Introduction
Polycystic ovary syndrome (PCOS) is one of the most
common endocrine disorders in females, affecting 8-13% of
reproductive-age women (1,2). It is a multifactorial disorder with a
broad spectrum of clinical manifestations, characterized by
elevated levels of luteinizing hormone (LH) and androgen, ovulatory
dysfunction and irregular menstrual cycles, as well as the
appearance of a polycystic ovarian morphology on ultrasound
imaging.
Among patients with PCOS, 60-80% suffer from
hyperandrogenemia and most of them have slightly elevated levels of
circulating androgens (3-5).
The effects of androgen are mainly mediated via the androgen
receptor (AR), a ligand-dependent nuclear transcription factor
belonging to the steroid hormone nuclear receptor family.
Increasing evidence has suggested that AR may serve roles in the
development of PCOS (6-10).
Previous studies have demonstrated that AR (CAG)n repeats (5) and rs6152A (6) gene polymorphisms are associated with
the pathogenesis of PCOS (11-15).
Xia et al (16) performed a
case-control study involving 261 patients with PCOS and 278 healthy
controls, revealing that shorter alleles of (CAG)n in exon 1 of the
AR gene enhance the susceptibility to PCOS, either by upregulating
AR activity or by causing hyperandrogenism. Mohlig et al
(17) demonstrated that the AR CAG
repeat polymorphism may result in metabolic disorders by modifying
the impact of testosterone (T) on insulin resistance in PCOS, which
is consistent with previous studies (12,14).
Splice variants of AR have been reported to occur in various
androgen-sensitive types of cancer, including prostate cancer,
breast cancer and liver cancer cell lines (18). Wang et al (19) proposed that somatic mutations in AR
have an etiological role in the pathogenesis of PCOS. The study
revealed that in the majority of PCOS samples, ovarian granulosa
cells possess somatic insertions or deletions in the AR gene. These
samples have a higher total serial T, serial dehydroepiandrosterone
and follicular fluid free androgen index and only the insertion
allele is associated with higher follicular fluid levels of
anti-Müllerian hormone (AMH), a growth factor produced solely by
small follicles (19-22).
Furthermore, Nam et al (23)
observed that a patient with AR-mutated PCOS gave birth to a baby
girl with androgen insensitivity syndrome. Therefore, it was
hypothesized that abnormally expressed and/or dysfunctional AR may
serve certain roles in the pathogenesis of PCOS.
In the present study, a total of 258 Han Chinese
patients with PCOS were recruited and analyzed for the presence of
AR mutations with the aim of exploring the potential involvement of
AR mutations in the pathogenesis of PCOS.
Materials and methods
Patients and blood samples
A total of 258 infertile females with PCOS (average
age, 27.85±3.46 years; age range, 21-41 years) who underwent in
vitro fertilization/intracytoplasmic sperm injection-embryo
transfer (IVF/ICSI-ET) cycles were recruited at Jiangxi Provincial
Maternal and Child Health Hospital (Nanchang, China) between
October 2016 and September 2018. PCOS was diagnosed according to
the Rotterdam criteria (24),
requiring the presence of two of the following features: i)
Oligo/anovulation; ii) hyperandrogenism; and iii) polycystic
ovaries detected by ultrasound imaging. Hyperandrogenism was
diagnosed on the basis of either hirsutism or hyperandrogenemia.
Hirsutism was determined by means of a modified Ferriman-Gallwey
score >6(25). Hyperandrogenemia
was defined as an elevated total T level according to laboratory
criteria (normal level, 10.83-56.94 ng/dl). Polycystic ovaries on
ultrasound imaging were defined as the presence of ≥12 antral
follicles measuring 2-9 mm in diameter and/or an increased ovarian
volume (>10 cm3) (26). Other causes of hyperandrogenism and
ovulation dysfunction, including ovarian interstitial tumor or
adrenal tumor, congenital adrenal hyperplasia, hyperprolactinemia
and thyroid dysfunction, were ruled out.
Patients were excluded from the present study if
they had congenital or acquired uterine malformations, including
septate uterus, duplex uterus, adenomyosis, submucous myoma or
intrauterine adhesion, abnormal results of chromosome karyotyping
or medical conditions that contraindicated assisted reproductive
technology or pregnancy. Patients with controlled diabetes and
hypertension were not excluded. There were no male-factor
exclusions and the use of donor semen was not allowed. In addition,
a total of 520 female Han Chinese control (average age, 31.48±5.59
years; age range, 20-42 years) subjects without PCOS were recruited
at Jiangxi Provincial Maternal and Child Health Hospital (Nanchang,
China) between October 2016 and September 2018. Details of the
cases and controls are provided in Table I.
 | Table IPotential association analysis of
clinical data and potential pathogenic mutations in the androgen
receptor gene. |
Table I
Potential association analysis of
clinical data and potential pathogenic mutations in the androgen
receptor gene.
