Introduction
Lumbar spinal stenosis (LSS) is a common
degenerative disease that is prevalent among the elderly
population. LSS can be divided into lumbar central spinal stenosis
(LCSS), lateral recess stenosis (LRS) and foraminal stenosis; LCSS
is commonly combined with LRS (1).
The pathogenesis behind LCSS and LRS was discovered to be
responsible for compression of the dural sac and nerve roots, which
are directly caused by disc herniation (DH), hypertrophic
ligamentum flavum (LF) and hypertrophic facet joint (2,3). The
main aim of surgical treatment in LCSS and LRS is to decompress the
nerve roots and relieve the symptoms (4). As a consequence, the majority of
patients who suffer from LCSS and LRS will undergo surgery if
traditional treatment regimens fail to relieve the neurological
symptoms (5).
Traditional open surgery encompasses fenestration,
semi-laminectomy and total laminectomy; however, although these
traditional surgical methods can improve the neurological symptoms,
surgery is often associated with postoperative complications,
especially in elderly populations with comorbidities (6,7).
Compared with traditional surgical procedures, minimally invasive
spinal surgery (MISS) has been observed to minimize iatrogenic
traumatization, promote recovery and preserve the segmental
stability (8,9). Notably, following the development of
medical instruments, complicated degenerative neurological
disorders such as LSS have also been successfully treated using
MISS (6). Microendoscopic
discectomy (MED) is one of the MISS procedures that is used to
treat LSS (10-12).
At first, MED was only used to treat LCSS with unilateral recess
stenosis; however, following the development of the MED system,
bilateral over-the-top decompression under microendoscopy has also
been successfully performed using a unilateral approach, which is
now known as the unilateral laminectomy for bilateral decompression
(ULBD) technique (13).
Microendoscopic ULBD is the standard procedure for the treatment of
LCSS and LRS in the General Hospital of Central Theater Command of
PLA (Wuhan, China).
Following the advancement of the full endoscopic
system, another MISS procedure, known as percutaneous endoscopic
lumbar discectomy (PELD), has also demonstrated favorable clinical
results for the treatment of lumbar degenerative disease (8,14-16).
PELD is primarily used to treat intervertebral DH; however, certain
limitations, such as the lack of effective surgical instruments,
narrow endoscopic vision and a steep learning curve, restrict its
application for the treatment of more complicated degenerative
neurological disorders, such as LSS. Therefore, the Interlaminar
Endoscopic Surgical System (iLESSYS®) Delta system
(Joimax® GmbH) has been subsequently developed from the
traditional PELD system for the treatment of LSS. The
iLESSYS® Delta system is equipped with a larger size
working cannula and endoscopic instruments, which permits big
osteophytes or soft tissues to be removed without extra maneuvers
under good endoscopic visualization (8,16,17).
This design has made the treatment of LCSS and LRS more efficient
through using the interlaminar approach (8,16,17).
Therefore, the present study aimed to retrospectively compare the
radiographic and clinical outcomes of LCSS and LRS treated with
both the MED and iLESSYS® Delta approaches.
Materials and methods
Patient studies
Between November 2015 and November 2017, 134
patients (85 males and 49 females; range 53-82 years) underwent MED
or the iLESSYS® Delta approach in the General Hospital
of Central Theater Command of PLA (Wuhan, China). The patients were
categorized into two groups: i) The iLESSYS® Delta group
(52 patients; 34 males and 18 females; range 54-79 years) and the
MED group (82 patients; 51 males and 31 females; range 53-82
years). These surgical procedures were performed by one experienced
surgeon. All the procedures in the present study were approved by
the Ethics Committee of the General Hospital of Central Theater
Command of PLA (Wuhan, China), and were in accordance with the
Helsinki Declaration. Written informed consent was obtained from
each patient. The following inclusion criteria were used to select
the patients: i) Patients with symptoms of neurogenic claudication
and/or radicular leg pain; ii) single-level degenerative LCSS and
LRS, which were diagnosed using CT scanning and MRI with the
Schizas Grading System applied (18); iii) neurological symptoms which were
consistent with the CT scans and MRI findings; iv) no dynamic
spinal instability observed; and v) patients who had received
traditional therapeutic regimens for a period of at least 6 weeks.
The following exclusion criteria were applied: i) Dynamic spinal
instability; ii) degenerative spondylolisthesis of a Meyerding
grade >I (15,19); iii) combined foraminal stenosis at
the same or a lower level; iv) patients with severe cardiopulmonary
diseases who were unable to tolerate surgery; and v) prior surgery
at the same segment. In the present study, all patients were
informed objectively about the surgical procedure, benefits and
potential risks, and each patient was able to freely elect for the
surgical option.
Clinical assessment
The medical data from all included patients were
collected and assessed for basic demographic, perioperative and
postoperative data. Each patient was evaluated using the visual
analogue scale (VAS) for back pain and leg pain; and the Oswestry
disability index (ODI) questionnaires (20). Both questionnaires were asked
preoperatively and at each follow-up time point (1-week, 6-months
and the latest follow-up). The VAS and ODI scores were recorded in
the questionnaires at each follow-up in the outpatient department.
Postoperative Modified Macnab criteria was also used for the
clinical global outcome assessment (21). Occasionally, follow-ups were
obtained by telephone communication.
MRI was also performed to determine the extent of
the spinal canal decompression. The cross-sectional area of the
dural sac (CSAD) was analyzed using ImageJ software (1.50; National
Institutes of Health) and the preoperative and postoperative MRIs
were compared to evaluate the efficiency and safety of the
decompression between the two groups.
Surgical approaches
MED
All patients underwent surgery in the prone position
under general anesthesia. The intervertebral disc space at the
stenosis level was located using C-arm fluoroscopy. Briefly, a
1.5-2 cm vertical incision was made beside the spinous process on
the dominant symptomatic side. The fascia and subcutaneous tissue
were dissected, and hemostasis was achieved by bipolar coagulation.
