Introduction
Chronic obstructive pulmonary disease (COPD) is a
type of pulmonary disease characterized by airflow restriction that
is largely irreversible and a progressive course (1). According to the World Health
Organization, COPD will become the third deadliest disease
worldwide by 2030, and is projected to affect an increasingly large
proportion of the global population (2,3).
Airway inflammation and remodeling are major types of structural
and functional changes in COPD, which contribute to exaggerated
airway narrowing and resistance to airflow (4). Air pollution, tobacco exposure and
repeated respiratory tract infection lead to persistent lung
inflammation, which eventually causes deterioration of lung
function (1).
Airway smooth muscle and the mucous membrane receive
sensory innervation, and the sensory terminals can release a series
of regulatory factors (e.g. neurotrophic factors) (5). Brain-derived neurotrophic factor
(BDNF) is a major member of the neurotrophic factor family, which
also plays an important role in the regulation of airway neurogenic
inflammation (6). BDNF is a key
neuroprotective factor that promotes and maintains the survival of
sensory neurons, and the growth of neurites (7). BDNF can be produced by and act on
immune inflammatory cells (8).
Moreover, the levels of BDNF are increased in inflammatory,
autoimmune and allergic diseases, such as asthma and allergic
rhinitis (9).
Although its presence in the nervous system is
well-known (10), BDNF is also
expressed by structural cells of the lung. Thus, it has the
potential to influence airway structure and function (11,12).
For example, sputum and bronchoalveolar lavage fluid from patients
with asthma show increased levels of BDNF (13,14).
Previous studies regarding the effect of BDNF on the airway mainly
focused on asthma and airway inflammation after viral infection
(15-17).
Few studies have focused on the role of BDNF in COPD-related airway
inflammation. Thus, the aim of the present study was to investigate
the effect of BDNF on pulmonary function and airway inflammation in
a rat model of COPD.
Materials and methods
Animals and models
A total of 28 male Sprague-Dawley rats (age, 6-8
weeks; weight, 180-200 g) were obtained from Shanghai Sipper-BK
Laboratory Animal Co. All animal experiments and procedures were
approved (approval nos. AS20180042GZL and 20180213) by the Animal
Care and Use Committee of the Affiliated Kunshan Hospital of
Jiangsu University (Kunshan, China). They were performed in
accordance with the Guide for the Care and Use of Laboratory
Animals, published by the United States National Institutes of
Health (18). All animals were fed
in a silent environment at 18-25˚C (relative humidity, 40-70%),
housed away from bright light under a 10/14 h day/night cycle, and
given free access to food and water. The rats were acclimated for 1
week before the experiments. The animals were divided into control,
COPD, COPD + anti-BDNF and COPD + normal saline (NS) groups (n=7
rats per group).
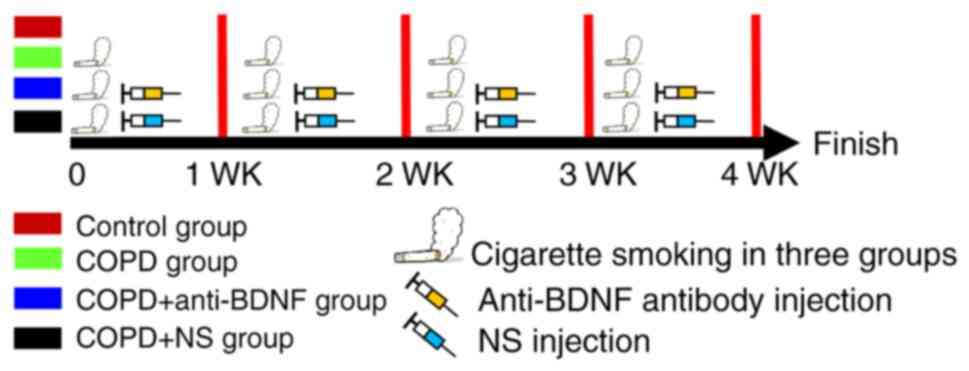
Rats in the COPD, COPD + anti-BDNF and COPD + NS
groups were exposed to cigarette smoke (Hongmei cigarettes; 13 mg
CO; 13 mg tar oil) for 30 min/day, twice per day at 6-h intervals.
This treatment was performed 6 days per week for 16 weeks in an
8050™ inhalation exposure system (Tianjin Hope Industry & Trade
Co., Ltd.) (19). Rats in the COPD
+ anti-BDNF and COPD + NS groups were intraperitoneally injected
with anti-BDNF antibody (1:1,000; 0.1 g/ml; 4 ml/kg; cat. no.
ab108319; Abcam) and NS (4 ml/kg), respectively, once per week for
4 consecutive weeks. The experimental procedure is shown in
Fig. 1.
Lung function
Lung function was assessed based on the ratio of
forced expiratory volume (FEV) at 0.2 sec (FEV0.2) to
forced vital capacity (FVC), as well as the peak expiratory flow
(PEF) (20). Rats were injected
with 1% pentobarbital sodium (40 mg/kg, intraperitoneal injection),
and then administered with appropriate anesthetics for the
maintenance of anesthesia. The trachea of each rat was cut,
intubated, and attached to a ventilator at a respiratory rate of 75
beats/min with a tidal volume of 5 ml/kg. The FEV0.2/FVC
and PEF were measured using the AniRes2005 pulmonary mechanics
analyzer (Beijing Bestlab High-Tech).
Specimen processing
After lung function measurements were performed,
rats were anesthetized with 1% pentobarbital sodium (40 mg/kg,
intraperitoneal injection), and subsequently transcardially
perfused with 0.3% PBS. Lung and bronchial tissues were rapidly
removed. Left lung tissue was sectioned at 5 µm for H&E
staining, immunohistochemistry and western blotting. Right lung
tissue was used for enzyme-linked immunosorbent assay and detection
of oxidative stress.
H&E staining
Lung tissues were fixed in 10% neutral formalin for
24 h at room temperature and subsequently paraffin-embedded.
Sections (5 µm) were prepared from the paraffin-embedded tissue
blocks by dehydration through a graded ethanol series (75, 85, 95
and 100%) and washed with xylene. Sections were stained with
H&E for 12 min at room temperature. Morphological changes in
the lung tissues were evaluated using an Olympus light microscope
(magnification, x400; Olympus Corporation).