| | PCOS cases
(n=258) | |
|---|
| Parameter | Mutation (n=3) | Without or with
benign mutations (n=255) |
P-valuea |
|---|
| Age (years) | 27.33±4.51 | 27.86±3.46 | 0.795 |
| Duration of
infertility (years) | 3.67±1.53 | 4.12±2.48 | 0.753 |
| BMI
(kg/m2) | 20.94±0.65 | 23.33±3.4 | 0.225 |
| Basal FSH
(IU/l) | 6.94±1.66 | 5.82±1.39 | 0.169 |
| Basal LH
(IU/l) | 9.92±0.81 | 9.76±5.19 | 0.803 |
| LH/FSH | 1.48±0.36 | 1.73±1.08 | 0.690 |
| Basal E2
(pg/ml) | 41.45±14.4 | 55.03±99.94 | 0.252 |
| Basal T
(ng/dl) | 44.12±13.87 | 60.29±210.68 | 0.317 |
| Basal PRL
(ng/ml) | 17.71±6.08 | 16.33±14.62 | 0.870 |
| AMH (ng/ml) | 6.52±1.71 | 9.28±4.95 | 0.337 |
| FT3 (pg/ml) | 3.26±0.44 | 3.36±0.41 | 0.677 |
| FT4 (ng/dl) | 1.44±0.05 | 1.43±1.03 | 0.813 |
| TSH (mIU/l) | 1.95±0.31 | 2.4±1.79 | 0.665 |
| CA125 (U/ml) | 22.79±26.25 | 17.67±25.23 | 0.727 |
| FBG (mM) | 4.9±0.17 | 4.84±0.5 | 0.828 |
| Triglyceride
(mM) | 0.72±0.23 | 1.39±0.95 | 0.226 |
| TC (mM) | 4.02±0.46 | 4.46±0.81 | 0.349 |
| HDL (mM) | 1.26±0.24 | 1.25±0.27 | 0.926 |
| LDL (mM) | 2.43±0.34 | 2.58±0.74 | 0.730 |
| AFC (n) | 19.00±3.61 | 23.27±5.28 | 0.164 |
| Length of menstrual
cycle (days) | 45.83±13.77 | 63.81±42.25 | 0.463 |
| Duration of ovarian
stimulation (days) | 12.00±1.73 | 12.99±2.93 | 0.559 |
| Total dose of
gonadotrophins (IU) | 1404.17±199.35 | 1989.85±954.69 | 0.290 |
| Oocytes retrieved
(n) | 13.33±2.52 | 17.08±7.94 | 0.416 |
| LH level on hCG
injection day (IU/l) | 1.40±0.58 | 0.94±0.77 | 0.304 |
| Progesterone level
on hCG injection day (ng/ml) | 0.78±0.22 | 0.62±0.33 | 0.426 |
| E2 level on hCG
injection day (pg/ml) | 2227.00±184.82 |
3180.24±1710.25 | <0.001 |
| 2PN fertilized
oocytes (n) | 10.00±2.00 | 11.01±6.04 | 0.772 |
| Available embryos
(n) | 6.33±1.53 | 4.67±2.89 | 0.322 |
| High-quality
embryos (n) | 3.67±2.52 | 2.69±2.50 | 0.500 |
| Embryo transfer
rate | 1/3(33.33) | 146/255(57.25) | 0.579 |
| Clinical pregnancy
rate | 1/1(100) | 98/142(69.01) | 1.000 |
Measurement of hormones and
biochemical parameters
All hormones and biochemical indicators were
assessed at the Clinical Laboratory of Jiangxi Provincial Maternal
and Child Health Hospital (Nanchang, China). The basal levels of
follicle-stimulating hormone (FSH), LH, estrogen (E2), T, prolactin
(PRL), AMH, free triiodothyronine (FT3), free thyroxine (FT4),
thyroid-stimulating hormone (TSH) and cancer antigen 125 (CA125),
and the levels of LH, progesterone and E2 on the day of human
chorionic gonadotropin (hCG) injection were measured by
radioimmunoassay methods as described previously (27). Fasting blood glucose (FBG),
triglyceride, total cholesterol (TC), high-density lipoprotein
cholesterol (HDL) and low-density lipoprotein cholesterol (LDL)
levels were examined using a Beckman AU5800 fully automatic
biochemical analyzer (Beckman Coulter, Inc.) and the gold-labeling
method (28). Other clinical data,
including age, duration of infertility, body mass index (BMI),
antral follicle count (AFC), length of menstrual cycle, duration of
ovarian stimulation, total dose of gonadotrophins and number of
oocytes retrieved, were collected from the clinical records of the
patients (Table I).
Mutational analysis of the AR
gene
Genomic DNA was isolated from the peripheral blood
samples of patients with PCOS using the DNeasy Blood kit (cat. no.
69504; Qiagen, Inc.) according to the manufacturer's protocol. The
entire coding regions and the adjacent exon/intron boundaries of
the AR gene were amplified by PCR with 10 sets of primer pairs
(Table II). In brief, for each PCR
amplification reaction, ~50 ng total DNA was used in a final volume
of 30 µl, with the following amplification protocol: Initial
pre-denaturation step at 94˚C for 3 min, followed by 35 cycles of
denaturation at 94˚C for 30 sec, annealing at different
temperatures (52-60˚C; Table II)
for 30 sec and extension at 72˚C for 30 sec; final extension at
72˚C for 7 min. PCR was performed using a Thermal Cycler 2720
(Applied Biosystems; Thermo Fisher Scientific, Inc.). The PCR
amplification products were then purified and sequenced on an ABI
Prism 3730 DNA sequencer (Applied Biosystems; Thermo Fisher
Scientific, Inc.). An additional independent PCR amplification and
DNA sequencing experiment was performed with samples of patients
with PCOS harboring potential AR mutations. PCR amplification and
DNA sequencing were performed as described above. The identified
mutations were confirmed by bidirectional sequencing on ABI 3730
Prism DNA sequencer (Applied Biosystems; Thermo Fisher Scientific,
Inc.).
