Introduction
Intervertebral disc degeneration (IDD) is considered
to be an important contributor to low back pain. In 2010, the
lifetime prevalence of low back pain worldwide has been reported to
be >80% and low back pain associated long-term sick leave or
unemployment ensues an enormous economic burden (1-4).
Recent reports have demonstrated that several risk factors are
associated with IDD progression, including ageing and obesity
(5,6). The primary aim of clinical treatment
for IDD is primarily associated with alleviating symptoms (7), though the specific mechanism of IDD
pathogenesis and aetiology is not completely understood. There are
three types of cells that have been reported to be involved in IDD,
namely endplate chondrocytes cells, inner and outer annulus
fibrosus cells and the internal nucleus pulposus (NP) cells
(8-10).
During IDD progression, a variety of inflammatory factors and
extracellular matrix (ECM) degradation products accumulate in NP
tissues, which affect NP cell physiology and function (11).
Long non-coding RNAs (lncRNAs) are a group of RNAs
with a length of 200 nucleotides that do not encode proteins
(12). Recently, lncRNAs have been
reported to be abnormally expressed in multiple diseases, where
they participate in pathophysiological processes, including cell
proliferation, apoptosis and migration (13,14).
In particular, Pei et al (14) previously demonstrated that lncRNA
small nucleolar RNA host gene 14 promoted colorectal cancer cell
proliferation, migration and invasion whilst reducing apoptosis
through the PI3K/AKT signaling pathway. Accumulating evidence has
suggested that lncRNA prostate androgen-regulated transcript 1
(PART1) functions as a carcinogen pyrene in various diseases,
including non-small cell lung (15)
and colorectal (16) cancer. Cui
et al (8) previously
demonstrated that lncRNA MAGI2 antisense RNA 3 is downregulated in
IDD, which is associated with the reduced mediation of Fas ligand
expression levels in NP cells (8).
lncRNA PART1 has been reported to be upregulated in the central
nucleus pulposus tissue of patients with IDD (17). In addition, a recent study reported
that lncRNA PART1 promotes IDD by downregulating the miR-93/MMP2
pathway in nucleus pulposus cells (18). However, the specific mechanism
underlying the role of PART1 in IDD is not completely
understood.
MicroRNAs (miRNAs/miRs) represent a family of highly
conserved RNAs that are ~22 nucleotides in length. A number of
studies have demonstrated that miRNAs regulate gene expression by
pairing with the 3'-untranslated regions (UTR) of target mRNAs
(19-21).
miRNAs serve vital roles in numerous diseases by regulating gene
expression, cell proliferation, inflammation, apoptosis and
invasion (22-24),
such that miRNA dysregulation has been previously associated with a
number of human diseases (25). A
recent study also revealed that miR-190a-3p is involved in glioma
(26), where it was indicated that
lncRNA PART1 exerts tumor suppressive effects by sponging
miR-190a-3p, suggesting a regulatory effect of lncRNA PART1 on
miR-190a-3p function (26).
However, the role of miR-190a-3p in IDD progression is not
completely understood and whether lncRNA PART1 can affect IDD by
regulating miR-190a-3p remains unclear.
Therefore, present study aimed to investigate the
roles of lncRNA PART1 in in vitro IDD models. In
vitro IDD models were constructed by stimulating NP cells with
10 ng/ml LPS for 24 h, after which the effects of PART1-short
hairpin (sh)RNA on cell viability, cell apoptosis, the inflammatory
response and ECM degradation were determined.
Materials and methods
Cell culture and LPS stimulation
Human NP cells (cat no. CP-H097; Procell Life
Science & Technology Co., Ltd.) were cultured in DMEM/F12
(Gibco; Thermo Fisher Scientific, Inc.) supplemented with 10% FBS
(Gibco; Thermo Fisher Scientific, Inc.) and 1%
penicillin/streptomycin at 37˚C in an incubator with 5%
CO2. Human NP cells were stimulated with 10 ng/ml LPS
(Sigma-Aldrich; Merck KGaA) at 37˚C for 24 h to construct in
vitro IDD models.
Dual luciferase reporter assay
A previous study has identified a binding site on
lncRNA PART1 for miR-190a-3p (26).
Therefore, in the present study, Starbase version 2.0 (http://starbase.sysu.edu.cn/) was used to verify the
potential interaction between lncRNA PART1 and miR-190a-3p, which
was confirmed using Dual-luciferase reporter assay. The lncRNA
PART1 3'-UTR containing the potential miR-190a-3p binding site and
the mutated version of the target site were synthesized through
reverse transcription with a Transcriptor First Strand cDNA
Synthesis kit (Roche Molecular Systems). The conditions were as
follows: 5 min at 25˚C followed by 60 min at 42˚C. and cloned into
the pGL-luciferase reporter control vector (Promega Corporation) to
generate the wild-type PART1 plasmid (PART1-wt) or PART1 mutated
plasmid (PART1-mut). Subsequently, NP cells (5x104 per
well) were co-transfected with 100 nM mimic control
(5'-UCACAACCUCCUAGAAAGAGUAGA-3') or 100 nM miR-190a-3p mimic
(5'-UGAUAUGUUUGAUAUAUUAGGU-3'; Guangzhou RiboBio Co., Ltd.) and 1
ng PART1-wt or 1 ng PART1-mut using Lipofectamine® 2000
(Invitrogen; Thermo Fisher Scientific, Inc.). At 48 h
post-transfection, luciferase activity was measured using the
Dual-Luciferase Reporter Assay System (Promega Corporation)
following the manufacturer's protocols. Firefly luciferase activity
was normalized to that of Renilla luciferase activity.
Cell transfection
Silencing of PART1 was performed by cloning short
hairpin RNA (shRNA) oligonucleotides into the pCMV vector (Shanghai
GenePharma Co., Ltd.). Control-shRNA (5'-AAGGCUAUGAAGAGAUAC-3';
Shanghai GenePharma Co., Ltd.; 1 µg), PART1-shRNA
(5'-GAAAACGCAGCTACACCTGG-3'; Shanghai GenePharma Co., Ltd.; 1 µg),
50 nM inhibitor control (5'-UCACAACCUCCUAGAAAGAGUAGA-3') and 50 nM
miR-190a-3p inhibitor (5'-ACCUAAUAUAUCAAACAUAUCA-3') were all
synthesized by Guangzhou RiboBio Co., Ltd. NP cells
(5x104 cells per well) were transfected using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.) according to the manufacturer's protocol.
Subsequent experiments were performed 24 h after transfection.
ELISA
NP cells (5x104 cells per well) were
cultured at 37˚C and transfected with control-shRNA, PART1-shRNA,
inhibitor control or miR-190a-3p inhibitor for 24 h. Following
stimulation with 10 ng/ml LPS at 37˚C for 24 h, the levels of TNF-α
(cat. no PT518), IL-1β (cat. no. PI305) and IL-6 (cat. no. PI330)
in the cell culture supernatant (centrifugation: 500 x g; 5 min;
4˚C) were quantitatively detected using ELISA kits (Beyotime
Institute of Biotechnology) according to the manufacturer's
protocol. Cells were divided into the following six groups: i)
Control; ii) LPS; iii) LPS + control-shRNA; iv) LPS + PART1-shRNA;
v) LPS + PART1-shRNA + inhibitor control; and vi) LPS + PART1-shRNA
+ miR-190a-3p inhibitor. The optical density (OD) value of each
well at was measured at a wavelength of 450 nm using a Multiskan™
Spectrum spectrophotometer (Thermo Fisher Scientific, Inc.).
MTT assay
Cell viability was assessed by performing an MTT
assay. NP cells (5x104 cells per well) were cultured at
37˚C and transfected with control-shRNA, PART1-shRNA, inhibitor
control or miR-190a-3p inhibitor for 24 h. Subsequently, cells were
stimulated with 10 ng/ml LPS at 37˚C for 24 h. Following treatment,
cells were incubated with 10 µl MTT solution (5 mg/ml; Beyotime
Institute of Biotechnology) at 37˚C for 4 h. DMSO was used to
dissolve the formazan crystals. OD values were measured at a
wavelength of 570 nm using a microplate reader (BioTek Instruments,
Inc.).
