Introduction
Bone mineral density (BMD) modification in psoriatic
arthritis still represents a largely widespread issue, being the
source of several medical controversies. There are few studies
regarding the manifestation of osteopenia, generalized osteopenia
and osteoporosis in psoriatic arthritis (1).
Localized and systemic bone loss due to increased
activity of osteoclasts is well established in PsA. In contrast,
the mechanisms responsible for pathological bone remodeling in PsA
remain enigmatic although new candidate molecules and pathways have
been identified (2).
The bony skeleton is made of 80% cortical bone and
20% trabecular bone. The trabecular bone has an elevated metabolic
turnover, due to the high surface-volume ratio, eight times higher
than that of the cortical bone.
The BMD variations can be measured earlier in the
trabecular bone, as compared with the cortical one. Concerning the
spine, the articular vertebrae are mainly composed of trabecular
bone, compared with the vertebral plates and the spinal apophyses,
made of cortical bone. The trochanteric area of the femur has a
bone content that is similar to that resulting from the
anteroposterior measurement of the spine, namely trabecular bone,
whereas the femoral neck contains predominantly cortical bone.
There are several techniques used in order to
determine the BMD, four of which are currently available. According
to the anatomical areas measured, they differ in precision and
accuracy: Single photon absorptiometry (SPA); dual ohoton
absorptiometry (DPA); dual-energy X-ray absorptiometry (DEXA) and
quantitative computed tomography (QCT).
Subjects and methods
DEXA represents the most modern and widely accepted
technique. It determined the mineral content of the spine, the
proximal femur and the entire body; it can also be used for
measurements in the forearm. The term mineral content describes the
mineral quantity within the measured area. This allows the
determination of the BMD value, by reporting on the measured
surface or volume. Therefore, the BMD determined by absorptiometric
techniques does not represent a volumetric density, but an area
density, considering the scan is bi-dimensional. The DEXA method is
also used to scan the extremities, a technique known as peripheral
DEXA (pDEXA).
The irradiation, determined by a DEXA examination,
is 0.5 to 5 µSv. It varies depending on the type of device used, as
well as on the area at which the examination is performed. The
irradiation dose corresponds to one tenth of the irradiation area
generated by a lung X-ray.
The direct measurement of the spine BMD allows a
faster determination of trabecular bone loss in early menopausal
women and post-cortisone treatments. The measurement of BMD in the
femur may generate errors by different positioning of the bone
throughout repeated determinations. The cause of errors, which can
lead to increased BMD, are large osteophytes, as well as vertebral
bundles; therefore, in order to avoid these sources of error,
paralleled standard radiological examination is required.
The results obtained by DEXA are: Bone mineral
content (BMC) expressed in grams; bone surface area (area per
square centimeter) and BMD expressed in g/cm2. These
values must be interpreted according to the device used, as well as
the position and the age of the subject.
For the objective determination of the diagnosis,
two scores are currently used:
i) The Z-score represents the difference between the
measured value of BMD and the average value of persons of the same
age and sex with the examined subject, expressed in standard
deviations.
ii) The T-score represents the difference between
the BMD, measured for an individual and the average value of a
young adult, of the same sex, expressed in standard deviations.
Considering the bone mass and the BMD are relatively
stable at the end of growth and upon achieving the peak bone mass,
they are used as reference value in expressing the BMD changes in
standard deviations.
In 1994, WHO established the BMD values measured by
DEXA, which characterizes the diagnosis and severity of
osteoporosis, based on the T-score: Normal BMD: T-score >-1. Low
BMD, with less than a standard deviation from that of a young
adult. Osteopenia: <-2.5 T-score >-1. BMD between -1 and -2.5
standard deviations, compared with that of a young adult.
Osteoporosis: T-score <-2.5. BMD lower than -2.5 standard
deviations, compared with that of a young adult. Confirmed
osteoporosis: T-score <-2.5 plus fracture. BMD lower than -2.5
standard deviations, compared with that of a young adult, when one
or more fractures due to bone fragility occur.
The authors chose a group of 36 patients with
psoriatic arthritis, with different types of arthropathy, out of
the total 82 patients with psoriatic arthritis in the study lot,
for which the BMD was measured, using the DEXA technique.
The chosen study group comprised 12 men, 12
premenopausal women and 12 menopausal women, with psoriatic joint
damage and a group of 36 healthy individuals, divided based on the
same criteria: Men, premenopausal and menopausal women.
The distribution of the cases in the study group by
age was similar precisely so that the age does not represent a
factor that could influence the values of bone densitometry,
considering that age constitutes an important element in the
alteration of BMD and particularly, in the onset of osteoporosis
(1).