Subsequently, the sequential dilators were inserted to expose the
desired upper lamina. A tubular retractor was passed over the
dilator, which was then removed and the flexible arm was attached
to the tubular retractor firmly. The endoscope was subsequently
inserted into the tubular retractor and connected to it. Following
the identification of the inferior border of the upper lamina,
ipsilateral semi-laminectomy was performed. The base of the spinous
process was undercut using a high-speed drill, known as the
‘over-the-top’ technique (22). The
LF located at the dorsal side of the dural sac was resected using a
Kerisson punch (Medtronic Sofamor Danek, Memphis, TN) to initiate
the decompression of the central stenosis. The tubular retractor
was then tilted to expose the contralateral recess. Finally, the
contralateral recess decompression was performed until the
contralateral nerve roots were decompressed.
iLESSYS
® Delta approach. All procedures
were performed using the iLESSYS® Delta system
(Joimax® GmbH). Each patient underwent surgery in the
prone position under general anesthesia. Briefly, under the
guidance of C-arm fluoroscopy, the interlaminar space at the
desired level was identified by inserting a guide needle near the
spinous process on the dominant symptomatic side. A skin incision
(1-1.5 cm) was made at the entry site of the needle and the guide
wire was introduced through the needle, which was subsequently
withdrawn. Subsequently, sequential dilators were introduced
through the surface of the inferior margin of the upper lamina over
the guide wire and the tubular retractors for the endoscope were
placed over the dilators. The guide wire and the dilators were then
removed. An endoscope system was assembled using two irrigation
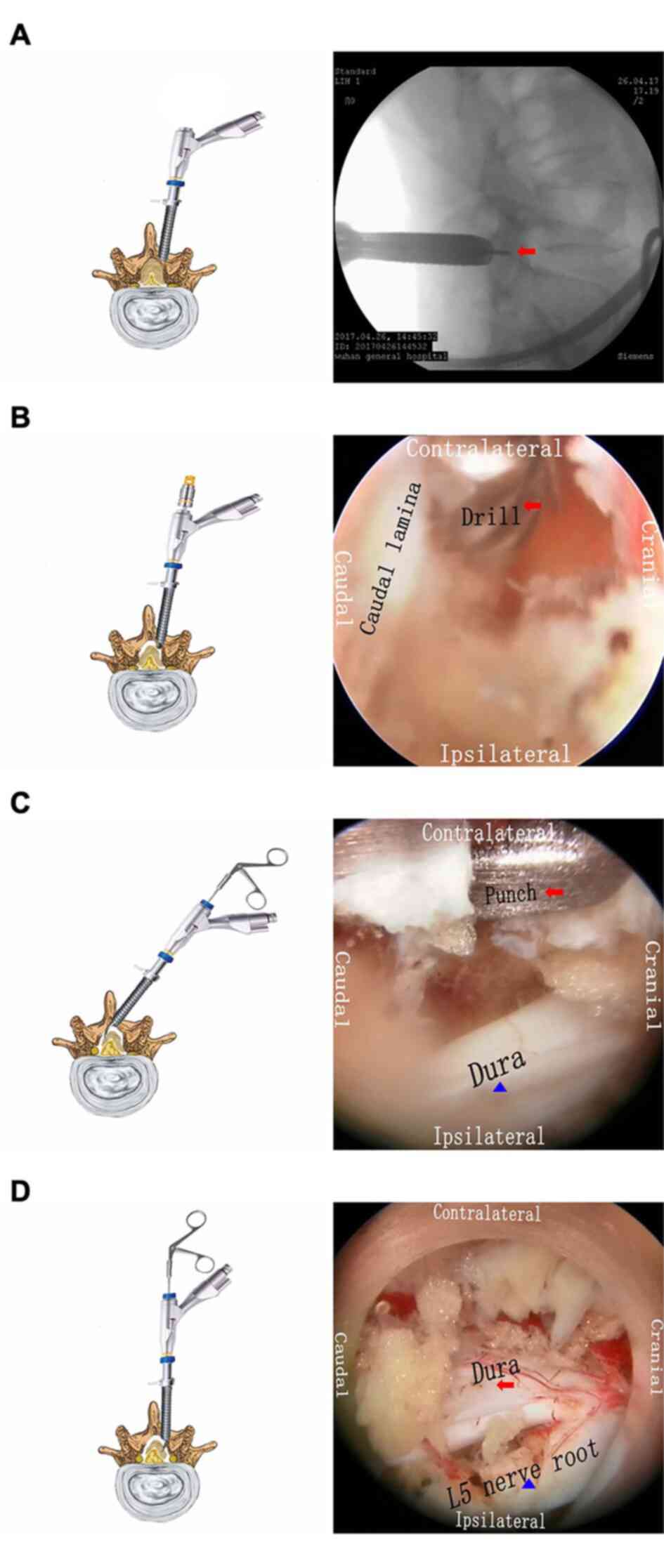
channels and an eccentrically placed 6-mm working cannula (Fig. 1A). The upper and lower lamina were
located, and the soft tissue was removed using bipolar
radiofrequency and grasper forceps. In addition, the cranial and
caudal lamina, as well as the partial facet joint were removed
using a high-speed drill (Fig. 1B).
The LF located at the dorsal side of the dural sac was resected
using a Kerrison punch (Joimax® GmbH) to decompress the
central stenosis. The contralateral decompression was performed by
tilting the working cannula and endoscope, and the base of spinous
process was undercut. Subsequently, the ventral portion of the
upper articular process and the LF were removed to promote the
decompression of the contralateral LRS (Fig. 1C). The working cannula and endoscope
were then moved away for the ipsilateral lateral recess
decompression (Fig. 1D). Finally,
the decompression was determined by assessing the retained mobility
of the dural sac and nerve roots.
Statistical analysis
Statistical analysis was performed using SPSS
version 17.0 software (SPSS, Inc.). Significant differences between
the mean age, duration of symptoms, follow-up, incision length,
duration of surgery and time to return to work were determined
using unpaired Student's t-tests. Significant differences between
sex, diabetes status, lower extremity atherosclerosis, operative
level, Schizas grade and MacNab evaluation were analyzed using
χ2 tests. The CSAD was verified using Student's t-tests
before and after the operation between the two treatments. VAS and
ODI were compared using Mann Whitney U tests and post-hoc
Bonferroni adjustments. Measurement data are expressed as mean ±
standard deviation, and enumeration data was shown by rate (%).
P<0.05 (or P<0.0125 with Bonferroni adjustments) was
considered to indicate a statistically significant difference.