Flow cytometry analysis
NP cell apoptosis was evaluated by performing flow
cytometry. Following transfection and LPS stimulation, cells were
assessed using an Annexin V-FITC/PI Apoptosis Detection kit (BD
Biosciences) according to the manufacturer's protocol. Brifely, a
total of 1x106 NP cells were harvested and stained with
5 µl Annexin V-FITC and 5 µl propidium iodide at room temperature
for 15 min in the dark. Apoptotic cells (early + late apoptosis:
Quadrants 2 and 3) were analyzed using a BD FACSCalibur™ flow
cytometer (Becton-Dickinson and Company) with the CellQuest
software (version 5.1; BD Biosciences).
Reverse transcription-quantitative PCR
(RT-qPCR)
Total RNA was isolated from NP cells using
TRIzol® reagent (Invitrogen; Thermo Fisher Scientific,
Inc.) according to the manufacturer's protocol. Total RNA was
reverse transcribed into cDNA using the PrimeScript™ RT reagent kit
(Takara Bio, Inc.) according to the manufacturer's protocol.
Temperature protocol used for RT were 25˚C for 5 min, 42˚C for 60
min and 80˚C for 2 min. Subsequently, qPCR was performed using
using SYBR Premix Ex Taq™ II (TliRNaseH Plus) kit (Takara Bio,
Inc.) according to the manufacturer's protocol. The thermocycling
conditions were as follows: Initial denaturation for 5 min at 95˚C;
followed by 37 cycles of denaturation at 94˚C for 1 min, annealing
at 60˚C for 1 min and extension at 72˚C for 1 min, followed by a
final extension step at 72˚C for 10 min. mRNA and miRNA expression
levels were quantified using the 2-ΔΔCq method (27) and normalized to those of the
internal reference genes GAPDH and U6, respectively. Primer
sequences were listed as following: lncRNA PART1 forward,
5'-AAGGCCGTGTCAGAACTCAA-3' and reverse, 5'-GTTTTCCATCTCAGCCTGGA-3';
miR-190a-3p forward, 5'-ACACTCCAACAAACTATATATCGGGTCTC-3' and
reverse, 5'-TGGTGATCTGCAGTC-3'; aggrecan forward,
5'-CTACCAGTGGATCGGCCTGAA-3' and reverse,
5'-CGTGCCAGATCATCACCACA-3'; collagen type II forward,
5'-GGCAATAGCAGGTTCACGTACA-3' and reverse,
5'-CGATAACAGTCTTGCCCCACTT-3'; GAPDH forward,
5'-GTCTCCTCTGACTTCAACAGCG-3' and reverse,
5'-ACCACCCTGTTGCTGTAGCCAA-3' and U6 forward,
5'-CTCGCTTCGGCAGCACATATACT-3' and reverse,
5'-ACGCTTCACGAATTTGCGTGTC-3'.
Western blotting
Total protein was extracted from cells using RIPA
lysis buffer (Beyotime Institute of Biotechnology). The
bicinchoninic acid protein assay kit (cat. no. BCA1-1KT;
Sigma-Aldrich; Merck KGaA) was used to determine protein
concentration. Proteins (30 mg per lane) were then separated by 10%
SDS-PAGE and transferred onto PVDF membranes, which were blocked
with 5% skim milk in PBS with 0.1% Tween-20 at room temperature for
1.5 h. The membranes were incubated with primary antibodies
targeted against the following proteins overnight at 4˚C: Cleaved
caspase-3 (cat. no. ab32042; 1:1,000; Abcam), pro-caspase-3 (cat.
no. ab32499; 1:1,000; Abcam), aggrecan (cat. no. ab36861; 1:1,000;
Abcam), collagen type II (cat. no. ab188570; 1:1,000; Abcam) and
GAPDH (cat. no. ab9485; 1:1,000; Abcam). Following washing four
times with TBST (0.1% Tween-20), the membranes were incubated with
horseradish peroxidase-conjugated secondary antibodies (cat. no.
ab7090; 1:2,000; Abcam) at room temperature for 1 h. Proteins were
visualized using Pierce™ ECL Western Blotting Substrate (Pierce;
Thermo Fisher Scientific, Inc.). Band densities were quantified
using the Gel-Pro Analyzer densitometry software (version 6.3;
Media Cybernetics, Inc.).
Statistical analysis
Statistical analyzes were performed using SPSS
software (version 20.0; IBM Corp.). Data are presented as the mean
± SD from three independent experiments. Comparisons among groups
were analyzed using one-way ANOVA with Tukey's post hoc test and
the unpaired Student's t-test. P<0.05 was considered to indicate
a statistically significant difference.
Results
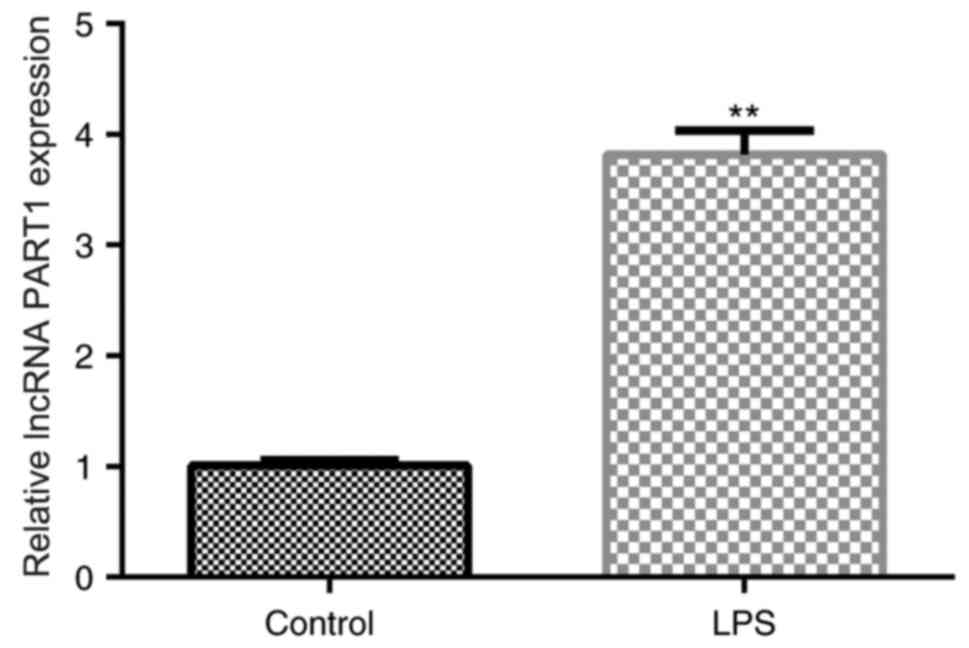
lncRNA PART1 is upregulated in
LPS-stimulated human NP cells
Previous studies have revealed that LPS promoted
inflammatory factor production and ECM degeneration by NP cells
(28,29). Therefore, LPS was used as a
stimulating factor to generate in vitro IDD models in the
present study. To determine the biological roles of lncRNA PART1 in
IDD, lncRNA PART1 expression was assessed via RT-qPCR in NP cells.
lncRNA PART1 expression levels in LPS-stimulated human NP cells
were significantly higher compared those in the untreated cells of
the control group (Fig. 1). The
results suggest that lncRNA PART1 participates in the development
of IDD.