The study was approved by the Ethics Committee of
the Oradea County Emergency Clinic Hospital (Oradea, Romania)
(approval nos 1386/2019 and 460/2019, respectively), and written
informed consent was obtained from all the patients.
Results and Discussion
Besides the total demineralizations that affect all
three evaluated segments simultaneously: Lumbar spine, left and
right femur, patients with psoriatic arthritis also present partial
demineralizations, located in one or two of the evaluated segments.
Thus, out of the 36 patients with psoriatic arthritis, there are
partial demineralizations in five patients (13.88%). Of the
patients with psoriatic arthritis with partial demineralization,
only one has both locations at femoral level (2.7%), while the rest
have a partial demineralization with double localization, in which
there is lumbar spine demineralization.
Study of partial bone demineralization
in men
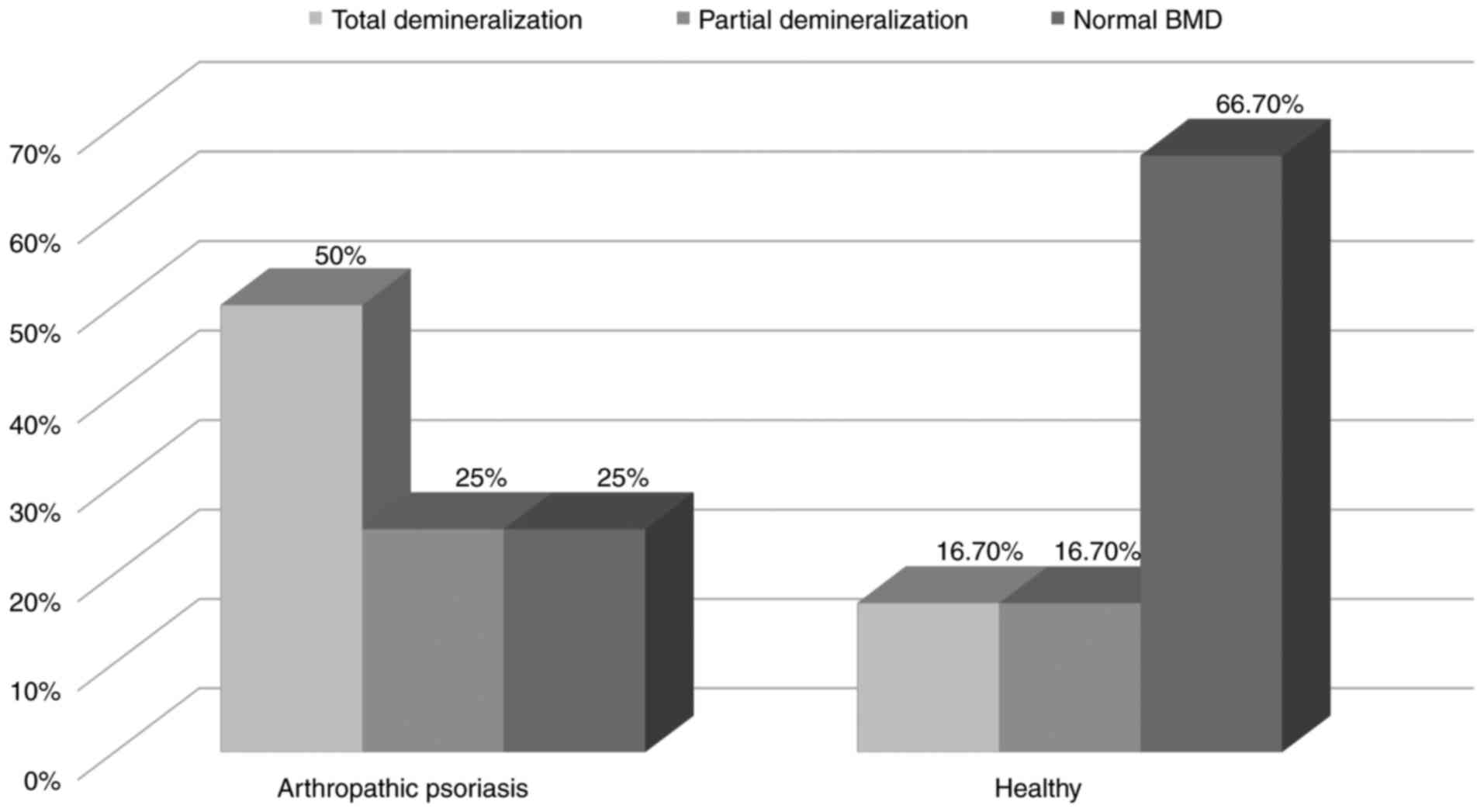
In male patients with psoriatic arthritis, there are
demineralizations in all three evaluated segments (six patients),
representing 50% of the sample volume. There are partial
demineralizations with double localization in three patients (25%)
compared with healthy men, where there is demineralization in all
three analyzed segments in two patients (16.7%) and partial
demineralization in two patients (16.7%), while the rest presents a
normal BMD (Table I) (Fig. 1).
