Introduction
Atopic dermatitis (AD) is a complex inflammatory
skin disease with different clinical aspects. This pathology
affects 20% of children and 3% of adults. Several mechanisms have
been described to determine AD: These mechanisms include
dysfunction of the immune system with Th2 predominance with IL4,
IL5, and IL13 production, associated with increased IgE and
decreased gamma interferon. Another mechanism implicated in DA is
the dysfunction of the epidermal barrier. By disrupting this
barrier, antigens can penetrate the skin and generate the
production of inflammatory cytokines that support the underlying
mechanism of the pathology (1).
Quality of life (QoL) is a crucial parameter for the
patient's health, also representing an essential indicator in the
follow-up of patients with atopic dermatitis. Characterized by an
unpredictable evolution, AD evolves from mild forms, when the
manifestations affect only the patient's appearance to severe forms
that require treatment by a multidisciplinary team. Fortunately,
most cases in children are mild forms, but in some cases, they may
present symptoms of aggravation (2).
AD typically starts around the age of 2 months, but
there are cases when the symptoms manifest later. Essential for the
assessment of the disease evolution is the follow-up of daily
activity, sleep, itching, and in more severe cases of depressive
manifestations. Although at first sight, AD appears to be a mild
disease, the diagnosis and treatment must be made by specialists in
allergic diseases with a thorough knowledge of physiology,
pathophysiology, and pharmacology (3). Anamnesis and clinical examination were
the only ways of assessing the QoL in patients with AD, even though
other methods have been elaborated to allow a more objective
assessment. These include the appreciation of sleep, itching and
daily activities.
Several tools can be used to assess the QoL: These
include HRQoL (Health Related Quality of Life). This tool is
multidimensional and analyzes different aspects of life, such as
mental, emotional, and social aspects. The questionnaires for HRQoL
analyze the intensity of the symptoms and their frequency. The
Dermatology Quality Life Index (DLQI) is the most utilized in
dermatology, analyzing such items as the weekly itching, pain and
inflammation. There are also similar questionnaires, such as
Patient-Oriented Eczema Measure (POEM), that analyze weekly
symptoms as well as their daily changes (4).
The age of the patient also influences the QoL of
patients with AD. It has been found that the highest prevalence of
the disease is found in children, about 20%, and consequently, the
disturbance of QoL is higher in children (5). The QoL is mainly influenced by the
severity of AD, and affecting moderate and severe forms rather than
mild forms. As AD is increasing, early recognition of the
manifestations and prompt implementation of therapeutical measures
can limit the consequences of the disease. Far from an acute
disease, AD is a chronic inflammatory pathology, with phases of
remission and exacerbation which are impacted by nutritional,
environmental and psycho-emotional factors.
This study assessed the QoL of patients with AD.
This can be assessed by parameters such as itching, disturbance of
sleep, disturbance of play activity, and community activities. QoL
of patients with AD was assessed by evaluating the QoL indices for
infants and young children (IDQoL-Infants' Dermatitis Quality of
Life Index) and the QoL for children over 4 years (CDQoL-Children's
Dermatology Life Quality Index). The severity of the disease was
also monitored by evaluating the SCORAD index (6).
Patients and methods
Participants
The study is an observational analytical study
performed in the 2nd Pediatrics Clinic Department, Cluj-Napoca,
Romania between January 2018 and June 2019. In total, 64 patients
aged 0 to 16 years were included in the study. The inclusion
criteria were the following: Age 3 months to 16 years and the
presence of skin lesions typical for AD at the beginning of the
study. The major diagnostic criteria is itching. The minor criteria
include the following: History of flexural lesions (elbow,
popliteal fossa, perimaleolar region, laterocervical region);
personal history of asthma or rhinitis (or history of atopic
disease in first-degree relatives in children <4 years); history
of xerotic skin in the previous year, onset of symptoms under 2
years of age (this criterion is not valid in children <4 years);
lesions that affect the flexural areas and for children <4 years
old-lesions on the forehead and cheeks. For AD diagnosis, the
patient must present the major criteria and 3 or more minor
criteria. The exclusion criteria in the study were the following:
Acute infectious diseases, autoimmune diseases, skin manifestations
of other diseases, lack of informed consent.