Immunohistochemistry
Lung tissues were frozen with optimal cutting
temperature compound (cat. no. ZLI9302; ZSBIO Co.) and coronally
sectioned using a Leica freezing microtome (Leica Microsystems,
Inc.). Lung tissue sections were incubated with 3%
H2O2 for 15 min to block endogenous
peroxidase activity, washed with 0.3% PBS (3x5 min), incubated for
1 h at room temperature with a blocking solution (10% goat serum;
cat. no. ZLI9022; ZSBIO Co.), and then incubated at 4˚C overnight
with the primary antibody (rabbit anti-BDNF; 1:1,000; cat. no.
ab108319; Abcam). Tissue sections were washed with 0.3% PBS (3x5
min) and then incubated for 1 h at room temperature with a
biotinylated secondary antibody (goat anti-rabbit; 1:500; cat. no.
ab6721; Abcam). After tissue sections had been washed with 0.3% PBS
(3x5 min), they were incubated for 30 min with avidin/biotinylated
horseradish peroxidase, washed with 0.3% PBS (3x5 min), and reacted
with DAB as a chromogen. Sections were observed using an Olympus
light microscope (Olympus Corporation).
Enzyme-linked immunosorbent assay
The bronchi and lungs were weighed, boiled (100˚C)
for 10 min in 1 M acetic acid (1:10, wt/vol), suspended in 0.1 M
PBS, and homogenized. Homogenates were transferred to polypropylene
tubes and centrifuged (40,000 x g, 4˚C, 20 min). Before
measurements were taken, the supernatant was centrifuged again at
40,000 x g and 4˚C for 20 min. BDNF (cat. no. DBNT00; R&D
Systems, Inc.), IL-6 and TNF-α (cat. no. 31857; Cayman Chemical
Company) concentrations were measured using enzyme-linked
immunosorbent assay kits, according to the manufacturer's
instructions.
Western blotting
Lung samples were placed in lysis buffer containing
protease inhibitors, and then homogenized and centrifuged at 15,000
x g and 4˚C for 10 min. Protein concentrations were measured using
a BCA protein assay kit. A total of 50 µg total protein was
separated via 10% SDS-PAGE gel electrophoresis, and then
transferred by electroblotting onto PVDF membranes. The membranes
were blocked at room temperature with 3% BSA (cat. no. 9998; CST
Biological Reagents Co., Ltd.) in TBS containing 0.1% Tween-20 for
1 h, and then incubated overnight at 4˚C with the primary antibody
rabbit, anti-BDNF (1:500; cat. no. ab108319; Abcam). The membranes
were then washed with TBS containing 0.1% Tween-20 and incubated
for 1 h at room temperature with a horseradish
peroxidase-conjugated secondary antibody (1:2,000; cat. no. 31461;
Invitrogen; Thermo Fisher Scientific, Inc.). Protein bands were
detected using an ECL substrate kit (cat. no. WP20005; Invitrogen;
Thermo Fisher Scientific, Inc.) and then exposed to CL-XPosure film
(Pierce; Thermo Fisher Scientific, Inc.). GAPDH (1:4,000; cat. no.
9545; Sigma-Aldrich; Merck KGaA) was used as the internal
control.
Oxidant stress detection
The levels of malondialdehyde (MDA; cat. no.
A003-1-2), glutathione peroxidase (GSH; cat. no. A005-1-2) and
superoxide dismutase (SOD; cat. no. A001-3-2) were measured in the
lung tissues using appropriate kits (Nanjing Jiancheng
Bioengineering Institute).
Statistical analysis
All experiments were performed in triplicate. Data
are expressed as the mean ± standard deviation and were analyzed
using SPSS software (17.0; SPSS Inc.). Comparisons among multiple
groups were performed using one-way analysis of variance, followed
by Tukey's post hoc test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Lung functions and histological
changes
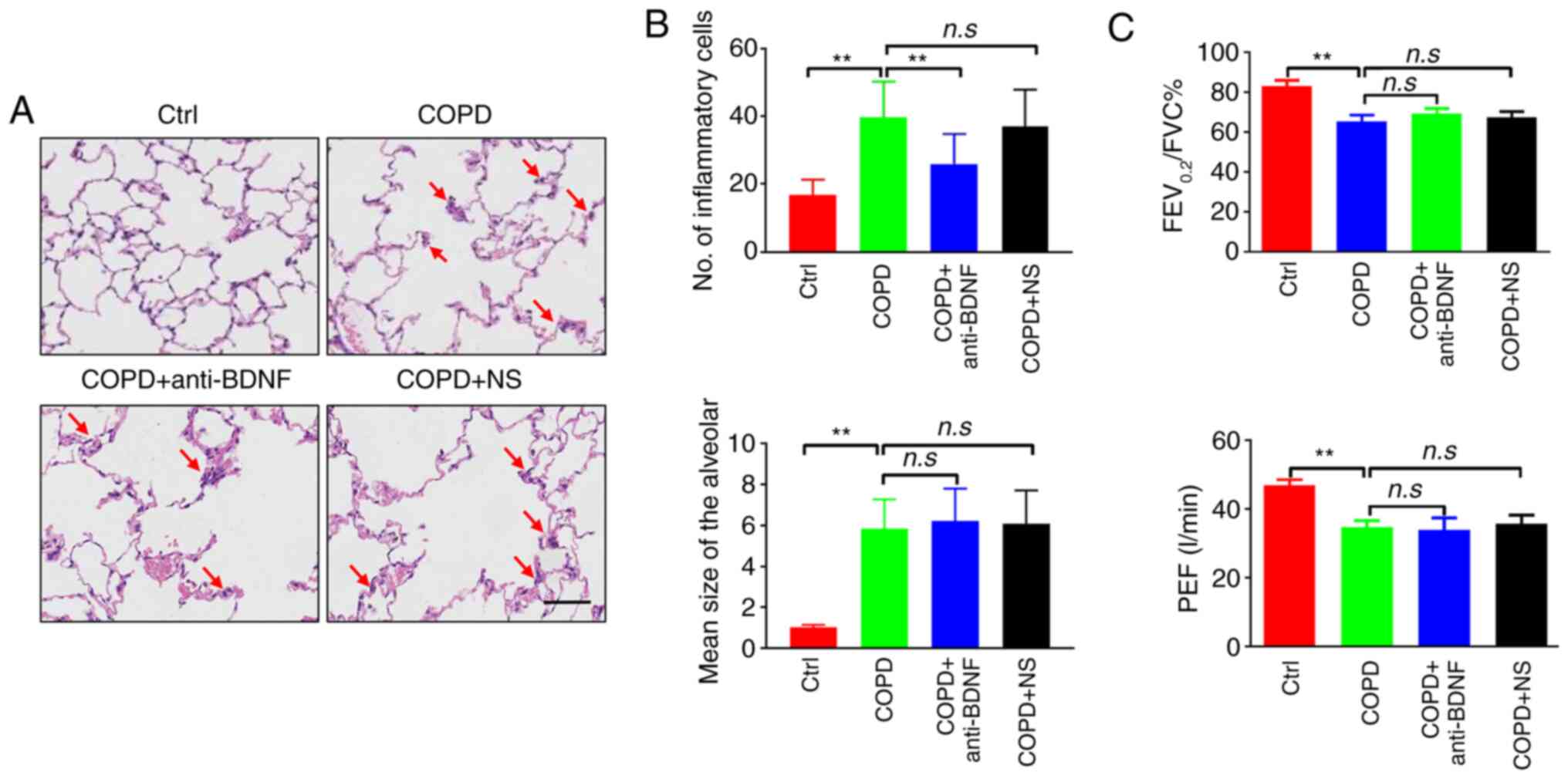
Smoking is a major risk factor for the development
of COPD. In the control group, the bronchial mucosa was normal and
the alveoli were uniform. In the COPD group, the bronchial mucosa
epithelium was necrotic and showed exfoliation with infiltrating
inflammatory cells (mainly neutrophils and macrophages). The
alveoli were of different sizes, and their walls were thinned and
broken, as some had fused to form pulmonary bullae. Anti-BDNF
treatment alleviated the inflammation compared with the COPD group
(Fig. 2A and B). After long-term heavy cigarette
exposure, the FEV0.2/FVC and PEF values in rats with
COPD were reduced significantly compared with control rats
(P<0.01). However, there were no differences between rats in the
COPD group and those in the COPD + anti-BDNF or COPD + NS groups
(P>0.05; Fig. 2C). These results
indicated that anti-BDNF intervention did not affect lung function
or histopathological findings.