 | Table IChi-square, bone demineralization in
men according to the type of patient. |
Table I
Chi-square, bone demineralization in
men according to the type of patient.
| | Patient type | |
|---|
| Demineralization
type | Arthropathic
psoriasis | Healthy | Total |
|---|
| Partial | | | |
|
Frequency | 3 | 2 | 5 |
|
Expected
frequency | 2.5 | 2.5 | 5.0 |
|
% patient
type | 25.0 | 16.7 | 20.8 |
|
% total | 12.5 | 8.3 | 20.8 |
| Total | | | |
|
Frequency | 6 | 2 | 8 |
|
Expected
frequency | 4.0 | 4.0 | 8.0 |
|
% patient
type | 50.0 | 16.7 | 33.3 |
|
% total | 25.0 | 8.3 | 33.3 |
| No
demineralization | | | |
|
Frequency | 3 | 8 | 11 |
|
Expected
frequency | 5.5 | 5.5 | 11.0 |
|
% patient
type | 25.0 | 66.7 | 45.8 |
|
% total | 12.5 | 33.3 | 45.8 |
| TOTAL | | | |
|
Frequency | 12 | 12 | 24 |
|
Expected
frequency | 12.0 | 12.0 | 24.0 |
|
% patient
type | 100.0 | 100.0 | 100.0 |
|
% total | 50.0 | 50.0 | 100.0 |
This study did not emphasize an association between
the patient type and the presented bone demineralization type
(χ2(2)=4.473, P=0.107) in men (Table II).
 | Table IIChi-square values for bone
demineralization present in men depending on the type of
patient. |
Table II
Chi-square values for bone
demineralization present in men depending on the type of
patient.
| Test | χ2 | df |
Pbilateral |
|---|
| Pearson's
Chi-square | 4.473 | 2 | 0.107 |
Study of partial bone demineralization
in premenopausal women
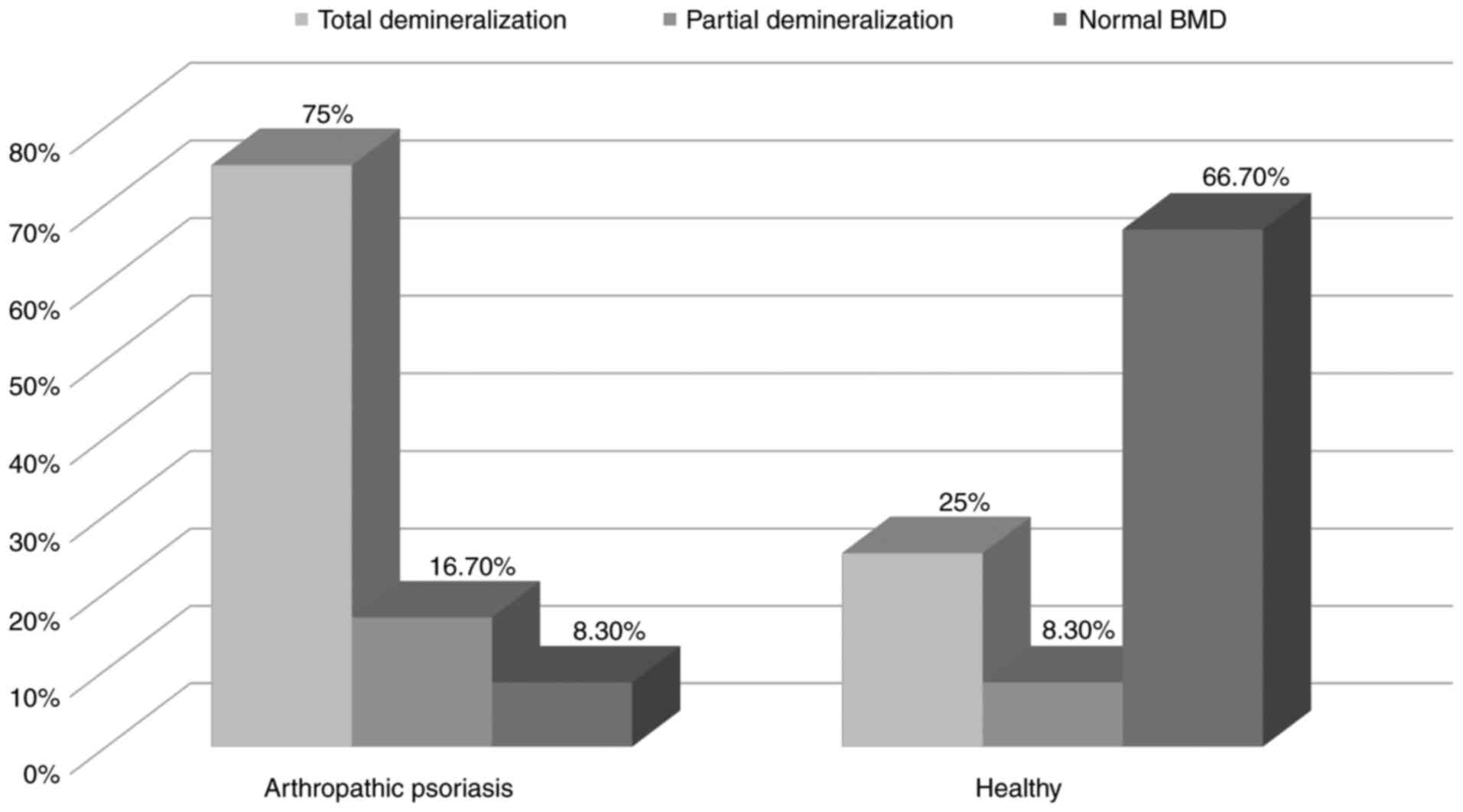
In premenopausal female patients with psoriatic
arthritis, there are demineralizations in all three evaluated
segments (nine patients), representing 75% of the sample volume.
There are partial demineralizations with double localization in two