 | Table IIPrimers for PCR mutational analyses
of the androgen receptor gene. |
Table II
Primers for PCR mutational analyses
of the androgen receptor gene.
| Target region | Annealing
temperature (˚C) | Forward primer
(5'-3') | Reverse primer
(5'-3') | PCR amplicon length
(bp) |
|---|
| Exon 1-1 | 52 |
GTGGGCAGCTAGCTGCAGC |
GTAATTGTCCTTGGAGGA | 789 |
| Exon 1-2 | 56 |
ACAGCAGCAGGAAGCAGT |
AGGTCCCCATAGCGGCACT | 645 |
| Exon 1-3 | 54 |
CCACGCTCGCATCAAGCTG |
ACGGGAGAGCTCTAGGTT | 611 |
| Exon 2 | 55 |
GCAGGTTAATGCTGAAGAC |
CTCCTAAGTTATTTGATAG | 377 |
| Exon 3 | 58 |
TCATGTGGTAGGATATAAT |
TGGCTGATGGCCACGTTGC | 388 |
| Exon 4 | 58 |
AAGGAGTTTAGAGTCTGTG |
ATTGAGACTTGTAACAAT | 571 |
| Exon 5 | 52 |
TAGGGGATGCCCGAATACC |
GCCAGTTGGCTGAAAGCC | 430 |
| Exon 6 | 50 |
TCCCTGGAGCACCAGCAGG |
TTGTTTCTTGTTAGGAA | 442 |
| Exon 7 | 60 |
AGCACACAGACTTCAACTA |
TTCACAATATCCAGCTGG | 497 |
| Exon 8 | 55 |
TCGCTGTCTCTCTCTAACA |
TGTGGCTGGCACAGAGTA | 693 |
Bioinformatics prediction of the
pathogenicity of AR mutations
Two online bioinformatic programs, PolyPhen-2
(http://genetics.bwh.harvard.edu/pph2/) (29) and MutationTaster (http://mutationtaster.org/) (30) were used to analyze the
disease-causing potential of the identified missense mutations.
Bioinformatics analysis was performed in July 2019. PolyPhen-2 and
MutationTaster automatically assessed whether each mutation was
either pathogenic or benign, respectively.
Evolutionary conservation analysis of
AR mutations
The protein sequences from 14 vertebrate species in
the GenBank database (https://www.ncbi.nlm.nih.gov/genbank/) were used to
analyze the evolutionary conservation status of the AR mutations.
The species included Homo sapiens (NP_000035), Pan
troglodytes (XP_024208738), Rattus norvegicus
(NP_036634), Sus scrofa (NP_999479), Bos taurus
(NP_001231056), Canis lupus familiaris (NP_001003053),
Equus caballus (NP_001157363), Felis catus (XP_023105265),
Loxodonta africana (XP_003412790), Myotis brandtii
(XP_003412790), Octodon degus (XP_004644568), Orycteropus
afer (XP_007954477), Ovis aries (NP_001295513) and
Acinonyx jubatus (XP_026909508). Multiple sequence alignment
was performed using the ‘ClustalW’ tool of the alignment function
in the Molecular Evolutionary Genetics Analysis software (version
4.0) which was created and developed by Kumar et al
