Introduction
Granulomatous lobular mastitis (GLM) is a rare,
chronic inflammatory breast disease, which is primarily
characterized by nonspecific lobulitis involving multiple lobules
(1,2). GLM is more common in postpartum
females compared with nullipara females and the clinical
manifestations and imaging findings at the early stage of the
disease are similar to those of breast cancer (3,4),
consisting of a lump, pain in the breast, red and swollen skin,
ulceration and even abscesses in severe cases (5). Due to the extended duration of the
disease, recurrent ulceration and the formation of multiple
sinuses, GLM results in poor quality of life of affected patients,
and in certain cases, it even causes depression (6). thus, there is an urgent requirement to
discover a safe, well-tolerated and inexpensive therapeutic option
for GLM.
Previous studies have suggested that expanded
excision (7,8), corticosteroid therapy (8-11)
and anti-tuberculosis therapy (12)
may be effective treatment options for GLM; however, to the best of
our knowledge, no consensus has been reached regarding the most
effective treatment regimen. The aforementioned therapies have
numerous side effects, such as Cushing's syndrome and
immunosuppression following corticosteroid therapy, liver damage or
peripheral neuritis caused by anti-tuberculosis drugs or
deformities of the breast following expanded excision (13,14).
Therefore, discovering a novel treatment that has fewer and less
traumatic side effects remains a major challenge in the treatment
of GLM.
Corynebacterium kroppenstedtii has been
considered the major pathogenic factor for GLM and also the major
causative factor contributing to the unresponsiveness of patients
to routine antibiotics and the recurrence (15-17).
The present study investigated the effect of local heat therapy as
a treatment for GLM. Local heat therapy has been used as an
anti-inflammatory strategy for decades, with efficacy in several
conditions (18); however, to the
best of our knowledge, the present study was the first to report on
the application of local heat therapy for GLM. The present study
investigated the cure rate, recurrence rate and adverse effects of
local heat therapy.
Materials and methods
Study population
Female patients newly diagnosed with GLM by core
needle biopsy and treated by the Department of Breast Surgery, The
Second Affiliated Hospital of Guangzhou Medical University
(Guangzhou, China) between January 2015 and December 2018 were
included in the study for retrospective analysis. This study was
approved by the Ethics Review Board of Guangzhou Medical University
and the Ethics Review Board of The Second Affiliated Hospital of
Guangzhou. Written informed consents were provided by the study
participants and/or their legal guardians (approval no.
2017-ky-ks-11). The exclusion criteria were as follows: i) Other
types of non-lactating mastitis; ii) failure of biopsy or
pathological diagnosis; iii) incomplete medical records; and iv) a
follow-up time of <3 months.
Patients were divided into three groups based on
their treatment protocol: i) Corticosteroid therapy (n=14); ii)
extensive excision (n=21); and iii) local heat therapy groups
(n=39). Patients in the corticosteroid therapy group were
administered 1 mg/kg/day + glucocorticoid + 5 mg/week methotrexate
orally, and dosage reduction was started 2 weeks following the
initiation of the treatment or the stabilization of the disease,
with weekly reductions to the smallest dose that maintained
stabilization of GLM. All patients received a course of
glucocorticoids and methotrexate for >3 months. Patients in the
extensive excision group underwent excision of the entire involved
lobular system, including the posterior lacteal space with a gross
margin clearance of >1 cm of the normal glands. The tumor
plastic technique (19) was used to
repair any defects following the removal of the lesion if
necessary. Patients in the local heat therapy group were requested
to use the automated heating patch (20) on the lesion to maintain the
temperature at 42-65˚C. For patients with multiple lesions, patches
were applied for each lesion. Patches were not placed in direct
contact with the skin to avoid burning and were changed every 3 h
during the day and 6 h during the night. The treatment was
maintained until the disappearance of local symptoms was confirmed
via physical examination and ultrasound or MRI.
Remission was defined as the disappearance of local
symptoms in the breast, including redness, swelling, pain and
fistulas, and reduction in systemic symptoms, such as fever. In
addition, no inflammatory lesions were to be observed by ultrasound
examination.
Criteria for no response to
treatment
The following criteria were used to determine no
response to treatment: i) No response to either corticosteroid or
local heat therapy was defined as a reduction in the lesion of
<20%, an increase in the volume of measurable lesions of >25%
or the appearance of any new lesions following 3 months of
continuous treatment; or ii) the appearance of any new lesions
within the original lesion within 1 month after extensive
excision.
Definition of recurrence
The following definition of recurrence was used in
the present study for both the corticosteroid and local heat
therapy groups: Emergence of new lesion(s) within the range of the
primary location or any other part of the ipsilateral breast 1
month following the termination of therapy.
The following definition of recurrence was used in
the present study for the extensive excision group: The detection
of new lesion(s) within the range of the primary location or any
other part of the ipsilateral breast by ultrasound 1 month
following extensive excision.