patients (16.66%) compared with premenopausal female patients,
where there is demineralization in all three analyzed segments in
three patients (25%) and partial demineralization in one patient
(8.66%), while the rest presents a normal BMD (66.66%) (Table III) (Fig. 2).
 | Table IIIChi-square, bone demineralization in
premenopausal women according to the type of patient. |
Table III
Chi-square, bone demineralization in
premenopausal women according to the type of patient.
| | Patient type | |
|---|
| Demineralization
type | Arthropathic
psoriasis | Healthy | Total |
|---|
| Partial | | | |
|
Frequency | 2 | 1 | 3 |
|
Expected
frequency | 1.5 | 1.5 | 3.0 |
|
% patient
type | 16.7 | 8.3 | 12.5 |
|
% total | 8.3 | 4.2 | 12.5 |
| Total | | | |
|
Frequency | 9 | 3 | 12 |
|
Expected
frequency | 6.0 | 6.0 | 12.0 |
|
% patient
type | 75.0 | 25.0 | 50.0 |
|
% total | 37.5 | 12.5 | 50.0 |
| No
demineralization | | | |
|
Frequency | 1 | 8 | 9 |
|
Expected
frequency | 4.5 | 4.5 | 9.0 |
|
% patient
type | 8.3 | 66.7 | 37.5 |
|
% total | 4.2 | 33.3 | 37.5 |
| TOTAL | | | |
|
Frequency | 12 | 12 | 24 |
|
Expected
frequency | 12.0 | 12.0 | 24.0 |
|
% patient
type | 100.0 | 100.0 | 100.0 |
|
% total | 50.0 | 50.0 | 100.0 |
In premenopausal women, there was a significant
association between the patient type and the presented bone
demineralization type (χ2(2)=8.778, P=.012),
as the female patients with psoriatic arthritis present total and
partial demineralization to a larger degree, compared with healthy
individuals (Table IV).
 | Table IVChi-square values for bone
demineralization present in premenopausal women depending on the
type of patient. |
Table IV
Chi-square values for bone
demineralization present in premenopausal women depending on the
type of patient.
