1. Introduction
Since late December, 2019, humanity has been facing
an unprecedented situation due to the coronavirus disease 2019
(COVID-19) outbreak which began in Wuhan, China. COVID-19 is a
highly contagious disease, caused by severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2), which has evolved into an
ongoing pandemic (1). The World
Health Organization declared this viral infection as a public
health emergency of international concern on January 31, 2020
(https://bit.ly/2Tud4mX) and as a pandemic on
March 11, 2020 (https://bit.ly/3qF3IRA). Eighteen months into this
unprecedented and rapidly evolving situation, according to the
latest data, the pandemic has led to >195 million cases with
confirmed SARS-CoV-2 infection and to >4.1 million deaths
worldwide (https://bit.ly/2TktAGl). Despite the
extensive commitment from the global biopharmaceutical industry to
address COVID-19 and its rapid development, and the worldwide
distribution of several vaccines with demonstrated efficacy in
preventing symptomatic infections and COVID-19 related admissions
to hospital and deaths (2), there
is currently no available medication for the effective treatment of
the disease; thus, clinical management relies on symptomatic
relief, supportive care and isolation. There is, also, uncertainty
as regards the long-lasting immunity and potential long-term
adverse effects of the vaccines, the duration of the pandemic and
the extent of the effects of the pandemic on the mental health of
the world's population. Moreover, the precautionary restrictive
measures taken to control the spread of the virus, ranging from
social distancing to strict lockdown regulations, have created an
insecure and stressful environment at all levels, health, economic
and social (3). Stressful
situations, such as the intense insecurity of a contagious
life-threating virus, fear of being infected or having contracted
the virus, being hospitalized with less or more severe COVID-19,
being admitted to an intensive care unit (ICU), the loss of a loved
one, mandatory and drastic changes to everyday life with uncertain
financial and future prospects, alongside insufficient coping
skills and stress management strategies (4), have all contributed to posing a
significant burden on the mental health of individuals (5-7).
These situations and may also be perceived as traumatic events
(8). Studies have suggested that
health-related pandemic disasters may lead to post-traumatic stress
disorder (PTSD) symptomatology (9-11),
a mental health impact described as the ‘second tsunami’ in the
SARS-CoV-2 pandemic (12). The
COVID-19 pandemic is a potentially traumatic event given its
characteristics (unpredictable, extreme, prolonged, based on an
unknown/unfamiliar danger, posing threat of death). However,
according to the Diagnostic and Statistical Manual of Mental
Disorders (DSM-5), only some individuals may meet the qualifying
trauma exposure criteria for PTSD as a result of the pandemic and
these are the following: Those who have themselves suffered from
severe COVID-19 illness and potential death; individuals who, as
family members and health care workers, have witnessed the
suffering and death of others; individuals who have learned of the
death or risk of death of a family member or friend due to the
virus; and individuals who have experienced extreme exposure to
aversive details (e.g., first responders and hospital personnel).
The DSM-5 diagnosis of PTSD requires the presence of symptoms from
the following four symptom clusters: Intrusion symptoms associated
with traumatic event(s); persistent avoidance of stimuli associated
with traumatic event(s); negative alterations in cognition and mood
associated with traumatic event(s); and marked alterations in
arousal and reactivity associated with traumatic event(s)
commencing or becoming more severe following the occurrence of
traumatic event(s) (13).
2. Neuropsychiatric manifestations of
SARS-CoV-2
An association between psychological distress and
the neuropathological manifestations of the disease has already
been suggested, as patients with COVID-19 have consistently been
shown to exhibit significantly higher levels of anxiety, depression
and stress-related disorders when compared with non-COVID-19
subjects (14). Indeed, apart from
the prominent respiratory symptoms, SARS-CoV-2 has been shown to
induce neurological and neuropsychiatric manifestations that vary
both in intensity and duration; neurological symptoms include
headaches, dizziness, hyposmia or anosmia, ageusia, ataxia,
seizures, encephalitis, encephalopathy, sensory impairment, cranial
neuropathies, acute cerebrovascular disease, para-infectious
peripheral nerve-related disorders, such as Guillain-Barré and
Miller Fisher syndromes, and in certain cases, neuronal
autoimmunity (15,16). Neuropsychiatric symptoms include
cognitive decline, confusion, delirium, dementia, insomnia,
anxiety, depression and psychotic spectrum disorders (17-19).
Viral neurotropism has already been documented for
coronaviruses SARS-CoV-1 and Middle East respiratory syndrome
(MERS-CoV). However, there is no sufficient evidence to also
support the neuro-invasive potential of SARS-CoV-2 (16,19,20);
most arguably, the virus interacts with the angiotensin converting
enzyme 2 (ACE2) receptor on host cells to facilitate entry. Neural
cells expressing ACE2 are found in circumventricular organs that
are involved in cardiovascular and respiratory regulation, and have
little or no protection of the blood brain barrier (BBB), thus
representing central nervous system (CNS) sites that are quite
vulnerable to viral infection (18). Clinical presentations of PTSD,
depression, pain disorder, panic disorder and obsessive-compulsive
disorder in survivors with SARS-CoV-1 have been shown to be
markedly increased at 31-50 months post-infection, as compared with
their prevalence pre-infection (19,21).