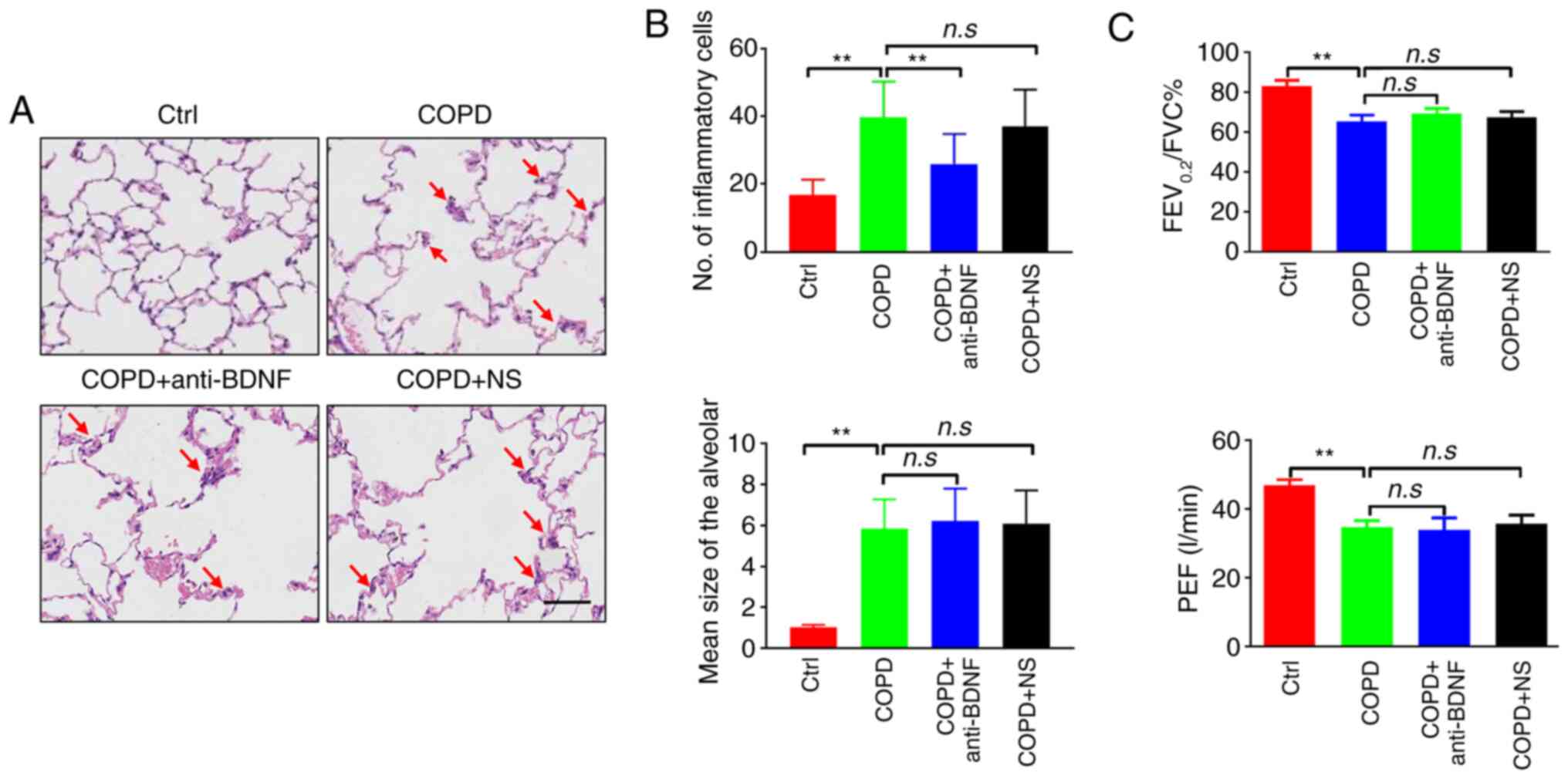 | Figure 2Effect of anti-BDNF treatment on
airway inflammation and lung function. (A) Histological changes
observed in the lung tissues. Inflammatory cells were marked by red
arrows. In the control group, the alveoli exhibited uniform size,
and there was no obvious inflammatory cell infiltration in the
airway. In the COPD group, the bronchial mucosa epithelium was
necrotic and exhibited exfoliation with infiltrating inflammatory
cells. Additionally, multiple alveoli were fused to form pulmonary
bullae. In the COPD + anti-BDNF group, inflammatory cells in the
airway were slightly reduced compared with the COPD group, but
alveolar fusion was similar to that observed in the COPD group.
Pulmonary histopathological changes in the COPD + NS group were
similar to those in the COPD group. Scale bar, 200 µm. (B) Numbers
of inflammatory cells and mean size of alveoli. Cigarette smoke
inhalation may cause airway inflammation, emphysema and
inflammatory cell infiltration of bronchial tissue. The numbers of
inflammatory cells were greater in the COPD group than in the
control group. When rats were treated with anti-BDNF antibody, the
number of inflammatory cells was significantly lower than that in
the COPD group. There were no significant differences between the
COPD + anti-BDNF and COPD + NS groups. The alveolar space was
markedly dilated in the COPD, COPD + anti-BDNF and COPD + NS
groups, indicating that anti-BDNF antibody treatment did not
improve emphysema. (C) Lung functions. After cigarette smoke
exposure, lung function indices (FEV0.2/FVC% and PEF)
were significantly decreased compared with the control group.