| Test | χ2 | df |
Pbilateral |
|---|
| Pearson's
Chi-square | 8.778 | 2 | 0.012 |
Study of partial bone demineralization
in menopausal women
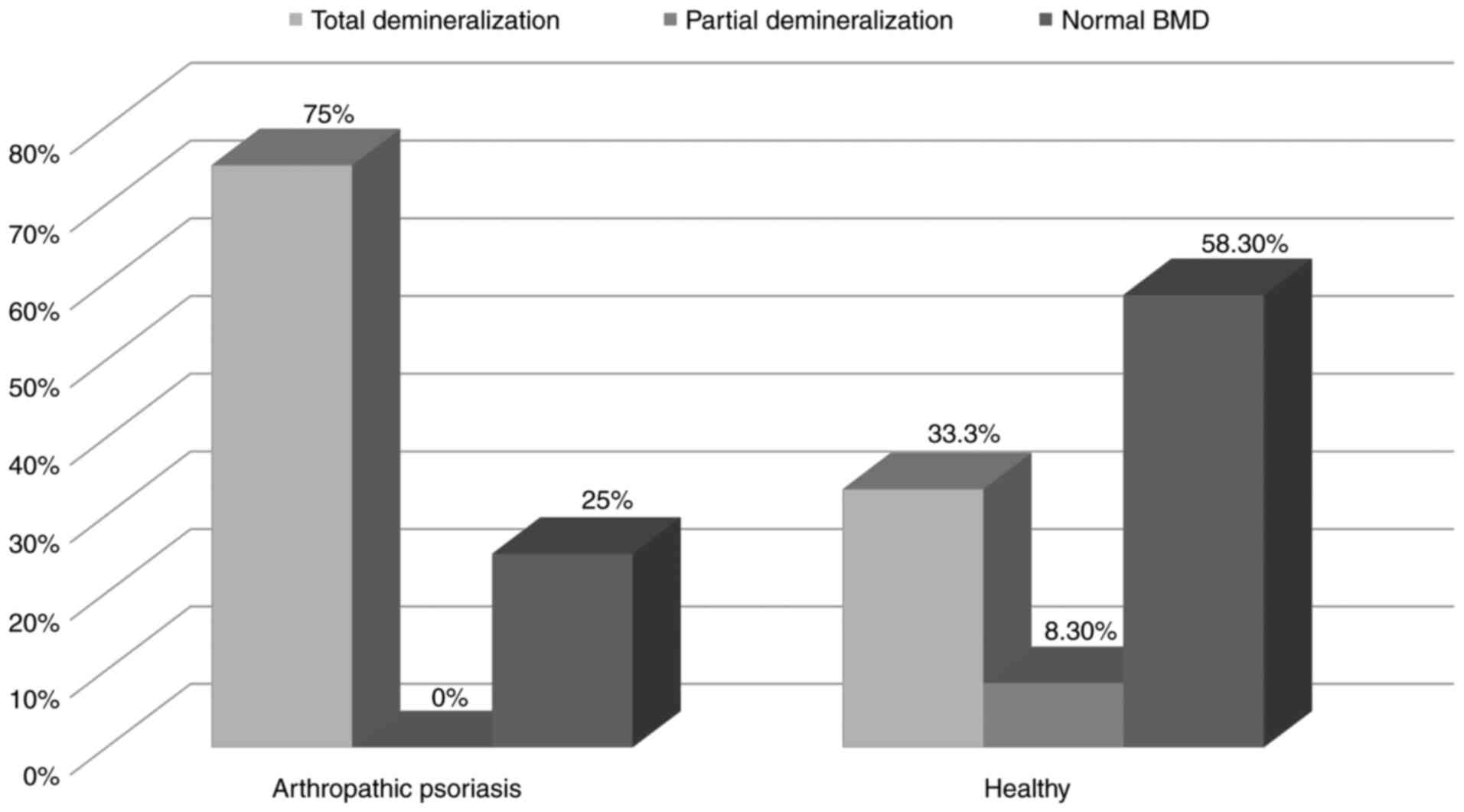
In menopausal female patients with psoriatic
arthritis, there are demineralizations in all three evaluated
segments (nine patients), representing 75% of the sample volume.
There are partial demineralizations with double localization in
three patients (25%) compared with healthy menopausal female
patients, where there is demineralization in all three analyzed
segments in four patients (33.33%) and partial demineralization in
one patient (8.66%), while the rest presents a normal BMD (Table V) (Fig.
3).
 | Table VChi-square, bone demineralization in
menopausal women according to the type of patient. |
Table V
Chi-square, bone demineralization in
menopausal women according to the type of patient.
| | Patient type | |
|---|
| Demineralization
type | Arthropathic
psoriasis | Healthy | Total |
|---|
| Partial | | | |
|
Frequency | 0 | 1 | 1 |
|
Expected
frequency | 0.5 | 0.5 | 1.0 |
|
% patient
type | 0.0 | 8.3 | 4.2 |
|
% total | 0.0 | 4.2 | 4.2 |
| Total | | | |
|
Frequency | 9 | 4 | 13 |
|
Expected
frequency | 6.5 | 6.5 | 13.0 |
|
% patient
type | 75.0 | 33.3 | 54.2 |
|
% total | 37.5 | 16.7 | 54.2 |
| No
demineralization | | | |
|
Frequency | 3 | 7 | 10 |
|
Expected
frequency | 5.0 | 5.0 | 10.0 |
|
% patient
type | 25.0 | 58.3 | 41.7 |
|
% total | 12.5 | 29.2 | 41.7 |
| TOTAL | | | |
|
Frequency | 12 | 12 | 24 |
|
Expected
frequency | 12.0 | 12.0 | 24.0 |
|
% patient
type | 100.0 | 100.0 | 100.0 |
|
% total | 50.0 | 50.0 | 100.0 |
In menopausal women, this study did not highlight an
association between the patient type and the presented bone
demineralization type (χ2(2)=4.523, P=0.104)
(Table VI).