Bacterial cultivation and
identification
Tween80 was added to a common blood plate to make a
high-fat blood plate. Pus and blood from the newly diagnosed
patients were evenly precoated on the plate at room temperature for
1 min and tissue was cut in to 1 mm pieces and placed on the plate
within 6 h of collection. Pus and tissue samples were allowed to
grow at 37˚C for 48 h. Bacterial samples were collected and sent to
Life Corporation (Thermo Fisher Scientific, Inc.) for PCR and the
products was purified and extracted for DNA sequencing and sequence
alignment. Routine bacterial identification including fungi,
mycobacteria, anaerobes or aerobes of tissue, blood and pus
collected from the 74 patients was performed in the Germ Lab in The
Second Affiliated Hospital of Guangzhou Medical University
(Guangzhou, China).
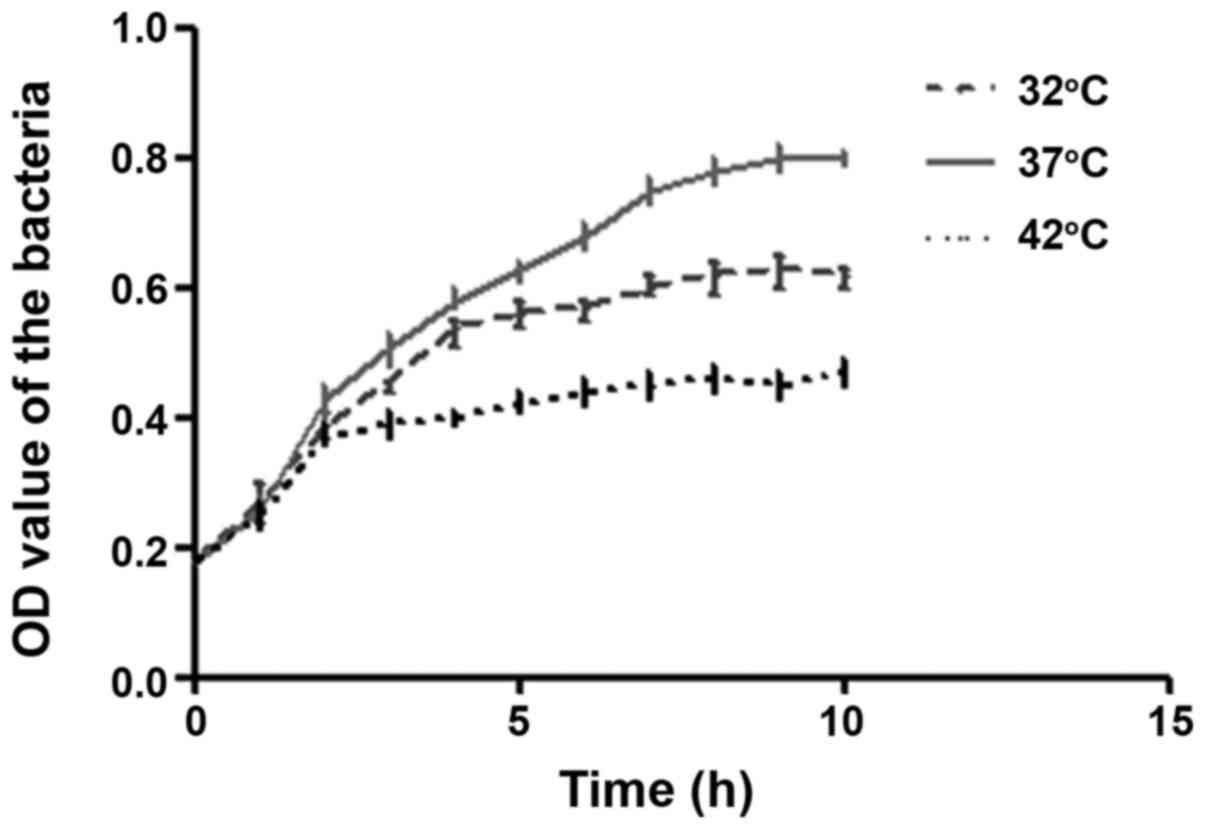
Growth of Corynebacterium
kroppenstedtii
Corynebacterium kroppenstedtii separated from
the tissue was incubated in Luria-Bertani liquid medium
(Sigma-Aldrich; Merck KGaA) at 32, 37 or 42˚C respectively for 72
h. To determine the growth of the bacterium, the optical density at
600 nm of the suspension was measured hourly using a
spectrophotometer system (Tristar2 SLB942; Berthold
Technologies) according to the manufacturer's protocol.
Statistical analysis
SPSS 21.0 software (IBM Corp.) was used to create
the database and R software was used for statistical analysis.
Clinical characteristics were descirbed using median (and
Interquartile range, IQR) or number (and percent) as appropriate.