Anti-BDNF antibody and NS injection both caused no significant
changes in the COPD + anti-BDNF or COPD + NS group relative to the
COPD group. n=7 rats per group. **P<0.01 vs. COPD
group. COPD, chronic obstructive pulmonary disease; BDNF,
brain-derived neurotrophic factor; NS, normal saline;
FEV0.2, forced expiratory volume at 0.2 sec; FVC, forced
vital capacity; PEF, peak expiratory flow. |
BDNF expression in the airway
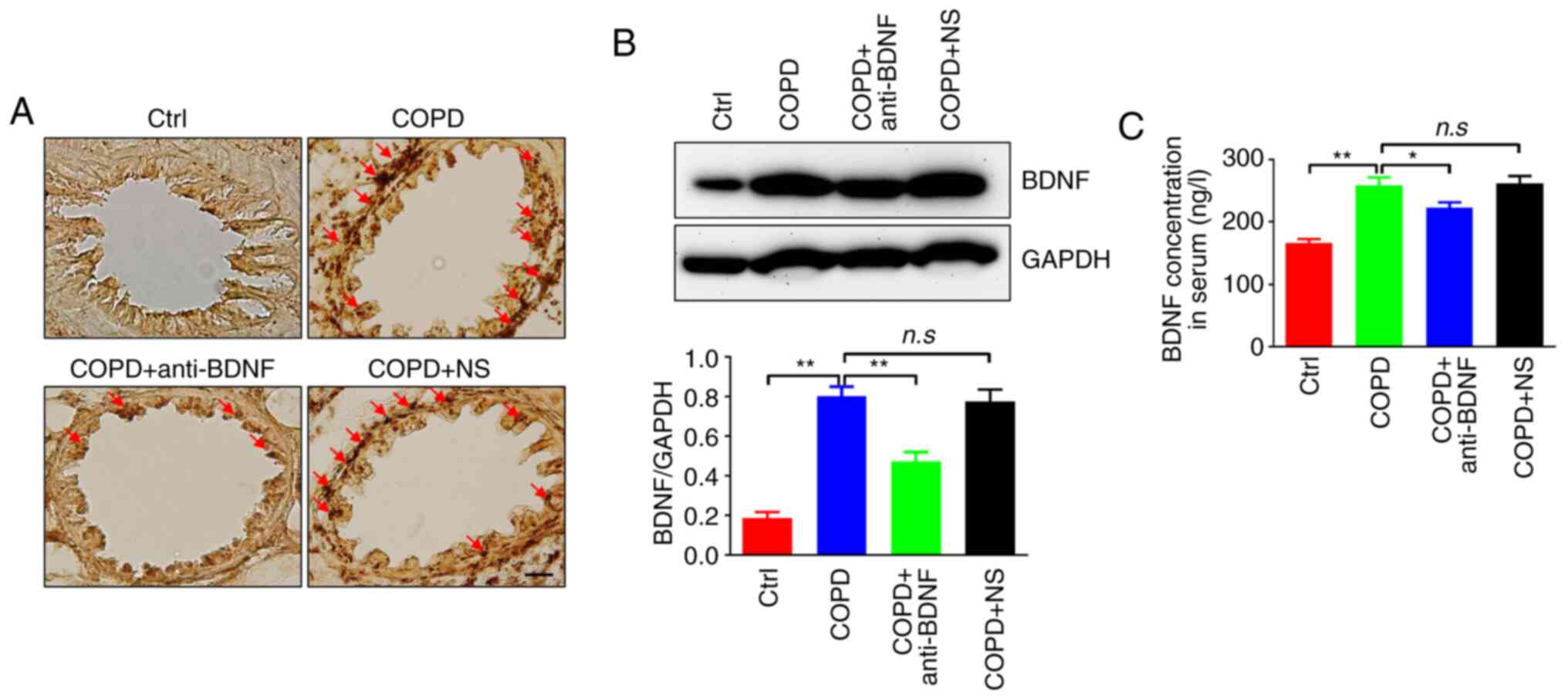
BDNF-like immunoreactivity (red arrow) was indicated
by brown staining of bronchial and lung tissues, predominantly in
the cytoplasm of epithelial cells in the peribronchial region
(Fig. 3A). The BDNF expression
level measured by western blotting was significantly increased in
the COPD group compared with the control group (P<0.01).
However, this level was decreased in the COPD + anti-BDNF group
compared with the COPD group (P<0.01). BDNF expression did not
significantly differ between the COPD and COPD + NS groups
(P>0.05; Fig. 3B). BDNF
concentrations measured by enzyme-linked immunosorbent assay showed
similar results. The BDNF concentration was higher in the COPD
group than in the control group (P<0.01). Conversely, the BDNF
concentration was lower in the COPD + anti-BDNF group than in the
COPD group (P<0.05). The BDNF concentration did not
significantly differ between the COPD and COPD + NS groups
(P>0.05; Fig. 3C). These results
indicated that anti-BDNF antibody injection could reduce BDNF
expression level in the airway.