Results
Comparison of basic demographic
characteristics
A total of 134 participants (iLESSYS®
Delta, 52 cases; MED, 82 cases) who met the inclusion criteria were
enrolled in the present study. The basic demographic
characteristics (age, sex, comorbidities, duration of symptoms,
operative level, Schizas grade and follow-up) were compared and
presented in Table I. There were no
significant differences observed regarding the basic demographic
characteristics between the two groups.
 | Table IComparison of demographic
characteristics in the two groups. |
Table I
Comparison of demographic
characteristics in the two groups.
|
Characteristics | iLESSYS Delta
(n=52) | MED (n=82) |
t/χ2-value | P-value |
|---|
| Age, years | 67.35±7.20 | 65.72±6.36 | 1.37a | 0.17 |
| Gender, male
(%) | 34 (65.38) | 51 (62.20) | 0.14b | 0.71 |
| Diabetes (%) | 6 (11.54) | 9 (10.98) | 0.01b | 0.92 |
| Lower extremity
atherosclerosis disease (%) | 5 (9.62) | 10 (12.20) | 0.21b | 0.64 |
| Duration of
symptoms, months | 10.92±2.96 | 11.89±4.08 | 1.48a | 0.14 |
| Operative level,
L4/5/(L4/5+L5/S1) (%) | 35 (67.31) | 61 (74.39) | 0.79b | 0.38 |
| Schizas grade,
Schizas grade C/(Schizas | 17 (32.69) | 23 (28.05) | 0.33b | 0.57 |
| grade C + Schizas
grade D) (%) Follow-up, months | 20.54±5.49 | 21.22±5.09 | 0.73a | 0.47 |
Comparison of surgery-related
indicators between the two groups
The incision length (1.41±0.17 cm) in the
iLESSYS® Delta group was significantly shorter compared
with the MED group (1.89±0.26 cm). However, the duration of the
surgery in the iLESSYS® Delta group (83.81±11.07 min)
was significantly longer compared with the MED group (58.32±12.30
min). There was no significant difference reported in the time to
return to work between the iLESSYS® Delta group
(10.71±2.17 days) and the MED group (11.44±2.69 days) (Table II).
 | Table IIComparison of clinical operation
effects between the two groups. |
Table II
Comparison of clinical operation
effects between the two groups.
| Items | iLESSYS Delta
(n=52) | MED (n=82) | t-value | P-value |
|---|
| Incision length,
cm | 1.41±0.17 | 1.89±0.26 | 11.97 | <0.05 |
| Duration of
surgery, min | 83.81±11.07 | 58.32±12.30 | 12.15 | <0.05 |
| Time to return to
work, days | 10.71±2.17 | 11.44±2.69 | 1.64 | 0.10 |
Comparison of clinical and functional
outcomes
The average VAS score of back/leg pain following the
operation improved in both the MED group and the
iLESSYS® Delta group was analyzed. The average VAS score
of the leg pain was reduced from 7.95±0.99 to 1.71±0.74 in the MED
group and from 7.71±0.91 to 1.62±0.74 in the iLESSYS®
Delta group. The average VAS score of the back pain was reduced
from 4.93±1.04 to 1.52±0.76 in the MED group and from 5.13±1.03 to
1.58±0.70 in the iLESSYS® Delta group. In addition, the
average ODI scores following the operations were also improved; the
average ODI score were reduced from 76.90±9.43 to 28.15±6.59 in the
MED group and from 74.62±9.12 to 26.71±6.45 in the
iLESSYS® Delta group (Table III).
 | Table IIIComparison of VAS and ODI scores in
the two groups. |
Table III
Comparison of VAS and ODI scores in
the two groups.
| Items | iLESSYS Delta
(n=52) | MED (n=82) | P-value |
|---|
| VAS of Leg |
|
Pre-operation | 7.71±0.91 | 7.95±0.99 | 0.15 |
|
1-week after
operation | 2.10±0.10 | 2.17±0.68 | 0.48 |
|
6-month
after operation | 1.81±0.84 | 1.85±0.83 | 0.77 |
|
The latest
follow-up | 1.62±0.74 | 1.71±0.74 | 0.37 |
| VAS of Back |
|
Pre-operation | 5.13±1.03 | 4.93±1.04 | 0.34 |
|
1-week after
operation | 2.12±0.55 | 2.45±0.52 | <0.0125 |
|
6-month
after operation | 1.83±0.71 | 1.90±0.73 | 0.46 |
|
The latest
follow-up | 1.58±0.70 | 1.52±0.76 | 0.51 |
| ODI |
|
Pre-operation | 74.62±9.12 | 76.90±9.43 | 0.09 |
|
1-week after
operation | 32.15±8.38 | 35.46±9.26 | <0.0125 |
|
6-month
after operation | 27.08±7.15 | 27.95±6.47 | 0.16 |