Similarly, patients with COVID-19 have been found to present with a
significantly higher incidence of an altered mental status, mood
disorders, insomnia, anxiety and dementia, while the risk of
developing a post-infectious psychiatric disorder appears to be
~2-fold higher when compared with pre-infection rates (22-24).
In individuals with a predisposition to stress-related disorders or
with pre-existing neuropsychiatric conditions, SARS-CoV-2 can
accelerate the development of significant psychiatric disorders,
with significant implications for optimal medical and psychiatric
care (14,18).
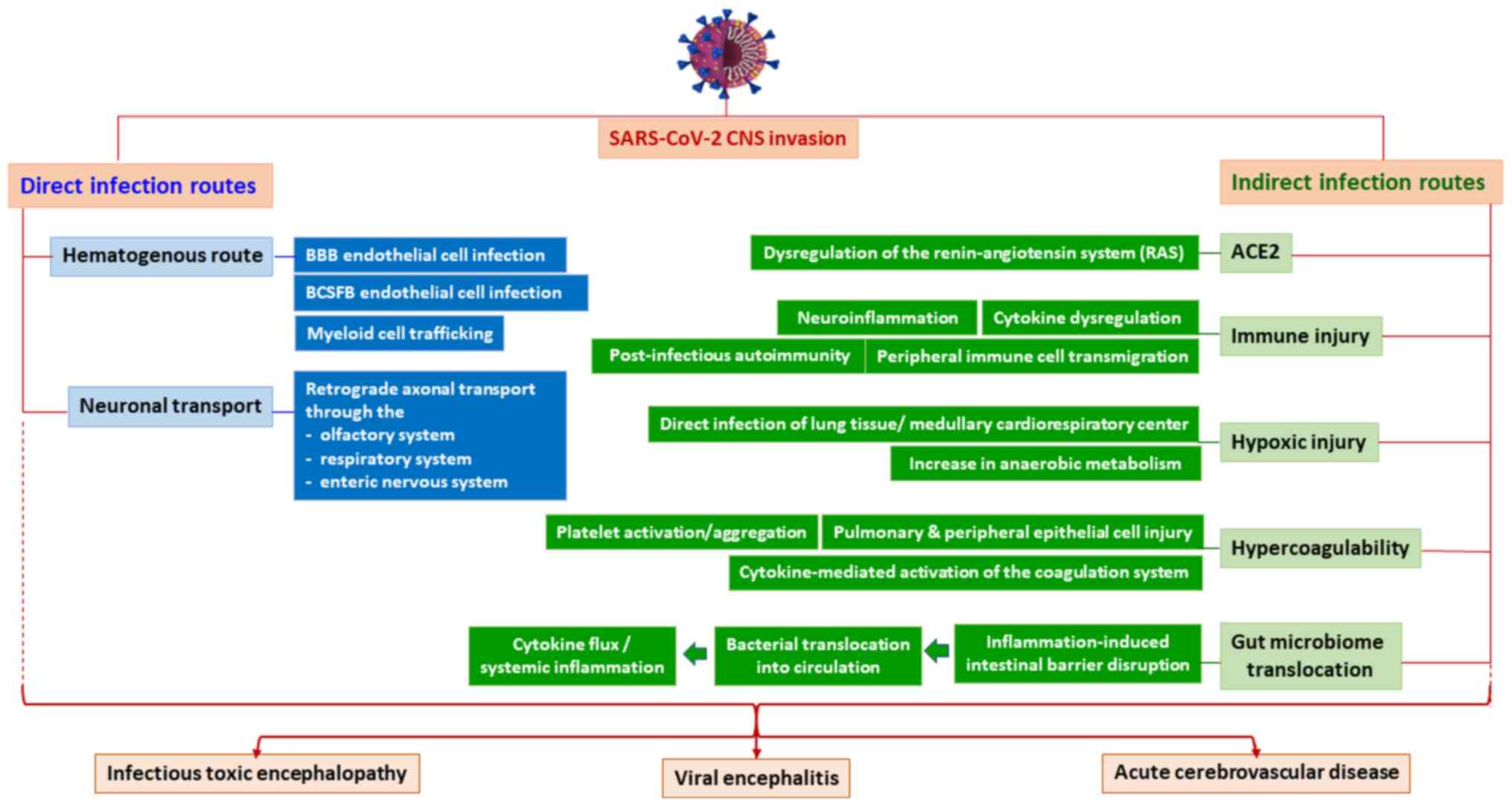
Even though the exact mechanisms of
COVID-19-associated neuropsychiatric symptoms are not well known,
neurotropic activity manifests as a viral infection of the nervous
tissue and has been postulated to occur via two possible pathways:
i) A hematogenous route, which may include the infection of BBB
endothelial cells, infection of the blood-cerebrospinal fluid
barrier epithelial cells, or via myeloid cell trafficking, a
process that essentially utilizes inflammatory cells as Trojan
horses to gain access to the CNS; ii) a neuronal transport route
which uses retrograde axonal transport through the olfactory, the
respiratory and the enteric nervous system (15,25).