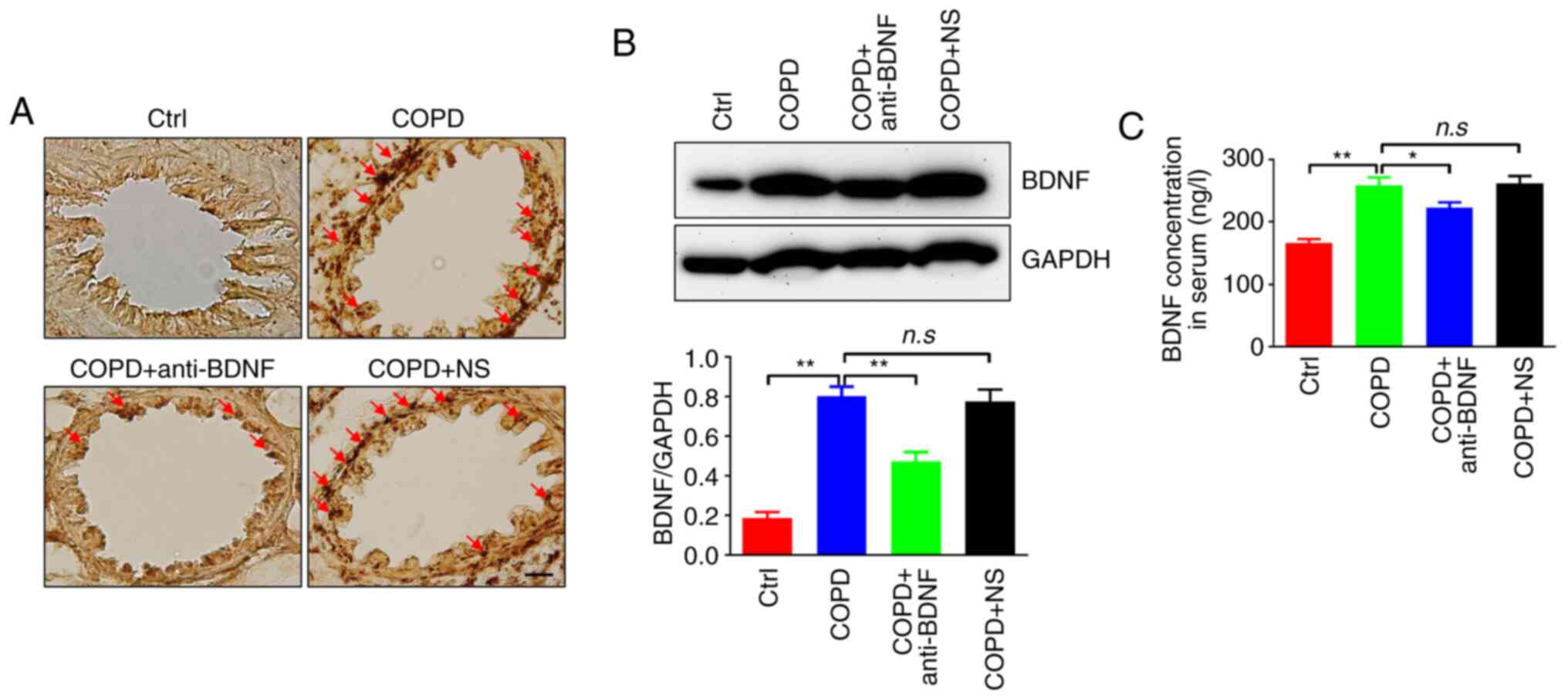 | Figure 3BDNF expression levels in the lung.
(A) Immunohistochemistry of BDNF expression levels (brown staining,
red arrow) in the airway. In the COPD group, the BDNF expression
level was significantly increased compared with the control group,
whereas it was decreased in the COPD + anti-BDNF group. In the COPD
+ NS group, the BDNF expression level was similar to that in the
COPD group. BDNF-like immunoreactivity was indicated by brown
staining in bronchi and lung tissues, predominantly in the
cytoplasm of epithelial cells in the peribronchial region. Scale
bar, 100 µm. (B) Western blotting of BDNF expression in the airway.
Similar to the immunohistochemistry findings, BDNF expression, as
detected by western blotting, was increased in the COPD group
compared with the control group. The ratio of BDNF/GAPDH was near
0.8 in the COPD group (vs. 0.2 in the control group), but decreased
in the COPD + anti-BDNF group. BDNF expression did not differ
between the COPD + anti-BDNF and COPD + NS groups. (C)
Enzyme-linked immunosorbent assay measurement of BDNF
concentrations. The BDNF concentration was higher in the COPD group
than in the control group, but decreased upon treatment with
anti-BDNF antibody. The BDNF concentration did not differ between
the COPD + anti-BDNF and COPD + NS groups. n=7 rats per group.
*P<0.05, **P<0.01 vs. COPD group. COPD,
chronic obstructive pulmonary disease; BDNF, brain-derived
neurotrophic factor; NS, normal saline. |
Oxidative stress in the airway
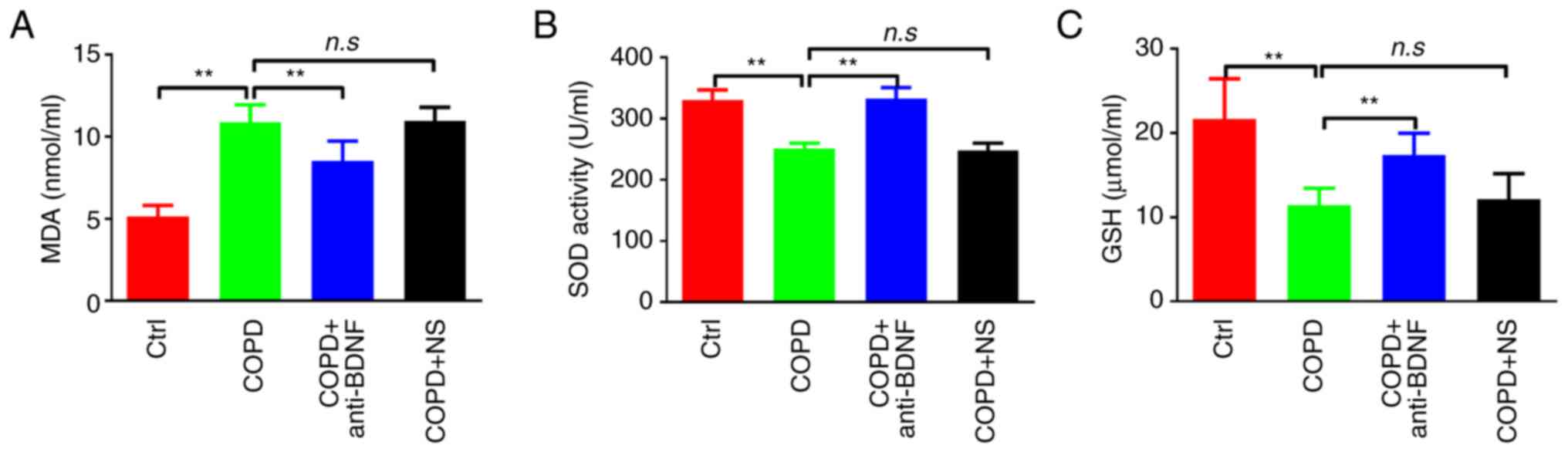
Long-term cigarette smoking induces oxidative stress
(21). Therefore, the levels of
MDA, SOD and GSH in the airway and lung were measured. After
cigarette smoke exposure, the level of MDA was significantly
increased in the COPD group compared with the control group
(P<0.01), and was significantly decreased in the COPD +
anti-BDNF group compared with the COPD group (P<0.01). The MDA
level did not significantly differ between the COPD and COPD + NS
groups (P>0.05; Fig. 4A). By
contrast, the levels of SOD and GSH were significantly decreased in
the COPD group compared with the control group (both P<0.01),
and were increased in the COPD + anti-BDNF group compared with the
COPD group (both P<0.01). The SOD and GSH levels did not
significantly differ between the COPD and COPD + NS groups (both
P>0.05; Fig. 4B and C). These data demonstrated that anti-BDNF
could improve the imbalance of oxidation and antioxidation in the
airway and lung.