χ2 tests were used to evaluate the differences in
remission and recurrence rates across the three groups, and used
the Kruskal-Wallis test to determine the intergroup differences in
Corynebacterium kroppenstedtii growth, the remission time.
Dunn's test was used following the Kruskal-Wallis for post-hoc
pairwise comparisons, with P-values adjusted using the
Benjamini-Hochberg method. Estimates with P<0.05 were considered
statistically significant.
Results
Patient characteristics
A total of 74 patients were included in the present
study, all of whom were female; the median follow-up time was 29.5
months (total range, 8-123 months) and the median age was 31.5
years (range, 20-50 years), Among the patients, 66/74 (89.1%) were
married and had children, 5/74 (6.8%) were married but childless
and 3/74 (4.1%) were unmarried and nulliparous. A total of 9/74
(13.2%) had a history of oral contraceptive use and 16/74 (21.6%)
did not lactate normally for reasons including nipple inversion or
reduced milk secretion (Table
I).
 | Table IBaseline characteristics of the
patients (n=74). |
Table I
Baseline characteristics of the
patients (n=74).
| Parameter | Value |
|---|
| Age (years) | |
|
Median
(range) | -31.5 (20-50) |
|
≤25 | 8 (10.8) |
|
25-29 | 20 (27.0) |
|
30-34 | 26 (35.1) |
|
35-40 | 13 (17.6) |
|
>40 | 7 (9.5) |
| Median follow-up
time (range), months | 29.5 (a total of
8-123) |
| Marital or
childbearing status | |
|
Married and
had children | 66 (89.1) |
|
Married but
childless | 5 (6.8) |
|
Unmarried
and without children | 3 (4.1) |
|
Unmarried
with children | 0 (0) |
| History of oral
contraceptives | 9 (13.2) |
| Lactation | |
|
Normal | 58 (78.3) |
|
Abnormal in
either breast | 16 (21.6) |
|
Abnormal in
the diseased breast | 9 (12.2) |
| Location of
lesion | |
|
Left
breast | 39 (52.7) |
|
Right
breast | 29 (39.2) |
|
Bilateral
breasts | 6 (8.1) |
| Involved
quadrant | |
|
Upper
external | 19 (25.7) |
|
Inferior
external | 9 (12.2) |
|
Upper
internal | 20 (27.0) |
|
Inferior
internal | 10 (13.5) |
|
>2 | 16 (21.6) |
| Time interval
between birth and onset of GLM (years) | |
|
≤3 | 50 (67.6) |
|
>3 | 24 (32.4) |
Clinical presentations were well balanced among the
treatment groups. The median maximum diameter of the lesion in the
local heat group was higher compared with that in the
corticosteroid and excision groups (5.00 cm vs. 4.20 cm and 3.70
cm, respectively); however, the differences between the groups were
not significant. In addition, in 22 (56.41%) patients in the local
heat group, 8 (57.14%) patients in the corticosteroid group and 9
(42.86%) patients in the extensive excision group, multiple lesions
were discovered. Furthermore, 7 (50.00%) patients in the
corticosteroid group, 16 (76.19%) patients in the extensive
excision group and 20 (51.28%) patients in the local heat group had
no abscesses. However, there were no significant differences in the
proportion of patients with multiple lesions and abscesses among
the three groups (Table II).
 | Table IIClinical characteristics of the
patients in the three groups. |
Table II
Clinical characteristics of the
patients in the three groups.
| Parameter | Corticosteroids
(n=14) | Extensive excision
(n=21) | Local heat therapy
(n=39) | P-value |
|---|
| Age (years) | 30.93±5.64 | 32.86±6.23 | 32.10±5.90 | 0.645 |
| Maximum diameter
(cm)a | 4.56±1.95 | 3.97±2.37 | 5.11±2.01 | 0.141 |
| Multiplicity of
lesionsb | | | | 0.590 |
|
Multiple | 8 (57.14) | 9 (42.86) | 22 (56.41) | |
|
Single | 6 (42.86) | 12 (57.14) | 17 (43.59) | |
|
Abscessc | | | | 0.165 |
|
No | 7 (50.00) | 16 (76.19) | 20 (51.28) | |
|
Yes | 7 (50.00) | 5 (23.81) | 19 (48.72) | |
Growth of Corynebacterium
kroppenstedtii at different temperatures
Routine bacterial culture was performed to identify
the pathogenic bacteria in the tissue, blood and pus of all
patients of the present study, but no bacteria, including fungi,
mycobacteria, anaerobes or aerobes, were detected in 64/74 (86.5%)
patients of the present study. The other patients were confirmed to
have gram-positive bacterial infections (13.5%). Corynebacterium
kroppenstedtii was discovered to be the major pathogenic
bacterium present in the tissue and pus of 11 patients with GLM
(data not shown). In addition, it was previously suggested that
Corynebacterium kroppenstedtii may be responsible for
multiple recurrence of GLM, and that the inhibition of
Corynebacterium kroppenstedtii may help to control GLM
(17). Therefore, the present study
determined the optimum temperature at which the growth of the
bacteria was inhibited in vitro. the results revealed that
the optimum growth temperature of Corynebacterium
kroppenstedtii was 37˚C, while the growth at 42˚C was markedly
inhibited (Fig. 1).