CNS invasion may also occur via deregulated inflammatory responses,
such as cytokine dysregulation and neuroinflammation, which may
increase BBB permeability, thereby facilitating viral entry, or as
a secondary effect of other organ system failure, such as
cardiorespiratory failure, or secondary to the embolic process
triggered by SARS-CoV-2 (15,18,25).
Furthermore, as certain anti-viral drugs, including chloroquine,
have already been shown to cause CNS-related adverse events, both
neurological and neuropsychiatric, it is possible that, in the
context of COVID-19, such treatments may contribute towards
increasing neuronal stress and neuroinflammation, ultimately
causing neuronal damage that is associated with neuropsychiatric
disturbances (14,26). A more-detailed overview of the
direct and indirect pathways of SARS-CoV-2 CNS invasion is
illustrated in Fig. 1.
3. COVID-19 trauma and post-traumatic stress
disorder in children and adolescents
The risk of the negative psychosocial effects of the
pandemic on the psychological well-being of young individuals has
been highlighted (27,28). The majority of children and
adolescents exposed to traumatic events develop short-term
psychological distress (29);
however, in some, particularly in those living in families facing a
prolonged complex and stressful situation, symptoms do not remit
spontaneously and instead become clinically significant, persistent
and impairing (30).
In the context of prior pandemics, a study on
families who were quarantined due to SARS or the H1N1 influenza
virus and based on parental reports, PTSD was found in 30% of the
confined children and in 25% of the parents; this indicated the
high traumatic potential of social isolation and living in
conditions of constant fear of the disease spreading (31). Longer durations of quarantine have
been shown to be associated with an increased prevalence of
PTSD-related symptoms. Indirect or direct exposure to another
individual with a diagnosis of SARS has also been shown to be
associated with PTSD and depressive symptoms (10). In addition, a study on
home-quarantined youth in China during the first month of the
COVID-19 outbreak revealed that 12.8% of the participants had
traumatic stress levels consistent with PTSD, exhibiting an
association with negative coping styles (32). Furthermore, a recent systematic
review and meta-analysis estimated the pooled prevalence of PTSD to
be 20.7% among Chinese children (33).
Although the COVID-19 pandemic, as mentioned above,
is not associated with the development of PTSD in everyone, the
pandemic situation increases the risk of multiple traumatic
experiences and complex trauma (34). For children living in socially
disadvantaged environments characterized by poverty, the lack of
access to developmentally appropriate resources, low levels of
stimulation and responsive care, or inadequate supervision, the
pandemic situation, by aggravated circumstances, may become an
adverse childhood experience, generating toxic levels of stress
(28).
There is growing neuroscientific evidence to
document that early adverse childhood experiences, including
prenatal stress and stress throughout childhood, have marked and
long-term effects on the development of neurobiological systems
(i.e., fronto-limbic circuitry), thereby ‘programming’ subsequent
increased stress reactivity and weaker emotion regulation (35). This altered neurobiological
response to stress may confer vulnerability to the development of
chronic trauma and stress-related disorders, such as PTSD, anxiety,
mood and attachment disorders, memory and learning problems, as
well as other psychopathological conditions (36).
The COVID-19 pandemic has been described as a
‘perfect storm’ with exposure to known risks and the lack of
support affecting the mental health of young individuals and their
families (37). First, prolonged
lockdown and severe financial difficulties necessitate changes in
family dynamics, which may trigger the use of dysfunctional
caregiver coping strategies (e.g., alcohol or substance abuse),
family discord, negative parent-child interactions, intrafamilial
violence and child abuse (38-40).
