cDNA was performed
following the instructions of the reverse transcription kit
(AQ202-01; TransGen Biotech). The reaction parameters were as
follows: 37˚C for 10 min, 45˚C for 30 min, 72˚C for 4 min.
miR-155-5p amplification system (PCR kit; AQ201-01; TransGen
Biotech): cDNA 1 µl, upstream and downstream primers 0.4 µl each,
2X TransTaq® Tip Green qPCR SuperMix 10 µl, Passive
Reference Dye (50X) 0.4 µl, ddH2O supplemented to 20 µl.
Amplification conditions: PCR reaction conditions were as follows:
Pre-denaturation at 94˚C for 45 sec, denaturation at 94˚C for 10
sec, annealing extension at 60˚C for 45 sec, a total of 40 cycles.
Each sample was provided with 3 repeated wells, and the experiment
was carried out 3 times. U6 was used as the internal reference and
2-ΔΔct was used to analyze the data.
Detection of VDBP, mAlb and other
biochemical indicators
Urine VDBP (ml023696; Shanghai Enzyme Linked
Biotechnology Co., Ltd.) was detected by ELISA and mAlb was
detected by immunoturbidimetry. Fasting venous blood (5 ml) of
patients was drawn, and then centrifuged for 10 min at 8,000 x g at
4˚C. Serum was taken and the serum glycosylated hemoglobin A1c
(HbA1c), serum creatinine (SCr), blood urea (UREA) and cystatin C
(Cys C) were detected by automatic biochemical analyzer, and 24-h
urine protein of patients was detected.
Statistical analysis
In this study, the experimental data were
statistically analyzed via SPSS 19.0 software, the counting data
were checked through Chi-square test, and the measurement data were
assessed via mean ± standard deviation. Moreover, t-test was
employed for comparison between the two groups, GraphPad Prism 6
software was employed for drawing the experimental illustrations,
and Pearson's was employed for correlation analysis. ROC results
were analyzed via STATA software. SPSS was used to analyze data of
the two groups, binary logistic analysis was used to calculate the
predictive factors, and then ROC curve analysis was carried out to
calculate the diagnostic sensitivity and specificity. Difference of
P<0.05 was considered to be statistically significant.
Results
General data
There was no significant difference in sex, age and
BMI between the two groups (P>0.05), as shown in Table I.
 | Table IGeneral data. |
Table I
General data.
| Factor | DN group (n=71) | Diabetes group
(n=74) | t/χ2
value | P-value |
|---|
| Sex | | | 0.008 | 0.927 |
|
Male | 37 (52.11) | 38 (51.35) | | |
|
Female | 34 (47.89) | 36 (48.65) | | |
| Age, years) | | | 0.003 | 0.959 |
|
≤68 | 31 (43.66) | 32 (43.24) | | |
|
>68 | 40 (56.34) | 42 (56.76) | | |
| BMI,
kg/m2 | | | 0.007 | 0.932 |
|
≤23 | 36 (50.70) | 37 (50.00) | | |
|
>23 | 35 (49.30) | 37 (50.00) | | |
| Educational
level | | | 0.011 | 0.916 |
|
Below junior
high school | 32 (45.07) | 34 (45.95) | | |
|
Junior high
school and above | 39 (54.93) | 40 (54.05) | | |
| Place of
residence | | | 0.000 | 0.987 |
|
Countryside | 45 (63.38) | 47 (63.51) | | |
|
City or
town | 26 (36.62) | 27 (36.49) | | |
| Fasting blood glucose
(mmol/l) | 8.35±1.58 | 8.47±1.53 | 0.465 | 0.643 |
| HbA1c (mmol/l) | 8.32±1.65 | 8.41±1.74 | 0.319 | 0.750 |
| SCr (µmol/l) | 93.21±21.66 | 48.26±9.52 | 16.29 | <0.001 |
| UREA (mmol/l) | 8.67±1.18 | 5.13±0.42 | 24.26 | <0.001 |
Expression levels of serum miR-155-5p
and urine VDBP
The expression levels of serum miR-155-5p and urine
VDBP in the DN group were significantly higher than those in the
diabetes group, with statistically significant difference
(P<0.05), as shown in Table
II.
 | Table IIExpression of serum miR-155-5p and
urine VDBP. |
Table II
Expression of serum miR-155-5p and
urine VDBP.