Comparison of first remission rates
among the different treatments
The first remission rate was compared between the
three groups; among the 14 patients treated with corticosteroids,
12 reached first remission and 2 were non-responsive to the
treatment (85.7%). Among the 39 patients treated with local heat
therapy, 30 cases were cured, while 9 cases were not cured (76.9%).
Among the 21 patients who received expanded excision, 19 reached
remission and 2 did not, and consequently, the remission rate was
90.4%. There were no significant differences in the remission rates
among the three groups (P=0.221; Table III).
 | Table IIIComparison of remission rates among
three different treatments. |
Table III
Comparison of remission rates among
three different treatments.
| Treatment | Reached first
remission (n) | No. remission
(n) | Total (n) | Remission rate
(%) |
|---|
|
Corticosteroids | 12 | 2 | 14 | 85.7 |
| Extensive
excision | 19 | 2 | 21 | 90.4 |
| Local heat
therapy | 30 | 9 | 39 | 76.9 |
Comparison of recurrence rates among
the three different treatments
As for the recurrence rate, the corticosteroid group
had one case of recurrence (8.33%), the expanded excision group had
two cases of recurrence (10%) and three cases of recurrence (10%)
were observed in the local heat therapy group. However, no
significant differences in the recurrence rates were obtained among
the three groups (P=0.985; Table
IV).
 | Table IVComparison of recurrence among three
different treatments. |
Table IV
Comparison of recurrence among three
different treatments.
| Treatment | Recurrence (n) | Primary healing
(n) | Recurrence rate
(%) |
|---|
|
Corticosteroids | 1 | 12 | 8.33 |
| Extensive
excision | 2 | 19 | 10.0 |
| Local heat
therapy | 3 | 30 | 10.0 |
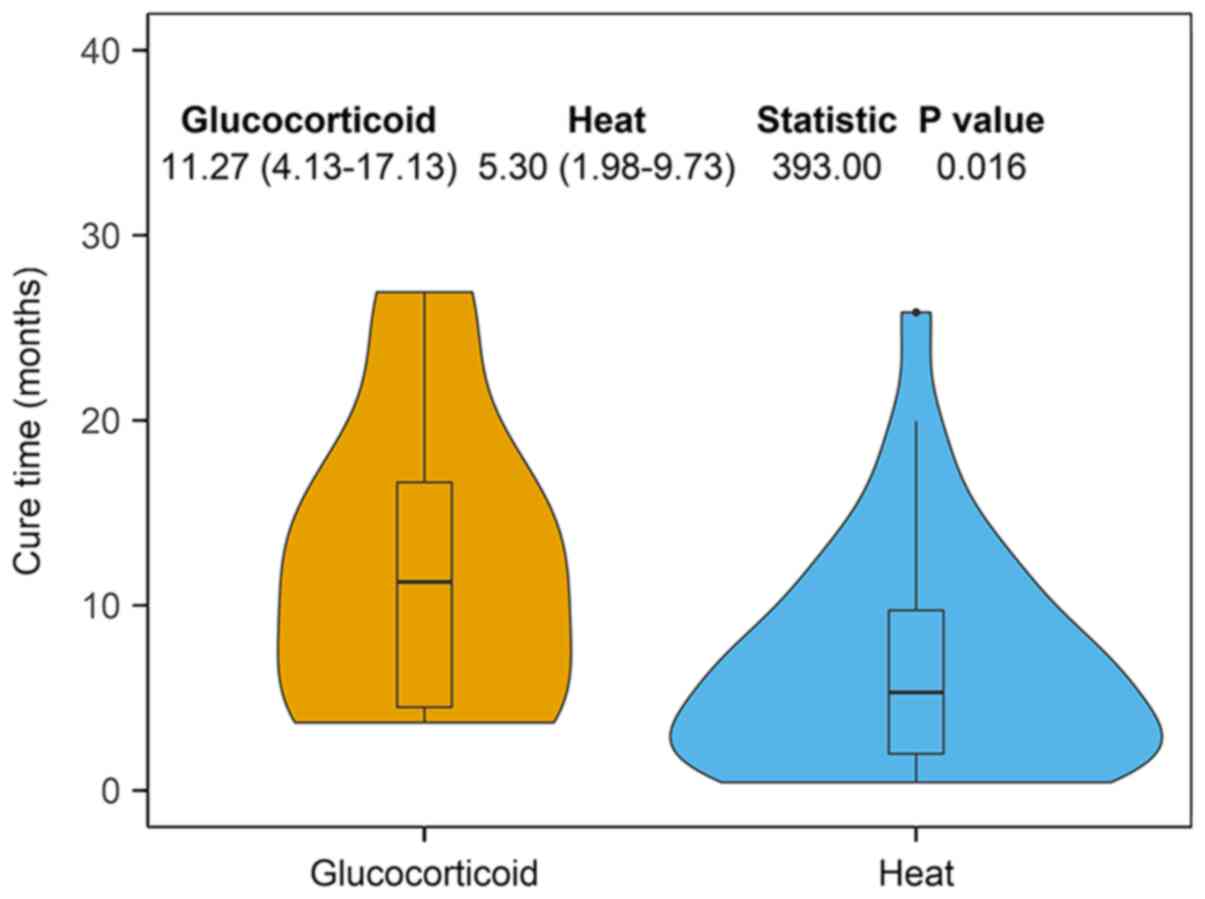
Comparison of first remission time
between corticosteroid therapy and local heat therapy
The median remission time (treatment duration: Time
from initiation of treatment to the first-time remission) between
the corticosteroid and local heat therapy groups was investigated.