For young children, unsafe living conditions, in parallel with
delays in scheduled healthcare visits and developmental checks, the
suspension or interruption of interventions for developmental
delays (e.g., language), lost access to child care and early
education programs, the disruption of support offered by social
services and the loss of supportive social networks, may adversely
affect brain development, leading to long-term negative health
outcomes (41). Second, for
school-aged children and adolescents affected by adverse
experiences in early life, i.e., neglect and child abuse or
exposure to violence, automatic physiological responses are likely
to be reactivated and may further increase the risk of developing
PTSD and stress-related disorders. Third, exposure to increased
levels of depression, anxiety and psychological distress in
adults/caregivers (42), which are
potential factors of adversity for cohabiting children and
adolescents, may lead to secondary trauma and persistent or
delayed-onset distress symptoms. Fourth, given that adolescence is
a particularly stressful period due to the occurrence of related
developmental changes, such as a marked increase in social
sensitivity and interpersonal stress coupled with low tolerance to
frustration, a heightened emotional reactivity and a low capacity
to effectively engage in cognitive and emotion regulation (43,44),
the COVID-19 pandemic, and in particular the prolonged lockdown,
may increase the levels of stress in adolescents. Social isolation,
the lack of face-to-face contact with peers and teachers due to
school closures, a change in daily behaviors (decreased physical
activity, increased screen time, irregular sleep patterns and less
appropriate diets) and concern for the economic future of their
family and country, are among some of the identified
pandemic-related stressors that generate psychological
repercussions in adolescents (45). A recent study examining the impact
of the pandemic, and its related restrictions, on the emotional
health of Canadian adolescents found that concerns related to
COVID-19, difficulties with online learning and increased family
conflict were associated with higher levels of depression and
anxiety, whereas feeling socially connected during the COVID-19
lockdown protected the adolescents against poor mental health
(46). Given that different types
of trauma exposure (e.g., interpersonal or non-interpersonal)
probably have differential effects on adolescent cognition and
traumatic- and stress-related symptoms, as well as PTSD onset
(47-50),
and that adolescents rely on peer connections and relationships for
their emotional support and social development (51), it is argued that social isolation
and social distancing may be an important adversity factor for
developing brain systems engaged in social and emotional processes
(44). Although it may take years
and numerus research studies to fully understand the sequelae of
the COVID-19 pandemic during different developmental stages,
available data have consistently demonstrated an association of
several COVID-19-related stressors with mental health outcomes.
Future studies are required to explore these stressors in
conjunction with protective factors and prospective changes in
mental health to identify which of these may influence both the
typical trajectory of COVID-19-related traumatic experience and the
development of psychopathology in the long-term, as well as to
determine the underlying mechanisms.
4. Post-traumatic stress disorder and
COVID-19 survivors
Scientific evidence from previous epidemics
indicates that a severe physical illness can lead to the
development of various psychiatric conditions, including, among
others, PTSD symptoms following recovery. According to a previous
meta-analysis, 17-44% of critical illness survivors, particularly
those who required hospitalization and/or admission to an ICU,
reported clinically significant PTSD symptoms (52). Due to the fact that the severity of
the medical condition seems to be a predicting factor for the
development of PTSD symptomatology, the early identification of
vulnerable and high-risk patients seems a perquisite for timely
effective interventions (53).
A previous literature review on past coronavirus
outbreaks, suggested a high likelihood of COVID-19 survivors
developing psychiatric symptoms and disorders, most notably PTSD
symptoms (54). Even among
individuals who do not meet the full diagnostic criteria for PTSD,
post-traumatic stress symptoms (PTSS) have also been shown to be
associated with functional impairment (55). As also previously indicated, 42% of
individuals who survived MERS presented scores which were above the
clinical cut-off for PTSD at 1 year following the outbreak, and
almost 26% of individuals who survived SARS met the full diagnostic
criteria for PTSD at 30 months following the outbreak (56,57).
In addition, hospitalization is a potentially
traumatic experience, particularly in severe cases (58). In spite of this, the vast amount of
available research on COVID-19 and mental health is focused on
health professionals and the general population. Studies involving
hospitalized patients have mainly focused on treatments for the
disease (59) and limited
information has been reported regarding potential mental health
outcomes. Hospitalization, in general, and more specifically, the
admission to an ICU may impose a significant burden on the mental
health of patients and may lead to the development of diverse
conditions, including PTSD and other trauma- and stress-related
disorders. Indeed, the highest PTSD rates have been found among
patients who had experienced a life-threatening situation in an ICU
(14-59%), while the lowest rates were childbirth-related (1.7-5.6%)
(60). Hospitalization likely
increases the perception of how critical an event is for the lives
of individuals, which is usually associated with increased
post-traumatic stress (61). In
addition, exposure to the severity and life-threatening aspects of
the infection may also lead to higher levels of stress and
associated reactions (62). This
is reasonable, as the development of more severe symptoms may
result in an enhanced experience of threat, particularly for
symptoms such as dyspnea. Indeed, symptom load was associated with
higher levels of post-traumatic stress reactions (6). Patients in the ICU have been found to
experience traumatic stress related to both the severity of
symptoms and the invasiveness of the medical procedures, which may
lead to the development of PTSD symptomatology. In particular,
respiratory symptoms can cause significant distress and fear of
respiratory failure (63). Other
factors potentially related to PTSD symptomatology include a fear
of death, pain from medical interventions, such as endotracheal
intubation, a limited ability to communicate and feelings of a loss
of control (64). A study among
hospitalized patients with COVID-19 indicated that almost 20% of
the participants developed significant PTSS within 1 month
following hospitalization, which was significantly associated with
the length of the hospitalization period and the resulting feelings
of social disconnection and mental exhaustion (65). Another study reported a 13.2%
prevalence of PTSD among hospitalized patients who were affected by
reports of negative news, had a greater exposure to traumatic
experiences and lower levels of perceived social support (59). These rates are lower than the
prevalence reported by studies on patients with similar infectious
diseases, although higher than those in other groups, such as
medical residents and medical staff, during the COVID-19 pandemic
(66). These findings suggest that
hospitalized patients with COVID-19 infection may present with the
most adverse mental health issues during this pandemic.