| Factor | DN group (n=71) | Diabetes group
(n=74) | t value | P-value |
|---|
| miR-155-5p | 3.25±1.53 | 1.82±0.93 | 6.832 | <0.001 |
| Urine VDBP
(ng/ml) | 61.98±31.85 | 22.51±9.16 | 10.23 | <0.001 |
Detection of other relevant
indicators
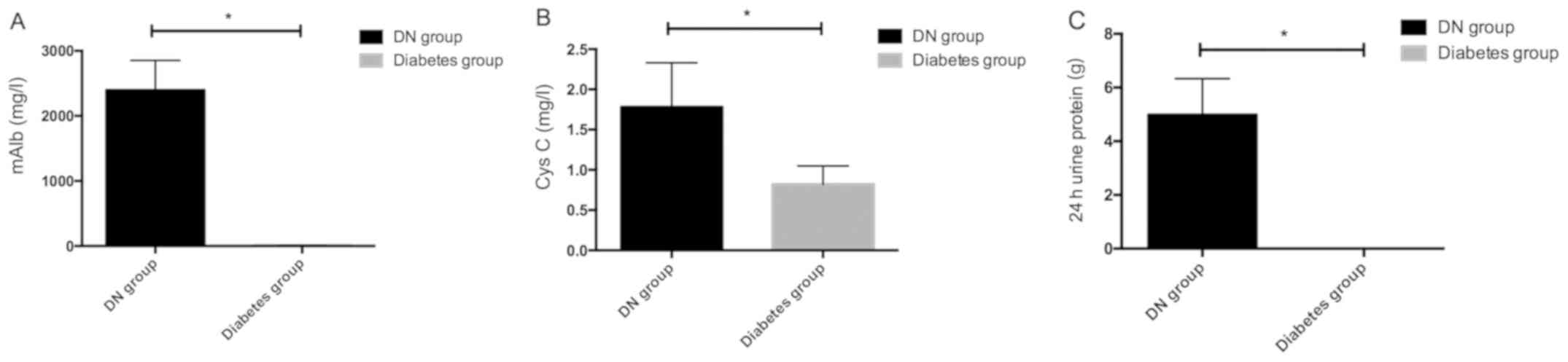
In order to further compare differences between DN
patients and non-DN patients, we further compared the expression
levels of mAlb, Cys C and 24-h urine protein of patients in the two
groups. The results showed that mAlb, Cys C and 24-h urine protein
in the DN group were significantly higher than those in the
diabetes group, with statistically significant differences
(P<0.05), as shown in Fig.
1.
Correlation analysis of serum
miR-155-5p, urine VDBP and mAlb, Cys C and 24-h urine protein in DN
patients
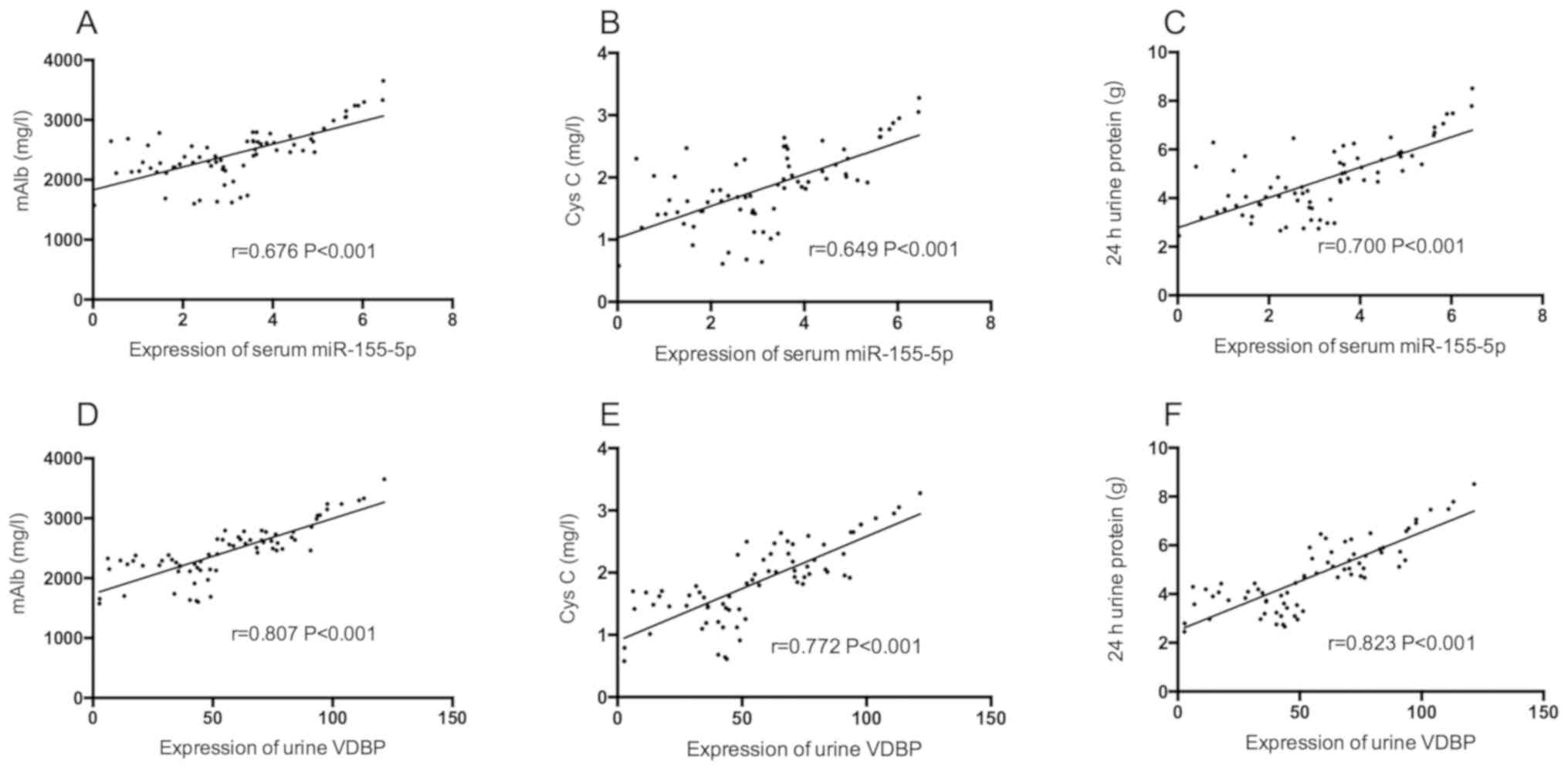
Serum miR-155-5p and mAlb, Cys C and 24-h urine
protein in DN patients were positively correlated (P<0.05),
while urine VDBP and mAlb, Cys C and 24-h urine protein were
positively correlated (P<0.05), as shown in Table III and Fig. 2.
 | Table IIICorrelation analysis of serum
miR-155-5p, urine VDBP and mAlb, Cys C and 24-h urine protein in DN
patients. |
Table III
Correlation analysis of serum
miR-155-5p, urine VDBP and mAlb, Cys C and 24-h urine protein in DN
patients.
| | Serum miR-155-5p | Urine VDBP |
|---|
| Indicators | r value | P-value | r value | P-value |
|---|
| mAlb | 0.676 | <0.001 | 0.807 | <0.001 |
| Cys C | 0.649 | <0.001 | 0.772 | <0.001 |
| 24-h urine
protein | 0.700 | <0.001 | 0.823 | <0.001 |
Diagnostic value of single and joint