|
The latest
follow-up | 26.71±6.45 | 28.15±6.59 | 0.98 |
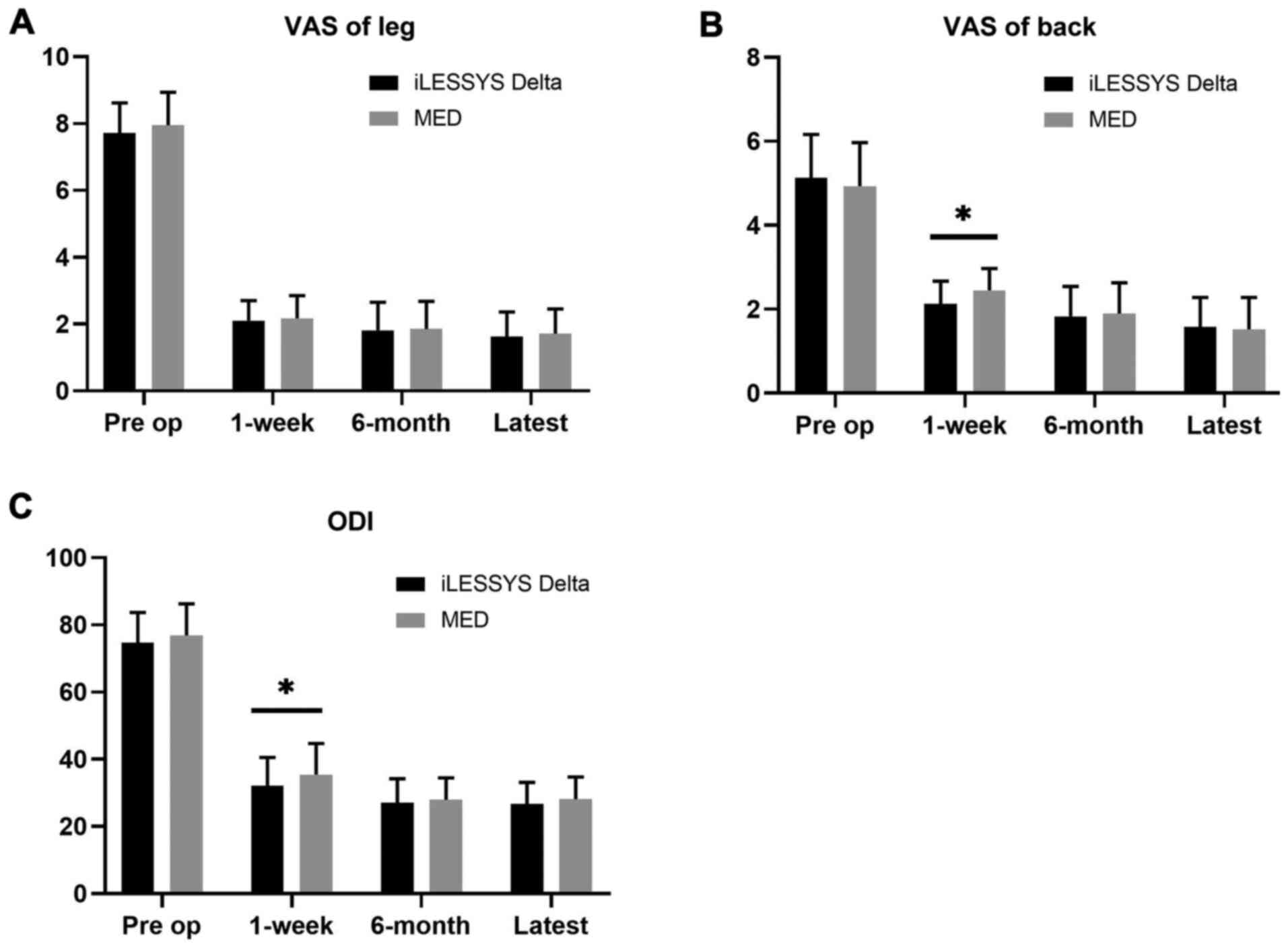
There was also no significant difference found
between the two groups for the average VAS score of the leg pain at
any time point (Fig. 2A). Notably,
the average VAS score of the back pain in the iLESSYS®
Delta group was significantly lower compared with the MED group at
the 1-week follow-up; however, there was no significant difference
between the two groups at both the 6-month and the latest follow-up
(Fig. 2B). Similarly, the ODI score
in the iLESSYS® Delta group was significantly lower
compared with the MED group at the 1-week follow-up; however, there
was no significant difference between the two groups at the 6-month
and the latest follow-up (Fig.
2C).
Following the application of the modified MacNab
criteria, a good-to-excellent evaluation was found in 89.0% of the
patients in the MED group, whereas a good-to-excellent rate of
90.4% was found in the iLESSYS® Delta group. There was
no significant difference observed between the good-to-excellent
rates between the two groups (Table
IV).
 | Table IVComparison of MacNab evaluation in
the two groups. |
Table IV
Comparison of MacNab evaluation in
the two groups.
| Groups | n | Excellent | Good | Fair | Poor |
|---|
| iLESSYS Delta | 52 | 29 (55.77) | 18 (34.62) | 3 (5.77) | 2 (3.85) |
| MED | 82 | 37 (45.12) | 36 (43.90) | 6 (7.32) | 3 (3.66) |
| χ² | 1.53 | | | | |
| P-value | 0.68 | | | | |
Comparison of the CSAD
There were no significant differences reported in
the preoperative CSAD between the two groups. In addition, there
were no significant differences observed in the postoperative area
and reduced CSAD between the two groups (Table V).
 | Table VResults of clinical images study. |
Table V
Results of clinical images study.
| Outcome
(mm2) | iLESSYS Delta
(n=52) | MED (n=82) | t-value | P-value |
|---|
| Pre-operation
area | 55.14±5.27 | 53.98±5.58 | 1.19 | 0.23 |
| Post-operation
area | 168.96±7.60 | 170.13±7.23 | 0.89 | 0.37 |
| Reduced area | 113.82±7.37 | 116.15±8.31 | 1.65 | 0.10 |
Comparison of complications and
recurrence
Complications occurred in three patients (3.66%) in
the MED group and two patients (3.85%) in the iLESSYS®
Delta group. One patient in the MED group experienced transient
urinary retention following the operation, which resolved itself
with bed rest within 2 days postoperatively. In addition, two
patients in the MED group had the procedure converted to open
surgery due to a dural tear. One patient in the iLESSYS®
Delta group experienced a small sized dural tear (<5 mm) and
complained of a headache following the operation, which improved
following bed rest and Etoricoxib tablets (60 mg, 1/day; orally).
One patient in the iLESSYS® Delta group also complained
of postoperative dysesthesia, with these symptoms being reversed
following a combination of physical treatment and Mecobalamin
Tablets (500 ug, 3/day; orally). No patient in either group
presented with complications such as neurological injury,
spondylodiscitis, surgical wound infection or cauda equina
syndrome. Altogether, there was no significant difference
discovered in the complication rates between the two groups.
One patient in the iLESSYS® Delta group
and two patients in the MED group who suffered with neurogenic
claudication and/or radicular leg pain prior to the surgery,
suffered from the same symptoms following the operation. The
patients with recurrent neurogenic claudication and/or radicular
leg pain were subjected to transforaminal posterior lumbar
interbody fusion upon the failure of traditional management
regimens. Notably, the symptoms of these patients were successfully
alleviated up to the final follow-up. There were no significant
differences found in the recurrence rates between the two
groups.