In addition, it has been suggested that a
sub-threshold diagnosis of PTSD can be considered a risk factor for
more severe mental health outcomes, and more specifically, with an
increased risk of depression, suicidal ideation, alcohol
consumption and other comorbidities (67). Notably, male gender seems to be a
significant protective factor against PTSD. On the other hand, the
strongest predictor for the development of PTSD among hospitalized
patients with COVID-19 infection appears to be a pre-existing
mental health condition (mainly anxiety and depressive disorders),
followed by obesity, which similar to chronic pulmonary disease,
lead to an increased risk of developing severe disease (58). PTSD, depression and anxiety
disorders are often comorbid, linked to high levels of general
distress in the acute stage of trauma and are described as a
‘symptom network’ (59,68).
To summarize, the severity of the medical condition
has the potential to determine the future risk of patients to
develop PTSD. Research into COVID-19-related PTSD symptomatology
and its determinants is of paramount importance in identifying
possible modifiable risk factors and vulnerable patients, as well
as in evidence-informed decision-making interventions (53). Moreover, effective professional
mental health services should be designed to support the
psychological wellbeing of inpatients with COVID-19, and
particularly those who required hospitalization and/or ICU
care.
5. Conclusion
The present review demonstrates that COVID-19 has a
substantial impact on mental health and poses a significant risk
for the development of trauma-related disorders, including PTSD
among individuals who are most vulnerable, such as children,
adolescents and COVID-19 survivors (who required hospitalization
and/or ICU admission). Therefore, the prompt identification of
at-risk populations, early intervention and the effective
management of PTSD is of utmost importance. A multi-disciplinary
approach should be adopted aiming at enhancing the resilience and
coping mechanisms of different sub-groups through early
identification, prevention and the implementation of intervention
strategies. Lessons learnt from past pandemics together with the
ongoing research on COVID-19 and its mental health consequences
highlight the need for evidence-based targeted and proactive mental
health interventions aiming at minimizing the potential risks and
vulnerabilities.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
IG, SG, EK, MA, IT, SK wrote the original draft,
edited and critically revised the manuscript. ER, KT, EA, NS, VZ
and DAS critically revised and edited the manuscript. IG and ER
confirm the authenticity of all the raw data. All authors
substantially contributed to the conception, writing and revision
of the work and approved the final content of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong
Y, Ren R, Leung KSM, Lau EHY, Wong JY, et al: Early Transmission
Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia.
N Engl J Med. 382:1199–1207. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Blumental S and Debré P: Challenges and
Issues of Anti-SARS-CoV-2 Vaccines. Front Med (Lausanne).
8(664179)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tsamakis K, Tsiptsios D, Ouranidis A,
Mueller C, Schizas D, Terniotis C, Nikolakakis N, Tyros G,
Kympouropoulos S, Lazaris A, et al: COVID-19 and its consequences
on mental health (Review). Exp Ther Med. 21(244)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Agorastos A, Tsamakis K, Solmi M, Correll
CU and Bozikas VP: The need for holistic, longitudinal and
comparable, real-time assessment of the emotional, behavioral and
societal impact of the COVID-19 pandemic across nations.
Psychiatriki. 32:15–18. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Einvik G, Dammen T, Ghanima W, Heir T and
Stavem K: Prevalence and Risk Factors for Post-Traumatic Stress in
Hospitalized and Non-Hospitalized COVID-19 Patients. Int J Environ
Res Public Health. 18(2079)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gautam M, Kaur M and Mahr G:
COVID-19-Associated Psychiatric Symptoms in Health Care Workers:
Viewpoint From Internal Medicine and Psychiatry Residents.
Psychosomatics. 61:579–581. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Tsamakis K, Triantafyllis AS, Tsiptsios D,
Spartalis E, Mueller C, Tsamakis C, Chaidou S, Spandidos DA, Fotis
L, Economou M, et al: COVID-19 related stress exacerbates common
physical and mental pathologies and affects treatment (Review). Exp
Ther Med. 20:159–162. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang L, Pan R, Cai Y and Pan J: The
Prevalence of Post-Traumatic Stress Disorder in the General
Population during the COVID-19 Pandemic: A Systematic Review and
Single-Arm Meta-Analysis. Psychiatry Investig. 18:426–433.