(31).
Statistical analysis
Clinical data and the frequency differences of AR
mutations were analyzed by two-tailed Fisher's exact tests using
SPSS software (version 18.0; SPSS, Inc.). Continuous quantitative
data are expressed as the mean ± standard deviation. Differences
among groups were compared using Student's t-test. P<0.05 was
considered to indicate a statistically significant difference.
Results
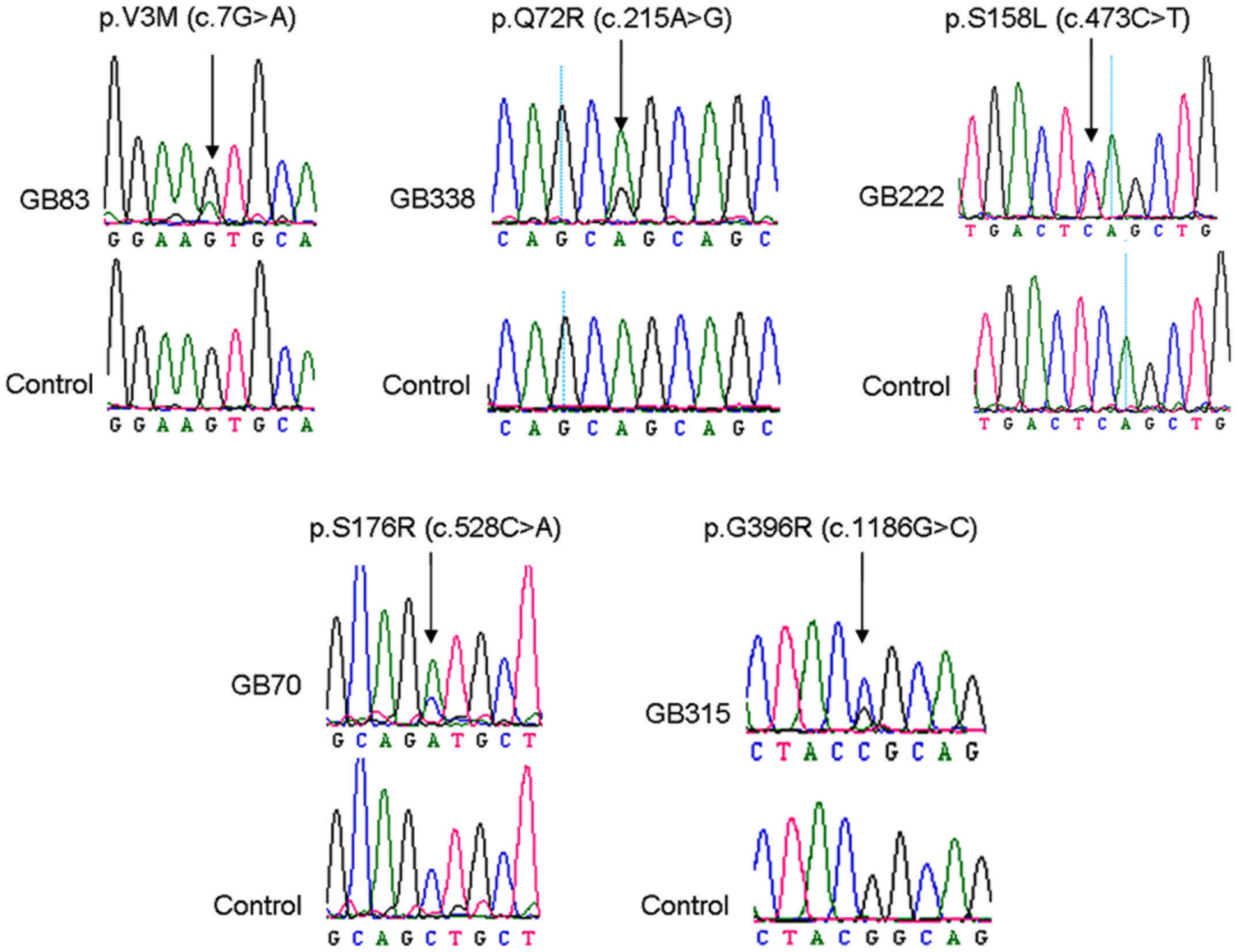
AR mutations
In the present study, all eight coding exons of the
AR gene were sequenced for the presence of AR mutations in 258
samples from patients with PCOS. A total of five heterozygous
missense mutations, p.V3M (c.7G>A), p.Q72R (c.215A>G),
p.S158L (c.473C>T), p.S176R (c.528C>A) and p.G396R
(c.1186G>C), were identified in 5/258 PCOS samples (Fig. 1; Table
III). Among these mutations, p.S158L was a novel mutation and,
to the best of our knowledge, has not been reported previously. In
addition, it was not detected in either the 520 Han Chinese control
subjects or in the Exome Aggregation Consortium (EXAC) database.
The remaining four mutations were previously reported in public
databases; however, they were absent or only detected in the 520
Han Chinese control subjects and the EXAC database at low
frequencies (Table III). Compared
with the 520 Chinese patients without PCOS, the mutation frequency
of each of the five AR mutations exhibited no statistically
significant difference; however, three of these mutations, p.V3M,
p.Q72R and p.S158L, exhibited significant differences in mutation
frequency when compared with those in the EXAC database
(P<0.05).
 | Table IIIAndrogen receptor mutations
identified in the present study. |
Table III
Androgen receptor mutations
identified in the present study.
| Mutation | Polyphen-2
prediction | MutationTaster
prediction | ID in dbSNP | Novel mutation | PCOS cases
(n=258) | Control subjects
(n=520) |
P-valuea | EXAC |
P-valuea |
|---|
| p.V3M | Probably
damaging |
Disease-causing | rs778912582 | No | 1/516 | 0/1040 | 0.332 | 5/73236 | 0.041 |
| p.Q72R | Benign | Polymorphism | rs767121593 | No | 1/516 | 0/1040 | 0.332 | 0/48582 | 0.011 |
| p.S158L | Probably
damaging |
Disease-causing | - | Yes | 1/516 | 0/1040 | 0.332 | 0/43682 | 0.012 |
| p.S176R | Probably
damaging |