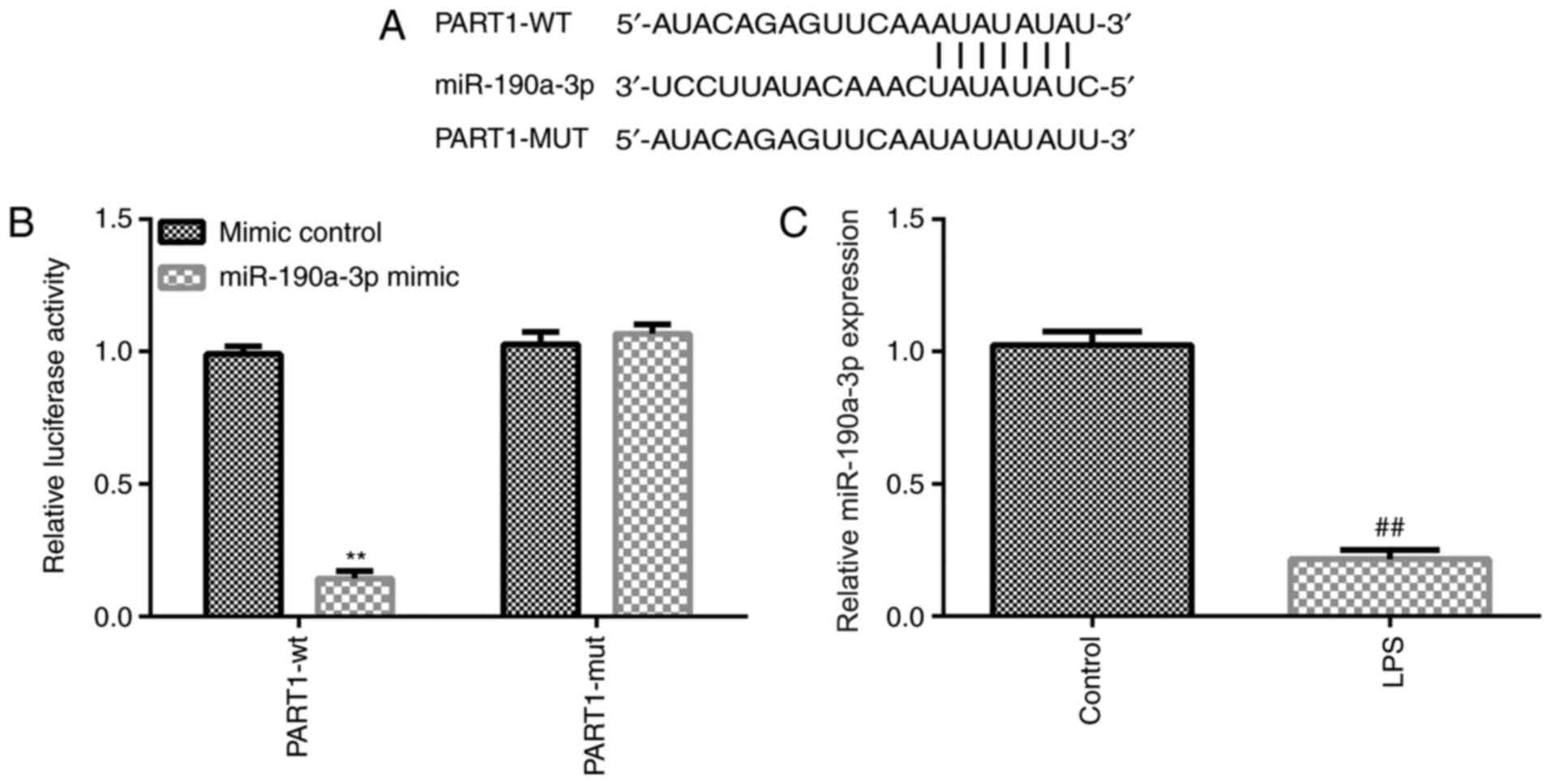
miR-190a-3p is a target of lncRNA
PART1 that is downregulated in LPS-stimulated human NP cells
To identify the mechanism underlying the role of
lncRNA PART1 in IDD development, potential targets of PART1 were
predicted using bioinformatics analysis. Starbase version 2.0
analysis results indicated that miR-190a-3p was a candidate
interaction partner for lncRNA PART1 (Fig. 2A). The dual luciferase reporter
assay was performed to verify if miR-190a-3p directly targeted
lncRNA PART1. The results indicated that PART1-wt luciferase
activity was significantly decreased compared with that in the
control group, whereas the luciferase activity of PART1-mut was not
significantly altered (Fig. 2B),
suggesting that miR-190a-3p was directly targeted by lncRNA PART1.
To further clarify the association between miR-190a-3p and lncRNA
PART1, miR-190a-3p expression levels were assessed using RT-qPCR.
The results indicated that miR-190a-3p expression was significantly
decreased in NP cells following LPS treatment (Fig. 2C).
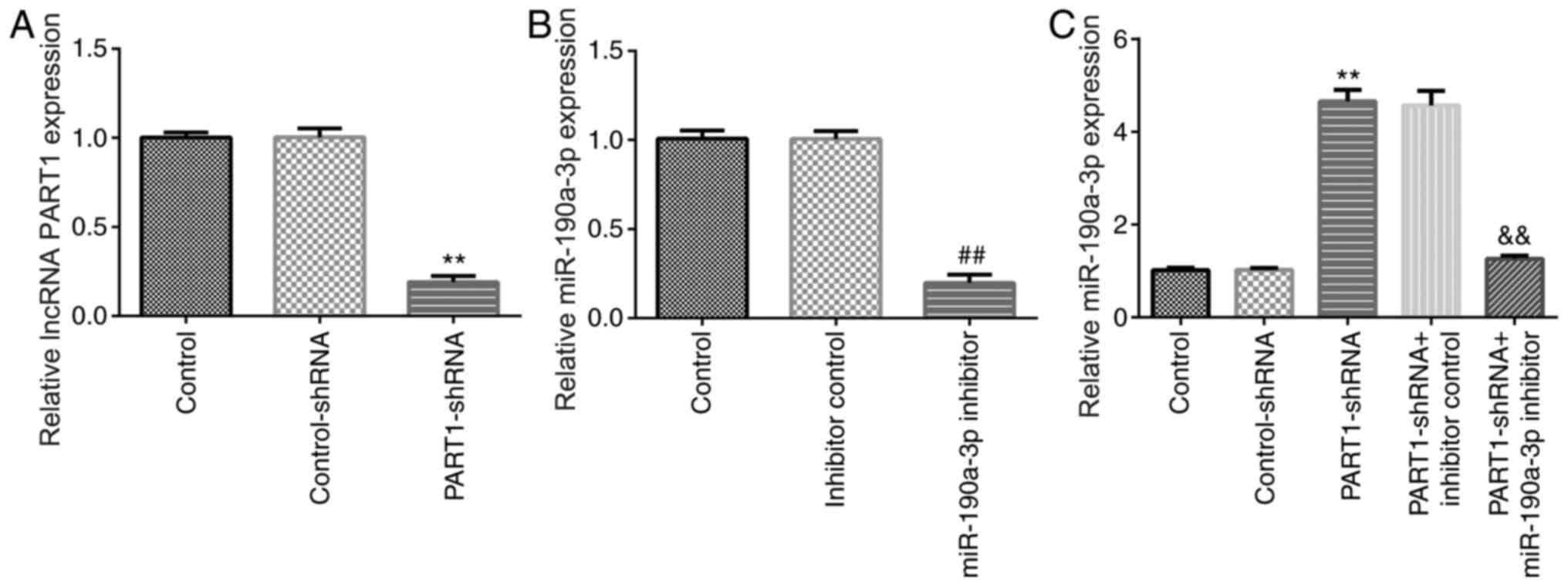
PART1-shRNA promotes NP cell viability
and decreases apoptosis by regulating miR-190a-3p expression
To explore whether miR-190a-3p affected the effects
of PART1-shRNA on NP cell functions, NP cells were first
transfected with control-shRNA, PART1-shRNA, inhibitor control or
miR-190a-3p inhibitor for 24 h. The RT-qPCR results indicated that
PART1 expression was significantly downregulated in NP cells
following PART1-shRNA transfection compared with those transfected
with control-shRNA (Fig. 3A). In
addition, the expression of miR-190a-3p was significantly reduced
in NP cells transfected with miR-190a-3p inhibitor compared with
those transfected with the inhibitor control (Fig. 3B). PART1 knockdown significantly
increased miR-190a-3p expression, which was significantly reversed
by transfection with the miR-190a-3p inhibitor (Fig. 3C). The results suggest that lncRNA
PART1 negatively regulated miR-190a-3p in NP cells.