Representative cases
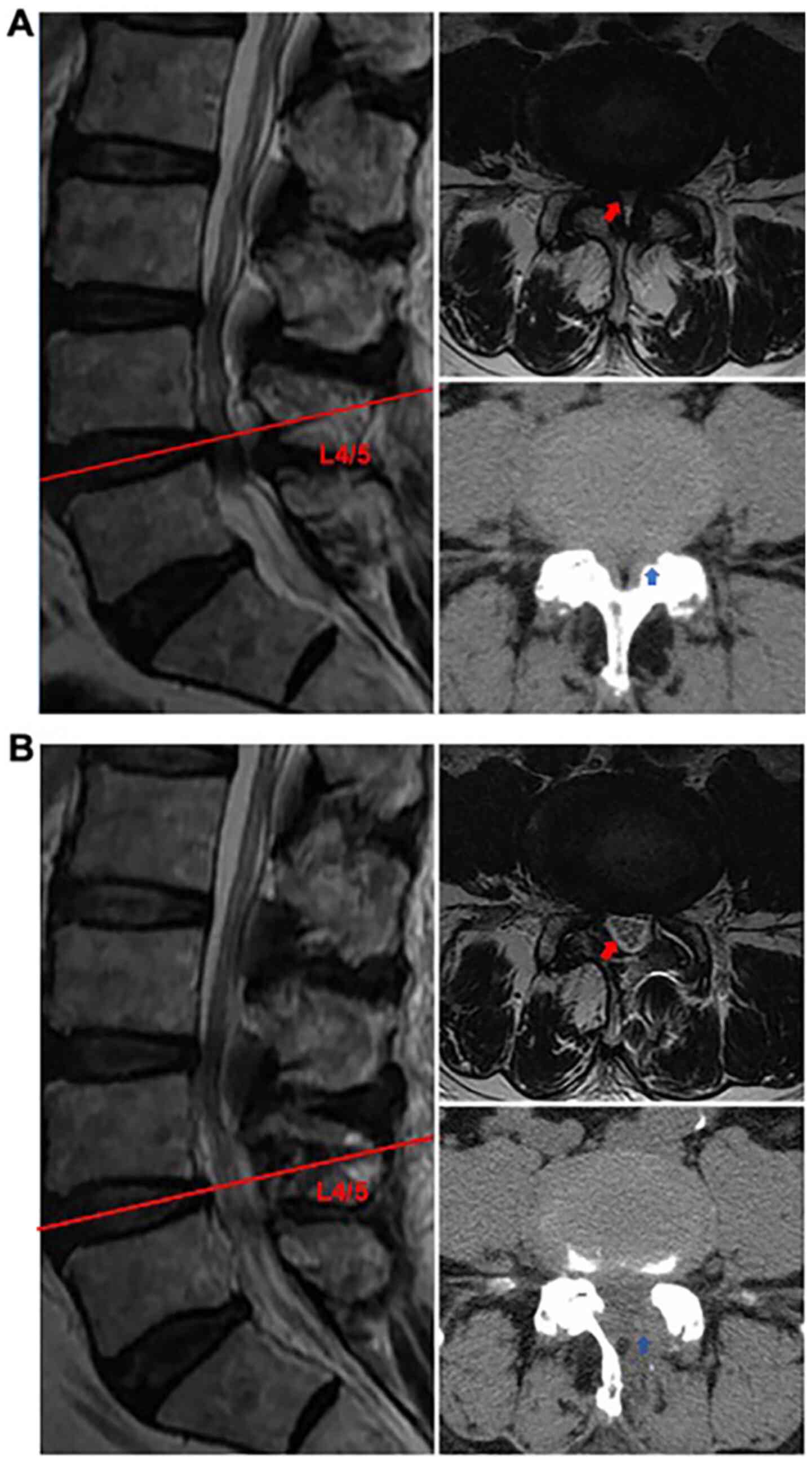
Representative cases who underwent an operation
using the iLESSYS® Delta system are presented. Pre- and
Post-operative CT and MRI scans (LCSS and LRS at L4/5) were
presented in Fig. 3.
Discussion
The present study aimed to retrospectively compare
MED and the iLESSYS® Delta system for the treatment of
LCSS and LRS. In the General Hospital of Central Theater Command of
PLA (Wuhan, China), MED is regarded as a standard minimally
invasive treatment option and routinely applied to treat LCSS and
LRS. The iLESSYS® Delta system is a newly developed
endoscopic technique used to treat LCSS and LRS; however, to the
best of our knowledge, no previous studies have compared this
technique with MED. Therefore, MED was used as a reference to
evaluate the efficiency and safety of the iLESSYS® Delta
system. The present study aimed to determine the demographic
characteristics, operation-related indicators, functional recovery,
radiographic changes, the complications, recurrence, efficiency and
safety of both MED and the iLESSYS® Delta system. The
preliminary results demonstrated that the iLESSYS® Delta
approach may have the potential to treat LCSS and LRS with
favorable clinical outcomes compared with MED.
The PELD technique was originally designed to
perform disc discectomy (23,24).
Compared with traditional open surgery, favorable clinical results
were achieved using this technique to treat DH (25,26).
Following the improvement of the PELD technique, the technique has
since been expanded from solely treating DH to being used to treat
LSS (27). The decompression of the
LSS can be performed using either a transforaminal or interlaminar
approach. The transforaminal approach is mainly used for the
decompression of the LRS and foraminal stenosis, whereas the
interlaminar approach is suitable for the decompression of the LCSS
and LRS. However, several limitations, such as ineffective surgical
instruments and narrow endoscopic vision, have prevented the
application of PELD for the treatment of LCSS and LRS. As
aforementioned, the iLESSYS® Delta system was
subsequently developed from the traditional PELD procedure. The
iLESSYS® Delta set contains specially designed
instruments to enable a comprehensive decompression of the spinal
canal and the size of the working cannula and endoscopic
instruments are larger compared with those used in the traditional
endoscope system (8,16,17).
The 10-mm outer diameter endoscope and 6-mm working cannula used in
the iLESSYS® Delta system have been found to provide a
broader endoscopic field of view, permitting the use of a larger
burr for the resection of osteophytes and more powerful grasper
forceps to remove the residual fragments (17). By taking advantage of these
advantages, ULBD can be performed under endoscopy using the
iLESSYS® Delta system to treat LCSS and LRS.