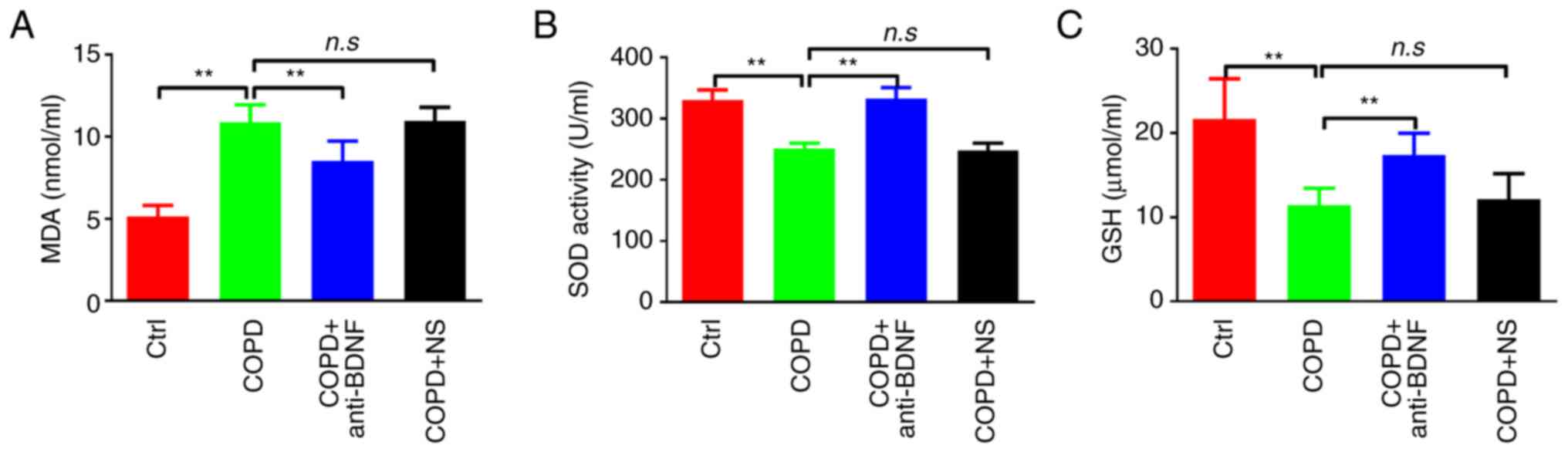 | Figure 4Effect of anti-BDNF treatment on
oxidative stress. Levels of (A) MDA, (B) SOD and (C) GSH. Cigarette
smoke exposure may induce an imbalance between oxidation and
antioxidation in the airway. The level of MDA was increased,
whereas those of SOD and GSH were decreased, in the COPD group
compared with the control group. After anti-BDNF antibody
administration, the levels of MDA, SOD and GSH were improved. There
was no difference in the MDA, SOD or GSH level between the COPD and
COPD + NS groups. n=7 rats per group. **P<0.01 vs.
COPD group. MDA, malondialdehyde; GSH, glutathione peroxidase; SOD,
superoxide dismutase; COPD, chronic obstructive pulmonary disease;
BDNF, brain-derived neurotrophic factor; NS, normal saline. |
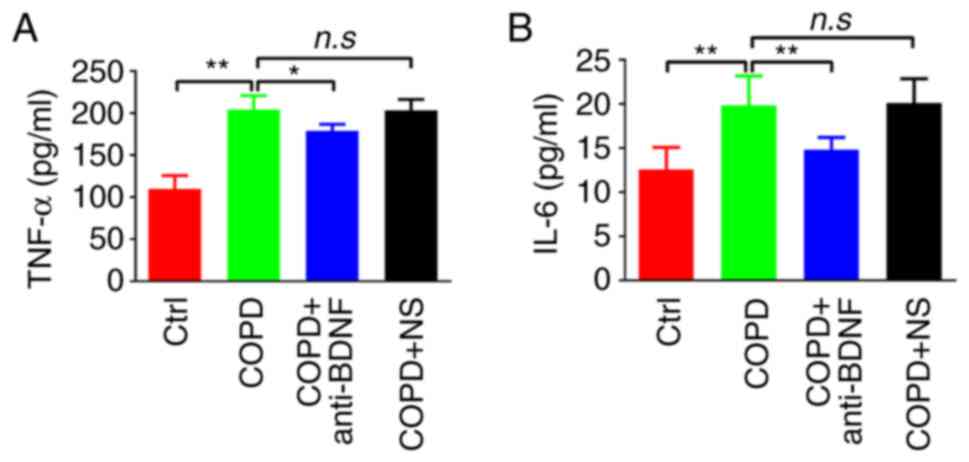
Pro-inflammatory cytokines in the
airway
Inflammation is an important component of COPD
pathogenesis (22). In this study,
levels of the representative inflammatory markers TNF-α and IL-6
were examined. The levels of both markers were significantly
increased in the COPD group compared with the control group (both
P<0.01). However, the levels of these markers were decreased in
the COPD + anti-BDNF group compared with the COPD group (P<0.05
and P<0.01, respectively). The levels of TNF-α and IL-6 did not
significantly differ between the COPD group and the COPD + NS group
(both P>0.05; Fig. 5A and
B). These results indicated that
anti-BDNF treatment could alleviate smoking-induced airway
inflammation.
Discussion
COPD is a common respiratory disease characterized
by progressive and irreversible airway obstruction. Because of the
long course of disease, repeated episodes, delays, exacerbation and
reduced quality of life, patients with COPD often experience
anxiety and depression (23). BDNF
is a protein synthesized in the brain and then widely distributed
in the central nervous system. BDNF plays an important role in the
survival, differentiation, and growth of neurons (24). Notably, it can prevent neurons from
being damaged and undergoing apoptosis, in addition to promoting
the regeneration and differentiation of damaged neurons (25). Therefore, BDNF is an important
target of antidepressant treatment (26,27).
Previous studies have reported that BDNF is closely
associated with multiple pulmonary diseases (28-31).
BDNF has shown an association with allergic airway inflammation,
especially asthma (32). Air
pollutant exposure is a risk factor for the development of allergic
diseases and respiratory infections (33). Active smoking and secondhand smoke
can both potentiate the effects of other allergens. In a mouse
model of allergic asthma, BDNF contributed to airway
hyperreactivity and allergic inflammation (16). Airway BDNF secretion is regulated at
multiple levels, thus influencing airway contractility and
remodeling (29,34). Specific BDNF gene polymorphisms may
contribute to bronchial asthma susceptibility, and a positive
association between selected functional BDNF polymorphisms (i.e.,
rs6265) and asthma has been suggested in children (35).