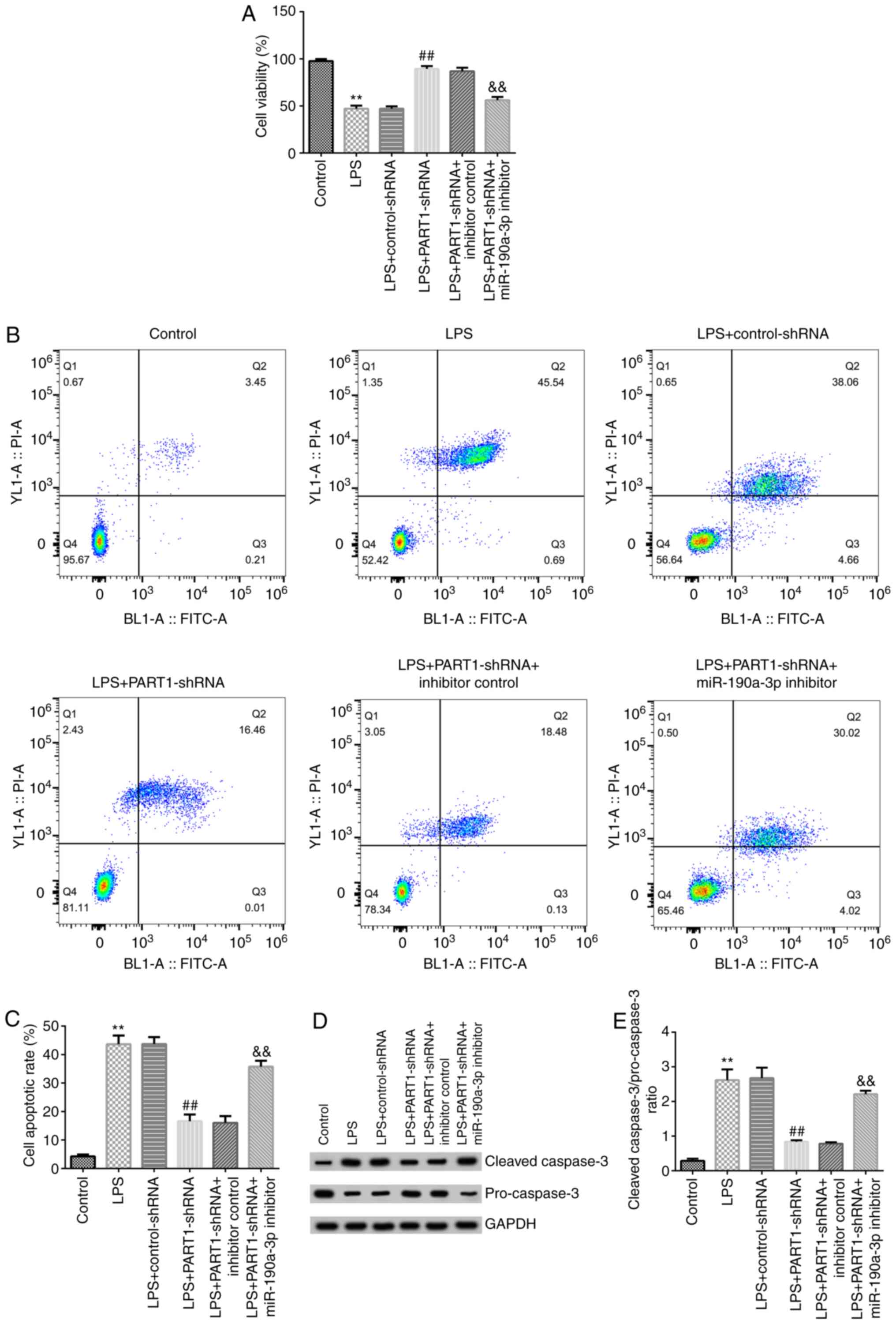
To further investigate if PART1 directly regulated
miR-190a-3p expression, NP cells were transfected with
control-shRNA, PART1-shRNA, inhibitor control or miR-190a-3p
inhibitor for 24 h, followed by stimulation with 10 ng/ml LPS. MTT
assay and flow cytometry were performed to determine cell viability
and apoptosis, respectively. The results indicated that PART1-shRNA
transfection significantly increased cell viability in
LPS-stimulated NP cells, which was significantly reversed in cells
in the LPS + PART1-shRNA + miR-190a-3p inhibitor group (Fig. 4A). Additionally, PART1-shRNA
transfection significantly inhibited LPS-induced cell apoptosis,
which was significantly reversed in cells in the LPS + PART1-shRNA
+ miR-190a-3p inhibitor group (Fig.
4B and C). Subsequently,
expression levels of apoptotic-related proteins were measured using
western blotting. The results indicated that cleaved-caspase-3
expression levels were markedly decreased whereas pro-caspase-3
expression levels were enhanced, such that the
cleaved-Caspase-3/pro-Caspase-3 ratio was significantly reduced in
cells in the LPS + PART1-shRNA group compared with that in cells in
the LPS + control-shRNA group (Fig.
4D and E). By contrast, in the
PART1-shRNA + miR-190a-3p inhibitor co-transfected cells that were
treated with LPS, the cleaved-Caspase-3/pro-Caspase-3 were
significantly higher compared with those in cells in the LPS +
PART-shRNA + inhibitor control group (Fig. 4D and E). These results suggest that miR-190a-3p
inhibitor reversed PART1-shRNA-mediated regulation of cell
viability and apoptosis induced in LPS-stimulated NP cells.
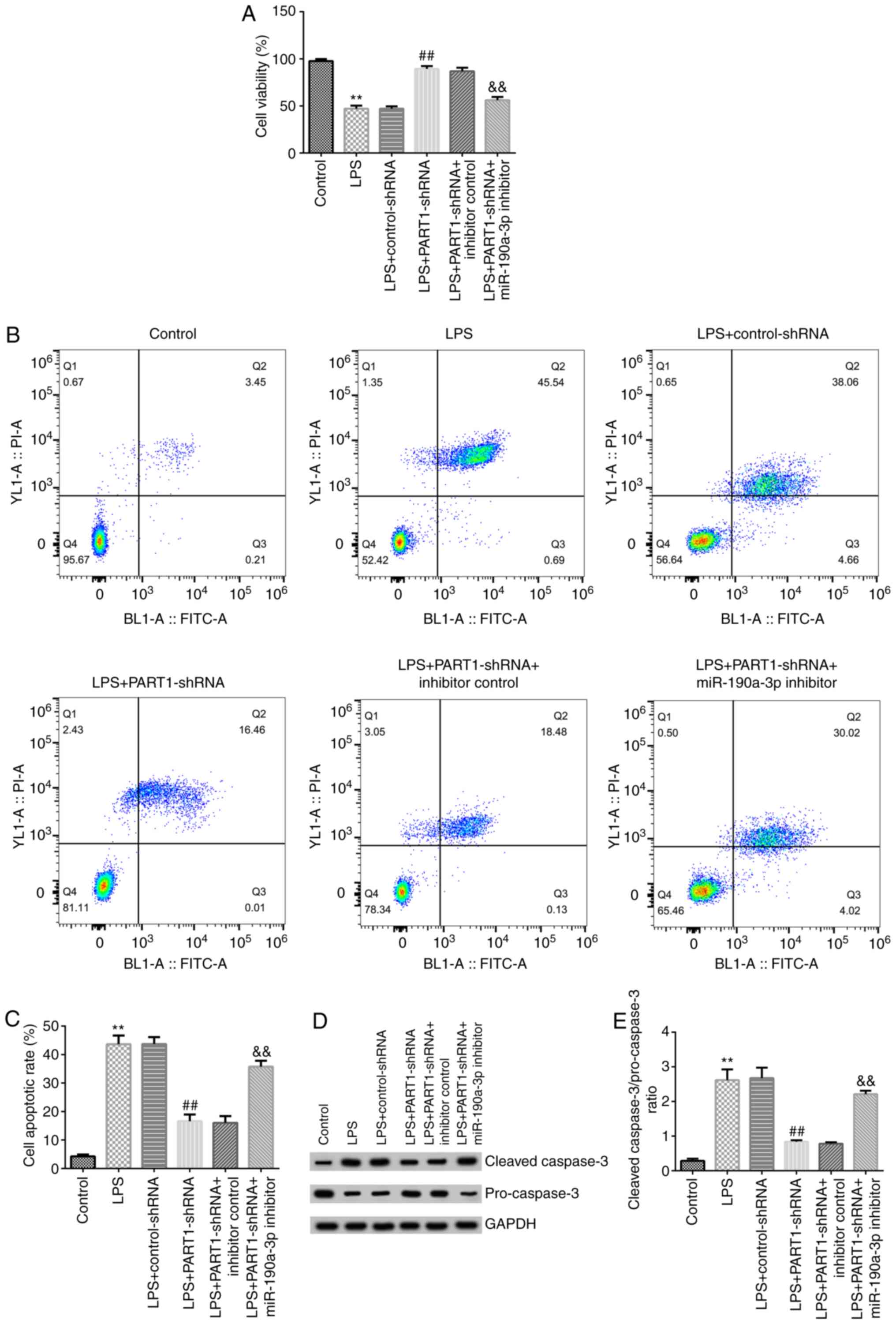 | Figure 4miR-190a-3p inhibitor reverses the
effects of PART1-shRNA on NP cell viability and apoptosis. NP cells
were transfected with control-shRNA, PART1-shRNA, inhibitor control
or miR-190a-3p inhibitor for 24 h before being treated with 10
ng/ml LPS. (A) MTT assay was performed to measure NP cell
viability. (B) NP cell apoptosis was assessed using flow cytometry
(C) and quantified. (D) Expression levels of apoptosis-related
proteins cleaved caspase-3 (molecular weight, 17 kDa) and
pro-caspase-3 (molecular weight, 35 kDa), and the loading control
GAPDH (molecular weight, 37 kDa) in NP cells were measured by
western blotting. (E) The ratio of cleaved caspase-3/pro-caspase-3
was quantified. Data are presented as the mean ± SD.