The surgical principle of the iLESSYS®
Delta system is similar to the MED; however, there are still
several differences between the two approaches, which have been
summarized in Table VI. Firstly,
unlike MED, the iLESSYS® Delta approach is performed
under continuous saline irrigation, which offers certain advantages
(16,28); for example, it has been suggested
that the release of inflammatory cytokines may be attenuated by the
saline irrigation and that the pressure of the saline solution may
reduce the bleeding, ensuring that the surgical field remains
clean. In addition, it is easier to resect the LF under endoscopy
compared with using MED. It was hypothesized that the infusion
pressure of the saline solution may establish a space between the
dural sac and the LF (28);
however, to the best of our knowledge, no relevant study has been
conducted to support this hypothesis. Secondly, the endoscopic
instruments are easier to handle using the iLESSYS®
Delta system compared with the MED system. In the MED system, the
endoscope is fixed firmly in one location with a fixed angle,
making the visualization of a desired surgical field difficult.
Furthermore, the patient is required to be positioned to the
contralateral side to expose the contralateral recess. Meanwhile,
in the iLESSYS® Delta system, improved surgical
visualization is solely acquired by adjusting the angle of the
endoscope (8,16,17).
Conversely, an advantage of the MED system is that it is more
convenient for surgeons to perform complicated maneuvers, since
more surgical devices can be manipulated by two hands concurrently
through using the tubular retractor (28).
 | Table VIComparison between the iLESSYS Delta
and MED approaches. |
Table VI
Comparison between the iLESSYS Delta
and MED approaches.
| Items | iLESSYS Delta | MED |
|---|
| Approach | Interlaminar | Interlaminar |
| Medium | Water | Air |
| Incision | Smaller | Small |
| Puncture site | Paraspinal muscle
1-1.5 cm lateral to the midline | Paraspinal muscle
1.5-2 cm lateral to the midline |
| Diameter of working
tube | 13.7 mm | 18 mm |
| Size of Kerrison
punch | 1.5 and 3 mm | 2 and 3 mm |
| Diameter of
burr | 4.5 mm | 3 mm |
| Hemostasis
instruments | Bipolar
radiofrequency, water pressure | Bipolar
coagulation, aspirator |
| Manipulation | One hand | Two hands |
In the present study, enrolled patients were
diagnosed with either LCSS and/or LRS, and a strict inclusion and
exclusion criteria were applied to avoid potential selection bias.
In total, there were 134 patients (range 53-82 years) with
>20-month follow-ups reported. No significant differences
regarding the demographic characteristics were found between the
two groups. Although comorbidities were common in the present
study, they were well controlled for at the study entry and the
surgical choices for these patients were not affected. The MISS
operation provides an opportunity for older populations with
pre-existing comorbidities to undergo the procedure. Compared with
the MED group, the incision length in the iLESSYS® Delta
group was significantly shorter; however, there was no significant
differences found in the time to return to work between the two
groups. These findings suggested that operation-related trauma was
minimized in both of the two techniques with both techniques having
little influence on the postoperative mobility. However, most
patients were at retirement age, which may have added bias towards
this result. Nonetheless, the duration of the surgery in the
iLESSYS® Delta group was significantly longer compared
with the MED duration. It was suggested that this may be due to the
more complex procedural steps and the relatively subtle endoscopic
manipulation in the iLESSYS® Delta group.
Both the VAS and ODI scores of the two groups were
improved compared with those at the pre-operative stage. The
improvements in the postoperative VAS score for lower back pain and
ODI score in the iLESSYS® Delta group were significantly
decreased compared with the MED group at the 1-week follow-up. This
may be explained by the fact that the prolonged tubular retraction
in the MED group may result in denervation and ischemia of the
paraspinal muscle, causing muscle atrophy and pain following the
operation in the MED group (29).
Compared with the MED, the damage to the paraspinal muscle caused
by the iLESSYS® Delta endoscope and working cannula were
markedly smaller. In addition, participants experienced greater VAS
leg pain relief compared with VAS back pain relief. Although the
MISS operation has been discovered to effectively decompress the
dural sac and/or nerve roots, it may exaggerate the tendency for
spinal instability (30), which is
a prominent cause of lower back pain (31). However, in the present study, it was
assumed that the patients tolerated the postoperative back pain
well, since the patients in both of the two treatment groups
returned to work within 2 weeks. The ODI is widely used to evaluate
the quality of life of patients following the operation, with a
>15% improvement in the ODI representing favorable surgical
outcomes (32). A similar change in
ODI was observed following both protocols. In addition, it has been
reported that the ODI score is strongly associated with the VAS and
SF-36 (the MOS 36-item short form health survey) (33), thus the changes in the ODI score may
be explained by the corresponding changes in the VAS scores
observed in the present study.
The present study also investigated the extent of
the spinal canal decompression through evaluating the CSAD using
MRI. It has been confirmed that a CSAD of <100 mm2 is
a reliable diagnostic parameter for LSS (34). The average CSAS in both groups were
significantly increased after the operation, however, no
significant differences in postoperative CSAD were observed between
the two groups. Similar results for the postoperative CSAD (145
mm2) following MED have also been reported in a previous
study (12). Although the diameter
of the iLESSYS® Delta tubular retractor is smaller than
the tubular retractor used in the MED system and markedly less bone
resection was performed in the iLESSYS® Delta group, an
equal post-operative decompression efficiency was still obtained in
the current study. Thus, it was suggested that the
iLESSYS® Delta technique may not only achieve
decompression of the spinal canal effectively, but it may also
preserve the integrity of the posterior stabilizing structures of
the spine. However, a longer-term follow-up study is required to
investigate the following biomechanical changes of the spine.
Postoperative dysesthesia is a one of the most
frequent complaints in patients treated with spinal endoscopic
surgery (6,15,16).
It has been suggested that postoperative dysesthesia is due to the
temporary compression of the nerve roots and dural sac, which is
caused by the frequent mobility of the working cannula during the
procedure (35,36). The exposure, striping or
displacement of the nerve roots may promote localized ischemia,
followed by mild nerve demyelination. Therefore, it has been
suggested that the working cannula should be mobilized gently
during the operation to reduce postoperative dysesthesia. The
occurrence of a dural tear (2.24%) in the present study was similar
to that reported in previous studies (9,15,37). A
total of 2 patients experienced a dural tear in the MED group and
in this circumstance, endoscopic surgery was changed to open
surgery. In addition, one participant experienced a small-sized
dural tear in the iLESSYS® Delta group; however, the
patient recovered following bed rest without any specific symptoms.