 | Table VIChi-square X2 values for
bone demineralization present in menopausal women depending on the
type of patient. |
Table VI
Chi-square X2 values for
bone demineralization present in menopausal women depending on the
type of patient.
| Test | χ2 | df |
Pbilateral |
|---|
| Pearson's
Chi-square | 4.523 | 2 | 0.104 |
The present study was performed on the three patient
groups: Men, premenopausal women and menopausal women, significant
modifications regarding the alteration of BMD can be observed in
terms of osteopenia in patients with psoriatic arthritis compared
with healthy patients.
According to the comparative study of partial
demineralizations, the following conclusions were drawn: In the
group of men in the study, there is a significant difference of
total demineralization between the patients with psoriatic
arthritis (50%) and the group of healthy patients (16.7%). The
difference is insignificant for partial demineralization: 25% in
patients with psoriatic arthritis and 16.7% in healthy
patients.
In the group of premenopausal women, total
demineralization was found in 75% of the patients with psoriatic
arthritis, compared with 25% in the group of healthy patients.
Partial demineralization was present in 16.7% of the patients with
psoriatic arthritis, and only 8.3% in the healthy patients. There
is a significant difference regarding total demineralization
between the male and female groups, in terms of total
demineralization, as it is more frequent in premenopausal
women.
In menopausal women, total demineralization was
found in 75% of patients with psoriatic arthritis and in 33% of
healthy patients, while no partial demineralization occurred in
women with psoriatic arthritis, compared with the group of healthy
patients (8.3%). The absence of partial demineralization in the
group of menopausal women with psoriatic arthritis, compared with
16.7% of the number of premenopausal women with psoriatic
arthritis, is explained by the role that menopause plays in
accentuating bone demineralization phenomena. Nevertheless, partial
demineralization occurs, in the same proportion, in the two groups
of women, both before menopause and during menopause, which points
to the fact that psoriatic arthritis has an important role in the
occurrence of osteopenia, regardless of the status of
menopause.
In a study on a group of 18 patients with non-axial
psoriatic arthritis and 100 healthy individuals, Frediani et
al (3) showed that BMD was
significantly lower in subjects with arthritis compared with
healthy patients, regardless of sex, age and the status of
menopause. Their study showed that demineralization was observed in
more than 2/3 of the patients with psoriatic arthritis. This
demineralization was not correlated with any signs of inflammation,
or with the duration of the disease. However, there is a delayed
correlation with age and number of menopausal years.
In a study on a group of 52 patients with peripheral
psoriatic arthritis and a control group of 52 healthy individuals,
Nolla et al (4) found no
significant differences between patients with psoriatic arthritis
and control subjects. Nonetheless, in menopausal patients with
psoriatic arthritis, a lower BMD of the femoral neck was found,
compared with the control group. There were no significant
differences in BMD in the lumbar spine in the subgroups of men,
premenopausal women and menopausal women (5). The mineral density of the femoral neck
was not significantly different in men or in premenopausal women
diagnosed with psoriatic arthritis and the control group (3).
In the present study, bone demineralization was
significant in all three patient groups, both total and partial, in
patients with psoriatic arthritis compared with healthy patients.
Bone demineralization manifested as osteopenia, with T-scores
ranging from -2.5 to -1, and not as osteoporosis. Determining BMD
by DEXA technique revealed osteopenia to a higher degree within the
group of patients with psoriatic arthritis compared with the
healthy patients, as well as the absence of osteoporosis in
psoriatic arthritis (6,7).
An important factor in modifying BMD is systemic
corticosteroid therapy, one of the foundations in inflammatory
rheumatism therapy. Treatment with glucocorticoid hormones causes
bone loss, because the rate of bone resorption exceeds that of
formation. The supraphysiological doses of hormones generate an
imbalance by reducing bone formation on the one hand, while
suppressing osteoblast function and increasing resorption on the
other (8,9). Clinical and densitometric studies on
subjects treated with Prednisone 30 mg/day for a long time
demonstrated, in 80% of them, either osteoporosis or the presence
of a complication of the same fractures (10-18).