detection of serum miR-155-5p and urine VDBP in DN
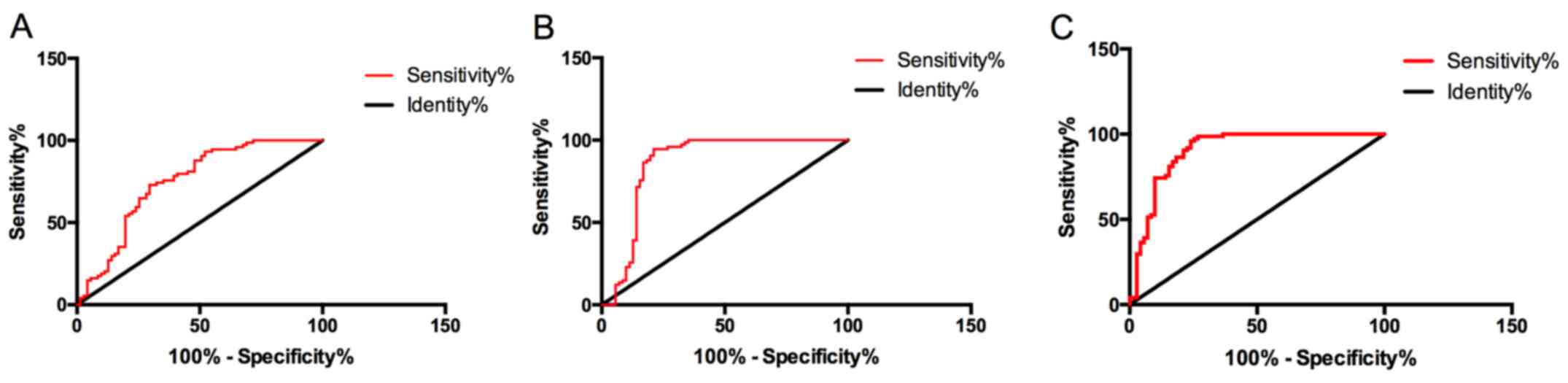
The diagnostic sensitivity of miR-155-5p to DN was
75.68%, specificity was 64.79%, AUC was 0.746, 95% CI was
0.664-0.828, and cut-off value was 2.6; the diagnostic sensitivity
of urine VDBP to DN was 85.14%, specificity was 83.10%, AUC was
0.859, 95% CI was 0.787-0.931, and cut-off value was 31.24 ng/ml;
the diagnostic sensitivity of joint diagnosis of serum miR-155-5p
and urine VDBP was 93.24%, specificity was 76.06%, AUC was 0.904,
and 95% CI was 0.851-0.958. Although serum miR-155-5p and urine
VDBP had certain diagnostic value for DN, the sensitivity and AUC
of joint diagnosis were higher than that of single diagnosis, and
the former had higher diagnostic value, as shown in Fig. 3.
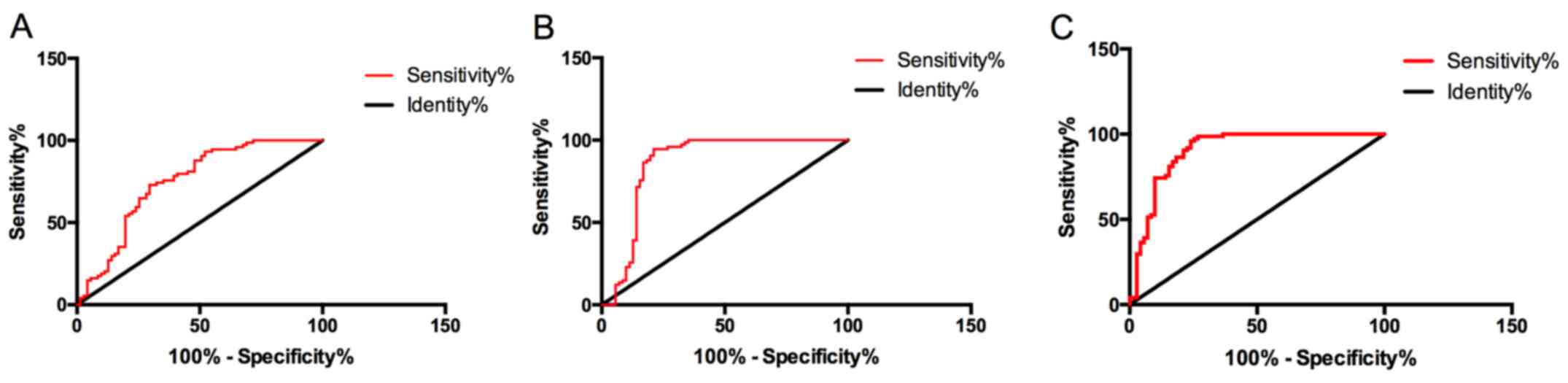 | Figure 3Diagnostic value of single and joint
detection of serum miR-155-5p and urine VDBP in DN. (A) The
diagnostic sensitivity of serum miR-155-5p to DN was 75.68%,
specificity was 64.79%, AUC was 0.746, 95% CI was 0.664-0.828, and
cut-off value was 2.6. (B) The diagnostic sensitivity of urine VDBP
to DN was 85.14%, specificity was 83.10%, AUC was 0.859, 95% CI was
0.787-0.931, and the cut-off value was 31.24 ng/ml. (C) The
diagnostic sensitivity of joint diagnosis of serum miR-155-5p and
urine VDBP for DN was 93.24%, specificity was 76.06%, AUC was
0.904, and 95% CI was 0.851-0.958. VDBP, vitamin D binding protein;
DN, diabetic nephropathy. |
Prognostic value of serum miR-155-5p
and urine VDBP in poor prognosis of patients with DN
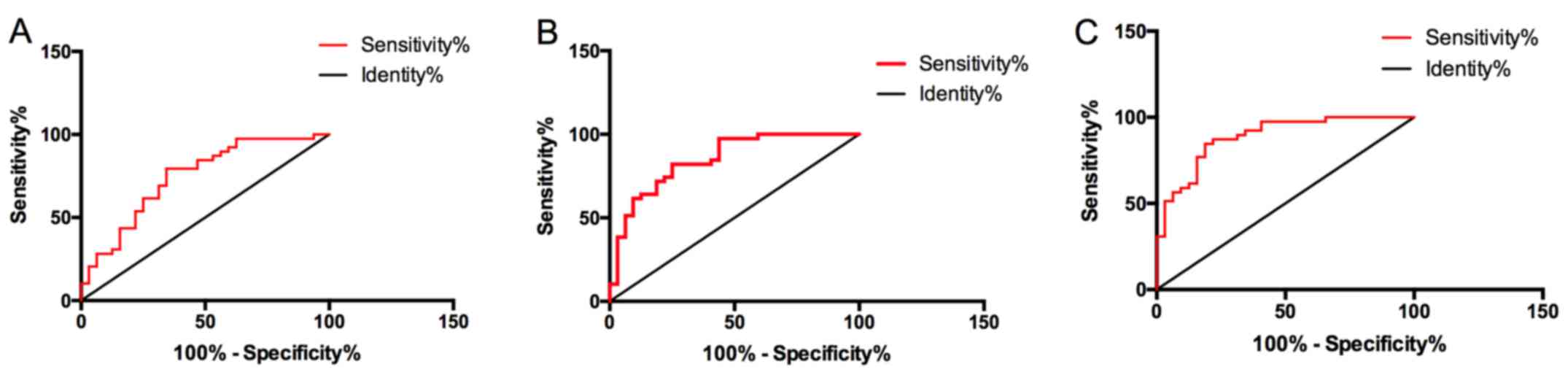