However, to the best of our knowledge, there have
been few studies regarding the relationship between BDNF expression
and airway inflammation in patients with COPD. In the present
study, the effects of anti-BDNF treatment on airway inflammation
and lung function in a rat model of COPD were explored. The results
indicated that cigarette smoking could induce BDNF expression in
the airway. Although anti-BDNF treatment did not improve lung
function in rats with COPD, the inflammatory cytokine levels and
imbalance between oxidation and antioxidation in the airway were
alleviated. Regarding the underlying mechanism, increased BDNF may
promote airway irritability via the nervous system, modulate
epithelium-derived bronchodilator responses, or increase airway
smooth muscle [Ca2+]i and contractility,
especially in the presence of inflammatory cytokines (36). BDNF may modulate airway remodeling
via proliferation, migration, and secretion of inflammatory
mediators and modulators (37).
Furthermore, BDNF secretion is controlled by nerves. As a growth
factor, BDNF (potentially derived from local tissues or nerves
themselves) can enhance the survival or expansion of receptive
fields of sensory nerve endings (38). Importantly, increased BDNF
expression and secretion by airway smooth muscle in the inflamed
airway may act on postganglionic parasympathetic airway nerves
(39). Given that neuronal activity
itself can enhance BDNF expression and release, a positive feedback
cycle may be established in the disease state, which would promote
nerve expansion (40). BDNF can
also enhance the expression levels of other receptors, and synaptic
transmission, thereby enhancing bronchoconstriction (41,42).
In patients with COPD, abnormal activity of the vagal nerve
innervating the airway may lead to increased secretion of BDNF and
further aggravation of airway inflammation, thus affecting
respiratory function (17).
However, in the present study, anti-BDNF treatment did not improve
lung function in the experimental rats. This may be related to the
short-duration cigarette smoke exposure. Therefore, further
experiments are needed with longer smoke exposure to confirm
whether BDNF has an effect on lung function.
There are a number of limitations to the present
study. Smoke exposure is a key causative factor of COPD, however,
alternative factors, such as environmental pollution and infection
may also impact the pathophysiological process of COPD. Thus,
further investigation into the role of anti-BDNF treatment in the
improvement of airway inflammation in COPD induced by fine
particulate matter exposure or respiratory infection is
required.
In conclusion, this study showed that cigarette
smoke exposure could lead to increased BDNF expression levels in
the airway of rats with COPD. Thus, BDNF may be related to airway
inflammation. Anti-BDNF treatment could alleviate airway
inflammation and improve the imbalance between oxidation and
antioxidation in the airway.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by grants from the
Kunshan Science Project (grant no. KS1723) and Jiangsu University
(grant no. JLY2021068).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZG, SL and BX were responsible for performing the
experiments and writing the manuscript. LL and YX were responsible
for designing the study, performing the experiments and collecting
the data. HL was responsible for providing experimental ideas, data
analysis, interpretation of data and reviewing the manuscript. ZG
and HL confirm the authenticity of all the raw data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
All animal experiments and procedures were approved
(approval nos. AS20180042GZL and 20180213) by the Animal Care and
Use Committee of the Affiliated Kunshan Hospital of Jiangsu
University (Kunshan, China). They were performed in accordance with
the Guide for the Care and Use of Laboratory Animals, published by
the United States National Institutes of Health.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lareau SC, Fahy B, Meek P and Wang A:
Chronic obstructive pulmonary disease (COPD). Am J Respir Crit Care
Med. 199:P1–P2. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
López-Campos JL, Tan W and Soriano JB:
Global burden of COPD. Respirology. 21:14–23. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mathers CD and Loncar D: Projections of
global mortality and burden of disease from 2002 to 2030. PLoS Med.
3(e442)2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Barnes PJ: Inflammatory endotypes in COPD.
Allergy. 74:1249–1256. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mazzone SB and Undem BJ: Vagal afferent
innervation of the airways in health and disease. Physiol Rev.
96:975–1024. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bennedich Kahn L, Gustafsson LE and Olgart
Höglund C: Brain-derived neurotrophic factor enhances
histamine-induced airway responses and changes levels of exhaled
nitric oxide in guinea pigs in vivo. Eur J Pharmacol. 595:78–83.
2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lu B, Nagappan G and Lu Y: BDNF and
synaptic plasticity, cognitive function, and dysfunction. Handb Exp
Pharmacol. 220:223–250. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hahn C, Islamian AP, Renz H and Nockher
WA: Airway epithelial cells produce neurotrophins and promote the
survival of eosinophils during allergic airway inflammation. J
Allergy Clin Immunol. 117:787–794. 2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Raap U and Braunstahl GJ: The role of
neurotrophins in the pathophysiology of allergic rhinitis. Curr
Opin Allergy Clin Immunol. 10:8–13. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hempstead BL: Brain-derived neurotrophic
factor: Three ligands, many actions. Trans Am Clin Climatol Assoc.
126:9–19. 2015.PubMed/NCBI
|
|
11
|
Prakash Y, Thompson MA, Meuchel L,
Pabelick CM, Mantilla CB, Zaidi S and Martin RJ: Neurotrophins in
lung health and disease. Expert Rev Respir Med. 4:395–411.
2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Watanabe T, Fajt ML, Trudeau JB, Voraphani
N, Hu H, Zhou X, Holguin F and Wenzel SE: Brain-derived
neurotrophic factor expression in asthma. Association with severity
and type 2 inflammatory processes. Am J Respir Cell Mol Biol.
53:844–852. 2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Braun A, Lommatzsch M, Mannsfeldt A,
Neuhaus-Steinmetz U, Fischer A, Schnoy N, Lewin GR and Renz H:
Cellular sources of enhanced brain-derived neurotrophic factor
production in a mouse model of allergic inflammation. Am J Respir
Cell Mol Biol. 21:537–546. 1999.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Virchow JC, Julius P, Lommatzsch M,
Luttmann W, Renz H and Braun A: Neurotrophins are increased in
bronchoalveolar lavage fluid after segmental allergen provocation.
Am J Respir Crit Care Med. 158:2002–2005. 1998.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zang N, Li S, Li W, Xie X, Ren L, Long X,
Xie J, Deng Y, Fu Z, Xu F and Liu E: Resveratrol suppresses
persistent airway inflammation and hyperresponsivess might
partially via nerve growth factor in respiratory syncytial
virus-infected mice. Int Immunopharmacol. 28:121–128.