**P<0.01 vs. control; ##P<0.01 vs. LPS
+ control-shRNA; &&P<0.01 vs. LPS +
PART1-shRNA + inhibitor control. miR, microRNA; PART1, prostate
androgen-regulated transcript 1; shRNA, short hairpin RNA; NP,
nucleus pulposus; LPS, lipopolysaccharide. |
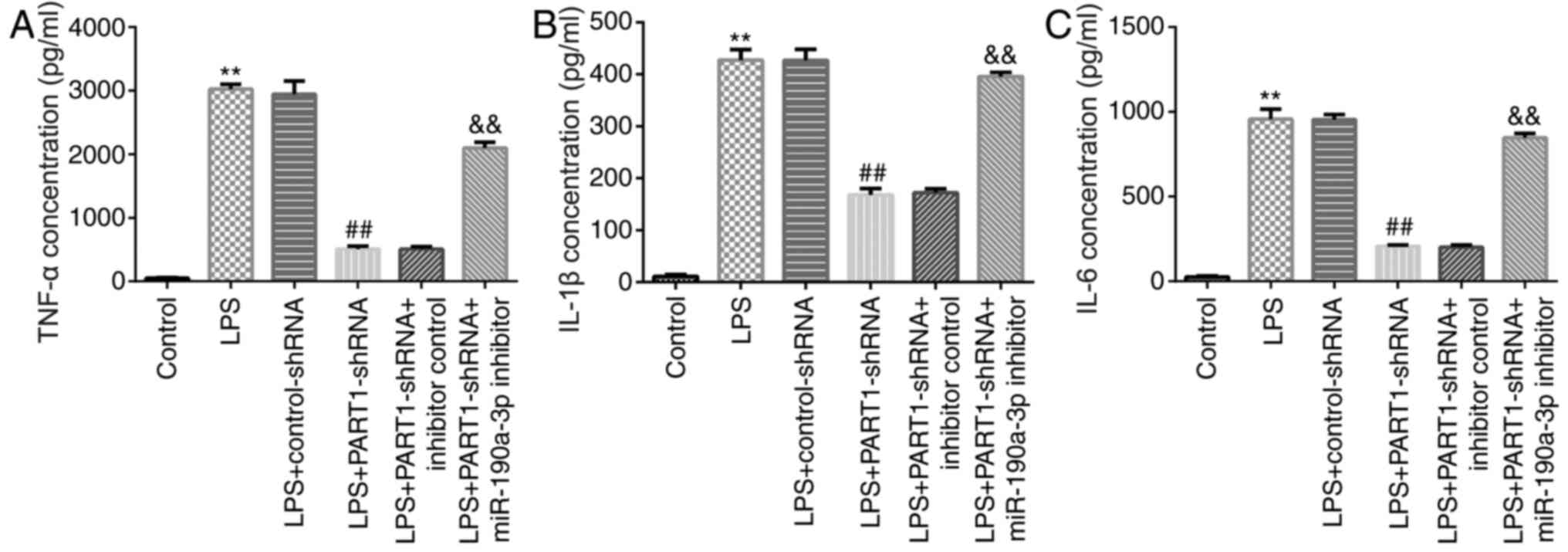
miR-190a-3p inhibitor reverses the
effects of PART1-shRNA on inflammatory factor secretion in
LPS-stimulated NP cells
The possible role of PART1 in inflammatory factor
secretion was next investigated by knocking down PART1 expression
in LPS-stimulated NP cells. The results indicated that PART1-shRNA
transfection reduced TNF-α, IL-1β and IL-6 secretion compared with
cells in LPS + control-shRNA group (Fig. 5). However, miR-190a-3p inhibitor
co-transfection significantly increased TNF-α, IL-1β and IL-6
secretion compared with that in cells in the LPS + PART1-shRNA +
inhibitor control group (Fig. 5).
This suggest that LPS and PART1-mediated inflammatory response may
be associated with the development of IDD.
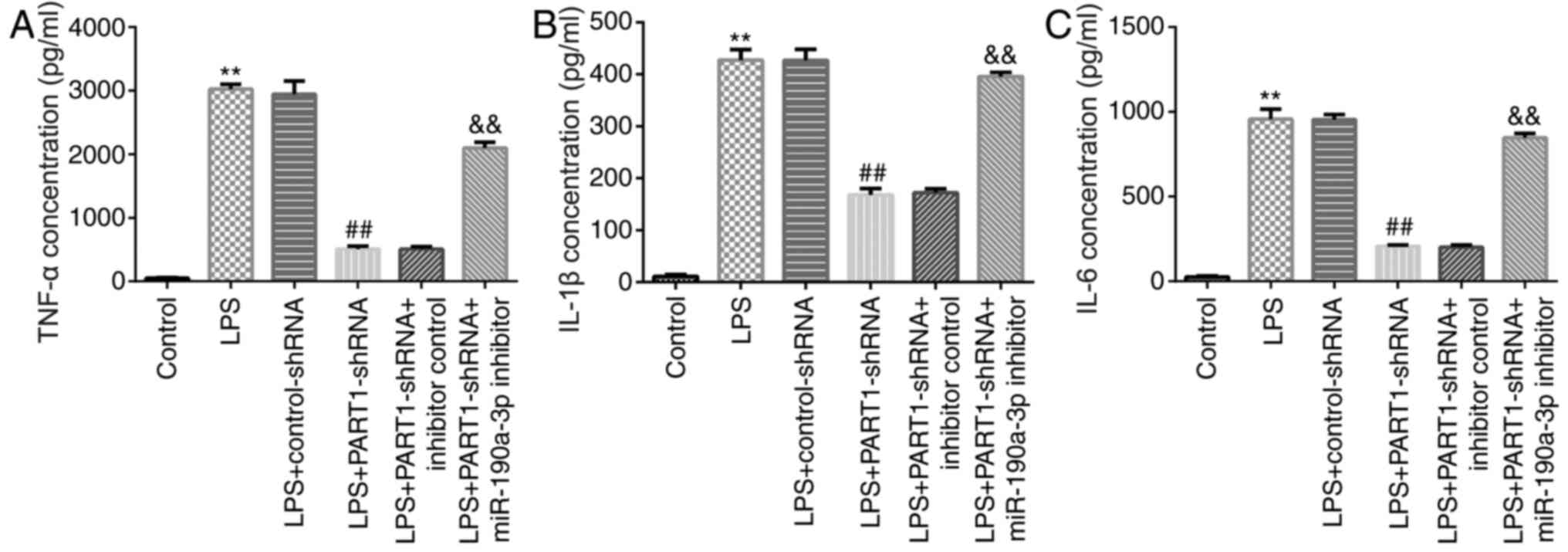 | Figure 5Transfection with miR-190a-3p
inhibitor enhances inflammatory cytokine secretion in NP cells. NP
cells were transfected with control-shRNA, PART1-shRNA, inhibitor
control or miR-190a-3p inhibitor for 24 h before being treated with
10 ng/ml LPS. Cells were divided into the following six groups: i)
Control; ii) LPS; iii) LPS + control-shRNA; iv) LPS + PART1-shRNA;
v) LPS + PART1-shRNA + inhibitor control; and vi) LPS + PART1-shRNA
+ miR-190a-3p inhibitor. Concentrations of inflammatory factors (A)
TNF-α, (B) IL-1β and (C) IL-6 were measured in the cell culture
supernatants by performing ELISA. Data are presented as the mean ±
SD. **P<0.01 vs. control; ##P<0.01 vs.