All DN patients were followed up for 2 years, among
them 32 patients entered end-stage renal disease (ESRD) during the
follow-up period. The serum miR-155-5p and urine VDBP of ESRD
patients were significantly higher than those of ESRD patients
without ESRD, with statistically significant difference
(P<0.05). ROC curve showed that the sensitivity, specificity,
AUC, 95% CI and cut-off value of serum miR-155-5p were 74.36,
65.63%, 0.744, 0.628-0.861, 3.409, 82.05 and 71.88%, respectively,
for predicting poor prognosis of DN patients. AUC was 0.849, 95% CI
was 0.759-0.939, and the cut-off value was 62.06 ng/ml. The
sensitivity of joint detection of serum miR-155-5p and urine VDBP
to predict poor prognosis of DN patients was 89.74%, specificity
was 65.63%, AUC was 0.886, 95% CI was 0.810-0.963, and the joint
detection had higher prediction value for poor prognosis of DN
patients, as shown in Table IV and
Fig. 4.
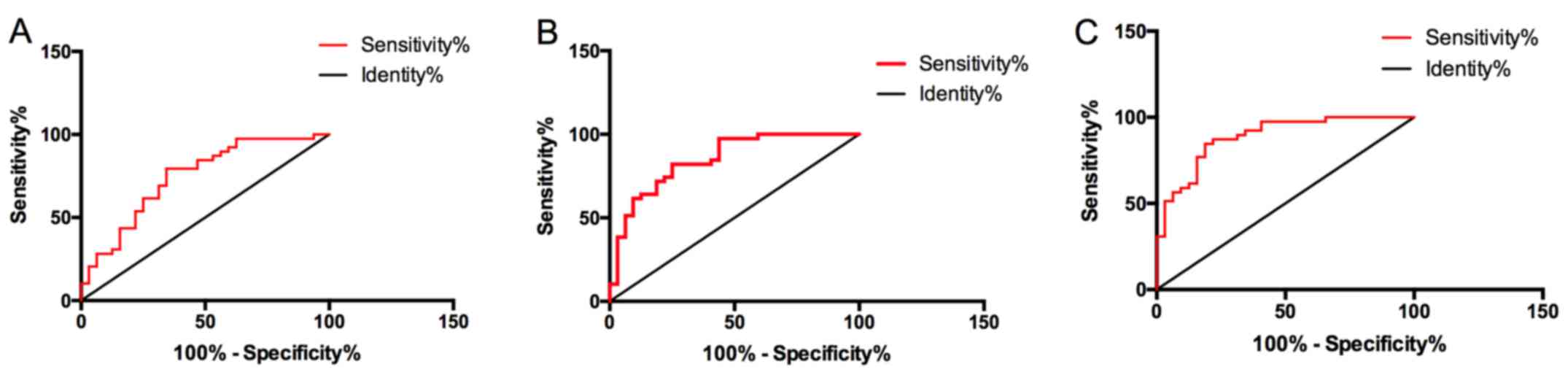 | Figure 4Predictive value of serum miR-155-5p
and urine VDBP for poor prognosis of DN patients. (A) The
predictive sensitivity of serum miR-155-5p to the occurrence of
ESRD was 74.36%, specificity was 65.63%, AUC was 0.744, 95% CI was
0.628-0.861, and cut-off value was 3.409. (B) The predictive
sensitivity of urine VDBP to the occurrence of ESRD was 782.05%,
specificity was 71.88%, AUC was 0.849, 95% CI was 0.759-0.939, and
the cut-off value was 62.06 ng/ml. (C) The predictive sensitivity
of joint detection of serum miR-155-5p and urine VDBP for the
occurrence of ESRD was 89.74%, specificity was 65.63%, AUC was