Topical treatment with dermocorticoids has created a series of
controversies regarding the induced side effects. At skin level,
they can generate dermal atrophy with telangiectosis and purpura,
promote bacterial, fungal or viral skin infections, induce
transient, rosacea and, when applied to the eyelids, can even
induce glaucoma and cataract (19).
In addition, sudden discontinuing of corticosteroids induces
rebound phenomena. The issue of dermocorticoid penetration, which
may disrupt adrenal function, has raised discussion. Currently,
most studies conclude the pituitary-cortico-adrenal axis is not
affected, as well as the absence of the dermocorticoid resonance
regarding BMD. Reduced percutaneous absorption and rapid
biotransformation within the liver are responsible for the
extremely low systemic activity. All of these side effects, induced
by systemic and topical cortisone therapy, can be currently
counteracted by the introduction, even prophylactic, of classic and
alternative therapy on cortisone-induced osteopenia and
osteoporosis (20,21). Some comorbidity therapies have a
negative influence on the evolution of the disease. Beta-blockers
used in the treatment of associated cardiological disorders
negatively influence the evolution of the disease even in their
topical use (22,23). A study, performed on groups of
subjects treated with cortisone, shows a three-fold higher
incidence of fractures (11).
Nuti et al (12) showed that the best technique for
measuring bone density and for assessing the risk of fracture is
DEXA.
Osteodensitometry is considered a major indication
for the evaluation of patients with long-term corticosteroids
(5). Serial bone density
measurements by DEXA, every 6-12 months, are recommended when
long-term corticosteroids are at doses of at least 7.5 mg/day
Prednisone. Thus, it remains an essential method of monitoring
corticosteroids in patients with inflammatory rheumatisms.
Therefore, osteodensitometry is one of the most important methods
for the evaluation of osteoarticular modifications, by decreasing
BMD (18,24).
Osteodensitometry: The modification in BMD
correlates 75% with joint disease in psoriatic arthritis. The
mineral density was significantly lower, falling in the stage of
osteopenia <-2.5 T-score >-1 in subjects with psoriatic
arthritis compared with healthy individuals, without correlating
with sex, age or menopause status.
The presence of total bone demineralization, in
terms of osteopenia, determined by DEXA technique, on the three
levels: Lumbar spine, right femur and left femur, in 75% of
premenopausal women and in the group of menopausal women,
demonstrates the lack of correlation of osteopenia with the
menopause status in psoriatic arthritis.
Acknowledgements
Professional editing, linguistic and technical
assistance was provided by Irina Radu, Individual Service Provider,
certified translator in Medicine and Pharmacy (certificate
credentials: Series E no. 0048).
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
IB was responsible for the clinical management of
patients, the processing and scientific interpretation of the data.
AH was responsible for the statistical processing of the data and
the writing of the manuscript. DB was involved in the data analysis
and was responsible for studying and revising the manuscript. SLI
was responsible for the analysis of the specialized literature. GLF
was responsible for the data processing and revision of the
manuscript. MZ was responsible for the statistical data processing,
drafting and revising of the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Oradea County Emergency Clinic Hospital (Oradea, Romania)
(approval nos 1386/2019 and 460/2019, respectively), and written
informed consent was obtained from all the patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
IB-Head of the Department of Dermatology, Emergency
Clinical Hospital (Oradea, Romania).
References
|
1
|
Pedreira PG, Pinheiro MM and Szejnfeld VL:
Bone mineral density and body composition in postmenopausal women
with psoriasis and psoriatic arthritis. Arthritis Res Ther.
13(R16)2011.PubMed/NCBI View
Article : Google Scholar
|
|
2
|
Paine A and Ritchlin C: Altered bone
remodeling in psoriatic disease: New insights and future
directions. Calcif Tissue Int. 102:559–574. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Frediani B, Allegri A, Falsetti P, Storri
L, Bisogno S, Baldi F, Filippo P and Marcolongo R: Bone mineral
density in patients with psoriatic arthritis. J Reumatol.
28:138–143. 2001.PubMed/NCBI
|
|
4
|
Nolla JM, Fiter J, Rozadilla A,
Gomez-Vaquero C, Mateo L, Rodriguez-Moreno J and Roig-Escofet D:
Bone mineral density in patients with peripheral psoriatic
arthritis. Rev Rhum Engl Ed. 66:457–461. 1999.PubMed/NCBI
|
|
5
|
Chandran S, Aldei A, Johnson SR, Cheung
AM, Salonen D and Gladman DD: Prevalence and risk factors of low
bone mineral density in psoriatic arthritis: A systematic review.