As aforementioned, it was hypothesized that the infusion pressure
of the saline solution in the iLESSYS® Delta system may
prevent the occurrence of a dural tear. However, the occurrence of
dural tears between the two groups was not significant. In
addition, there were three patients (2.24%) who suffered from
reoccurrence, one in the iLESSYS® Delta group and two in
the MED group, which may have been due to the following reasons:
Recurrent stenosis and a progressive slip after laminectomy
(38,39) or the incomplete decompression of the
spinal canal during the operation (30,40).
Several limitations exist in the present study.
Firstly, this was a retrospective study without random assignment
and a small cohort of patients. A randomized, prospective study
with a larger sample size will therefore be required to confirm
these findings. Secondly, the follow-up period was insufficient to
evaluate the potential spinal instability following the MISS
operation. Thirdly, all the procedures were performed by the same
experienced surgeon; therefore, a multi-center study with surgeons
at various levels should be conducted in the future to determine
the clinical outcomes between the two techniques.
In conclusion, the iLESSYS® Delta
approach was found to be comparable to the MED approach for the
treatment of LCSS and LRS, exhibiting precise and limited
decompression. Moreover, the iLESSYS® Delta technique
was revealed to have several advantages, including minimal
short-term postoperative back pain and a faster recovery rate
compared with MED. As the iLESSYS® Delta approach was
found to be safe and exhibited effective results for the treatment
of LCSS and LRSS, it may be regarded as an effective treatment
alternative for the treatment of LCSS and LRS.
Acknowledgements
Not applicable.
Funding
The present study was funded by the Natural Science
Foundation of China (grant no. 81401802), the Natural Science
Foundation of Hubei Province (grant no. 2018CFB487), the China
Postdoctoral Science Foundation (grant no. 2016M593043), and the
Cultivation Project for Medical Science and Technology Youth of PLA
(grant no. 18QNP054).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
BW, CX and FX have made substantial contributions to
the conception and design. HK, CX and BW was involved in drafting
the manuscript or revising it critically for important intellectual
content. FX and HK performed the operation. LT and DZ collected and
analyzed the data. All authors read and approved the final version
of the manuscript.
Ethics approval and consent to
participate
All the procedures in the present study were
approved by the Ethics Committee of the General Hospital of Central
Theater Command and were in accordance with the Helsinki
Declaration. Written informed consent was obtained from each
patient.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ahn Y: Percutaneous endoscopic
decompression for lumbar spinal stenosis. Expert Rev Med Devic.
11:605–616. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Porter RW: Spinal stenosis and neurogenic
claudication. Spine (Phila Pa 1976). 21:2046–2052. 1996.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Kreiner DS, Shaffer WO, Baisden JL,
Gilbert TJ, Summers JT, Toton JF, Hwang SW, Mendel RC and Reitman
CA: North American Spine Society: An evidence-based clinical
guideline for the diagnosis and treatment of degenerative lumbar
spinal stenosis (update). Spine J. 13:734–743. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tosteson AN, Lurie JD, Tosteson TD,
Skinner JS, Herkowitz H, Albert T, Boden SD, Bridwell K, Longley M,
Andersson GB, et al: Surgical treatment of spinal stenosis with and
without degenerative spondylolisthesis: Cost-effectiveness after 2
years. Ann Intern Med. 149:845–853. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Weinstein JN, Tosteson TD, Lurie JD,
Tosteson AN, Blood E, Hanscom B, Herkowitz H, Cammisa F, Albert T,
Boden SD, et al: Surgical versus nonsurgical therapy for lumbar
spinal stenosis. New Engl J Med. 358:794–810. 2008.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Thomé C, Zevgaridis D, Leheta O, Bäzner H,
Pöckler-Schöniger C, Wöhrle J and Schmiedek P: Outcome after
less-invasive decompression of lumbar spinal stenosis: A randomized
comparison of unilateral laminotomy, bilateral laminotomy, and
laminectomy. J Neurosurg Spine. 3:129–141. 2005.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Deyo RA, Mirza SK, Martin BI, Kreuter W,
Goodman DC and Jarvik JG: Trends, major medical complications, and
charges associated with surgery for lumbar spinal stenosis in older
adults. JAMA. 303:1259–1265. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lee C, Yoon K and Ha S: Comparative
analysis between three different lumbar decompression techniques
(microscopic, tubular, and endoscopic) in lumbar canal and lateral
recess stenosis: Preliminary report. Biomed Res Int.
2019(6078469)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
McGrath LB, White-Dzuro GA and Hofstetter
CP: Comparison of clinical outcomes following minimally invasive or
lumbar endoscopic unilateral laminotomy for bilateral
decompression. J Neurosurg Spine. 1–9. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Xu BS, Tan QS Xia Q, Ji N and Hu YC:
Bilateral decompression via unilateral fenestration using mobile
microendoscopic discectomy technique for lumbar spinal stenosis.
Orthop Surg. 2:106–110. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yagi M, Okada E, Ninomiya K and Kihara M:
Postoperative outcome after modified unilateral-approach
microendoscopic midline decompression for degenerative spinal
stenosis. J Neurosurg Spine. 10:293–299. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ikuta K, Arima J, Tanaka T, Oga M, Nakano
S, Sasaki K, Goshi K, Yo M and Fukagawa S: Short-term results of
microendoscopic posterior decompression for lumbar spinal stenosis.
J Neurosurg Spine. 2:624–633. 2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Minamide A, Yoshida M, Yamada H, Nakagawa
Y, Kawai M, Maio K, Hashizume H, Iwasaki H and Tsutsui S:
Endoscope-assisted spinal decompression surgery for lumbar spinal
stenosis. J Neurosurg Spine. 19:664–671. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Youn MS, Shin JK, Goh TS, Son SM and Lee
JS: Endoscopic posterior decompression under local anesthesia for
degenerative lumbar spinal stenosis. J Neurosurg Spine. 29:661–666.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Komp M, Hahn P, Oezdemir S, Giannakopoulos
A, Heikenfeld R, Kasch R, Merk H, Godolias G and Ruetten S:
Bilateral spinal decompression of lumbar central stenosis with the
full-endoscopic interlaminar versus microsurgical laminotomy
technique: A prospective, randomized, controlled study. Pain
Physician. 18:61–70. 2015.PubMed/NCBI
|
|
16
|
Lee C, Yoon K and Jun J: Percutaneous
endoscopic laminotomy with flavectomy by uniportal, unilateral
approach for the lumbar canal or lateral recess stenosis. World
Neurosurg. 113:e129–e137. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Middleton SD, Wagner R and Gibson JA:
Multi-level spine endoscopy: A review of available evidence and
case report. EFORT Open Rev. 2:317–323. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Schizas C, Theumann N, Burn A, Tansey R,
Wardlaw D, Smith FW and Kulik G: Qualitative grading of severity of
lumbar spinal stenosis based on the morphology of the dural sac on
magnetic resonance images. Spine (Phila Pa 1976). 35:1919–1924.