0.886, and 95% CI was 0.810-0.963. VDBP, vitamin D binding protein;
DN, diabetic nephropathy; ESRD, end-stage renal disease. |
 | Table IVExpression of serum miR-155-5p and
urine VDBP in DN patients with different prognosis. |
Table IV
Expression of serum miR-155-5p and
urine VDBP in DN patients with different prognosis.
| Factor | ESRD group
(n=32) | Non-ESRD group
(n=39) | t value | P-value |
|---|
| miR-155-5p | 4.06±1.09 | 2.82±0.88 | 5.305 | <0.001 |
| Urine VDBP
(ng/ml) | 73.82±24.25 | 43.58±18.93 | 5.706 | <0.001 |
Discussion
Clinically, pathogenesis of DN has a relatively
complicated mechanism, and its occurrence is also a common cause of
renal failure. However, if diagnosis and treatment can be carried
out as soon as possible, the progression of patients can be delayed
or even reversed (13,14). Therefore, it is of great clinical
significance to find a diagnosis method with high sensitivity and
specificity for DN patients.
In the present study, it was first found that urine
VDBP and serum miR-155-5p in DN patients were higher than those in
diabetic patients, which suggested that both urine VDBP and serum
miR-155-5p might be tied to the pathogenesis of DN. As a
glycosylated α-globulin, VDBP is mainly synthesized by liver and
filtered by glomerulus. In addition to binding and transporting
vitamin D and its metabolic products, it can also be converted into
an activating factor of macrophages to promote polarization of
macrophages (15,16). The increase of VDBP is bound with
the injury degree of tubulointerstitium and inflammatory reaction
(17). However, miR, as a
non-coding microRNA, was revealed previously to exert a crucial