2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jeong H, Yim HW, Song YJ, Ki M, Min JA,
Cho J and Chae JH: Mental health status of people isolated due to
Middle East Respiratory Syndrome. Epidemiol Health.
38(e2016048)2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hawryluck L, Gold WL, Robinson S, Pogorski
S, Galea S and Styra R: SARS control and psychological effects of
quarantine, Toronto, Canada. Emerg Infect Dis. 10:1206–1212.
2004.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Asukai N, Kato H, Kawamura N, Kim Y,
Yamamoto K, Kishimoto J, Miyake Y and Nishizono-Maher A:
Reliability and validity of the Japanese-language version of the
impact of event scale-revised (IES-R-J): Four studies of different
traumatic events. J Nerv Ment Dis. 190:175–182. 2002.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Dutheil F, Mondillon L and Navel V: PTSD
as the second tsunami of the SARS-Cov-2 pandemic. Psychol Med.
51:1773–1774. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
American Psychiatric Association (APA):
Diagnostic and Statistical Manual of Mental Disorders
(DSM-5®). APA, Washington, DC, 2013.
|
|
14
|
Jansen van Vuren E, Steyn SF, Brink CB,
Möller M, Viljoen FP and Harvey BH: The neuropsychiatric
manifestations of COVID-19: Interactions with psychiatric illness
and pharmacological treatment. Biomed Pharmacother.
135(111200)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yapici-Eser H, Koroglu YE, Oztop-Cakmak O,
Keskin O, Gursoy A and Gursoy-Ozdemir Y: Neuropsychiatric Symptoms
of COVID-19 Explained by SARS-CoV-2 Proteins' Mimicry of Human
Protein Interactions. Front Hum Neurosci. 15(656313)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Orsini A, Corsi M, Santangelo A, Riva A,
Peroni D, Foiadelli T, Savasta S and Striano P: Challenges and
management of neurological and psychiatric manifestations in
SARS-CoV-2 (COVID-19) patients. Neurol Sci. 41:2353–2366.
2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Troyer EA, Kohn JN and Hong S: Are we
facing a crashing wave of neuropsychiatric sequelae of COVID-19?
Neuropsychiatric symptoms and potential immunologic mechanisms.
Brain Behav Immun. 87:34–39. 2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Steardo L Jr, Steardo L and Verkhratsky A:
Psychiatric face of COVID-19. Transl Psychiatry.
10(261)2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nakamura ZM, Nash RP, Laughon SL and
Rosenstein DL: Neuropsychiatric Complications of COVID-19. Curr
Psychiatry Rep. 23(25)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Rogers JP, Chesney E, Oliver D, Pollak TA,
McGuire P, Fusar-Poli P, Zandi MS, Lewis G and David AS:
Psychiatric and neuropsychiatric presentations associated with
severe coronavirus infections: A systematic review and
meta-analysis with comparison to the COVID-19 pandemic. Lancet
Psychiatry. 7:611–627. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lam MH, Wing YK, Yu MW, Leung CM, Ma RC,
Kong AP, So WY, Fong SY and Lam SP: Mental morbidities and chronic
fatigue in severe acute respiratory syndrome survivors: Long-term
follow-up. Arch Intern Med. 169:2142–2147. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Taquet M, Luciano S, Geddes JR and
Harrison PJ: Bidirectional associations between COVID-19 and
psychiatric disorder: Retrospective cohort studies of 62,354
COVID-19 cases in the USA. Lancet Psychiatry. 8:130–140.
2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ng JH, Sun A, Je HS and Tan EK:
Unravelling Pathophysiology of Neurological and Psychiatric
Complications of COVID-19 Using Brain Organoids. Neuroscientist:
May 26, 2021 (Epub ahead of print).
|
|
24
|
Guo Q, Zheng Y, Shi J, Wang J, Li G, Li C,
Fromson JA, Xu Y, Liu X, Xu H, et al: Immediate psychological
distress in quarantined patients with COVID-19 and its association
with peripheral inflammation: A mixed-method study. Brain Behav
Immun. 88:17–27. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Rege S: COVID-19 and the
Brain-Pathogenesis and Neuropsychiatric Manifestations of
SARS-CoV-2 CNS Involvement. Psych Scene hub, 2020. https://psychscenehub.com/psychinsights/covid-19-and-the-brain-pathogenesis-and-neuropsychiatric-manifestations-of-sars-cov-2-cns-involvement/.
Accessed May 17, 2020.
|
|
26
|
Juurlink DN: Safety considerations with
chloroquine, hydroxychloroquine and azithromycin in the management
of SARS-CoV-2 infection. CMAJ. 192:E450–E453. 2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Dalton L, Rapa E and Stein A: Protecting
the psychological health of children through effective
communication about COVID-19. Lancet Child Adolesc Health.