The patients receiving local heat therapy had a significantly
reduced remission time compared with those receiving
corticosteroids (5.30 months vs. 11.27 months; P=0.016; Fig. 2).
Side effects
The major side effects observed in the patients with
local heat therapy were redness of the skin and a mild rash
(Table SI), which did not require
extra treatment.
Discussion
GLM is a benign disorder of the breast that is
frequent in females of child-bearing age, but not during the
lactation period (21). Regarding
its occurrence, there is no preferential side of the breast and it
is usually unilateral instead of bilateral (22). The etiology of GLM has yet to be
fully elucidated; however, previous studies have suggested that it
may be associated with the following factors: i) Autoimmunity.
Kessler and Wolloch (23) first
hypothesized that GLM was a type of autoimmune disease, which was
later proved by the fact that the size of the lumps may be reduced
by treatment with glucocorticoids (24); ii) Infection, trauma, physical or
chemical factors. Fletcher et al (25) proposed that trauma, local breast
infection and other physical and chemical factors may stimulate the
breast duct and gland cavity to secrete milk or cause the
exfoliation of keratinized epithelium to the lobule, both of which
may lead to an inflammatory reaction in the lobules of the mammary
gland; and iii) Corynebacterium infection. In 2002, Paviour
et al (26) discovered that
Corynebacterium kroppenstedtii may be cultured from the
non-lactating mastitis tissue of 13/24 patients. In addition, in
2003, Taylor et al (27)
reported a Corynebacterium kroppenstedtii infection in 27/34
patients with GLM. In further studies, Corynebacterium
kroppenstedtii was also confirmed; Wong et al (28) used matrix-assisted laser
desorption/ionization-time-of-flight mass spectrometry to confirm
that Corynebacterium kroppenstedtii was the only pathogenic
bacteria in 39/42 (92.9%) cases. A bioinformatics analysis by Yu
et al (15) revealed that
Corynebacterium was present in patients with GLM, with gene
identification of Corynebacterium kroppenstedtiib ranging
from 1.1 to 58.9% and the predominance of Corynebacterium
kroppenstedtii infection (11/19, 57.9%). The predominance of
Corynebacterium kroppenstedtiib-associated breast specimens
in the present study was consistent with that reported in previous
studies (15,28). Other factors reported included the
use of oral contraceptives (29,30),
breast-feeding related events (31,32),
smoking (33) and α1-antitrypsin
deficiency (34).
As the in vitro experiment of the present
study indicated that the optimum growth temperature for
Corynebacterium kroppenstedtii was 37˚C and its growth was
notably inhibited at 42˚C, local temperature control may result in
growth arrest of Corynebacterium kroppenstedtii. Local heat
therapy has been evaluated as a treatment for inflammation and the
acceleration of wound healing; however, to the best of our
knowledge, the present study was the first trial to assess local
heat therapy as a treatment for GLM. Of note, 30 patients achieved
first remission (76.9%), with no significant differences compared
with the corticosteroid therapy and expanded excision groups.
Concurrently, the healing time following local heat therapy was
only 5.9 months, which was a shorter time compared with that
following corticosteroid therapy. Despite taking into consideration
the gradual tapering time of corticosteroids during treatment, the
differences in the median healing time between the two groups
remained >6 months, suggesting that the differences in the
healing time between local heat therapy and corticosteroids may not
only be explained by the long course of steroids withdrawal, but by
the advantages of local heat therapy itself. Of note, in the
present study, the presence of Corynebacterium was confirmed
in 11/15 patients diagnosed with GLM in both the affected tissue
and pus.
It has been suggested that patients with GLM should
not opt for surgery, as the recurrence rate may be as high as 50%
(35,36). In addition, the inevitable
complications, such as breast deformation and poor wound healing,
limit the application of surgery (9). Regarding the cause of recurrence,
previous studies have ascribed the incompleteness of excision to
the failure of surgical treatment and put forward the concept of
extensive excision of the lesion (8,37),
which has been suggested by several studies as a critical treatment
for GLM, demonstrating an instant remission and providing a
comprehensive pathological diagnosis (8,38).