influence on the development and progression of DN by regulating
various mechanisms, which suggested that it might be a target for
diagnosis and treatment of DN (18). These studies also confirmed our
conclusion. Subsequently, in order to further explore the clinical
value of urine VDBP and serum miR-155-5p on DN, other DN-related
indicators were also detected, mAlb, Cys C and 24-h urine protein,
and the correlation between them and urine VDBP as well as serum
miR-155-5p were analyzed; the results showed that mAlb, Cys C and
24-h urine protein in DN patients were significantly higher than
those in normal diabetic patients. mAlb is a sensitive and reliable
indicator for DN kidney injury, and was proven previously to be a
vital reference indicator for DN diagnosis (19). Cys C, as an endogenous indicator,
can freely filter through glomerulus and be reabsorbed and degraded
in proximal convoluted tubules. Cys C is very sensitive to the
early function of glomerulus and is also a sensitive indicator
reflecting glomerular filtration function (20). However, 24-h proteinuria is one of
the important indicators for judging glomerular function. When 24-h
proteinuria increases, it indicates further aggravation of
metabolic disorder and kidney injury in vivo (21). Through correlation analysis of urine
VDBP, serum miR-155-5p and the nephrotic sensitive indicators, it
was discovered that urine VDBP, serum miR-155-5p and mAlb, Cys C
and 24-h urine protein were positively correlated, which further
indicated that the occurrence of urine VDBP, serum miR-155-5p and
DN were relevant.