The main group was divided into 3 smaller groups
according to age: 3 months to 4, 5-9, and 10-16 years. We used the
existent questionnaires, that include 10 questions adapted to age,
and language concerning the QoL. The parents answered the
questionnaire for the 3 months to 4 years age group. We evaluated
the pruritus, sleep disorders, sleep duration, mood, play
intervals, family activities, nutrition, treatment, bathing
program, and dressing. In the 5-9 years and 10-16 years age groups,
the questions referred to itching, activity, dressing, friends,
leisure, sports such as swimming, school activities, sleep,
bullying behavior and treatment. In these age groups, the
questionnaires were completed by children and parents.
The study was approved by the Ethics Committee of
‘Iuliu Hatieganu’ University of Medicine and Pharmacy (Cluj-Napoca,
Romania), and written informed consent was obtained from the
parents or legal guardians of the children.
Clinical evaluation
Each question for evaluating the QoL was scored from
0 to 3. 0, indicates lack of manifestations, 1, mild
manifestations, 2, moderate manifestations, and 3, severe
manifestations. The maximum score obtained in the questionnaire is
30 points. The patients were evaluated concerning the severity of
AD using the SCORAD index. The objective SCORAD index evaluates the
presence and severity of the lesions (erythema, edema, crusts,
scoria, lesions of lichenification, skin xerosis) as well as the
assessment of the pruritus intensity and sleep disorders on a scale
from 1 to 10. Depending on the score obtained, AD is classified
into severity forms: <15 mild form, 15-40 moderate form and
>40 severe form.
Statistical analysis
Continuous variables were expressed by standard
deviation and categorical variables by frequency and percentage.
For assessing differences between the variables, the Student test
and the Kruskal-Wallis test were used. The correlation between
IDQoL and CDLQI scores and AD severity (SCORAD index) was evaluated
using Pearson correlation coefficients. Multiple linear regression
analysis was used to determine the age link of the IDQoL and CDLQI
scores. The dependent variables were the IDQoL and CDLQI scores.
The independent variables in all models were age, sex, presence of
atopic disease, family history of atopy, and severity of the
disease. P<0.05 was considered as statistically significant. All
statistical analyzes were performed with Statistical Package for
the Social Sciences (SPSS), version 20.0 for Windows.
Results
Study group characteristics
The study included 64 patients aged from 0 to 16
years. The evaluated parameters of the patients included in the
study according to age are shown in Table I. The cases were divided into 3
different age groups: 0-4 years (with a mean age of 1.94 years),
5-9 years (with a mean age of 7.08 years) and 10-16 years (with a
mean age of 13.12 years). In the 3 months to 4 years group the
predominant gender was male, representing 60.9%, and the females
were 39.1%. In the further two age groups, the ratio of female to
male patients was 50/50%. The 3 age groups did not differ
significantly according to gender. Analyzing the associations with
other diseases, we found statistically significant differences,
regarding the presence of the associated atopic diseases and the
severity of AD. The association of concomitant allergic diseases
was more common in children from groups 5-9 and 10-16 years, than
in the youngest group. The severity score, estimated with the help
of the SCORAD index, was higher in the age groups 5-9 and 10-16
years. The most widespread form, according to severity was the mild
form (54.7%), followed by the moderate form (35.9%) and the severe
form (9.4%). The severe form was found with predilection in
patients over 5 years of age.
 | Table ICharacteristics of the study group by
age. |
Table I
Characteristics of the study group by
age.