4:346–347. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Holmes EA, O'Connor RC, Perry VH, Tracey
I, Wessely S, Arseneault L, Ballard C, Christensen H, Cohen Silver
R, Everall I, et al: Multidisciplinary research priorities for the
COVID-19 pandemic: A call for action for mental health science.
Lancet Psychiatry. 7:547–560. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Danese A, Smith P, Chitsabesan P and
Dubicka B: Child and adolescent mental health amidst emergencies
and disasters. Br J Psychiatry. 216:159–162. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Yule W, Perrin S and Smith P: Traumatic
events and post-traumatic stress disorder. In: Cambridge child and
adolescent psychiatry. Anxiety disorders in children and
adolescents: Research, assessment and intervention. Silverman WK
and Treffers PDA (eds). Cambridge University Press, Cambridge,
pp212-234, 2001.
|
|
31
|
Sprang G and Silman M: Posttraumatic
stress disorder in parents and youth after health-related
disasters. Disaster Med Public Health Prep. 7:105–110.
2013.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Liang L, Gao T, Ren H, Cao R, Qin Z, Hu Y,
Li C and Mei S: Post-traumatic stress disorder and psychological
distress in Chinese youths following the COVID-19 emergency. J
Health Psychol. 25:1164–1175. 2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Ma Z, Idris S, Zhang Y, Zewen L, Wali A,
Ji Y, Pan Q and Baloch Z: The impact of COVID-19 pandemic outbreak
on education and mental health of Chinese children aged 7-15 years:
An online survey. BMC Pediatr. 21(95)2021.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Vézina D, Brend D and Beeman I: When it
counts the most: Trauma-informed care and the COVID-19 global
pandemic. Dev Child Welf. 2:172–179. 2020.
|
|
35
|
Herringa RJ: Trauma, PTSD, and the
Developing Brain. Curr Psychiatry Rep. 19(69)2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
De Bellis MD and Zisk A: The biological
effects of childhood trauma. Child Adolesc Psychiatr Clin N Am.
23:185–222, vii. 2014.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Danese A and Smith P: Debate: Recognising
and responding to the mental health needs of young people in the
era of COVID-19. Child Adolesc Ment Health. 25:169–170.
2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Brooks SK, Webster RK, Smith LE, Woodland
L, Wessely S, Greenberg N and Rubin GJ: The psychological impact of
quarantine and how to reduce it: Rapid review of the evidence.
Lancet. 395:912–920. 2020.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Wang G, Zhang Y, Zhao J, Zhang J and Jiang
F: Mitigate the effects of home confinement on children during the
COVID-19 outbreak. Lancet. 395:945–947. 2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Abdo C, Miranda EP, Santos CS, Júnior JB
and Bernardo WM: Domestic violence and substance abuse during
COVID19: A systematic review. Indian J Psychiatry. 62 (Suppl
3):S337–S342. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Yoshikawa H, Wuermli AJ, Britto PR, Dreyer
B, Leckman JF, Lye SJ, Ponguta LA, Richter LM and Stein A: Effects
of the Global Coronavirus Disease-2019 Pandemic on Early Childhood
Development: Short- and Long-Term Risks and Mitigating Program and
Policy Actions. J Pediatr. 223:188–193. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen
S, Wang Y, Fu H and Dai J: Mental health problems and social media
exposure during COVID-19 outbreak. PLoS One.
15(e0231924)2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Bailen NH, Green LM and Thompson RJ:
Understanding Emotion in Adolescents: A Review of Emotional
Frequency, Intensity, Instability, and Clarity. Emot Rev. 11:63–73.
2019.
|
|
44
|
Somerville LH, Jones RM and Casey BJ: A
time of change: Behavioral and neural correlates of adolescent
sensitivity to appetitive and aversive environmental cues. Brain
Cogn. 72:124–133. 2010.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Guessoum SB, Lachal J, Radjack R,
Carretier E, Minassian S, Benoit L and Moro MR: Adolescent
psychiatric disorders during the COVID-19 pandemic and lockdown.
Psychiatry Res. 291(113264)2020.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Ellis WE, Dumas TM and Forbes LM:
Physically isolated but socially connected: Psychological
adjustment and stress among adolescents during the initial COVID-19
crisis. Can J Behav Sci. 52:177–187. 2020.
|
|
47
|
Luthra R, Abramovitz R, Greenberg R,
Schoor A, Newcorn J, Schmeidler J, Levine P, Nomura Y and Chemtob
CM: Relationship between type of trauma exposure and posttraumatic
stress disorder among urban children and adolescents. J Interpers
Violence. 24:1919–1927. 2009.PubMed/NCBI View Article : Google Scholar
|
|
48
|
McLaughlin KA, Fairbank JA, Gruber MJ,
Jones RT, Osofsky JD, Pfefferbaum B, Sampson NA and Kessler RC:
Trends in serious emotional disturbance among youths exposed to
Hurricane Katrina. J Am Acad Child Adolesc Psychiatry. 49:990–1000,
1000.e1-1000.e2. 2010.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Nuttman-Shwartz O: Behavioral Responses in
Youth Exposed to Natural Disasters and Political Conflict. Curr
Psychiatry Rep. 21(42)2019.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Nöthling J, Simmons C, Suliman S and
Seedat S: Trauma type as a conditional risk factor for
posttraumatic stress disorder in a referred clinic sample of
adolescents. Compr Psychiatry. 76:138–146. 2017.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Ellis W, Zarbatany L, Chen X, Kinal M and
Boyko L: Peer Groups as a Context for School Misconduct: The
Moderating Role of Group Interactional Style. Child Dev.