Schelfout et al (34)
reported a success rate of 90.3% and a recurrence rate of 8.7% with
surgical intervention. In this previous study, extensive excision
was defined as the excision of the lesion and the surrounding
normal gland tissue; the patients experienced little recurrence, as
the lesions reported were mainly a single mass and relatively
small, with an average size of 3.8±2.3 cm. In the present study, a
cure rate of 90.4% was achieved with expanded excision. The
possible reasons for this cure rate were that a total of 10 (47.6%)
cases in this group presented with single, relatively small lumps
(<3 cm), which were easy to surgically remove, and that one
patient opted for mastectomy and breast reconstruction;
furthermore, the cure mentioned here refers to the first remission,
which was defined as the disappearance of local symptoms by
physical examination and imaging examination lasting for 1 month
after the operation. The application of oncoplastic techniques also
makes extensive resection feasible which may lead to a low
recurrence rate. Therefore, these results suggested that surgery
may be suitable for patients with GLM with relatively small single
lumps. Surgery may also be considered for larger lesions, if the
surgeon is skilled in the application of oncoplastic
techniques.
A high recurrence rate is one of the features of GLM
that make it challenging to manage, and recurrence has been
reported for all currently available therapeutic options, including
surgical resection and oral steroids (39). In the present study, certain
patients in the corticosteroid, extensive excision and local heat
therapy groups all experienced recurrence, with rates of 8.3, 10.0
and 10.0%, respectively. However, no significant differences were
present among the three groups. Thus, the recurrence rate in
patients receiving local heat therapy was not increased compared
with that in patients who had received extensive excision or
corticosteroid therapy, which suggested that local heat therapy may
not be inferior to the other two approaches in terms of
recurrence.
The major side effects of local heat therapy were
redness of the skin, a mild rash and the requirement to change the
hot patch frequently. However, all patients were able to tolerate
the above side effects; none of the 39 patients who received local
heat therapy developed severe rash or severe burns to the skin on
the breast. In the corticosteroid group, concentric obesity,
abnormal glucose tolerance and facial acne were the most common
side effects. Expanded excision is not widely used at the early
stage of GLM due to the poor postoperative appearance of the
breast; however, the application of oncoplastic surgery has made
surgical excision a more popular option for patients with GLM
(40). However, due to the loss of
a large volume of the affected breast, contralateral breast
reduction surgery is at times indicated, providing a dilemma for
patients and clinicians. By contrast, local heat therapy does not
markedly affect the appearance and volume of the breast, and even
if the treatment fails, it does not cause any severe psychological
trauma in the patients. However, in certain patients, the remaining
local malformation due to ulceration in the local heat therapy
group may still require surgical adjustment.
As a limitation of the present study, the
combination of local heat therapy with surgery or corticosteroids
therapy was not assessed. It is clear from the present study that
extensive excision caused huge tissue losses in the patients and
recurrence were more frequently observed in the local heat therapy
group than in the other two groups, As such, it is possible that
extensive excision following local heat therapy could reduce the
resection range. While corticosteroid therapy may achieve a prompt
response to reduce the local symptoms, whether the combination of
local heat therapy and corticosteroids could provide rapid control
of local manifestations and reach a quick remission requires to be
further investigated.
Due to the lack of response to routine
anti-inflammatory therapies, high recurrence rates and adverse
effects of the current treatments, GLM remains a refractory
disease. To the best of our knowledge, the present study was the
first to investigate local heat therapy as a treatment option for
patients with GLM, which demonstrated certain advantages over
extensive excision and corticosteroid therapy. Thus, compared with
standard treatments, local heat therapy may be a promising option
to explore due to its low cost, relatively fewer side effects and
similar cure rate, as well as feasibility for all patients.
Supplementary Material
Side-effect of the three
therapies.
Acknowledgements
Not applicable.
Funding
Funding: The present was supported by grants from the Natural
Science Foundation of Guangdong Province (grant no.
2018A030310184). This work was also supported by the Youth Program
of the National Natural Science Foundation of China (grant no.
81802817).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LZ contributed to study design and coordination, and
supervision of the study. XC performed analysis and interpretation
of data; generated all figures and tables; conducted most of the
experiments; drafted and revised the manuscript. QY participated in
data collection and patient follow-up. WZ was responsible for all
statistical analyses. XH, TX TC and HJ performed sample collection.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Review Board
of Guangzhou Medical University and the Ethics Review Board of The
Second Affiliated Hospital of Guangzhou Medical University
(Guangzhou, China). Written informed consent was provided by the
study participants and/or their legal guardians.
Patient consent for publication
Not applicable
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hwang MJ, Rogers A and Vidya R: Idiopathic
granulomatous mastitis: Rare but important. BMJ Case Rep.