| Variables | All ages | 0-4 years | 5-9 years | 10-16 years | P-value |
|---|
| No. of patients | 64 | 44 (68.7%) | 12 (18.8%) | 8 (12.5%) | |
| Age (mean ± SD) | 7.38±4.18 | 1.94±0.96 | 7.08±1.38 | 13.12±1.32 | |
| Sex | | | | | 0.184 |
|
Male | 39 (60.9%) | 29 (65.9%) | 6 (50%) | 4 (50%) | |
|
Female | 25 (39.1%) | 15 (34.1%) | 6 (50%) | 4 (50%) | |
| Atopy | | | | | <0.001 |
|
Only Atopic
Dermatitis | 28 (43.8%) | 29 (65.9%) | 4 (33.3%) | 3 (37.5%) | |
|
Atopic
disease associated | 36 (56.2%) | 15 (34.1%) | 8 (66.7%) | 5 (62.5%) | |
| SCORAD index | | | | | 0.002 |
|
Mild | 35 (54.7%) | 35 (79.5%) | 0 | 0 | |
|
Moderate | 23 (35.9%) | 8 (18.2%) | 10 (83.3%) | 5 (62.5%) | |
|
Severe | 6 (9.4%) | 1 (2.3%) | 2 (16.7%) | 3 (37.5%) | |
| SCORAD index (mean
value) | 21.4±10.4 | 16.4±10.9 | 21.4±9.8 | 20.9±10.6 | |
QoL assessment
In order to assess the QoL, several parameters were
analyzed, both at younger and older ages, illustrated in Table II. The highest IDQOL scores were
found in pruritus, child's disposition, and treatment problems. The
lowest scores were related to sleep disturbance and the time needed
to fall asleep. In older children, the QoL assessed by CDLQI, in
both age groups, the highest scores were related to problems during
school, holidays and pruritus. The lowest scores for these age
groups were obtained on questions related to sleep and treatment.
The significant difference between the 2 groups, respectively 5-9
and 10-16 years, was obtained concerning the swimming questions. At
this question, the highest QoL deficiency was obtained in children
aged 5-9 years. Other significant elements between the 2 groups
would be questions about teasing, intimidation, sleep problems and
hobbies. These questions had higher values in children aged 5-9
years compared with those in the group of 10-16 years.
 | Table IIQuality of life of patients with
atopic dermatitis by age. |
Table II
Quality of life of patients with
atopic dermatitis by age.
| IDQOL | CDLQI |
|---|
| Parameter | 0-4 years Mean ±
SD | Parameter | 5-9 years Mean ±
SD | 10-16 years Mean ±
SD | P-value |
|---|
| Itch | 1.39±0.82 | Itch | 2.19±0.62 | 1.43±0.69 | <0.015 |
| Mood change | 1.85±0.79 | Embarrassing
situations | 1.78±1.03 | 1.51±1.15 | 0.261 |
| Sleep duration | 1.30±0.85 | Friends | 2.03±0.85 | 1.85±0.82 | 0.258 |
| Sleeping
disturbance | 1.10±0.81 | Clothes/Shoes | 1.76±0.79 | 1.51±0.94 | 0.123 |
| Play | 1.40±0.80 | Free
time/hobbies | 2.20±0.75 | 1.83±0.85 | 0.034 |
| Family
activities | 1.45±0.88 | Swimming/sport | 2.10±0.82 | 1.45±1.09 | <0.001 |
| Food | 1.42±0.81 | Șchool/holiday | 2.40±0.65 | 2.20±0.62 | 0.109 |
| Treatment | 1.69±0.86 |
Teasing/intimidation | 1.91±0.73 | 1.64±0.83 | 0.021 |
| Bandage | 1.35±0.85 | Sleep | 1.45±0.65 | 1.16±0.85 | 0.027 |
| Bathroom
schedule | 1.41±0.89 | Treatment | 1.48±0.74 | 1.23±0.74 | 0.187 |
Correlations
The correlation between IDQOL, CDLQI, and the
severity of AD, according to the SCORAD index, are presented in
Table III. The most significant
correlation between the parameters and the severity levels
according to SCORAD was identified in the age group 5-9 years, as
seen in Fig. 1. The most
significant correlation was observed between the CDLQI and SCORAD
scores in the 5-9 years age group (0.89) and moderate correlation
in the other 2 age groups (0-4, 0.59 and 10-16 years, 0.43). There
was also a moderate correlation between the CDLQI score and the
SCORAD index, for the entire age range of 5-16 years.