Disease-causing | rs777131133 | No | 1/516 | 0/1040 | 0.332 | 45/39906 | 0.446 |
| p.G396R | Benign | Polymorphism | rs202150225 | No | 1/516 | 1/1040 | 0.553 | 4/28463 | 0.086 |
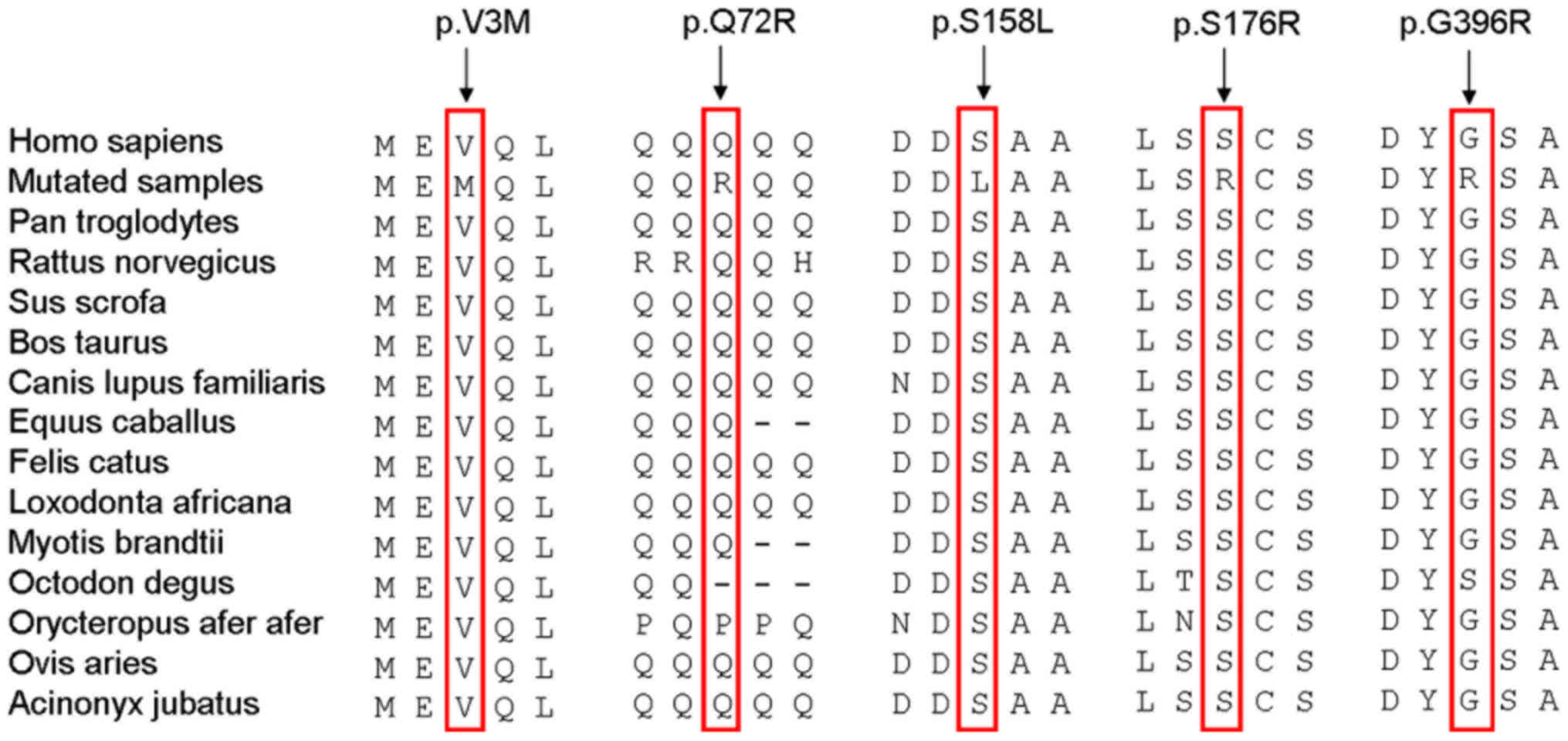
Evolutionary conservation and in
silico analysis of AR mutations
Evolutionary conservation analysis revealed that
three AR mutations, p.V3M, p.S158L and p.S176R, were highly
conserved among the 14 vertebrate species ranging from Homo
sapiens to Acinonyx jubatus, while the p.Q72R and
p.G396R mutations were not generally conserved among these
vertebrate species, except for Orycteropus afer and
Octodon degus for p.Q72R and Octodon degus for
p.G396R (Fig. 2). Furthermore,
in silico analysis of these mutations demonstrated that the
p.V3M, p.S158L and p.S176R mutations were pathogenic, while the
p.Q72R and p.G396R mutations were likely to be benign. These
combined results implicated that p.V3M, p.S158L and p.S176R, but
not the p.Q72R and p.G396R mutations, may be pathogenic.
Clinical characteristics of patients
with PCOS
The general clinical features of the 258 patients
with PCOS are summarized in Table
I. The detailed clinical features of the 3 patients with PCOS
with potential pathogenic AR mutations (p.V3M, p.S158L and p.S176R)
are listed in Table IV. In brief,
the average BMI was 20.94±0.65 kg/m2 and the average
basal levels of serum FSH, LH, E2 and T were 6.94±1.66 IU/l,
9.92±0.81 IU/l, 41.45±14.4 pg/ml and 44.12±13.87 ng/dl,
respectively. The average serum AMH level was 6.52±1.71 ng/ml and
the average serum levels of FBG, triglyceride, TC, HDL and LDL were
4.9±0.17, 0.72±0.23, 4.02±0.46, 1.26±0.24 and 2.43±0.34 mM,
respectively. Of note, the patient with the p.S158L mutation was 27
years old and had slightly elevated serum levels of T (57.51 ng/dl)
and FT3 (3.75 pg/ml), while the patient with the p.S176R mutation
was 23 years old and had elevated serum levels of CA125 (52.96
U/ml). However, for the patient with the p.V3M mutation (age, 32
years), no distinctly aberrant clinical parameters were
identified.
 | Table IVDetailed clinical characteristics of
the three patients with polycystic ovary syndrome with potential
pathogenic androgen receptor mutations. |
Table IV
Detailed clinical characteristics of
the three patients with polycystic ovary syndrome with potential
pathogenic androgen receptor mutations.