2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Britt RD Jr, Thompson MA, Wicher SA,
Manlove LJ, Roesler A, Fang YH, Roos C, Smith L, Miller JD,
Pabelick CM and Prakash YS: Smooth muscle brain-derived
neurotrophic factor contributes to airway hyperreactivity in a
mouse model of allergic asthma. FASEB J. 33:3024–3034.
2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Papp C, Pak K, Erdei T, Juhasz B, Seres I,
Szentpéteri A, Kardos L, Szilasi M, Gesztelyi R and Zsuga J:
Alteration of the irisin-brain-derived neurotrophic factor axis
contributes to disturbance of mood in COPD patients. Int J Chron
Obstruct Pulmon Dis. 12:2023–2033. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Guide for the Care and Use of Laboratory
Animals. Washington (DC). National Academies Press (US), 1996.
|
|
19
|
Lin L, Yin Y, Hou G, Han D, Kang J and
Wang Q: Ursolic acid attenuates cigarette smoke-induced emphysema
in rats by regulating PERK and Nrf2 pathways. Pulm Pharmacol Ther.
44:111–121. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yu N, Sun YT, Su XM, He M, Dai B and Kang
J: Treatment with eucalyptol mitigates cigarette smoke-induced lung
injury through suppressing ICAM-1 gene expression. Biosci Rep: Jul
6, 2018 (Epub ahead of print). doi: 10.1042/BSR20171636.
|
|
21
|
Hikichi M, Mizumura K, Maruoka S and Gon
Y: Pathogenesis of chronic obstructive pulmonary disease (COPD)
induced by cigarette smoke. J Thorac Dis. 11 (Suppl
17):S2129–S2140. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Rabe KF and Watz H: Chronic obstructive
pulmonary disease. Lancet. 389:1931–1940. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Yohannes AM and Alexopoulos GS: Depression
and anxiety in patients with COPD. Eur Respir Rev. 23:345–349.
2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Binder DK and Scharfman HE: Brain-derived
neurotrophic factor. Growth Factors. 22:123–131. 2004.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wang H, Zhao Y, Wang YJ, Song L, Wang JL,
Huang C, Zhang W and Jiang B: Antidepressant-like effects of
tetrahydroxystilbene glucoside in mice: Involvement of BDNF
signaling cascade in the hippocampus. CNS Neurosci Ther.
23:627–636. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Brunoni AR, Baeken C, Machado-Vieira R,
Gattaz WF and Vanderhasselt MA: BDNF blood levels after
non-invasive brain stimulation interventions in major depressive
disorder: A systematic review and meta-analysis. World J Biol
Psychiatry. 16:114–122. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Tuon T, Valvassori SS, Dal Pont GC,
Paganini CS, Pozzi BG, Luciano TF, Souza PS, Quevedo J, Souza CT
and Pinho RA: Physical training prevents depressive symptoms and a
decrease in brain-derived neurotrophic factor in Parkinson's
disease. Brain Res Bull. 108:106–112. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lieu T and Undem BJ: Neuroplasticity in
vagal afferent neurons involved in cough. Pulm Pharmacol Ther.
24:276–279. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Freeman MR, Sathish V, Manlove L, Wang S,
Britt RD Jr, Thompson MA, Pabelick CM and Prakash YS: Brain-derived
neurotrophic factor and airway fibrosis in asthma. Am J Physiol
Lung Cell Mol Physiol. 313:L360–L370. 2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Zhang SY, Hui LP, Li CY, Gao J, Cui ZS and
Qiu XS: More expression of BDNF associates with lung squamous cell
carcinoma and is critical to the proliferation and invasion of lung
cancer cells. BMC Cancer. 16(171)2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Yao Q, Zaidi SI, Haxhiu MA and Martin RJ:
Neonatal lung and airway injury: A role for neurotrophins. Semin
Perinatol. 30:156–162. 2006.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Nassenstein C, Braun A, Erpenbeck VJ,
Lommatzsch M, Schmidt S, Krug N, Luttmann W, Renz H and Virchow JC
Jr: The neurotrophins nerve growth factor, brain-derived
neurotrophic factor, neurotrophin-3, and neurotrophin-4 are
survival and activation factors for eosinophils in patients with
allergic bronchial asthma. J Exp Med. 198:455–467. 2003.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Brauer M, Hoek G, Smit HA, de Jongste JC,
Gerritsen J, Postma DS, Kerkhof M and Brunekreef B: Air pollution
and development of asthma, allergy and infections in a birth
cohort. Eur Respir J. 29:879–888. 2007.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Aravamudan B, Thompson MA, Pabelick CM and
Prakash YS: Mechanisms of BDNF regulation in asthmatic airway
smooth muscle. Am J Physiol Lung Cell Mol Physiol. 311:L270–L279.
2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Jesenak M, Babusikova E, Evinova A,
Banovcin P and Dobrota D: Val66Met polymorphism in the BDNF gene in
children with bronchial asthma. Pediatr Pulmonol. 50:631–637.
2015.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Prakash YS, Thompson MA and Pabelick CM:
Brain-derived neurotrophic factor in TNF-alpha modulation of
Ca2+ in human airway smooth muscle. Am J Respir Cell Mol
Biol. 41:603–611. 2009.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Bai TR: Evidence for airway remodeling in
chronic asthma. Curr Opin Allergy Clin Immunol. 10:82–86.
2010.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Numakawa T, Suzuki S, Kumamaru E, Adachi
N, Richards M and Kunugi H: BDNF function and intracellular
signaling in neurons. Histol Histopathol. 25:237–258.
2010.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Pan J, Rhode HK, Undem BJ and Myers AC:
Neurotransmitters in airway parasympathetic neurons altered by
neurotrophin-3 and repeated allergen challenge. Am J Respir Cell
Mol Biol. 43:452–457. 2010.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Park H and Poo MM: Neurotrophin regulation
of neural circuit development and function. Nat Rev Neurosci.
14:7–23. 2013.PubMed/NCBI View
Article : Google Scholar
|
|
41
|
Meuchel LW, Stewart A, Smelter DF, Abcejo
AJ, Thompson MA, Zaidi SI, Martin RJ and Prakash YS:
Neurokinin-neurotrophin interactions in airway smooth muscle. Am J
Physiol Lung Cell Mol Physiol. 301:L91–L98. 2011.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Piedimonte G: Contribution of neuroimmune
mechanisms to airway inflammation and remodeling during and after
respiratory syncytial virus infection. Pediatr Infect Dis J. 22
(Suppl 2):S66–S75. 2003.PubMed/NCBI View Article : Google Scholar
|