 | Table IIICorrelation between quality of life
(IDQOL/CDLQI) and severity of atopic dermatitis (SCORAD), according
to age groups. |
Table III
Correlation between quality of life
(IDQOL/CDLQI) and severity of atopic dermatitis (SCORAD), according
to age groups.
| Age groups | 0-4 years | 5-9 years | 10-16 years | 5-16 years | All ages |
|---|
| Pearson’s correlation
coefficient | 0.59 | 0.89 | 0.43 | 0.52 | 0.57 |
Discussion
QoL represents the main goal for patients, parents,
and physicians. The purpose of therapy is to augment the patients'
QoL, thus offering the ability to normalize social interactions and
activities for the patient. It is known that ‘invisible diseases’
are easier to bear psychologically than those that have an
aesthetic impact (7). Most often,
the psychological implications have an impact on the evolution of
the disease, treatment, and can ultimately lead to social isolation
and school dropout. It is precisely for this reason that diseases,
such as atopic dermatitis, should be addressed, considering all the
aspects that can cause an unfavorable evolution (8). Fortunately, in children, mild and
moderate forms of the disease are the most frequent, but severe
forms have a significant impact on the social integration of
children. For the correct approach of patients with severe forms,
teams of pediatric allergologists, dermatologists, psychiatrists
and psychologists are needed (9-11).
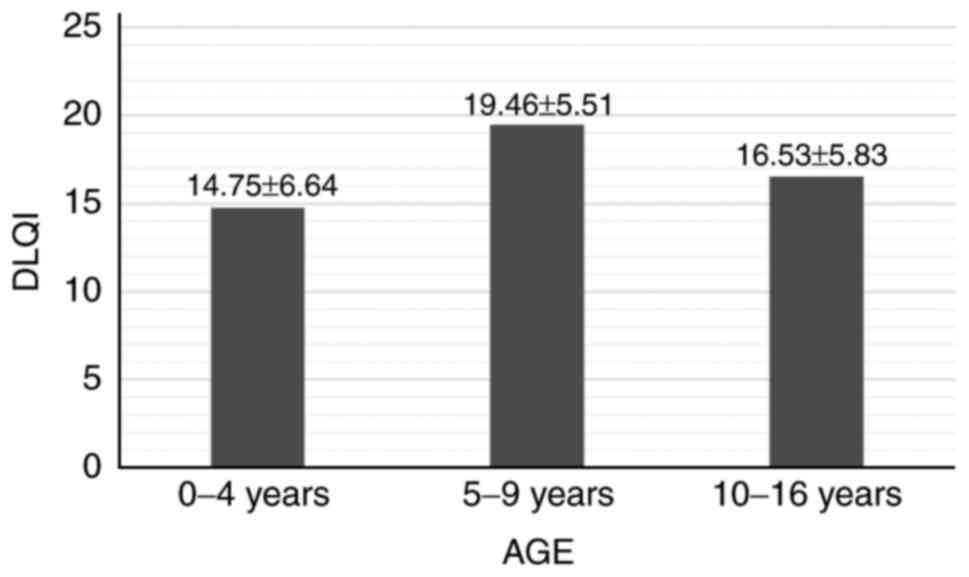
Our study of AD QoL evaluation in pediatric patients
is, to our knowledge, the first study of this kind undertaken in
Romania. Analyzing comparatively the QoL by age groups, we found
that the most affected was the group of 5-9 years (mean score was
19.46±5.5), followed closely by the group aged 10-16 years (mean
score was 16.53±5.83). In the age group of 0-4 years, the mean
score was 14.75±6.64. The study analyzed the correlations between
IDQOL and CDLQI and the severity of atopic dermatitis evaluated by
calculating the SCORAD index. The most significant correlation was
observed in the group of 5-9 years, whose Pearson correlation
coefficient was 0.89. In the other two age groups, moderate
correlations, respectively, at 0-4 years of 0.59, and at 10-16
years of 0.43 were found. A moderate correlation was also found
between CDLQI and the SCORAD index in the age group 5-16 years,
with a correlation coefficient of 0.57.