| Parameter | p.V3M | p.S158L | p.S176R | Reference
range |
|---|
| Age (years) | 32 | 27 | 23 | - |
| Duration of
infertility (years) | 4 | 2 | 5 | - |
| BMI
(kg/m2) | 20.83 | 20.36 | 21.64 | 18.50-25.00 |
| Basal FSH
(IU/l) | 8.85 | 6.08 | 5.89 | 3.03-8.08 |
| Basal LH
(IU/l) | 9.57 | 10.84 | 9.34 | 1.80-11.78 |
| Basal E2
(pg/ml) | 56.78 | 39.38 | 28.2 | 21.00-251.00 |
| Basal T
(ng/dl) | 45.04 | 57.51 | 29.82 | 10.83-56.94 |
| Basal PRL
(ng/ml) | 21.12 | 10.69 | 21.33 | 5.18-26.53 |
| AMH (ng/ml) | 6.16 | 5.02 | 8.38 | 20-29 year-olds:
1.18-9.49 |
| | | | | 30-39 year-olds:
0.67-5.24 |
| FT3 (pg/ml) | 2.91 | 3.75 | 3.11 | 1.71-3.71 |
| FT4 (ng/dl) | 1.46 | 1.39 | 1.48 | 0.70-1.48 |
| TSH (mIU/l) | 2.13 | 2.13 | 1.59 | 0.35-4.95 |
| CA125 (U/ml) | 10.2 | 5.21 | 52.96 | 0.00-35.00 |
| FBG (mM) | 4.8 | 5.1 | 4.8 | 3.90-6.10 |
| TG (mM) | 0.69 | 0.97 | 0.51 | 0.34-1.69 |
| TC (mM) | 3.68 | 4.54 | 3.84 | 0.00-5.20 |
| HDL (mM) | 1.01 | 1.3 | 1.48 | 0.90-2.00 |
| LDL (mM) | 2.36 | 2.8 | 2.13 | 0.00-3.74 |
| AFC (n) | 15 | 22 | 20 | - |
| Length of menstrual
cycle (days) | 45 | 32.5 | 60 | - |
| Duration of ovarian
stimulation (days) | 14 | 11 | 11 | - |
| Total dose of
gonadotrophins (IU) | 1625 | 1237.5 | 1350 | - |
| Oocytes retrieved
(n) | 11 | 13 | 16 | - |
| LH level on hCG
injection day (IU/l) | 1.17 | 2.06 | 0.98 | - |
| Progesterone level
on hCG injection day (ng/ml) | 0.86 | 0.53 | 0.94 | - |
| E2 level on hCG
injection day (pg/ml) | 2109 | 2132 | 2440 | - |
| 2PN fertilized
oocytes (n) | 8 | 12 | 10 | |
| Available embryos
(n) | 5 | 8 | 6 | |
| Fresh embryos
transferred (n) | 0 | 0 | 2 | |
| Clinical
outcomes | All embryos | All embryos | Delivery of | |
| | frozen | frozen | 2 newborns | |
Associations between AR mutations and
clinical features
In the present study, the differences in demographic
and clinical characteristics between the three patients with PCOS
with potential pathogenic AR mutations (p.V3M, p.S158L and p.S176R)
were compared with those of the remaining 255 patients with PCOS
without AR mutations or with likely benign AR mutations. The
average serum E2 level on the day of hCG injection in the three
patients with pathogenic AR mutations was 2,227.00±184.82 pg/ml,
which was significantly lower than that of the 255 patients with
PCOS with benign AR mutations or without AR mutations
(3,180.24±1,710.25 pg/ml; P<0.01 (Table I).
Discussion
Previous studies have demonstrated that androgens
serve crucial roles in the regulatory process of follicle
development. They mediate their regulatory actions mainly via their
specific AR receptors, affecting the transcription and translation
of multiple female follicle development-associated downstream
target genes (32,33). Furthermore, previous studies have
revealed that nucleotide change (19,34) or
aberrant expression (32,35) of AR may promote the progression of
PCOS.
In the present study, a total of five AR missense
mutations were detected among 258 Han Chinese patients with PCOS.
Among these, p.S158L was a novel mutation which, to the best of our
knowledge, has not been reported previously. It was neither
detected in the 520 Han Chinese control subjects nor in the EXAC
database. Furthermore, the evolutionary conservation and in
silico analysis results suggested that the p.S158L mutation may
be harmful. Of note, the patient with the p.S158L mutation had
slightly elevated serum levels of T and FT3. It was speculated that
the increased level of T may be attributed to partial androgen
insensitivity caused by the mutation. However, this hypothesis
requires further validation by in vitro or in vivo
studies.
Among the remaining four mutations, the p.V3M and
p.S176R mutations have been reported in the EXAC database with low
frequency, while they were not detected in the 520 Han Chinese
control subjects. The evolutionary conservation and in
silico analysis results revealed that these two mutations may
be pathogenic. On the other hand, it was speculated that the p.Q72R
and p.G396R mutations may be benign based on the evolutionary
conservation and in silico analysis results.
In the present study, the potential association
between the three pathogenic AR mutations and available clinical
characteristics, including age, duration of infertility, BMI, basal
levels of FSH, LH, E2, T and PRL, AMH, FT3, FT4, TSH, CA125, FBG,
triglyceride, TC, HDL, LDL, AFC, length of menstrual cycle,
duration of ovarian stimulation, total dose of gonadotrophins,
number of oocytes retrieved, the levels of LH, progesterone and E2
on the day of hCG injection, 2PN fertilized oocytes, number of
available embryos, number of high-quality embryos, embryo transfer
rate and clinical pregnancy rate, was analyzed. Compared with the
255 patients with PCOS with benign AR mutations or without AR
mutations, significantly lower serum E2 levels on the day of hCG
injection were observed in the three patients with PCOS with
potentially pathogenic AR mutations (P<0.01). Furthermore, the
patients with AR mutations had a lower number of oocytes retrieved;
however, this difference was not statistically significant. In
addition, no significant association was observed between AR
mutations and any of the other clinical parameters.