Subsequently, ROC analysis was carried out in order
to study the diagnostic value of urine VDBP and serum miR-155-5p
for DN. ROC is currently a common method for evaluating the medical
diagnostic efficiency. And the results demonstrated that although
urine VDBP and serum miR-155-5p had good diagnostic value, the AUC
of their joint detection for DN diagnosis was as high as 0.904,
which indicated that urine VDBP and serum miR-155-5p might be used
as a new diagnostic mode for DN diagnosis. Previous studies
(22) reported that miR-155-5p was
highly expressed in renal tissues of DN patients, and its
expression gradually increased with the progression of the disease,
which revealed that it might also be tied to disease progression.
Once entering stage ESRD, DN patients become more difficult to
treat, and their condition will be almost impossibile to reverse,
which also indicates poor prognosis (23). Therefore, patients were divided into
ESRD group and non-ESRD group according to the follow-up situation,
and the predictive value of urine VDBP and serum miR-155-5p was
analyzed for poor prognosis of DN patients; the results showed that
urine VDBP had higher sensitivity to poor prognosis of DN patients
than serum miR-155-5p, but the sensitivity was the highest when
joint detection was performed, and the diagnostic AUC could be as
high as 0.886, which indicated that the joint detection of urine
VDBP and serum miR-155-5p also had higher predictive value for
their poor prognosis. This was also the first time that the joint
detection of urine VDBP and serum miR-155-5p was found to have good
predictive value for the onset and prognosis of DN.
In conclusion, urine VDBP and serum miR-155-5p have
good diagnostic value for DN, but their joint diagnostic value is
higher, and their expression levels are all linked to mAlb of DN
patients, which may be used as new biological indicators for
diagnosis and disease assessment. However, we did not further
analyze the risk factors for poor prognosis of DN patients, nor did
we conduct relevant basic experiments to clarify the effects of
VDBP and miR-155-5p on the kidneys. Therefore, further study with
expanded sample numbers is still required.
Acknowledgements
Not applicable.
Funding
The study was supported by the Nephrology Research
Center of East Zhejiang (Zhejiang Health Commission 2015, no. 21)
and the ‘Ningbo City Focuses on Fostering Disciplines’ project (no.
2016022).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XB and LG conceived and designed the study. XB, QL,
KT and LG were responsible for the acquisition, analysis and
interpretation of the data. XB drafted the manuscript. QL revised
the manuscript critically for important intellectual content. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
HwaMei Hospital (Ningbo, China). Signed informed consents were
obtained from the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhuang L, Jin G, Hu X, Yang Q and Shi Z:
The inhibition of SGK1 suppresses epithelial-mesenchymal transition
and promotes renal tubular epithelial cell autophagy in diabetic
nephropathy. Am J Transl Res. 11:4946–4956. 2019.PubMed/NCBI
|
|
2
|
Coskun ZM, Ersoz M, Adas M, Hancer VS,
Boysan SN, Gonen MS and Acar A: Kruppel-like transcription factor-4
gene expression and DNA methylation status in type 2 diabetes and
diabetic nephropathy patients. Arch Med Res. 50:91–97.
2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Jiang S, Yu T, Zhang Z, Fang J, Wang Y,
Yang Y, Liu L, Zou G, Gao H, Zhuo L, et al: Prognostic nomogram and
score to predict renal survival of patients with biopsy-proven
diabetic nephropathy. Diabetes Res Clin Pract.
155(107809)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Grujicic M, Salapura A, Basta-Jovanovic G,
Figurek A, Micic-Zrnic D and Grbic A: Non-diabetic kidney disease
in patients with type 2 diabetes mellitus - 11-year experience from
a single center. Med Arh. 73:87–91. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Fawzy MS and Beladi FI: Association of
circulating vitamin D, VDBP, and vitamin D receptor expression with
severity of diabetic nephropathy in a group of Saudi type 2
diabetes mellitus patients. Clin Lab. 64:1623–1633. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mirković K, Doorenbos CR, Dam WA, Lambers
Heerspink HJ, Slagman MC, Nauta FL, Kramer AB, Gansevoort RT, van
den Born J, Navis G, et al: Urinary vitamin D binding protein: A
potential novel marker of renal interstitial inflammation and
fibrosis. PLoS One. 8(e55887)2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Gu J, Huang W, Zhang W, Zhao T, Gao C, Gan
W, Rao M, Chen Q, Guo M, Xu Y, et al: Sodium butyrate alleviates
high-glucose -induced renal glomerular endothelial cells damage via
inhibiting pyroptosis. Int Immunopharmacol.