Previous studies that analyzed a possible
correlation between the age of the child and the QoL of the patient
with AD were found in literature. The study of Campos et al
(12) showed that the average CDLQI
score was higher for younger children compared with older children.
An international study by Chernyshov et al (13) revealed a significant correlation of
CDLQI with children's age.
Not all parameters of QoL analyzed have similar
effects on the patient's activity. In the young age groups, the
most common symptoms were itching, child's disposition, and
treatment. In older age groups, most problems were related to
school attendance, vacations, itching, leisure, and hobbies.
Itching, defined as an unpleasant sensation that
causes the desire to scratch, is a significant symptom of atopic
dermatitis and other atopic diseases. Pruritus is the major
diagnostic criterion in AD, and can severely affect the QoL of
these patients. Itching had the highest score in all age groups and
negatively impacted the QoL. The frequent need for scratching and
grating of the lesions leads to nocturnal awakening, fatigue, and
irritability (14-16).
Studies in other centers show that sleep can be
disturbed in over 60% of cases, and during exacerbations in over
80%. Our study confirmed these results. It is found that patients
can lose about 2 h of sleep per night due to wakefulness caused by
itching (16,17). In our study, the QoL due to sleep
disorders affected up to 50% of patients. The consequences of sleep
deprivation are significant and may include mood swings, fatigue,
and lack of concentration. These manifestations will ultimately
affect school performance and social activities. The issue of sport
had a greater impact on the age group 5-9 years in the studied
group. School isolation, teasing, and intimidation led to the onset
of depression, generating school absenteeism and social separation
(18-21).
In conclusion, the present study showed significant
correlation between the QoL and the manifestations of the severity
of atopic dermatitis. These results encourage the creation of
integrative therapy guidelines, aimed at improvement of clinical
symptoms and QoL alike.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MS, LS and RFI were responsible for the acquisition
and analysis of the data regarding the disease and the
questionnaire parameters. EF, AT and ANB contributed to the
conception and design of the study, and revised the manuscript
critically for important intellectual content. MS, ANB and RFI
contributed to the writing of the manuscript. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
‘Iuliu Hatieganu’ University of Medicine and Pharmacy (Cluj-Napoca,
Romania), and written informed consent was obtained from the
parents or legal guardians of the children.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Solomon I, Ilie M, Draghici C, Voiculescu
VM, Căruntu C, Boda D and Zurac S: The impact of lifestyle factors
on evolution of atopic dermatitis: An alternative approach
(Review). Exp Ther Med 1078-1084, 2018.
|
|
2
|
Olsen JR, Gallacher J, Finlay AY, Piguet V
and Francis NA: Quality of life impact of childhood skin conditions
measured using the Children's Dermatology Life Quality Index
(CDLQI): A meta-analysis. Br J Dermatol. 174:853–861.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kage P, Simon J and Treudler R: Atopic
dermatitis and psychosocial comorbidities. J Dtsch Dermatol Ges.
18:93–102. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Olsson M, Bajpai R, Yew YW, Koh MJA, Thng
S, Car J and Järbrink K: Associations between health-related
quality of life and health care costs among children with atopic
dermatitis and their caregivers: A cross-sectional study. Pediatr
Dermatol. 37:284–293. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Holm J, Agner T, Clausen ML and Thomsen S:
Quality of life and disease severity in patients with atopic
dermatitis. J Eur Acad Dermatol Venereol. 30:1760–1767.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ražnatović Đurović M, Janković J, Tomić
Spirić V, Relić M, Sojević Timotijević Z, Ćirković A, Đurić S and
Janković S: Does age influence the quality of life in children with
atopic dermatitis? PLoS One. 14(e0224618)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Xerfan EMS, Tomimori J, Andersen ML, Tufik
S and Facina AS: Sleep disturbance and atopic dermatitis: A
bidirectional relationship? Med Hypotheses.