It should be noted that the present study had
certain limitations. First, the clinical observations should be
treated with caution due to the relatively small sample size of
patients with AR mutations (n=3) in the present study. A larger
number of samples should be collected to confirm these observations
in a future study. Furthermore, the collection scope of samples was
limited to IVF/ICSI-ET and there may be potential selection bias
due to the setting of the present study (IVF clinic). Finally, for
the AR mutations identified, only a bioinformatics analysis was
performed and functional analysis in vitro is required in a
future study to understand the role of the AR gene in the
pathogenesis of PCOS.
In summary, the present study identified a total of
three potential pathogenic mutations in 258 Han Chinese patients
with PCOS and the current study hypothesizes that these mutations
may serve a role in the pathogenesis of PCOS.
Acknowledgements
Not applicable.
Funding
The present study was supported by the GanPo
Outstanding Talents 555 Project of Jiangxi Province, China, to OH
and the Social Development Foundation of Jiangxi Province, China
(grant no. 20151BBG70100 to LT).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
LT performed the experiments and prepared the
manuscript. JT, YW, LXu and GC performed mutation screening. YZ
performed conservation and mutation analysis. LXi performed data
analysis. YW and JC collected the samples and data analysis. OH and
QW designed the study and revised the manuscript. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of Jiangxi Provincial Maternal and Child Health
Hospital (Nanchang, China) and written informed consent was
obtained from all patients prior to the study. The present study
was performed according to the Declaration of Helsinki and the
ethical guidelines of Jiangxi Provincial Maternal and Child Health
Hospital (Nanchang, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Teede H, Deeks A and Moran L: Polycystic
ovary syndrome: A complex condition with psychological,
reproductive and metabolic manifestations that impacts on health
across the lifespan. BMC Med. 8(41)2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Azziz R, Carmina E, Chen Z, Dunaif A,
Laven JS, Legro RS, Lizneva D, Natterson-Horowtiz B, Teede HJ and
Yildiz BO: Polycystic ovary syndrome. Nat Rev Dis Primers.
2(16057)2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Azziz R, Carmina E, Dewailly D,
Diamanti-Kandarakis E, Escobar-Morreale HF, Futterweit W, Janssen
OE, Legro RS, Norman RJ, Taylor AE, et al: Androgen Excess Society:
Positions statement: Criteria for defining polycystic ovary
syndrome as a predominantly hyperandrogenic syndrome: An Androgen
Excess Society guideline. J Clin Endocrinol Metab. 91:4237–4245.
2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Chang WY, Knochenhauer ES, Bartolucci AA
and Azziz R: Phenotypic spectrum of polycystic ovary syndrome:
Clinical and biochemical characterization of the three major
clinical subgroups. Fertil Steril. 83:1717–1723. 2005.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Livadas S, Pappas C, Karachalios A,
Marinakis E, Tolia N, Drakou M, Kaldrymides P, Panidis D and
Diamanti-Kandarakis E: Prevalence and impact of hyperandrogenemia
in 1,218 women with polycystic ovary syndrome. Endocrine.
47:631–638. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Owens LA, Kristensen SG, Lerner A,
Christopoulos G, Lavery S, Hanyaloglu AC, Hardy K, Yding Andersen C
and Franks S: Gene expression in granulosa cells from small antral
follicles from women with or without polycystic ovaries. J Clin
Endocrinol Metab. 104:6182–6192. 2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Younas K, Quintela M, Thomas S,
Garcia-Parra J, Blake L, Whiteland H, Bunkheila A, Francis LW,
Margarit L, Gonzalez D, et al: Delayed endometrial decidualisation
in polycystic ovary syndrome; the role of AR-MAGEA11. J Mol Med
(Berl). 97:1315–1327. 2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Xu G, Wang Q, Zhang AD, Liu JD, Feng JW
and Chen YL: Effect of electroacupuncture at different acupoints on
steroid hormones and ovarian androgen receptor expression in
polycystic ovary syndrome rats. Zhen Ci Yan Jiu. 43:543–549.
2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li X, Pishdari B, Cui P, Hu M, Yang HP,
Guo YR, Jiang HY, Feng Y, Billig H and Shao R: Regulation of
androgen receptor expression alters AMPK phosphorylation in the
endometrium: In vivo and in vitro studies in women with polycystic
ovary syndrome. Int J Biol Sci. 11:1376–1389. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Caldwell AS, Edwards MC, Desai R, Jimenez
M, Gilchrist RB, Handelsman DJ and Walters KA: Neuroendocrine
androgen action is a key extraovarian mediator in the development
of polycystic ovary syndrome. Proc Natl Acad Sci USA.
114:E3334–E3343. 2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Rajender S, Carlus SJ, Bansal SK, Negi MP,
Sadasivam N, Sadasivam MN and Thangaraj K: Androgen receptor CAG
repeats length polymorphism and the risk of polycystic ovarian
syndrome (PCOS). PLoS One. 8(e75709)2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Peng CY, Xie HJ, Guo ZF, Nie YL, Chen J,
Zhou JM and Yin J: The association between androgen receptor gene
CAG polymorphism and polycystic ovary syndrome: A case-control
study and meta-analysis. J Assist Reprod Genet. 31:1211–1219.
2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Schüring AN, Welp A, Gromoll J, Zitzmann
M, Sonntag B, Nieschlag E, Greb RR and Kiesel L: Role of the CAG
repeat polymorphism of the androgen receptor gene in polycystic
ovary syndrome (PCOS). Exp Clin Endocrinol Diabetes. 120:73–79.