2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Meyerding HW: Spondylolisthesis: Surgical
treatment and results. Surg Gynec Obst. 54:371–377. 1932.
|
|
20
|
DeVine J, Norvell DC, Ecker E, Fourney DR,
Vaccaro A, Wang J and Andersson G: Evaluating the correlation and
responsiveness of patient-reported pain with function and
quality-of-life outcomes after spine surgery. Spine(Phila Pa 1976).
36 (Suppl 21):S69–S74. 2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Xiong C, Li T, Kang H, Hu H, Han J and Xu
F: Early outcomes of 270-degree spinal canal decompression by using
TESSYS-ISEE technique in patients with lumbar spinal stenosis
combined with disk herniation. Eur Spine J. 28:78–86.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Siepe CJ, Sauer D and Michael Mayer H:
Full endoscopic, bilateral over-the-top decompression for lumbar
spinal stenosis. Eur Spine J. 27 (Suppl 27):S563–S565.
2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Choi G, Lee S, Raiturker PP, Lee S and
Chae Y: Percutaneous endoscopic interlaminar discectomy for
intracanalicular disc herniations at L5-S1 using a rigid working
channel endoscope. Oper Neurosurg. 58 (Suppl 1):ONS59–68;
discussion ONS59-68. 2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Ruetten S, Komp M and Godolias G: A new
full-endoscopic technique for the interlaminar operation of lumbar
disc herniations using 6-mm endoscopes: Prospective 2-year results
of 331 patients. Minim Invasive Neurosurg. 49:80–87.
2006.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ruan W, Feng F, Liu Z, Xie J, Cai L and
Ping A: Comparison of percutaneous endoscopic lumbar discectomy
versus open lumbar microdiscectomy for lumbar disc herniation: A
meta-analysis. Int J Surg. 31:86–92. 2016.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Liu X, Yuan S, Tian Y, Wang L, Gong L,
Zheng Y and Li J: Comparison of percutaneous endoscopic
transforaminal discectomy, microendoscopic discectomy, and
microdiscectomy for symptomatic lumbar disc herniation: Minimum
2-year follow-up results. J Neurosurg Spine. 28:317–325.
2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ahn Y: Endoscopic spine discectomy:
Indications and outcomes. Int Orthop. 43:909–916. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Li H, Jiang C, Mu X, Lan W, Zhou Y and Li
C: Comparison of MED and PELD in the treatment of adolescent lumbar
disc herniation: A 5-year retrospective follow-up. World Neurosurg.
112:e255–e260. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Taylor H, McGregor AH, Medhi-Zadeh S,
Richards S, Kahn N, Zadeh JA and Hughes SP: The impact of
self-retaining retractors on the paraspinal muscles during
posterior spinal surgery. Spine (Phila Pa 1976). 27:2758–2762.
2002.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Minamide A, Yoshida M, Yamada H, Nakagawa
Y, Hashizume H, Iwasaki H and Tsutsui S: Clinical outcomes after
microendoscopic laminotomy for lumbar spinal stenosis: A 5-year
follow-up study. Eur Spine J. 24:396–403. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Panjabi MM: Clinical spinal instability
and low back pain. J Electromyogr Kines. 13:371–379.
2003.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Casal-Moro R, Castro-Menéndez M,
Hernández-Blanco M, Bravo-Ricoy JA and Jorge-Barreiro FJ: Long-term
outcome after microendoscopic diskectomy for lumbar disk
herniation: A prospective clinical study with a 5-year follow-up.
Neurosurgery. 68:1568–1575. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Liu H, Tao H and Luo Z: Validation of the
simplified Chinese version of the Oswestry Disability Index. Spine
(Phila Pa 1976). 34:1211–1216. 2009.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Schonstrom NS, Bolender N and Spengler DM:
The pathomorphology of spinal stenosis as seen on CT scans of the
lumbar spine. Spine (Phila Pa 1976). 10:806–811. 1985.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Yang JS, Chu L, Chen CM, Wang XF, Xie PG,
Deng R, Yu KX, Shi L, Zhang ZX, Rong LM, et al: Foraminoplasty at
the tip or base of the superior articular process for lateral
recess stenosis in percutaneous endoscopic lumbar discectomy: A
multicenter, retrospective, controlled study with 2-year follow-up.
Biomed Res Int. 2018(7692794)2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Yang J, Wu H, Kong Q, Wang Y, Peng Z,
Zhang L, Yan Y, Guo C and Zhang D: Full endoscopic transforaminal
decompression surgery for symptomatic lumbar spinal stenosis in
geriatric patients. World Neurosurg. 127:e449–e459. 2019.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Heo DH, Quillo-Olvera J and Park CK: Can
percutaneous biportal endoscopic surgery achieve enough canal
decompression for degenerative lumbarstenosis? Prospective
case-control study. World Neurosurg. 120:e684–e689. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Fritsch EW, Heisel J and Rupp S: The
failed back surgery syndrome: Reasons, intraoperative findings, and
long-term results: A report of 182 operative treatments. Spine
(Phila Pa 1976). 21:626–633. 1996.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Gerling MC, Leven D, Passias PG, Lafage V,
Bianco K, Lee A, Lurie JD, Tosteson TD, Zhao W, Spratt KF, et al:
Risk factors for reoperation in patients treated surgically for
lumbar stenosis: A subanalysis of the 8 year data from the SPORT
trial. Spine (Phila Pa 1976). 41:901–909. 2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Schöller K, Steingrüber T, Stein M, Vogt
N, Müller T, Pons-Kühnemann J and Uhl E: Microsurgical unilateral
laminotomy for decompression of lumbar spinal stenosis: Long-term
results and predictive factors. Acta Neurochir (Wien).
158:1103–1113. 2016.PubMed/NCBI View Article : Google Scholar
|