140(109637)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Chernyshov PV: Stigmatization and
self-perception in children with atopic dermatitis. Clin Cosmet
Investig Dermatol. 9:159–166. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Xu X, van Galen LS, Koh MJA, Bajpai R,
Thng S, Yew YW, Ho VPY, Alagappan U, Järbrink KSA and Car J:
Factors influencing quality of life in children with atopic
dermatitis and their caregivers: A cross-sectional study. Sci Rep.
9(15990)2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gabes M, Chamlin SL, Lai J, Cella D,
Mancini AJ and Apfelbacher CJ: Development of a validated
short-form of the Childhood Atopic Dermatitis Impact Scale, the
CADIS-SF15. J Eur Acad Dermatol Venereol: Mar 16, 2020 doi:
10.1111/jdv.16362. (Online ahead of print).
|
|
11
|
Gerbens LAA, Prinsen CAC, Chalmers JR,
Drucker AM, von Kobyletzki LB, Limpens J, Nankervis H, Svensson Å,
Terwee CB, Zhang J, et al: Evaluation of the measurement properties
of symptom measurement instruments for atopic eczema: A systematic
review. Allergy Eur J Allergy Clin Immunol. 72:146–163.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Campos ALB, Araújo FM, Santos MALD, Santos
AASD and Pires CAA: Impact of atopic dermatitis on the quality of
life of pediatric patients and their guardians. Rev Paul Pediatr.
35:5–10. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chernyshov PV, Ho RC, Monti F, Jirakova A,
Velitchko SS, Hercogova J and Neri E: Gender differences in
self-assessed health-related quality of life in children with
atopic dermatitis. J Clin Aesthet Dermatol. 9:19–24.
2016.PubMed/NCBI
|
|
14
|
Harrison IP and Spada F: Breaking the
itch-scratch cycle: Topical options for the management of chronic
cutaneous itch in atopic dermatitis. Medicines (Basel).
6(76)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
El Hachem M, Di Mauro G, Rotunno R,
Giancristoforo S, De Ranieri C, Carlevaris CM, Verga MC and Dello
Iacono I: Pruritus in pediatric patients with atopic dermatitis: A
multidisciplinary approach - summary document from an Italian
expert group. Ital J Pediatr. 46(11)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yang EJ, Beck KM, Sekhon S, Bhutani T and
Koo J: The impact of pediatric atopic dermatitis on families: A
review. Pediatr Dermatol. 36:66–71. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ramirez FD, Chen S, Langan SM, Prather AA,
McCulloch CE, Kidd SA, Cabana MD, Chren MM and Abuabara K:
Association of atopic dermatitis with sleep quality in children.
JAMA Pediatr. 173(e190025)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Bonamonte D, Filoni A, Vestita M, Romita
P, Foti C and Angelini G: The role of the environmental risk
factors in the pathogenesis and clinical outcome of atopic
dermatitis. Biomed Res Int. 2019(2450605)2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Na CH, Chung J and Simpson EL: Quality of
life and disease impact of atopic dermatitis and psoriasis on
children and their families. Children (Basel).
6(133)2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Maksimovic N, Zaric M, Reljic V, Nikolic M
and Gazibara T: Factors associated with improvement of quality of
life among parents of children with atopic dermatitis: 1-year
prospective cohort study. J Eur Acad Dermatology Venereol.
34:325–332. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Al-Afif KAM, Buraik MA, Buddenkotte J,
Mounir M, Gerber R, Ahmed HM, Tallman AM and Steinhoff M:
Understanding the burden of atopic dermatitis in Africa and the
Middle East. Dermatol Ther (Heidelb). 9:223–241. 2019.PubMed/NCBI View Article : Google Scholar
|