75(105832)2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ebadi Z, Moradi N, Kazemi Fard T,
Balochnejadmojarrad T, Chamani E, Fadaei R and Fallah S: Captopril
and spironolactone can attenuate diabetic nephropathy in Wistar
rats by targeting microRNA-192 and microRNA-29a/b/c. DNA Cell Biol.
38:1134–1142. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Shi Q, Zhang Y, Liu W, Xiao H, Qi Y, Li J
and Luo B: Latent membrane protein 2A inhibits expression level of
Smad2 through regulating miR-155-5p in EBV-associated gastric
cancer cell lines. J Med Virol. 92:96–106. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wang J, Wang G, Liang Y and Zhou X:
Expression profiling and clinical significance of plasma microRNAs
in diabetic nephropathy. J Diabetes Res.
2019(5204394)2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Xie J, Wang X, Zhang Y, Li H, Xu Y and
Zheng D: The longitudinal effect of subclinical hypothyroidism on
urine microalbumin-to-urine creatinine ratio in patients with type
2 diabetes mellitus. BMC Endocr Disord. 19(84)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Krueger DA, Northrup H, Northrup H,
Krueger DA, Roberds S, Smith K, Sampson J, Korf B, Kwiatkowski DJ,
Mowat D, et al: International Tuberous Sclerosis Complex Consensus
Group: Tuberous sclerosis complex surveillance and management:
Recommendations of the 2012 International Tuberous Sclerosis
Complex Consensus Conference. Pediatr Neurol. 49:255–265.
2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kocak MZ, Aktas G, Erkus E, Duman TT, Atak
BM and Savli H: Mean platelet volume to lymphocyte ratio as a novel
marker for diabetic nephropathy. J Coll Physicians Surg Pak.
28:844–847. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Prabu P, Rome S, Sathishkumar C, Gastebois
C, Meugnier E, Mohan V and Balasubramanyam M: MicroRNAs from
urinary extracellular vesicles are non-invasive early biomarkers of
diabetic nephropathy in type 2 diabetes patients with the ‘Asian
Indian phenotype’. Diabetes Metab. 45:276–285. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fawzy MS and Abu AlSel BT: Assessment of
vitamin D-binding protein and early prediction of nephropathy in
type 2 Saudi diabetic patients. J Diabetes Res.
2018(8517929)2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Shoukry A, Bdeer S-A and El-Sokkary RH:
Urinary monocyte chemoattractant protein-1 and vitamin D-binding
protein as biomarkers for early detection of diabetic nephropathy
in type 2 diabetes mellitus. Mol Cell Biochem. 408:25–35.
2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tian XQ, Zhao LM, Ge JP, Zhang Y and Xu
YC: Elevated urinary level of vitamin D-binding protein as a novel
biomarker for diabetic nephropathy. Exp Ther Med. 7:411–416.
2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Akhbari M, Khalili M, Shahrabi-Farahani M,
Biglari A and Bandarian F: Expression level of circulating cell
free miR-155 gene in serum of patients with diabetic nephropathy.
Clin Lab. 65(65)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yang H, Xu W, Zhou Z, Liu J, Li X, Chen L,
Weng J and Yu Z: Curcumin attenuates urinary excretion of albumin
in type II diabetic patients with enhancing nuclear factor
erythroid-derived 2-like 2 (Nrf2) system and repressing
inflammatory signaling efficacies. Exp Clin Endocrinol Diabetes.
123:360–367. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Siddiqi Z, Karoli R, Kaul A, Fatima J,
Varshney S and Beg MS: Evaluation of neutrophil
gelatinase-associated lipocalin and cystatin C as early markers of
diabetic nephropathy. Ann Afr Med. 16:101–106. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Liu R, Zhu H, Yang JH, Gao ZA, Yuan XX, Li
XC, Wang JY and Chang BC: Can urine albumin/creatinine ratio
replace 24 hs urinary albumin? Zhonghua Nei Ke Za Zhi. 58:377–381.
2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
22
|
Huang Y, Liu Y, Li L, Su B, Yang L, Fan W,
Yin Q, Chen L, Cui T, Zhang J, et al: Involvement of
inflammation-related miR-155 and miR-146a in diabetic nephropathy:
Implications for glomerular endothelial injury. BMC Nephrol.
15(142)2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Wang G, Ouyang J, Li S, Wang H, Lian B,
Liu Z and Xie L: The analysis of risk factors for diabetic
nephropathy progression and the construction of a prognostic
database for chronic kidney diseases. J Transl Med.
17(264)2019.PubMed/NCBI View Article : Google Scholar
|