2010(bcr1020092334)2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Altintoprak F, Kivilcim T and Ozkan OV:
Aetiology of idiopathic granulomatous mastitis. World J Clin Cases.
2:852–858. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Aslan H, Pourbagher A and Colakoglu T:
Idiopathic granulomatous mastitis: Magnetic resonance imaging
findings with diffusion MRI. Acta Radiol. 57:796–801.
2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mahmodlou R, Dadkhah N, Abbasi F, Nasiri J
and Valizadeh R: Idiopathic granulomatous mastitis: Dilemmas in
diagnosis and treatment. Electron Physician. 9:5375–5379.
2017.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Benson JR and Dumitru D: Idiopathic
granulomatous mastitis: Presentation, investigation and management.
Future Oncol. 12:1381–1394. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Yalcin Kehribar D, Izci Duran T and Ozgen
M: AB1052 Evaluation of symptoms, depression and anxiety levels in
young women with idiopathic granulomatous mastitis. Ann Rheum Dis.
79:1816. 2020.
|
|
7
|
Ahmed YS and Abd El Maksoud W: Evaluation
of therapeutic mammoplasty techniques in the surgical management of
female patients with idiopathic granulomatous mastitis with mild to
moderate inflammatory symptoms in terms of recurrence and patients'
satisfaction. Breast Dis. 36:37–45. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Yabanoglu H, Colakoglu T, Belli S, Aytac
HO, Bolat FA, Pourbagher A, Tezcaner T, Yildirim S and Haberal M: A
comparative study of conservative versus surgical treatment
protocols for 77 patients with idiopathic granulomatous mastitis.
Breast J. 21:363–369. 2015.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mizrakli T, Velidedeoglu M, Yemisen M,
Mete B, Kilic F, Yilmaz H, Ozturk T, Ozaras R, Aydogan F and Perek
A: Corticosteroid treatment in the management of idiopathic
granulomatous mastitis to avoid unnecessary surgery. Surg Today.
45:457–465. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pandey TS, Mackinnon JC, Bressler L,
Millar A, Marcus EE and Ganschow PS: Idiopathic granulomatous
mastitis-a prospective study of 49 women and treatment outcomes
with steroid therapy. Breast J. 20:258–266. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Altintoprak F, Kivilcim T, Yalkin O,
Uzunoglu Y, Kahyaoglu Z and Dilek ON: Topical steroids are
effective in the treatment of idiopathic granulomatous mastitis.
World J Surg. 39:2718–2723. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Farouk O, Abdelkhalek M, Abdallah A, Shata
A, Senbel A, Attia E, Elghaffar MA, Mesbah M, Soliman N, Amin M and
El-Tantawy D: Rifampicin for idiopathic granulomatous lobular
mastitis: A promising alternative for treatment. World J Surg.
41:1313–1321. 2017.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Al-Jarrah A, Taranikanti V, Lakhtakia R,
Al-Jabri A and Sawhney S: Idiopathic granulomatous mastitis:
Diagnostic strategy and therapeutic implications in Omani patients.
Sultan Qaboos Univ Med J. 13:241–247. 2013.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Kaviani A, Vasigh M, Omranipour R,
Mahmoudzadeh H, Elahi A, Farivar L and Zand S: Idiopathic
granulomatous mastitis: Looking for the most effective therapy with
the least side effects according to the severity of the disease in
374 patients in Iran. Breast J. 25:672–677. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yu HJ, Deng H, Ma J, Huang SJ, Yang JM,
Huang YF, Mu XP, Zhang L and Wang Q: Clinical metagenomic analysis
of bacterial communities in breast abscesses of granulomatous
mastitis. Int J Infect Dis. 53:30–33. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tauch A, Fernandez-Natal I and Soriano F:
A microbiological and clinical review on Corynebacterium
kroppenstedtii. Int J Infect Dis. 48:33–39. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Johnson MG, Leal S, Plongla R, Leone PA
and Gilligan PH: The brief case: Recurrent granulomatous mastitis
due to Corynebacterium kroppenstedtii. J Clin Microbiol.
54:1938–1941. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Schmidt KL, Ott VR, Rocher G and Schaller
H: Heat, cold and inflammation. Z Rheumatol. 38:391–404.
1979.PubMed/NCBI
|
|
19
|
Mathapati SN, Goel A, Mehta S, Aggarwal J,
Aravindan R, Nayak V, Panda SK, Pande PK and Kumar K: Oncoplastic
breast reconstruction in breast conservation surgery: Improving the
oncological and aesthetic outcomes. Indian J Surg Oncol.
10:303–308. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Klarzak I, Ura-Bińczyk E, Płocińska M and
Jurczyk-Kowalska M: Effect of temperature and humidity on heat
effect of commercial chemical warmers based on iron powder. Therm
Sci Eng Prog. 6:87–94. 2018.
|
|
21
|
Mathew M, Siwawa P and Misra S: Idiopathic
granulomatous mastitis: An inflammatory breast condition with
review of the literature. BMJ Case Rep.