89:248–263. 2018.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Parker AM, Sricharoenchai T, Raparla S,
Schneck KW, Bienvenu OJ and Needham DM: Posttraumatic stress
disorder in critical illness survivors: A metaanalysis. Crit Care
Med. 43:1121–1129. 2015.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Badenoch J, Cross B, Hafeez D, Song J,
Watson C, Butler M, Nicholson TR and Rooney AG: The SARS-COV-neuro
collaboration: Post-traumatic symptoms after COVID-19 may (or may
not) reflect disease severity. Psychol Med: Nov 27, 2020 (Epub
ahead of print).
|
|
54
|
Kaseda ET and Levine AJ: Post-traumatic
stress disorder: A differential diagnostic consideration for
COVID-19 survivors. Clin Neuropsychol. 34:1498–1514.
2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Shalev A, Liberzon I and Marmar C:
Post-traumatic stress disorder. N Engl J Med. 376:2459–2469.
2017.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Lee AM, Wong JG, McAlonan GM, Cheung V,
Cheung C, Sham PC, Chu CM, Wong PC, Tsang KW and Chua SE: Stress
and psychological distress among SARS survivors 1 year after the
outbreak. Can J Psychiatry. 52:233–240. 2007.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Mak IWC, Chu CM, Pan PC, Yiu MGC, Ho SC
and Chan VL: Risk factors for chronic post-traumatic stress
disorder (PTSD) in SARS survivors. Gen Hosp Psychiatry. 32:590–598.
2010.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Tarsitani L, Vassalini P, Koukopoulos A,
Borrazzo C, Alessi F, Di Nicolantonio C, Serra R, Alessandri F,
Ceccarelli G, Mastroianni CM, et al: Post-traumatic Stress Disorder
Among COVID-19 Survivors at 3-Month Follow-up After Hospital
Discharge. J Gen Intern Med. 36:1702–1707. 2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Chen Y, Huang X, Zhang C, An Y, Liang Y,
Yang Y and Liu Z: Prevalence and predictors of posttraumatic stress
disorder, depression and anxiety among hospitalized patients with
coronavirus disease 2019 in China. BMC Psychiatry.
21(80)2021.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Tedstone JE and Tarrier N: Posttraumatic
stress disorder following medical illness and treatment. Clin
Psychol Rev. 23:409–448. 2003.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Berntsen D and Rubin DC: The centrality of
event scale: A measure of integrating a trauma into one's identity
and its relation to post-traumatic stress disorder symptoms. Behav
Res Ther. 44:219–231. 2006.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Heir T, Piatigorsky A and Weisaeth L:
Longitudinal changes in recalled perceived life threat after a
natural disaster. Br J Psychiatry. 194:510–514. 2009.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Xie J, Tong Z, Guan X, Du B, Qiu H and
Slutsky AS: Critical care crisis and some recommendations during
the COVID-19 epidemic in China. Intensive Care Med. 46:837–840.
2020.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Gosselin E, Gelinas C, Bourgault P and
Lavoie S: Intervention for patients intubated and conscious to
decrease peritraumatic distress (IPIC-PTD)-Acceptability and
feasibility. Sci Nurs Health Pract. 1:1–15. 2018.
|
|
65
|
Matalon N, Dorman-Ilan S, Hasson-Ohayon I,
Hertz-Palmor N, Shani S, Basel D, Gross R, Chen W, Abramovich A,
Afek A, et al: Trajectories of post-traumatic stress symptoms,
anxiety, and depression in hospitalized COVID-19 patients: A
one-month follow-up. J Psychosom Res. 143(110399)2021.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Zhao YQ, An YY, Tan X and Li XH: Mental
health and its influencing factors among self-isolating ordinary
citizens during the beginning epidemic of COVID-19. J Loss Trauma.
25:580–593. 2020.
|
|
67
|
Bergman HE, Kline AC, Feeny NC and
Zoellner LA: Examining PTSD treatment choice among individuals with
subthreshold PTSD. Behav Res Ther. 73:33–41. 2015.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Watson D: Differentiating the mood and
anxiety disorders: A quadripartite model. Annu Rev Clin Psychol.
5:221–247. 2009.PubMed/NCBI View Article : Google Scholar
|