LPS + control-shRNA; &&P<0.01 vs. LPS +
PART1-shRNA + inhibitor control. miR, microRNA; NP, nucleus
pulposus; shRNA, short hairpin RNA; LPS, lipopolysaccharide; PART1,
prostate androgen-regulated transcript 1; IL, interleukin; TNF-α,
tumor necrosis factor-α. |
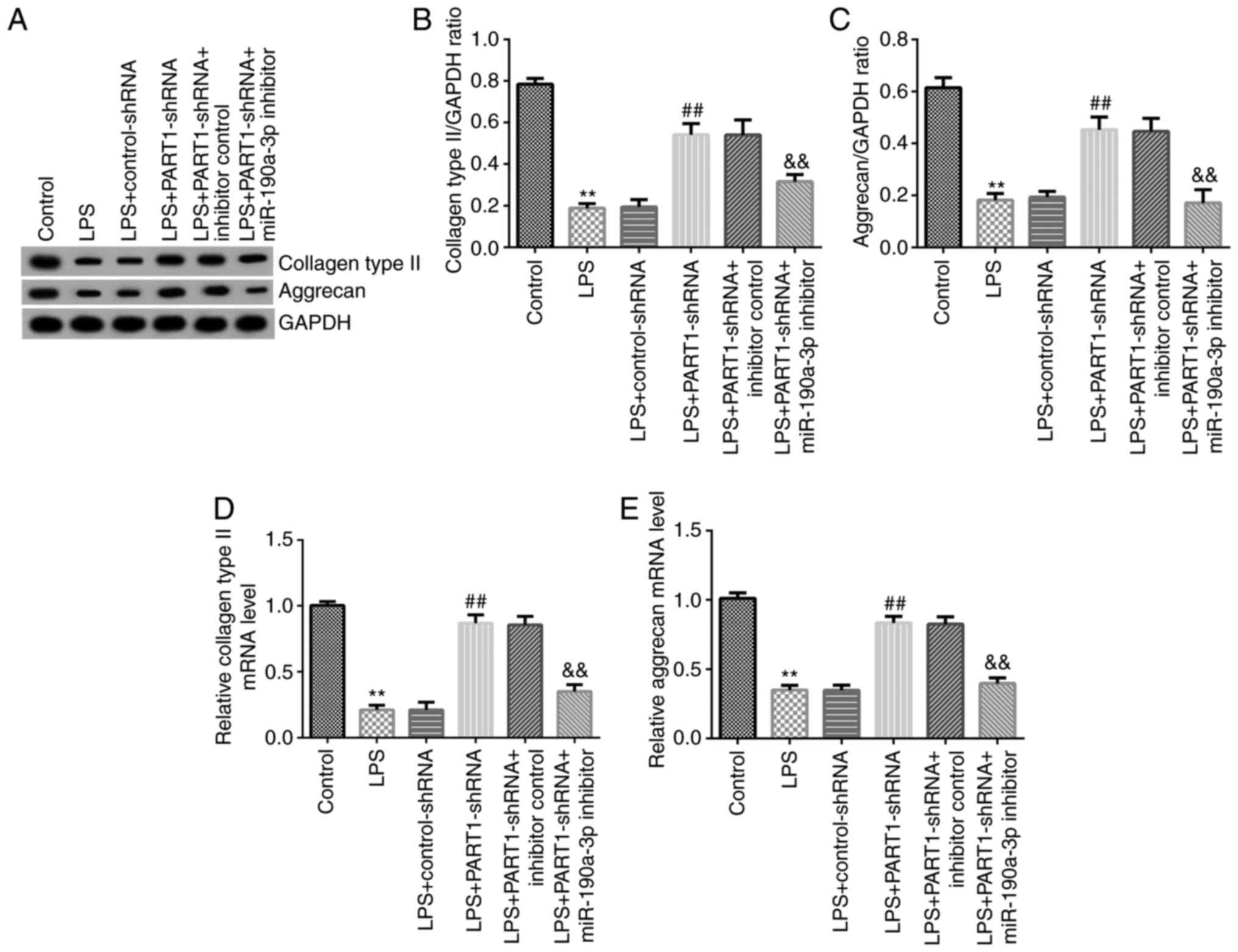
miR-190a-3p inhibitor reverses the
effects of PART1-shRNA on ECM degradation in LPS-stimulated NP
cells
ECM degradation is also considered to be a vital
element in regulating NP cell functions (30). Therefore, the levels of key ECM
components in LPS-stimulated NP cells were subsequently assessed.
The western blotting results suggested that PART1-shRNA
transfection significantly increased aggrecan and collagen type II
expression in LPS-stimulated NP cells, which was significantly
reversed following miR-190a-3p inhibitor co-transfection alongside
PART-shRNA (Fig. 6). Similarly,
RT-qPCR data indicated that aggrecan and collagen type II
expression levels in cells in the LPS + PART1-shRNA group were also
significantly increased, which were significantly reversed by
miR-190a-3p knockdown (Fig. 6A-E).
In conclusion, these observations suggest that PART1 regulates ECM
degradation by regulating miR-190a-3p.
Discussion
IDD is a musculoskeletal degeneration disease that
is characterized by prolonged low back pain, chronic inflammation
and lumbar dysfunction (1). IDD
seriously reduces the quality of life of patients, where effective
therapeutic strategies for IDD remain limited (31). Therefore, in the present study, a
novel target and its underlying mechanisms in IDD pathogenesis were
investigated. LPS has been widely applied to induce inflammation in
in vitro diseases models (32-34).
Previous studies have revealed that LPS could significantly
stimulate inflammatory in NP cells (29,35).
Zhang et al previously (35)
demonstrated that downregulation of miR-222 suppressed LPS-induced
inflammation and apoptosis in human NP cells. Therefore, LPS was
used to induce IDD in vitro using a NP cell model in the
present study and to investigate the underlying physiological
effects of LPS.
lncRNAs have been documented to exert important
roles in the progression of various diseases (36). In particular, lncRNA PART1 is a
newly discovered lncRNA that has been previously reported to serve
as either an oncogene or suppressor gene in tumors (14,26,37).
Accumulating studies have suggested that aberrantly expressed
lncRNA PART1 is associated with the progression of various
diseases, including IDD (36,17,18).
Lou et al (38) revealed
that lncRNA PART1 promoted the development of colorectal cancer via
the miR-150-5p/leucine rich α2-glycoprotein 1 axis. However, the
specific mechanism underlying lncRNA PART1 in IDD is not completely
understood. In the present study, the level of lncRNA PART1
expression was detected in 10 ng/ml LPS-stimulated NP cells.
Previous reports have demonstrated that PART1 expression was
upregulated in patients with IDD (17,18).
In line with previous studies, the results of the present study
indicated that the level of lncRNA PART1 was higher in
LPS-stimulated NP cells compared with that in normal untreated
cells.
lncRNAs regulate gene transcription activity by
targeting miRNAs and have been reported to regulate physiological
processes downstream, including cell viability, differentiation,
apoptosis and carcinogenesis (39,40).