2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ibáñez L, Ong KK, Mongan N, Jääskeläinen
J, Marcos MV, Hughes IA, De Zegher F and Dunger DB: Androgen
receptor gene CAG repeat polymorphism in the development of ovarian
hyperandrogenism. J Clin Endocrinol Metab. 88:3333–3338.
2003.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kim JJ, Choung SH, Choi YM, Yoon SH, Kim
SH and Moon SY: Androgen receptor gene CAG repeat polymorphism in
women with polycystic ovary syndrome. Fertil Steril. 90:2318–2323.
2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Xia Y, Che Y, Zhang X, Zhang C, Cao Y,
Wang W, Xu P, Wu X, Yi L, Gao Q, et al: Polymorphic CAG repeat in
the androgen receptor gene in polycystic ovary syndrome patients.
Mol Med Rep. 5:1330–1334. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Möhlig M, Jürgens A, Spranger J, Hoffmann
K, Weickert MO, Schlösser HW, Schill T, Brabant G, Schüring A,
Pfeiffer AF, et al: The androgen receptor CAG repeat modifies the
impact of testosterone on insulin resistance in women with
polycystic ovary syndrome. Eur J Endocrinol. 155:127–130.
2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hu DG, Hickey TE, Irvine C, Wijayakumara
DD, Lu L, Tilley WD, Selth LA and Mackenzie PI: Identification of
androgen receptor splice variant transcripts in breast cancer cell
lines and human tissues. Horm Cancer. 5:61–71. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Wang F, Pan J, Liu Y, Meng Q, Lv P, Qu F,
Ding GL, Klausen C, Leung PC, Chan HC, et al: Alternative splicing
of the androgen receptor in polycystic ovary syndrome. Proc Natl
Acad Sci USA. 112:4743–4748. 2015.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Walters KA and Handelsman DJ: Androgen
receptor splice variants and polycystic ovary syndrome: Cause or
effect? Asian J Androl. 18:442–443. 2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Wadosky KM and Koochekpour S: Androgen
receptor splice variants and prostate cancer: From bench to
bedside. Oncotarget. 8:18550–18576. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hickey TE, Irvine CM, Dvinge H, Tarulli
GA, Hanson AR, Ryan NK, Pickering MA, Birrell SN, Hu DG, Mackenzie
PI, et al: Expression of androgen receptor splice variants in
clinical breast cancers. Oncotarget. 6:44728–44744. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Nam H, Kim CH, Cha MY, Kim JM, Kang BM and
Yoo HW: Polycystic ovary syndrome woman with heterozygous androgen
receptor gene mutation who gave birth to a child with androgen
insensitivity syndrome. Obstet Gynecol Sci. 58:179–182.
2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Rotterdam ESHRE/ASRM-Sponsored PCOS
Consensus Workshop Group. Revised 2003 consensus on diagnostic
criteria and long-term health risks related to polycystic ovary
syndrome. Fertil Steril. 81:19–25. 2004.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hatch R, Rosenfield RL, Kim MH and Tredway
D: Hirsutism: Implications, etiology, and management. Am J Obstet
Gynecol. 140:815–830. 1981.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Balen AH, Laven JS, Tan SL and Dewailly D:
Ultrasound assessment of the polycystic ovary: International
consensus definitions. Hum Reprod Update. 9:505–514.
2003.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wu J, Zou Y, Luo Y, Guo JB, Liu FY, Zhou
JY, Zhang ZY, Wan L and Huang OP: Prevalence and clinical
significance of mediator complex subunit 12 mutations in 362 Han
Chinese samples with uterine leiomyoma. Oncol Lett. 14:47–54.
2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Li GX, Jiao XH and Cheng XB: Correlations
between blood uric acid and the incidence and progression of type 2
diabetes nephropathy. Eur Rev Med Pharmacol Sci. 22:506–511.
2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Adzhubei IA, Schmidt S, Peshkin L,
Ramensky VE, Gerasimova A, Bork P, Kondrashov AS and Sunyaev SR: A
method and server for predicting damaging missense mutations. Nat
Methods. 7:248–249. 2010.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Schwarz JM, Cooper DN, Schuelke M and
Seelow D: MutationTaster2: Mutation prediction for the
deep-sequencing age. Nat Methods. 11:361–362. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kumar S, Stecher G and Tamura K: MEGA7:
Molecular evolutionary genetics analysis version 7.0 for bigger
datasets. Mol Biol Evol. 33:1870–1874. 2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Walters KA, Rodriguez Paris V, Aflatounian
A and Handelsman DJ: Androgens and ovarian function: translation
from basic discovery research to clinical impact. J Endocrinol.
242:R23–R50. 2019.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Walters KA and Handelsman DJ: Role of
androgens in the ovary. Mol Cell Endocrinol. 465:36–47.
2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Baculescu N: The role of androgen receptor
activity mediated by the CAG repeat polymorphism in the
pathogenesis of PCOS. J Med Life. 6:18–25. 2013.PubMed/NCBI
|
|
35
|
Lim JJ, Lima PDA, Salehi R, Lee DR and
Tsang BK: Regulation of androgen receptor signaling by
ubiquitination during folliculogenesis and its possible
dysregulation in polycystic ovarian syndrome. Sci Rep.
7(10272)2017.PubMed/NCBI View Article : Google Scholar
|