2015(bcr2014208086)2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Atak T, Sagiroglu J, Eren T, Ali Ozemir I
and Alimoglu O: Strategies to treat idiopathic granulomatous
mastitis: Retrospective analysis of 40 patients. Breast Dis.
35:19–24. 2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kessler E and Wolloch Y: Granulomatous
mastitis: A lesion clinically simulating carcinoma. Am J Clin
Pathol. 58:642–646. 1972.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Allen SG, Soliman AS, Toy K, Omar OS,
Youssef T, Karkouri M, Ayad E, Abdel-Aziz A, Hablas A, Tahri A, et
al: Chronic mastitis in egypt and morocco: Differentiating between
idiopathic granulomatous mastitis and IgG4-related disease. Breast
J. 22:501–509. 2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Fletcher A, Magrath IM, Riddell RH and
Talbot IC: Granulomatous mastitis: A report of seven cases. J Clin
Pathol. 35:941–945. 1982.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Paviour S, Musaad S, Roberts S, Taylor G,
Taylor S, Shore K, Lang S and Holland D: Corynebacterium species
isolated from patients with mastitis. Clin Infect Dis.
35:1434–1440. 2002.PubMed/NCBI View
Article : Google Scholar
|
|
27
|
Taylor GB, Paviour SD, Musaad S, Jones WO
and Holland DJ: A clinicopathological review of 34 cases of
inflammatory breast disease showing an association between
corynebacteria infection and granulomatous mastitis. Pathology.
35:109–119. 2003.PubMed/NCBI
|
|
28
|
Wong SCY, Poon RWS, Chen JHK, Tse H, Lo
JYC, Ng TK, Au JCK, Tse CWS, Cheung IYY, Yuk MT, et al:
Corynebacterium kroppenstedtii is an emerging cause of
mastitis especially in patients with psychiatric illness on
antipsychotic medication. Open Forum Infect Dis.
4(ofx096)2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Oran ES, Gurdal SO, Yankol Y, Öznur M,
Calay Z, Tunacı M and Soybir GR: Management of idiopathic
granulomatous mastitis diagnosed by core biopsy: A retrospective
multicenter study. Breast J. 19:411–418. 2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gurleyik G, Aktekin A, Aker F, Karagulle H
and Saglamc A: Medical and surgical treatment of idiopathic
granulomatous lobular mastitis: A benign inflammatory disease
mimicking invasive carcinoma. J Breast Cancer. 15:119–123.
2012.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Al-Khaffaf B, Knox F and Bundred NJ:
Idiopathic granulomatous mastitis: A 25-year experience. J Am Coll
Surg. 206:269–273. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sakurai K, Fujisaki S, Enomoto K, Amano S
and Sugitani M: Evaluation of follow-up strategies for
corticosteroid therapy of idiopathic granulomatous mastitis. Surg
Today. 41:333–337. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ozel L, Unal A, Unal E, Kara M, Erdoğdu E,
Krand O, Güneş P, Karagül H, Demiral S and Titiz MI: Granulomatous
mastitis: Is it an autoimmune disease? Diagnostic and therapeutic
dilemmas. Surg Today. 42:729–733. 2012.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Schelfout K, Tjalma WA, Cooremans ID,
Coeman DC, Colpaert CG and Buytaert PM: Observations of an
idiopathic granulomatous mastitis. Eur J Obstet Gynecol Reprod
Biol. 97:260–262. 2001.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Hovanessian Larsen LJ, Peyvandi B, Klipfel
N, Grant E and Iyengar G: Granulomatous lobular mastitis: Imaging,
diagnosis, and treatment. AJR Am J Roentgenol. 193:574–581.
2009.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Lin CH, Hsu CW, Tsao TY and Chou J:
Idiopathic granulomatous mastitis associated with
risperidone-induced hyperprolactinemia. Diagn Pathol.
7(2)2012.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Zhang Y, Zhou Y, Mao F, Guan J and Sun Q:
Clinical characteristics, classification and surgical treatment of
periductal mastitis. J Thorac Dis. 10:2420–2427. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Li J: Diagnosis and treatment of 75
patients with idiopathic lobular granulomatous mastitis. J Invest
Surg. 32:414–420. 2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Lei X, Chen K, Zhu L, Song E, Su F and Li
S: Treatments for idiopathic granulomatous mastitis: Systematic
review and meta-analysis. Breastfeed Med. 12:415–421.
2017.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Hladik M, Schoeller T, Ensat F and
Wechselberger G: Idiopathic granulomatous mastitis: Successful
treatment by mastectomy and immediate breast reconstruction. J
Plast Reconstr Aesthet Surg. 64:1604–1607. 2011.PubMed/NCBI View Article : Google Scholar
|