As another type of non-coding RNA, miRNAs regulate the translation
of target mRNAs by interacting with their 3'UTR (19-21).
Numerous reports have confirmed that lncRNAs are miRNA sponges that
indirectly affect the functions of mRNAs in multiple diseases
(41,42). Bioinformatics databases and
dual-luciferase reporter assays were performed in the present study
to predict any potential lncRNA PART1 target genes. Results from
the present study indicated that lncRNA PART1 directly targeted
miR-190a-3p to negatively regulate miR-190a-3p expression. In
addition, miR-190a-3p levels in LPS-stimulated NP cells were lower
compared with those in control cells, suggesting that miR-190a-3p
was involved in IDD progression.
Previous studies have indicated that the aberrant
regulation of lncRNAs was closely associated with the pathological
processes of IDD (17,43). Mi et al (43) previously reported that lncRNA Fas
associated factor 1 promotes IDD by targeting the ERK signaling
pathway. NP cell apoptosis is an important cause of IDD (44). Therefore, the present study analyzed
the effect of lncRNA PART1 on NP cell viability and apoptosis, in
addition to determining the levels of ECM components aggrecan and
collagen type II in LPS-stimulated NP cells by western blotting and
RT-qPCR. The results suggested that LPS suppressed NP cell
viability and induced cell apoptosis. Caspase-3, one of the most
important members of the caspase family, serves an important role
in the enzymatic cleavage of various important substrates to
activate cell death programs (45).
Cleaved caspase-3 has been widely applied as a marker of apoptotic
cells (46). Therefore, cleaved
caspase-3 and pro-caspase-3 levels were determined to measure cell
apoptosis. The results suggested that after LPS-stimulaton, the
expression levels of cleaved caspase-3 were increased whereas those
of pro-caspase-3 were decreased in NP cells. However, lncRNA PART1
transfection promoted cell proliferation and reduced the number of
apoptotic cells, which was in turn reversed by co-transfection with
the miR-190a-3p inhibitor.
A number of reports have previously revealed that
the inflammatory response and ECM degradation are the main
characteristics of IDD, which are associated with the development
of IDD (11-13).
Inflammation is the leading cause of IDD development, with various
inflammatory factors, including IL-6, TNF-α and IL-1β, being found
to be upregulated in patients with IDD (47). Therefore, to explore whether lncRNA
PART1 could affect IDD by regulating the inflammatory response and
ECM degradation, the secretion of inflammatory factors and ECM
degradation by NP cells were measured in the present study. The
results of the present study were consistent with previous studies
(29,35), suggesting that LPS induced
inflammatory factor release from NP cells. By contrast, PART1-shRNA
transfection alleviated LPS-induced inflammatory cytokine
secretion, in a manner that could be reversed by co-transfection
with the miR-190a-3p inhibitor. Aggrecan and collagen type II
levels were also significantly increased in those in the LPS +
PART1-shRNA group compared with those in the LPS + control-shRNA
group, which were also reversed by co-transfection with the
miR-190a-3p inhibitor. In conclusion, these results indicated that
PART1 knockdown inhibited ECM degradation, reduced inflammatory
factor secretion and inhibited cell apoptosis in NP cells by
regulating miR-190a-3p. However, in the present study, the
expression of aggrecan and collagen type II was determined using
only western blot assay and RT-qPCR, whilst the levels of
inflammatory factors was assessed using only ELISA.
Immunofluorescence staining of these indicators would drastically
support these observations, which serves as a limitation of the
present study.
To the best of our knowledge, the present study
revealed the protective effects of PART1-shRNA on LPS-stimulated NP
cells for the first time, as demonstrated by the increased cell
viability, reduced cell apoptosis, inhibition of the inflammatory
response and reduced ECM degradation. In addition, all of the
aforementioned effects downstream of PART-shRNA were mediated in
manners that were at least in part dependent on miR-190a-3p. The
results of the present study suggest a potential therapeutic target
for IDD treatment.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZZha conceived and designed the current study,
acquired, analyzed and interpreted the data, and prepared the
manuscript. YH acquired and analyzed the data, and prepared the
manuscript. ZZho, PZ and JH performed the experiments. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hoy D, March L, Brooks P, Blyth F, Woolf
A, Bain C, Williams G, Smith E, Vos T, Barendregt J, et al: The
global burden of low back pain: Estimates from the global burden of
disease 2010 study. Ann Rheum Dis. 73:968–974. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Walker BF: The prevalence of low back
pain: A systematic review of the literature from 1966 to 1998. J
Spinal Disord. 13:205–217. 2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Steenstra IA, Verbeek JH, Heymans MW and
Bongers PM: Prognostic factors for duration of sick leave in
patients sick listed with acute low back pain: A systematic review
of the literature. Occup Environ Med. 62:851–860. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Munir S, Rade M, Määttä JH, Freidin MB and
Williams FMK: Intervertebral disc biology: Genetic basis of disc
degeneration. Curr Mol Biol Rep. 4:143–150. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wu H, Shang Y, Yu J, Zeng X, Lin J, Tu M,
Cheang LH and Zhang J: Regenerative potential of human nucleus
pulposus resident stem/progenitor cells declines with ageing and
intervertebral disc degeneration. Int J Mol Med. 42:2193–2202.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Segar AH, Fairbank J and Urban J: Leptin
and the intervertebral disc: A biochemical link exists between
obesity, intervertebral disc degeneration and low back pain-an in
vitro study in a bovine model. Eur Spine J. 28:214–223.
2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kadow T, Sowa G, Vo N and Kang JD:
Molecular basis of intervertebral disc degeneration and
herniations: What are the important translational questions? Clin
Orthop Relat Res. 473:1903–1912. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cui S, Liu Z, Tang B, Wang Z and Li B:
lncRNA MAGI2-AS3 is down-regulated in intervertebral disc
degeneration and participates in the regulation of FasL expression
in nucleus pulposus cells. BMC Musculoskelet Disord.
21(149)2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gao C, Ning B, Sang C and Zhang Y:
Rapamycin prevents the intervertebral disc degeneration via
inhibiting differentiation and senescence of annulus fibrosus
cells. Aging (Albany NY). 10:131–143. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jiang C, Guo Q, Jin Y, Xu JJ, Sun ZM, Zhu
DC, Lin JH, Tian NF, Sun LJ, Zhang XL and Wu YS: Inhibition of EZH2
ameliorates cartilage endplate degeneration and attenuates the
progression of intervertebral disc degeneration via demethylation
of Sox-9. EBioMedicine. 48:619–629. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tan Y, Yao X, Dai Z, Wang Y and Lv G: Bone
morphogenetic protein 2 alleviated intervertebral disc degeneration
through mediating the degradation of ECM and apoptosis of nucleus
pulposus cells via the PI3K/Akt pathway. Int J Mol Med. 43:583–592.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liu J, Liu ZX, Wu QN, Lu YX, Wong CW, Miao
L, Wang Y, Wang Z, Jin Y, He MM, et al: Long noncoding RNA AGPG
regulates PFKFB3-mediated tumor glycolytic reprogramming. Nat
Commun. 11(1507)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zou X, Guo ZH, Li Q and Wang PS: Long
noncoding RNA LINC00460 modulates MMP-9 to promote cell
proliferation, invasion and apoptosis by targeting miR-539 in
papillary thyroid cancer. Cancer Manag Res. 12:199–207.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Pei Q, Liu GS, Li HP, Zhang Y, Xu XC, Gao
H, Zhang W and Li T: Long noncoding RNA SNHG14 accelerates cell
proliferation, migration, invasion and suppresses apoptosis in
colorectal cancer cells by targeting miR-944/KRAS axis through
PI3K/AKT pathway. Eur Rev Med Pharmacol Sci. 23:9871–9881.