Semin Arthritis Rheum. 46:174–182. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Martinez-Lopez A, Blasco-Morente G,
Giron-Prieto MS, Arrabal-Polo MA, Luque-Valenzuela M, Luna-Del
Castillo JD, Tercedor-Sanchez J and Arias-Santiago S: Linking of
psoriasis with osteopenia and osteoporosis: a cross-sectional
study. Indian J Dermatol Venereol Leprol. 85:153–159.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Muñoz-Torres M, Aguado P, Daudén E,
Carrascosa JM and Rivera R: Osteoporosis and psoriasis. Actas
Dermosifiliogr. 110:642–652. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Ciacli C and Cojocaru M: Systemic
osteoporosis - major complication of psoriatic arthritis. Rom J
Intern Med. 50:173–178. 2012.PubMed/NCBI
|
|
9
|
Kathuria P, Gordon KB and Silverberg JI:
Association of psoriasis and psoriatic arthritis with osteoporosis
and pathological fractures. J Am Acad Dermatol. 76:1045–1053.e3.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Riesco M, Manzano F, Font P, García A and
Nolla JM: Osteoporosis in psoriatic arthritis: An assessment of
densitometry and fragility fractures. Clin Rheumatol. 32:1799–804.
2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Busquets N, Vaquero CG, Moreno JR,
Vilaseca DR, Narváez J, Carmona L and Nolla JM: Bone mineral
density status and frequency of osteoporosis and clinical fractures
in 155 patients with psoriatic arthritis followed in a university
hospital. Reumatol Clin. 10:89–93. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Nuti R, Martini G and Gennari C: Total
body, spine, and femur dual X-ray absorptiometry in spinal
osteoporosis. Calcif Tissue Int. 53:388–93. 1993.PubMed/NCBI
|
|
13
|
Pfeil A, Krojniak L, Renz DM, Reinhardt L,
Franz M, Oelzner P, Wolf G and Böttcher J: Psoriatic arthritis is
associated with bone loss of the metacarpals. Arthritis Res Ther.
18(248)2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
D'Epiro S, Marocco C, Salvi M, Mattozzi C,
Luci C, Macaluso L, Giancristoforo S, Campoli M, Scarnò M,
Migliaccio S, et al: Psoriasis and bone mineral density:
Implications for long-term patients. J Dermatol. 41:783–787.
2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Attia EA, Khafagy A, Abdel-Raheem S, Fathi
S and Saad AA: Assessment of osteoporosis in psoriasis with and
without arthritis: Correlation with disease severity. Int J
Dermatol. 50:30–35. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Harrison BJ, Hutchinson CE, Adams J, Bruce
IN and Herrick AL: Assessing periarticular bone mineral density in
patients with early psoriatic arthritis or rheumatoid arthritis.
Ann Rheum Dis. 61:1007–1011. 2002.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lajevardi V, Abedini R, Moghaddasi M,
Nassiri SF and Goodarzi A: Bone mineral density is lower in male
than female patients with plaque-type psoriasis in Iran. Int J
Womens Dermatol. 3:201–205. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Batani A, Brănișteanu DE, Ilie MA, Boda D,
Ianosi S, Ianosi G and Caruntu C: Assessment of dermal papillary
and microvascular parameters in psoriasis vulgaris using in vivo
reflectance confocal microscopy. Exp Ther Med. 15:1241–1246.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tatu AL, Ionescu MA and Nwabudike LC:
Contact allergy to topical mometasone furoate confirmed by
rechallenge and patch test. Am J Ther. 25:e497–e498.
2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Tatu AL and Nwabudike LC:
Metoprolol-associated onset of psoriatic arthropathy. Am J Ther.
24:e370–e371. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Tatu AL, Elisei AM, Chioncel V, Miulescu M
and Nwabudike LC: Immunologic adverse reactions of β-blockers and
the skin. Exp Ther Med. 18:955–959. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Nwabudike LC and Tatu AL: Using
complementary and alternative medicine for the treatment of
psoriasis: A step in the right direction. JAMA Dermatol.
155(636)2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Nwabudike LC and Tatu AL: Response to use
of complementary and alternative medicine by patients with
psoriasis. J Am Acad Dermatol. 81(e105)2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Grisar J, Bernecker PM, Aringer M, Redlich
K, Sedlak M, Wolozcszuk W, Spitzauer S, Grampp S, Kainberger F,
Ebner W, et al: Ankylosing spondylitis, psoriatic arthritis, and
reactive arthritis show increased bone resorption, but differ with
regard to bone formation. J Rheumatol. 29:1430–1436.
2002.PubMed/NCBI
|