2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zhu D, Yu Y, Wang W, Wu K, Liu D, Yang Y,
Zhang C, Qi Y and Zhao S: Long noncoding RNA PART1 promotes
progression of non-small cell lung cancer cells via JAK-STAT
signaling pathway. Cancer Med. 8:6064–6081. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zhou T, Wu L, Ma N, Tang F, Zong Z and
Chen S: lncRNA PART1 regulates colorectal cancer via targeting
miR-150-5p/miR-520h/CTNNB1 and activating Wnt/β-catenin pathway.
Int J Biochem Cell Biol. 118(105637)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhao B, Lu M, Wang D, Li H and He X:
Genome-wide identification of long noncoding RNAs in human
intervertebral disc degeneration by RNA sequencing. Biomed Res Int.
2016(3684875)2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Gao D, Hao L and Zhao Z: Long non-coding
RNA PART1 promotes intervertebral disc degeneration through
regulating the miR-93/MMP2 pathway in nucleus pulposus cells. Int J
Mol Med. 46:289–299. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Attia H, Abdelrahman AH, Ibrahim MH, Eid
MM, Eid OM, Sallam MT, El Gammal MM and Kamel MM: Altered
expression of microRNAs in the bone marrow of multiple myeloma
patients and their relationship to cytogenetic aberrations. Curr
Pharm Biotechnol: Mar 20, 2020 (Epub ahead of print).
|
|
20
|
Lu TX and Rothenberg ME: MicroRNA. J
Allergy Clin Immunol. 141:1202–1207. 2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Liu B, Li J and Cairns MJ: Identifying
miRNAs, targets and functions. Brief Bioinform. 15:1–19.
2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Luo H, Han Y, Liu J and Zhang Y:
Identification of microRNAs in granulosa cells from patients with
different levels of ovarian reserve function and the potential
regulatory function of miR-23a in granulosa cell apoptosis. Gene.
686:250–260. 2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Veshkini A, Mohammadi-Sangcheshmeh A,
Alamouti AA, Kouhkan F and Salehi A: Maternal supplementation with
fish oil modulates inflammation-related MicroRNAs and genes in
suckling lambs. Trop Anim Health Prod. 52:1561–1572.
2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Shen S, Luo X, Gao K, Sun Y, Yao D and Zhu
L: Identification and integrative analysis of microRNAs and mRNAs
involved in proliferation and invasion of pressure-treated human
liver cancer cell lines. Mol Med Rep. 20:375–387. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Gao H, Han Z, Huang S, Bai R, Ge X, Chen F
and Lei P: Intermittent hypoxia caused cognitive dysfunction relate
to miRNAs dysregulation in hippocampus. Behav Brain Res. 335:80–87.
2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Jin Z, Piao L, Sun G, Lv C, Jing Y and Jin
R: Long non-coding RNA PART1 exerts tumor suppressive functions in
glioma via sponging miR-190a-3p and inactivation of PTEN/AKT
pathway. Onco Targets Ther. 13:1073–1086. 2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhu J, Tang H, Zhang Z, Zhang Y, Qiu C,
Zhang L, Huang P and Li F: Kaempferol slows intervertebral disc
degeneration by modifying LPS-induced osteogenesis/adipogenesis
imbalance and inflammation response in BMSCs. Int Immunopharmacol.
43:236–242. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wang H, Hao P, Zhang H, Xu C and Zhao J:
MicroRNA-223 inhibits lipopolysaccharide-induced inflammatory
response by directly targeting Irak1 in the nucleus pulposus cells
of intervertebral disc. IUBMB Life. 70:479–490. 2018.PubMed/NCBI View
Article : Google Scholar
|
|
30
|
Yuan M, Pai PJ, Liu X, Lam H and Chan BP:
Proteomic analysis of nucleus pulposus cell-derived extracellular
matrix niche and its effect on phenotypic alteration of dermal
fibroblasts. Sci Rep. 8(1512)2018.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Zhang C, Gullbrand SE, Schaer TP, Lau YK,
Jiang Z, Dodge GR, Elliott DM, Mauck RL, Malhotra NR and Smith LJ:
Inflammatory cytokine and catabolic enzyme expression in a goat
model of intervertebral disc degeneration. J Orthop Res: Feb 24,
2020 (Epub ahead of print).
|
|
32
|
Li L, Wan G, Han B and Zhang Z:
Echinacoside alleviated LPS-induced cell apoptosis and inflammation
in rat intestine epithelial cells by inhibiting the mTOR/STAT3
pathway. Biomed Pharmacother. 104:622–628. 2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Dong ZW and Yuan YF: Juglanin suppresses
fibrosis and inflammation response caused by LPS in acute lung
injury. Int J Mol Med. 41:3353–3365. 2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Ren Q, Zhao S, Ren C and Ma Z: Astragalus
polysaccharide alleviates LPS-induced inflammation injury by
regulating miR-127 in H9c2 cardiomyoblasts. Int J Immunopathol
Pharmacol. 32(2058738418759180)2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zhang Y, Yang J, Zhou X, Wang N, Li Z,
Zhou Y, Feng J, Shen D and Zhao W: Knockdown of miR-222 inhibits
inflammation and the apoptosis of LPS-stimulated human
intervertebral disc nucleus pulposus cells. Int J Mol Med.
44:1357–1365. 2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Shi X, Sun M, Liu H, Yao Y and Song Y:
Long non-coding RNAs: A new frontier in the study of human
diseases. Cancer Lett. 339:159–166. 2013.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Sun M, Geng D, Li S, Chen Z and Zhao W:
lncRNA PART1 modulates toll-like receptor pathways to influence
cell proliferation and apoptosis in prostate cancer cells. Biol
Chem. 399:387–395. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Lou T, Ke K, Zhang L, Miao C and Liu Y:
lncRNA PART1 facilitates the malignant progression of colorectal
cancer via miR-150-5p/LRG1 axis. J Cell Biochem. 121:4271–4281.
2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Zhuan B, Lu Y, Chen Q, Zhao X, Li P, Yuan
Q and Yang Z: Overexpression of the long noncoding RNA TRHDE-AS1
inhibits the progression of lung cancer via the miRNA-103/KLF4
axis. J Cell Biochem. 120:17616–17624. 2019.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Shu T, He L, Wang X, Pang M, Yang B, Feng
F, Wu Z, Liu C, Zhang S, Liu B, et al: Long noncoding RNA UCA1
promotes chondrogenic differentiation of human bone marrow
mesenchymal stem cells via miRNA-145-5p/SMAD5 and
miRNA-124-3p/SMAD4 axis. Biochem Biophys Res Commun. 514:316–322.
2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Huang Y: The novel regulatory role of
lncRNA-miRNA-mRNA axis in cardiovascular diseases. J Cell Mol Med.
22:5768–5775. 2018.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Wang W, Lou W, Ding B, Yang B, Lu H, Kong
Q and Fan W: A novel mRNA-miRNA-lncRNA competing endogenous RNA
triple sub-network associated with prognosis of pancreatic cancer.
Aging (Albany NY). 11:2610–2627. 2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Mi D, Cai C, Zhou B, Liu X, Ma P, Shen S,
Lu W and Huang W: Long non-coding RNA FAF1 promotes intervertebral
disc degeneration by targeting the Erk signaling pathway. Mol Med
Rep. 17:3158–3163. 2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Li Z, Li X, Chen C, Chan MTV, Wu WKK and
Shen J: Melatonin inhibits nucleus pulposus (NP) cell proliferation
and extracellular matrix (ECM) remodeling via the melatonin
membrane receptors mediated PI3K-Akt pathway. J Pineal Res 63,
2017.
|
|
45
|
Fuchs Y and Steller H: Live to die another
way: Modes of programmed cell death and the signals emanating from
dying cells. Nat Rev Mol Cell Biol. 16:329–344. 2015.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Soteriou D and Fuchs Y: A matter of life
and death: Stem cell survival in tissue regeneration and tumour
formation. Nat Rev Cancer. 18:187–201. 2018.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Guo Y, Tian L, Liu X, He Y, Chang S and
Shen Y: ERRFI1 inhibits proliferation and inflammation of nucleus
pulposus and is negatively regulated by miR-2355-5p in
intervertebral disc degeneration. Spine (Phila Pa 1976).
44:E873–E881. 2019.PubMed/NCBI View Article : Google Scholar
|